The Ultimate Guide to Drugs in Parkinsonism
Understanding the Complex World of Drugs in Parkinsonism

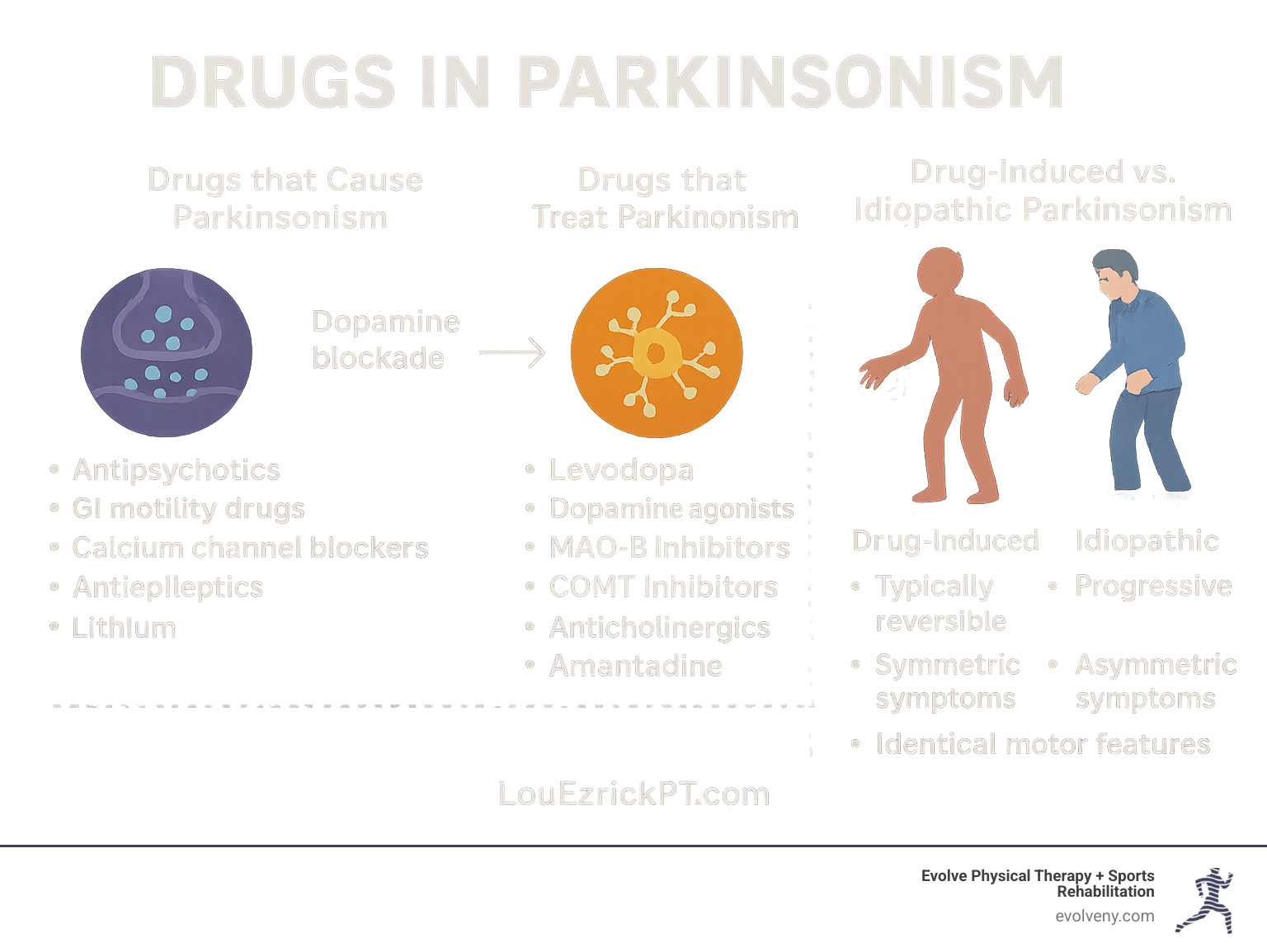
Drugs in parkinsonism fall into two main categories: those that cause parkinsonian symptoms and those that treat them. Here's a quick overview:
Drugs that can cause parkinsonism:
- Typical antipsychotics (haloperidol, chlorpromazine)
- Some atypical antipsychotics
- GI motility drugs (metoclopramide)
- Calcium channel blockers (flunarizine, cinnarizine)
- Antiepileptics (valproate)
- Lithium
Drugs that treat parkinsonism:
- Levodopa (often with carbidopa)
- Dopamine agonists (pramipexole, ropinirole)
- MAO-B inhibitors (selegiline, rasagiline)
- COMT inhibitors (entacapone, opicapone)
- Anticholinergics (trihexyphenidyl)
- Amantadine
Parkinsonism describes a group of neurological conditions characterized by movement problems similar to those seen in Parkinson's disease: tremor, rigidity, bradykinesia (slowness of movement), and postural instability. While Parkinson's disease is the most common cause, drug-induced parkinsonism (DIP) ranks as the second most prevalent form, especially in older adults.
