A Practical Guide to Post-Surgical Physical Therapy
Why Post-Surgical Physical Therapy Is Essential for Your Recovery

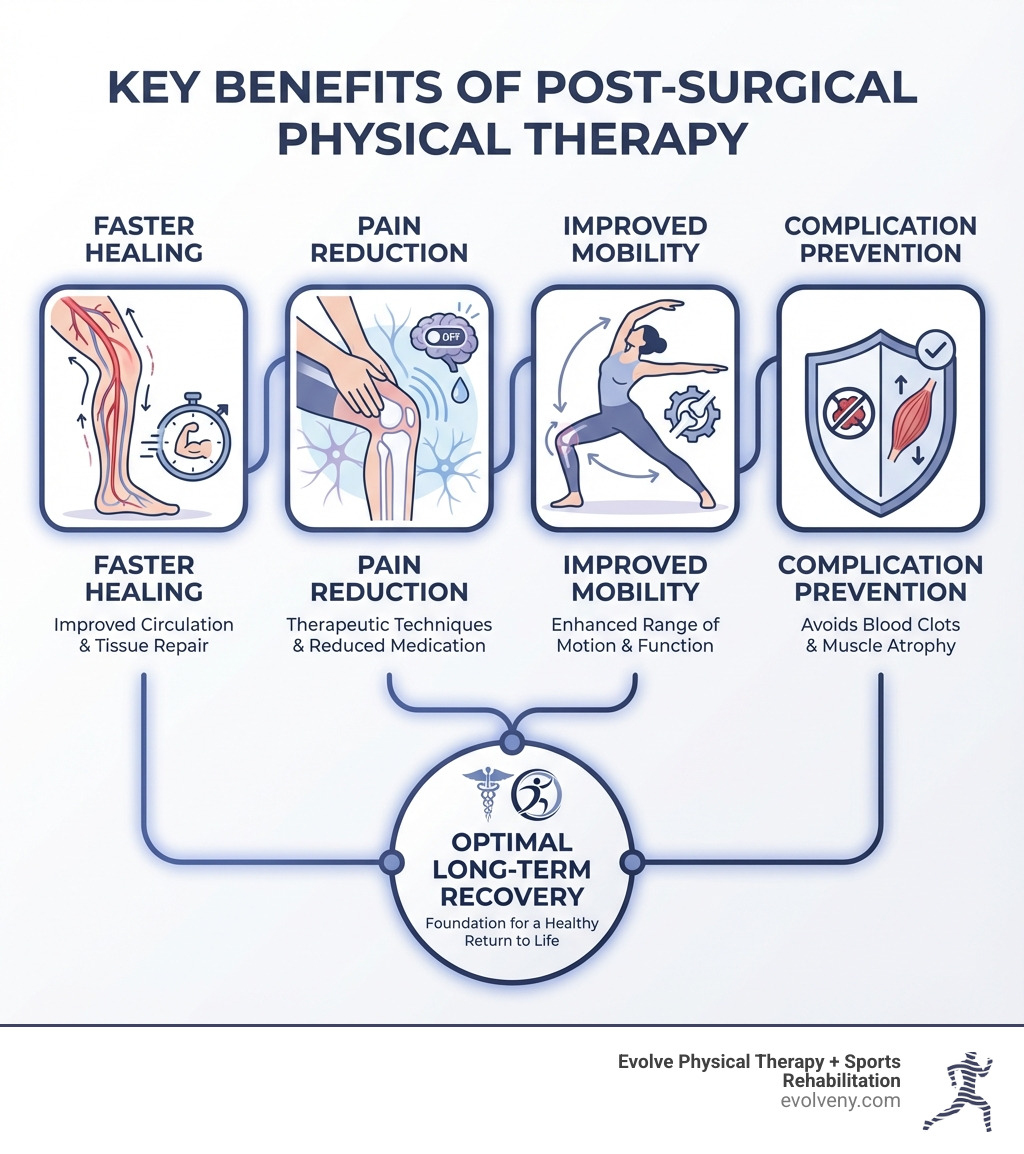
Post-surgical physical therapy is a structured rehabilitation program designed to help you regain strength, mobility, and function after surgery. Here's what you need to know:
- Faster Recovery: Early mobilization and targeted exercises help you heal more quickly than rest alone
- Pain Management: Physical therapy reduces post-operative pain and can decrease your need for pain medication
- Complication Prevention: Guided movement helps prevent blood clots, muscle atrophy, and joint stiffness
- Functional Restoration: Progressive exercises rebuild strength and return you to daily activities and sports
- Personalized Care: Your treatment plan is custom to your specific surgery, body, and recovery goals
Surgery is often just the first step toward full recovery. The real work of healing happens in the weeks and months that follow, when your body needs guidance to rebuild what was disrupted. Without proper rehabilitation, you risk incomplete healing, reduced range of motion, and long-term functional limitations.