The relationship between drugs and parkinsonism is complex. Some medications disrupt the delicate balance of dopamine in the brain, either by blocking dopamine receptors or interfering with dopamine production and storage. When this happens, the symptoms can mimic those of Parkinson's disease so closely that even experienced clinicians may struggle to tell them apart.
What makes this topic particularly important is that drug-induced parkinsonism is often reversible if caught early and the offending medication is stopped. However, studies show that in 10-50% of patients, symptoms may persist even after discontinuation, suggesting that some drugs might unmask an underlying predisposition to Parkinson's disease.
I'm Lou Ezrick, and throughout my career as a physical therapist, I've worked with numerous patients experiencing the physical limitations caused by drugs in parkinsonism, developing specialized protocols that complement medication management with targeted movement therapies.
Understanding Parkinsonism: Definitions, Types & Causes
Parkinsonism is an umbrella term for a group of neurological conditions that cause movement problems similar to those seen in Parkinson's disease. These include tremor (especially at rest), rigidity, bradykinesia (slowness of movement), and postural instability. While these symptoms might look the same on the surface, their underlying causes can vary significantly.

Idiopathic vs Secondary Syndromes
Idiopathic Parkinson's Disease (PD) is the most common form, affecting approximately 1% of individuals over the age of 65. It results from the progressive degeneration of dopamine-producing neurons in the substantia nigra, a region of the brain involved in movement control. This degeneration is associated with the accumulation of a protein called alpha-synuclein, which forms clumps known as Lewy bodies within neurons.
The progression of Parkinson's disease follows what scientists call Braak staging, where pathological changes begin in specific brain regions and spread in a predictable pattern. Interestingly, symptoms only become apparent after about 60-80% of dopaminergic neurons have been lost—highlighting the brain's remarkable compensatory abilities.
Secondary parkinsonism includes several subtypes:
Drug-Induced Parkinsonism (DIP): The second most common cause of parkinsonism, particularly in older adults. Several large, population-based studies in Europe estimated a prevalence of DIP ranging from 0.09% to 1.7%, which is only slightly lower than idiopathic PD (0.37% to 1.9%).
Vascular Parkinsonism: Caused by small strokes in brain regions controlling movement.
Post-traumatic Parkinsonism: Following severe head injury.
Toxin-induced Parkinsonism: From exposure to certain environmental toxins.
Genetic forms: Including those linked to specific gene mutations.
Key Risk Factors for Drug-Induced Cases
Understanding who's at risk for developing drug-induced parkinsonism is crucial for prevention and early intervention. Key risk factors include:
Age: The percentage of patients with drug-induced parkinsonism increases with age, with the highest incidence in those between 60 and 80 years. This is partly because dopamine cell count and transport naturally decline with age, lowering the threshold for developing parkinsonism.
Sex: Women appear more susceptible than men, with some studies showing a female-to-male ratio of 2:5.
Medication dose and duration: Higher doses and longer treatment durations increase risk.
Renal or hepatic impairment: These conditions can lead to higher blood levels of medications due to reduced clearance.
Polypharmacy: Taking multiple medications that affect dopamine pathways can have additive effects.
Genetic factors: Some genetic variants may predispose individuals to developing DIP.
It's worth noting that about 50% of patients with DIP are treated with dopamine receptor blocking agents for conditions unrelated to psychosis, including depression, gastrointestinal disturbances, anxiety, and insomnia—highlighting the importance of medication review across all specialties.
The Ultimate Breakdown of Drugs in Parkinsonism: Offending & Therapeutic Agents
When it comes to drugs in parkinsonism, there's a fascinating paradox at work. Some medications can trigger parkinsonian symptoms, while others are specifically designed to relieve them. Understanding this dual relationship is essential for anyone navigating this complex neurological territory.
Which Drugs in Parkinsonism Are Most Likely to Cause Symptoms?
The medications most likely to trigger parkinsonian symptoms typically work by interfering with dopamine—either by blocking its receptors or disrupting its storage and release in the brain.
The most common culprits are antipsychotics, especially the older "typical" ones like haloperidol and chlorpromazine. These medications pack a powerful dopamine-blocking punch, with studies showing that about 40% of patients taking chlorpromazine develop parkinsonian side effects. In fact, about 80% of people taking typical antipsychotics will experience at least one type of movement-related side effect.
Surprisingly, medications prescribed for completely unrelated conditions can also trigger parkinsonism. Metoclopramide, commonly used for nausea and digestive issues, crosses into the brain and blocks dopamine receptors. Similarly, certain calcium channel blockers like flunarizine, prescribed for migraines and dizziness, can cause parkinsonism through mechanisms that researchers are still working to fully understand.
Other medications to watch out for include the antiepileptic drug valproate (causing parkinsonism in about 5% of long-term users), mood stabilizers like lithium, and various antidepressants and cardiac medications. The prevalence of drug-induced parkinsonism ranges from 0.09% to 1.7% in the general population—nearly as common as Parkinson's disease itself.
Therapeutic Drugs for Managing Parkinsonism
On the flip side, several medication classes help manage parkinsonian symptoms by boosting dopamine function in the brain.
Levodopa/carbidopa remains the gold standard treatment. Levodopa converts to dopamine in the brain, while carbidopa prevents its breakdown outside the brain, reducing side effects. It comes in various formulations, from immediate-release tablets to extended-release capsules and even an intestinal gel for advanced cases. With a short half-life of about 90 minutes, long-term users often develop "wearing off" symptoms as the medication's effects fluctuate.
Dopamine agonists like pramipexole and ropinirole work differently—they directly stimulate dopamine receptors, bypassing the need for dopamine production entirely. These medications last longer in the body (4-6 hours) and may cause fewer motor fluctuations, but they tend to bring more psychiatric side effects like hallucinations and compulsive behaviors.
For many patients, the supporting cast of medications is just as important. MAO-B inhibitors like selegiline and rasagiline prevent dopamine breakdown in the brain, while COMT inhibitors like entacapone extend levodopa's effects. Amantadine, originally developed as an antiviral medication, helps release dopamine from nerve terminals and can reduce the involuntary movements (dyskinesias) that often develop with long-term levodopa use.
Anticholinergics such as trihexyphenidyl may help with tremor but come with significant cognitive side effects, especially for older adults. The newest addition to the arsenal, istradefylline, works through a completely different mechanism (adenosine A2A antagonism) to help with "off" episodes.
Pathophysiology & Course after Drug Exposure
Drug-induced parkinsonism differs from Parkinson's disease at the cellular level. While Parkinson's involves the death of dopamine-producing neurons, drug-induced parkinsonism temporarily blocks dopamine receptors without killing cells—like putting a lock on a door rather than demolishing the building.
After starting an offending medication, symptoms typically appear within days to months. The good news is that after stopping the medication, most people improve within weeks to months. However, in 10-50% of patients, symptoms persist or progress, suggesting that the medication may have unmasked an underlying predisposition to Parkinson's disease. Even more intriguingly, in about 7% of patients who fully recover, symptoms mysteriously return months later.
| Feature | Drug-Induced Parkinsonism | Idiopathic Parkinson's Disease |
|---|---|---|
| Onset | Subacute (days to months) | Gradual (months to years) |
| Symmetry | Usually symmetric | Typically asymmetric |
| Tremor | Less common, symmetric | Common, asymmetric rest tremor |
| DAT imaging | Normal DAT uptake | Reduced asymmetric DAT uptake |
| Response to levodopa | Limited or poor | Good |
| Progression after drug cessation | Usually resolves (50-90%) | Progressive |
| Risk factors | Age, female sex, high medication dose | Age, family history, environmental exposures |
Understanding these patterns helps clinicians distinguish between drug-induced and idiopathic parkinsonism—a critical distinction that determines treatment approach and long-term prognosis. At Evolve Physical Therapy, we work alongside your medical team to provide comprehensive care that addresses both the neurological and physical aspects of parkinsonism, regardless of its cause.