Research consistently shows that patients who engage in post-surgical physical therapy experience significantly better outcomes than those who don't. A 2017 study published in Acta Medica found that beginning physical therapy following joint replacement surgery can reduce hospital stays and speed up recovery. The evidence is clear: structured rehabilitation is not optional—it's essential for optimal healing.
Physical therapy addresses the natural consequences of surgery: muscle weakness, joint stiffness, scar tissue formation, and altered movement patterns. Your body needs strategic intervention to prevent these issues from becoming permanent. Through hands-on techniques, progressive exercises, and patient education, physical therapists guide your tissues through the healing process while preventing complications like blood clots and chronic pain.
The journey from surgery to full function requires expertise, patience, and a personalized approach. I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've spent nearly two decades specializing in post-surgical physical therapy, helping patients recover from complex orthopedic procedures and return to the activities they love. My experience treating trauma victims and athletes has taught me that successful recovery requires addressing not just symptoms, but the root causes of dysfunction.
The Crucial Role of Post-Surgical Physical Therapy in Your Recovery
Undergoing surgery is a significant event, and while the surgical procedure itself is critical, what happens afterward plays an equally vital role in your long-term health and well-being. Our bodies are incredibly resilient, but they need guidance to heal properly, regain strength, and restore full function. This is where post-surgical physical therapy becomes not just beneficial, but crucial.
The fundamental goal of physical therapy after surgery is to restore optimal body functionality. Without it, the body's natural response to surgery can lead to muscle and tissue tightness, swelling, limited range of motion, and a decline in overall physical capabilities. Patients who stay in bed after surgery, for instance, tend to lose muscle strength, heart capacity, and lung capacity due to a lack of physical activity. This inactivity can lead to improper healing, which can manifest as reduced range of motion, flexibility, and functionality, sometimes even necessitating further medical intervention.
Physical therapy is a specialized form of healthcare that aims to alleviate pain, expedite recovery, and restore optimal body functionality through techniques like targeted exercises, manual therapy, and advanced equipment. It's rooted in a deep understanding of musculoskeletal science, anatomy, and physiology, allowing our therapists to create personalized treatment plans that are evidence-based and highly effective.

Restoring Mobility and Function
One of the primary aims of post-surgical physical therapy is to restore the mobility and function that may have been lost due to injury, surgery, or prolonged immobilization. Surgery often causes temporary mobility limitations to the impacted region. Our physical therapists employ a variety of interventions to help you regain your range of motion (ROM) and improve flexibility. This can include gentle stretching, passive and active ROM exercises, and specialized techniques to address scar tissue.
Beyond just movement, we focus on rebuilding muscle strength, which is essential for supporting the surgical site and enabling functional independence. Through progressive resistance training and targeted exercises, we help strengthen not only the affected area but also surrounding muscles to ensure comprehensive support. For instance, after ACL and meniscus repair, we focus on building quadriceps and hamstring strength.
Improving balance and coordination is another key component, especially for surgeries affecting the lower extremities or spine. Exercises that strengthen core, back, and pelvic muscles increase stability and improve balance, reducing the risk of falls. In cases like neurosurgery, gait training helps to "rewire" the brain to control walking muscles through neuroplasticity, helping patients regain pre-surgery functionalities like increased range of movement, improved gait, and reduced spasticity. Research has shown that early ambulation after hip surgery accelerates recovery, and initiating physical therapy on the day of surgery can decrease length of stay without compromising functional outcomes for total hip arthroplasty patients. This evidence for accelerated recovery underscores the importance of early intervention.
Managing Pain and Preventing Complications
Pain is an inevitable part of the post-surgical experience, but post-surgical physical therapy plays a significant role in managing it effectively. Physical therapists use various techniques to reduce swelling and inflammation, which are major contributors to post-operative discomfort. These can include cold and heat therapy, gentle massage, and manual therapy techniques. By addressing the underlying causes of pain, physical therapy can often decrease your reliance on pain medication, including opioids, which is a significant benefit for your overall health and recovery.
Beyond pain management, a critical aspect of our work is preventing common post-surgical complications. Prolonged immobility after surgery can lead to serious issues such as blood clots (deep vein thrombosis or DVT), pneumonia, and muscle atrophy. Our therapists guide you through early, controlled movements and exercises designed to stimulate circulation, promote lung function, and maintain muscle mass, significantly reducing these risks. For example, staying active with physical therapy interventions can counteract the decline in cardiovascular fitness and respiratory issues caused by inactivity.