Diagnosing & Differentiating Drug-Induced Parkinsonism
Telling the difference between drug-induced parkinsonism (DIP) and idiopathic Parkinson's disease (PD) can feel like detective work. As someone who's worked with many patients facing this exact challenge, I can tell you that the distinction is crucial – yet the symptoms can look nearly identical to even trained eyes.

When a patient comes to us with parkinsonian symptoms, we start with a comprehensive approach:
First, we dive into their medication history – did symptoms appear after starting a new medication? We're particularly interested in recent additions of any dopamine-blocking agents. I once had a patient whose tremor began just weeks after starting an anti-nausea medication she didn't even realize could affect her movement.
Next comes a thorough medication review, including those over-the-counter supplements many patients forget to mention. You'd be surprised how often the culprit is hiding in plain sight!
During the neurological examination, we use tools like the Unified Parkinson's Disease Rating Scale (UPDRS) to objectively measure symptoms. We're looking for patterns – is the tremor symmetrical? How severe is the rigidity? Does the patient have that characteristic "masked face" expression?
Role of Imaging in Confirming or Ruling Out PD
Brain imaging has truly transformed how we distinguish between these conditions. When clinical evaluation leaves us uncertain, these tests can provide clarity:
DAT-SPECT imaging has become our gold standard. This specialized brain scan uses radioactive tracers that bind to dopamine transporters in the brain. What we're looking for is quite straightforward: in drugs in parkinsonism cases, these scans typically show normal dopamine transporter binding. In contrast, Parkinson's disease patients show reduced binding, usually in an asymmetric pattern.
Other options include PET scans (offering higher resolution) and Beta-CIT SPECT (with impressive 87.7% diagnostic accuracy in distinguishing between the two conditions).
These imaging tests become particularly valuable when symptoms stick around after stopping the suspected medication, or when something about the clinical picture just doesn't add up. Research published in the Journal of Neurology, Neurosurgery & Psychiatry has shown that DAT-SPECT can significantly improve diagnostic accuracy, with one study finding that nearly 7% of patients initially diagnosed with PD were actually suffering from drug-induced symptoms.
Red Flags Suggesting Underlying Degeneration
Sometimes what looks like simple medication side effects might actually be an underlying Parkinson's disease that was "unmasked" by the medication. Here are the warning signs we watch for:
Asymmetric symptoms often point to PD – when tremor or stiffness affects one side of the body more than the other, it's less likely to be medication-related. Classic rest tremor that has that "pill-rolling" quality between thumb and forefinger is another red flag.
Other concerning signs include reduced sense of smell (which often precedes motor symptoms in PD by years), REM sleep behavior disorder (acting out dreams during sleep), and continued progression despite stopping the medication.
I remember working with a gentleman who initially improved after stopping his antipsychotic medication, but then noticed his symptoms returning months later. His neurologist ordered a DAT scan, which revealed early Parkinson's disease – the medication had simply revealed what was already beginning.
Response to levodopa can also be telling – significant improvement with this medication typically suggests true Parkinson's rather than drug-induced symptoms.
At Evolve Physical Therapy + Sports Rehabilitation, we partner closely with neurologists to ensure our patients receive an accurate diagnosis. This collaboration forms the foundation for our specialized physical therapy interventions, allowing us to tailor our approach to each individual's unique needs and underlying condition.
Treating, Managing & Preventing Drug-Induced Parkinsonism
The management of drug-induced parkinsonism (DIP) differs significantly from that of idiopathic Parkinson's disease, primarily because DIP is often reversible when the offending medication is discontinued.

Do Standard Drugs in Parkinsonism Help Drug-Induced Cases?
When it comes to drugs in parkinsonism that's triggered by medications, the treatment approach is quite different from what works for Parkinson's disease itself.
Levodopa, the gold standard treatment for Parkinson's disease, typically doesn't work as well for drug-induced cases. This makes perfect sense when you think about it - in DIP, those dopamine receptors are being blocked rather than depleted. Adding more dopamine through levodopa is a bit like trying to enter a locked door by pushing harder - the key issue is the lock, not the force!
That said, we sometimes do try a careful course of levodopa if we can't stop the offending medication, or if symptoms stick around after withdrawal. Interestingly, contrary to what many doctors learned in medical school, giving levodopa to DIP patients doesn't necessarily make their psychotic symptoms worse.
Anticholinergic medications like trihexyphenidyl and benztropine can actually help in DIP cases by rebalancing the dopamine-acetylcholine relationship in the brain. The downside? They can make you feel like you've got a mouth full of cotton, blur your vision, and confuse your thinking - especially troublesome for older adults who are already the most vulnerable to DIP.
Amantadine often proves to be a better option, especially for our older patients. It works through several mechanisms and typically causes fewer cognitive side effects than anticholinergics.

The most effective approach to managing DIP is straightforward but requires careful coordination with your prescribing doctor. First and foremost, discontinuing or reducing the offending medication is the most effective strategy when possible. About 70% of patients show improvement within weeks to months after stopping the troublemaker drug.
If you can't completely stop a psychiatric medication, switching to alternatives with lower risk makes sense. Quetiapine or clozapine typically cause fewer movement problems than older antipsychotics. For digestive issues, domperidone (which doesn't cross into the brain) is preferable to metoclopramide.
When stopping medications, a gradual approach is usually best. Quitting certain drugs cold turkey (especially antipsychotics) can trigger withdrawal symptoms or a flare-up of the condition being treated.
For persistent symptoms, we might recommend anticholinergics or amantadine, but we'll keep a close eye on side effects, especially in our older patients. We typically limit how long someone stays on anticholinergics when possible.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen remarkable results when combining medication management with specialized physical therapy. Our programs include gait training to improve walking, balance exercises to prevent falls, and strength training to maintain muscle function. Many of our patients with parkinsonism symptoms have benefited tremendously from our Rock Steady Boxing program, which specifically targets Parkinson's symptoms through an engaging, fun format that doesn't feel like traditional therapy.
Prevention Strategies for High-Risk Populations
An ounce of prevention is worth a pound of cure - especially true for drugs in parkinsonism. For those at higher risk (older adults, women, and people with existing neurological issues), we recommend several protective strategies.
First, careful drug selection is crucial. When possible, avoid medications that block dopamine, especially in high-risk individuals. When these medications are necessary, use the lowest effective dose possible.
Regular monitoring makes a huge difference - checking for subtle signs of parkinsonism every 3-6 months can catch problems early. We also emphasize patient and caregiver education so everyone knows what early warning signs look like.
For conditions like nausea or vertigo, exploring alternative treatments without dopamine-blocking properties can prevent problems before they start. And regular medication reconciliation helps identify potential drug interactions that might increase DIP risk.
At Evolve Physical Therapy + Sports Rehabilitation, we work as part of your healthcare team, collaborating with neurologists and primary care physicians to provide comprehensive care. We combine our specialized physical therapy interventions with medication management guidance to help you recover faster and prevent recurrence. Our hands-on approach means we're with you every step of the way, celebrating each improvement and adjusting strategies as needed to optimize your recovery.
Frequently Asked Questions about Drugs in Parkinsonism
What is the difference between drug-induced and idiopathic Parkinson's disease?
If you've ever wondered about the key differences between these two conditions, you're not alone. While they may look similar on the surface, they're actually quite distinct under the hood.
Drug-induced parkinsonism (DIP) happens when certain medications disrupt your brain's dopamine system. Think of it as temporarily jamming the signals that control movement. In contrast, idiopathic Parkinson's disease involves the actual death of dopamine-producing cells in your brain – a much more permanent situation.
You can often spot the difference in how symptoms appear. DIP typically affects both sides of your body equally, while Parkinson's disease usually starts on one side before spreading. When doctors perform specialized brain scans (dopamine transporter imaging), DIP patients show normal dopamine activity, while those with Parkinson's show reduced activity.
Perhaps most importantly, DIP has a good chance of reversing once you stop taking the problematic medication, while Parkinson's disease continues to progress over time. This reversibility is why proper diagnosis is so crucial – it could mean the difference between a temporary and a lifelong condition.
How long does parkinsonism last after stopping the culprit drug?
"When will I feel normal again?" This is often the first question patients ask after learning their symptoms are medication-related. The good news is that improvement typically begins within days to weeks after stopping the offending medication.
Most people experience complete resolution within 2-6 months. Research shows the average recovery time is about 13 weeks, though this varies from person to person. Your age, how long you took the medication, and your overall health all influence your recovery timeline.
It's important to know that for some patients—about 10-50% according to studies—symptoms may persist even after stopping the medication. This doesn't necessarily mean the drug caused permanent damage; rather, it might have unmasked an underlying predisposition to Parkinson's disease that would have eventually emerged anyway.
In a small percentage of cases (around 7%), symptoms may completely resolve but then return months later. This is why we at Evolve Physical Therapy + Sports Rehabilitation recommend ongoing monitoring even after symptoms improve.
Can physical therapy replace medications for drug-induced parkinsonism?
While physical therapy can't replace the critical step of discontinuing the problematic medication, it plays an invaluable supporting role in recovery. I've seen how the right physical therapy approach can dramatically improve quality of life while patients wait for medication effects to wear off.
At Evolve Physical Therapy + Sports Rehabilitation, we focus on addressing the specific movement challenges caused by drugs in parkinsonism. Our specialized programs target rigidity, improve balance, and help restore normal movement patterns through neuroplasticity – your brain's remarkable ability to rewire itself with proper stimulation.
One of our most successful programs is Rock Steady Boxing, which was even featured on NBC News for its effectiveness in combating parkinsonian symptoms. The program's combination of high-intensity exercise, cognitive challenges, and social interaction creates the perfect environment for neurological recovery.
Even when medications cannot be discontinued (which happens in some psychiatric conditions), our physical therapy approaches can significantly improve function and prevent complications like muscle contractures and falls. We've seen patients regain independence in daily activities even while continuing necessary psychiatric medications.
The research strongly supports this combined approach – patients who receive both appropriate medication management and specialized physical therapy consistently show better outcomes than those receiving either intervention alone. This is why we work closely with neurologists and primary care physicians to coordinate care for optimal results.
Your body has an amazing capacity to heal when given the right support. Our team is here to guide that process every step of the way.
Conclusion
Navigating the complex world of drugs in parkinsonism is like finding your way through a maze—it requires understanding both the medications that trigger symptoms and those that provide relief. Throughout this guide, we've seen how drug-induced parkinsonism represents a significant portion of cases, especially among older adults, yet it often flies under the diagnostic radar.
The silver lining is that with proper identification and timely intervention, many people suffering from drug-induced parkinsonism can experience a reversal of their symptoms. Recovery begins with early recognition—noticing when tremors or stiffness appear shortly after starting a new medication. A proper diagnostic workup, sometimes including specialized brain imaging, helps distinguish drug-induced symptoms from Parkinson's disease.
When possible, the most effective approach is simply stopping the problematic medication. This often requires working with your doctor to find alternative treatments for your underlying condition—whether it's a mental health issue, digestive problem, or another medical concern. In some cases, medications specifically designed for Parkinson's disease may help manage symptoms while waiting for the effects of the offending drug to wear off.
Here at Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe that managing parkinsonism goes beyond medication adjustments. Our hands-on programs provide the human touch that complements medical care. Many of our patients find remarkable benefits from our Rock Steady Boxing program (the same one featured on NBC News), which specifically targets the motor symptoms that make daily activities challenging.
We take pride in our holistic approach, recognizing that each person's experience with parkinsonism is unique. Whether you're dealing with medication-induced symptoms or idiopathic Parkinson's disease, our team works in harmony with your neurologists and primary care physicians to create a coordinated care plan that addresses all aspects of your condition.
Drug-induced parkinsonism, while certainly challenging, stands out as one of the few potentially reversible forms of parkinsonism. With quick recognition, appropriate medical management, and specialized physical therapy, many patients can reclaim their mobility and quality of life.
If you're experiencing shakiness, stiffness, or slowness of movement and take any of the medications we've discussed, we encourage you to have a conversation with your healthcare provider. Consider how our specialized physical therapy services might complement your medical care and accelerate your recovery.
For our neighbors in Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin areas—our team at Evolve Physical Therapy + Sports Rehabilitation is ready to support your journey back to fluid, confident movement and improved quality of life. Your recovery doesn't have to be a solo journey—we're here to walk alongside you every step of the way.