Furthermore, physical therapy aids in proper wound healing by minimizing scar tissue formation. Mobilization techniques and therapeutic ultrasound can help soften scar tissue, improving flexibility and preventing stiffness. By actively engaging in rehabilitation, we also help prevent the development of chronic pain, especially after procedures like lumbar spinal stenosis surgery. Our custom exercises are designed to decrease the risk of infection and contractures, ensuring a smoother, more complete recovery.
Navigating the Phases of Post-Surgical Rehabilitation
The journey through post-surgical physical therapy is not a sprint, but a carefully planned marathon, divided into distinct phases. Each phase has specific goals, exercises, and precautions, all custom to your individual healing process and surgical procedure. Our approach at Evolve Physical Therapy in Brooklyn is always personalized, recognizing that every patient's recovery is unique. We collaborate closely with your surgeon and primary care providers to ensure a seamless continuity of care, adjusting your plan as your body progresses.
The progression through these phases is guided by your body's healing, pain levels, and functional milestones. While there are general timelines, these are merely guidelines; your physical therapist will assess your readiness to advance, ensuring you're not pushing too hard too soon, or holding back unnecessarily. Patient adherence to the prescribed exercises and recommendations is paramount for successful outcomes.

The Immediate Post-Operative Phase (Phase 1: Protection & Healing)
This initial phase typically begins within days to a few weeks after surgery, sometimes even on the day of surgery itself. The primary goals are pain and swelling control, protecting the surgical site, and preventing complications. Rest is crucial, but not prolonged bed rest, which can lead to loss of muscle strength, heart capacity, and lung capacity. Instead, we focus on gentle, controlled motion.
In this phase, you might learn techniques for safe movement, such as log-rolling to get out of bed after abdominal surgery, or specific ways to protect your incision during daily activities like coughing or sneezing. Diaphragmatic breathing exercises are often introduced to promote optimal respiratory function and prevent lung complications. For example, after abdominal core surgery, we recommend not lifting more than 5 pounds for the first 3 days, and not more than 10 pounds until 2 weeks post-operatively. Early mobilization, as gentle as it may be, is key here, as studies have shown it can prevent complications like muscle atrophy, joint stiffness, and blood circulation issues.
The Strengthening and Mobility Phase (Phase 2: Restoring Function)
Once initial pain and swelling have subsided and the surgical site shows signs of stable healing, we transition into Phase 2. This phase, typically spanning early weeks to several months, focuses on regaining a full range of motion, building strength, and improving stability. The pain should be reduced, allowing for more active engagement in rehabilitation.
Our physical therapists will introduce progressive exercises designed to challenge your muscles and joints safely. This might include active range of motion exercises, light resistance training, and balance exercises. For instance, after top surgery, patients progress to exercises like Serratus Pushes and Band Pull-Aparts to increase shoulder range of motion beyond 90 degrees. The research on early rehabilitation, such as a study on early inpatient rehabilitation after elective hip and knee arthroplasty, supports the effectiveness of this progressive approach. Our aim is to restore your movement patterns and build the foundational strength needed for more complex activities.
The Functional Restoration Phase (Phase 3: Returning to Life)
The final phase, often beginning several months after surgery and continuing as needed, is all about returning you to your desired daily activities, hobbies, and even sports. This phase involves advanced strengthening, endurance training, and highly specific functional movements that mimic the demands of your life.
For athletes recovering from sports injuries, this might include sport-specific drills, agility training, and plyometrics to ensure a safe return to play. For others, it might mean regaining the ability to lift groceries, garden, or play with grandchildren without pain or limitation. We also focus heavily on injury prevention, teaching you proper body mechanics and exercise techniques to minimize the risk of re-injury and ensure long-term success. The goal is not just to heal, but to thrive, equipped with the knowledge and strength to maintain your physical well-being.
What to Expect: From Common Surgeries to Your First Session
Starting on post-surgical physical therapy can feel like a big step, but knowing what to expect can ease any anxieties. Our process at Evolve Physical Therapy in Brooklyn is designed to be clear, supportive, and effective, guiding you every step of the way towards your recovery goals.
Common Surgeries That Benefit from Post-Surgical Physical Therapy
While many conditions benefit from physical therapy, certain surgeries almost universally require it for optimal recovery. Here are some of the most common procedures where physical therapy is a critical component:
- Joint Replacements (Knee, Hip, Shoulder): Whether it's a total knee arthroplasty (TKA), total hip arthroplasty (THA), or shoulder replacement, physical therapy is vital for regaining range of motion, strength, and mobility. Early initiation of PT for joint replacements can reduce hospital stays and speed up recovery.
- Ligament Reconstructions (ACL, MCL): For athletes and active individuals, surgeries like anterior cruciate ligament (ACL) reconstruction demand rigorous physical therapy to restore stability, strength, and return to sport. Our sports physical therapy programs in Brooklyn focus on specific strengthening and functional training.
- Rotator Cuff Repair: Shoulder surgeries, particularly rotator cuff repairs, require careful rehabilitation to restore shoulder function, prevent stiffness, and rebuild strength. Combining manual therapy with therapeutic exercise is often found to be superior for pain relief and functional improvements.
- Spinal Surgery (Laminectomy, Fusion): Procedures like lumbar laminectomy or spinal fusion necessitate physical therapy to improve core stability, mobility, and manage pain, ensuring a safe return to daily activities while protecting the spine.
- Fracture Repairs: After a bone fracture has been surgically stabilized, physical therapy helps to restore joint mobility, muscle strength around the fracture site, and overall function.
- Abdominal Surgery: Including hernia repairs and abdominal wall reconstruction, these surgeries benefit from physical therapy to restore core strength, manage pain, and guide safe movement patterns, with protocols often starting after week two post-operatively.
What to Expect During a Post-Surgical Physical Therapy Session
Your first visit to Evolve Physical Therapy in Brooklyn will begin with a thorough initial evaluation. This involves a detailed discussion about your surgical history, current symptoms, pain levels, and your personal recovery goals. We'll assess your range of motion, strength, balance, and functional capabilities. This comprehensive assessment allows us to understand your unique needs and tailor a treatment plan specifically for you.
During subsequent sessions, you can expect a dynamic and hands-on approach:
- Assessment of Pain and Mobility: Each session begins with a check-in on your current pain levels, how you're moving, and any changes since your last visit. This ongoing assessment ensures your treatment plan remains responsive to your body's needs.
- Manual Therapy: Our therapists are highly skilled in manual therapy techniques, using their hands to mobilize joints, release tight muscles, and reduce scar tissue. This hands-on approach helps improve circulation, reduce swelling, and improve flexibility, which is particularly effective for managing post-operative pain and stiffness.
- Therapeutic Exercises: You'll be guided through a series of therapeutic exercises, including stretching to improve flexibility and range of motion, and strengthening exercises to rebuild muscle mass and support the surgical area. These exercises are progressive, meaning they will gradually increase in intensity as your strength and mobility improve.
- Modalities: Depending on your needs, we may incorporate various modalities such as ice or heat therapy to manage pain and swelling, or electrical stimulation to aid muscle activation and pain relief.
- Education on Home Exercise Programs: A crucial part of your recovery happens outside the clinic. We'll teach you a personalized home exercise program, complete with clear instructions and demonstrations, empowering you to actively participate in your healing every day.
Taking an Active Role in Your Recovery
Your recovery journey after surgery is a partnership, and you are the most important member of the team. While our physical therapists are highly trained musculoskeletal experts who will guide and support you, your active engagement is key to achieving the best possible outcomes. A 2013 review showed that patients who actively participate in their own recovery process have better results and recovery experiences.
Formal Physical Therapy vs. Nurse-Assisted Ambulation
Sometimes, patients or even medical professionals might wonder about the difference between formal physical therapy and nurse-assisted ambulation. While both involve movement, their scope and impact on recovery can differ significantly. Let's look at some comparisons, based on research focusing on post-operative outcomes after elective spine surgery:
| Feature | Nurse-Assisted Ambulation | Formal Physical Therapy - The physical therapist will work on strengthening exercises to increase the muscle strength needed to protect the hip joint and increase mobility.
- Patients will also work on improving their balance and coordination, which is critical for preventing falls and regaining confidence in their movements.
- After hip surgery, patients will need to adhere to specific precautions to avoid dislocating the new hip joint. The physical therapist will educate the patient on these precautions.
Taking an Active Role in Your Recovery
Your recovery journey after surgery is a partnership, and you are the most important member of the team. While our physical therapists are highly trained musculoskeletal experts who will guide and support you, your active engagement is key to achieving the best possible outcomes. A 2013 review showed that patients who actively participate in their own recovery process have better results and recovery experiences.
Formal Physical Therapy vs. Nurse-Assisted Ambulation
Sometimes, patients or even medical professionals might wonder about the difference between formal physical therapy and nurse-assisted ambulation. While both involve movement, their scope and impact on recovery can differ significantly. Let's look at some comparisons, based on research focusing on post-operative outcomes after elective spine surgery:

