Brooklyn Physical Therapy News- Evolve NY
What is Hip Impingement and How Can PT Help?
What is hip impingement?
Femoracetabular impingement (FAI) is a condition in which bone spurs grow on the joint surfaces of the hip. These bone spurs eventually lead to irritation of the structures at the hip, which may lead to soft tissue damage such as labrum tears and potentially arthritis.
The two types of FAI are cam lesions and pincer lesions. Cam lesions develop on the head of the femur, therefore affecting the shape of the bone. Pincer lesions form on the pelvic surface of the hip joint. There are also situations in which both of these types of lesions are present…
By Nick Mazzone PT, DPT, CSCS
What is hip impingement?
Femoracetabular impingement (FAI) is a condition in which bone spurs grow on the joint surfaces of the hip. These bone spurs eventually lead to irritation of the structures at the hip, which may lead to soft tissue damage such as labrum tears and potentially arthritis.
The two types of FAI are cam lesions and pincer lesions. Cam lesions develop on the head of the femur, therefore affecting the shape of the bone. Pincer lesions form on the pelvic surface of the hip joint. There are also situations in which both of these types of lesions are present.
What causes FAI?
Cam and pincer lesions may form due to abnormal development of the hip joint during childhood. They may also develop after prolonged pressure on the front of the hip joint over time due to asymmetries in muscle strength among the prime movers of the hip (for example, overactive hip flexors and underactive glutes).
What can be done to improve FAI?
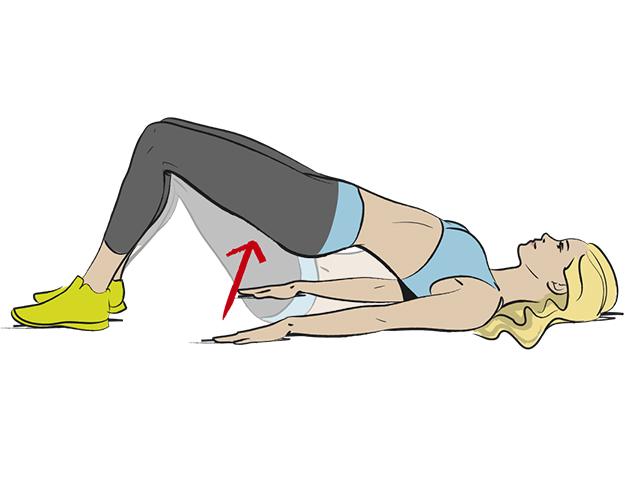
It is imperative that we address the strength deficits present in this situation. If you have weak gluteus maximus muscles and your hip flexors are overactive, you would expect the hip joint to be sitting in a suboptimal position during functional tasks. In this scenario, you would see the femur sitting in front of its optimal position in the socket. For this reason, you want to strengthen the gluteus maximus muscles in order to realign the hip joint and prevent excessive pressure on the structures in front of the hip. Sometimes it is indicated to stretch the hip flexors, but that should be dependent on the physical therapist’s evaluation. Just because a muscle is overactive and tense does not mean it is short of length. It is also important that we strengthen the lower abdominal muscles to help stabilize the pelvis. This should help decrease the tension in the hip flexor muscles which may have been acting as a pelvic stabilizer (thus leading to overactivity).
How can PT help?
Your physical therapist will develop a specific treatment plan according to the findings of the clinical exam. While two people may both be diagnosed with hip impingement, they may present in completely different ways and with different impairments to address. For this reason, it is important to be evaluated and treated with a plan specific to you and not a general exercise plan. Your specific treatment plan is aimed at helping you return to your prior level of physical activity without pain.
Click here for more information about hip physical therapy in Brooklyn, or
Check out this video that shows three simple exercises you can do to help improve your symptoms from hip impingement:
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com
Resources
Femoroacetabular Impingement - OrthoInfo - AAOS. (n.d.). Retrieved from https://orthoinfo.aaos.org/en/diseases--conditions/femoroacetabular-impingement
Main photo retrieved from https://reverehealth.com/live-better/what-is-hip-impingement/
Photo of bridging exercise retrieved from http://www.womenshealthmag.co.uk/fitness/find-a-workout/4456/how-to-do-glute-bridges/
Photo of cam and pincer lesions retrieved from https://orthoinfo.aaos.org/en/diseases--conditions/femoroacetabular-impingement
Photo of muscle asymmetries retrieved from http://www.racquetfit.com/articles/Coaching/controlling_your_posture_and_the_serve
Photo of plank exercise retrieved from https://www.waysandhow.com/good-reasons-plank-daily-6-benefits-planks-exercise/
Photo of runner retrieved from http://lisabaylis.com/2017/07/15/running-for-wellness/
Thoracic Mobility: Why is it Important?
What is the thoracic spine?
The thoracic spine is the middle portion of the spinal column that connects the neck to the lower back region. It consists of 12 separate segments that serve as connections for the ribs, which protect many vital organs including the heart and lungs.
By Nick Mazzone PT, DPT, CSCS
What is the thoracic spine?
The thoracic spine is the middle portion of the spinal column that connects the neck to the lower back region. It consists of 12 separate segments that serve as connections for the ribs, which protect many vital organs including the heart and lungs.
Why is mobility here so important?
It is vital that you have adequate mobility in this region because of the interdependent relationship it has with the cervical and lumbar spine. If you do not have enough motion in the mid back, the nervous system depends more heavily on the upper and lower spine to make up for that motion. This lack of thoracic mobility can then be a contributor to neck pain or low back pain.
Overhead mobility
We need adequate thoracic mobility in order to move our shoulder joints into their natural end ranges of motion. If we do not have enough mobility here, more strain is then placed on the glenohumeral joint (shoulder ball-and-socket joint). In this case, we usually see a compensatory increase in motion at the shoulder joint that may lead to increased pressure or strain on the soft tissue in this region. This may increase the chance of injury over time. It is also important to note that we need enough thoracic mobility when we perform overhead presses at the gym. If we cannot keep our thoracic spine extended to neutral (straight spine; not hunched over), we would have to compensate by extending the lumbar spine (bending low back in backward direction). This could lead to increased pressure on the discs of the lumbar region, especially when we load the exercise with too much weight.
Breathing and rib expansion
We just discussed how each thoracic segment is a connection point for the ribs. This means that adequate thoracic mobility is essential for normal expansion of the ribcage while we breathe. When we take a large inhalation, the thoracic spine extends (segment rotates backwards). This allows the ribs to create more space for the lungs to expand. When we exhale, the thoracic spine flexes in order to return to its resting position (flexion would be rotating forward). If we cannot extend the thoracic spine adequately, it limits the amount of air that can fill the lungs. This is important for regulation of the parasympathetic nervous system as well as the cardiovascular system.
Relationship to legs and lumbar spine during squat
You need normal thoracic extension in order to properly perform loaded lower body movements such as the squat. If you are starting to pick up on the theme of interdependence, you are on the right track here. When you perform a squat with resistance from a barbell at the gym, you are resting the bar on your shoulders. When you do not have adequate thoracic mobility, your center of mass shifts forward. This alters the biomechanics of the entire exercise form the floor to the head and neck. This makes it harder to keep your heels down and keep your buttocks back, which ensures that the load is properly handled by the hips and spine. The lumbar spine would then have to compensate by overextending itself, forcing it to handle more of the load than it normally would have to.
Check out this video that shows 3 simple exercises you can perform to help improve thoracic mobility:
Click here for more information about physical therapy for mid back pain
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Main photo retrieved from https://www.t-nation.com/training/tip-improve-thoracic-spine-mobility
Photo of ribs and vital organs retrieved from https://www.britannica.com/science/thoracic-cavity
Photo of neck and low back pain retrieved from http://posturedirect.com/17-exercises-to-improve-your-thoracic-spine/
Photo of overhead mobility retrieved from https://fitnesspainfree.com/the-correct-way-to-mobilize-your-thoracic-spine-with-a-foam-roller/
Photo of squat and thoracic spine position retrieved from https://www.ensomovementculture.com/blog-1/movement-training-for-sports-people-mobility/18/4/2017
Photo of rib expansion during breathing retrieved from https://newgradphysicaltherapy.com/role-breathing-physical-therapy/
What Are Cervicogenic Headaches and How Can PT Help?
What are cervicogenic headaches?
A cervicogenic headache is caused by dysfunction in the neck, whether it be from stiff joints in the upper cervical spine or from tension in the muscles near the base of the skull. Pain from this type of headache is typically felt around the skull, temple regions, and eye sockets…
By Nicholas Mazzone, PT, DPT, CSCS
What are cervicogenic headaches?
A cervicogenic headache is caused by dysfunction in the neck, whether it be from stiff joints in the upper cervical spine or from tension in the muscles near the base of the skull. Pain from this type of headache is typically felt around the skull, temple regions, and eye sockets. The origin of this condition can be traumatic, as in a whiplash injury from a motor vehicle accident, or it could be due to prolonged abnormal load on the joints and muscles of the neck (getactivephysio.com.au).
What would be a non-traumatic cause of these types of headaches?
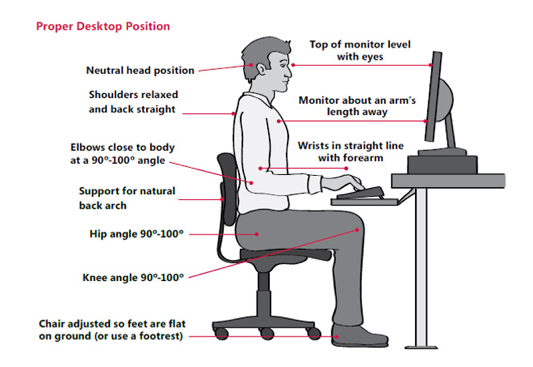
The most common non-traumatic cause of cervicogenic headaches is excessive, prolonged load on the joints and muscles of the neck. This is common in people who sit at a desk for most of their day at work. This occurs because the person winds up in a slumped posture in their spine, which eventually leads to what is known as “forward head posture”. This posture leads to increased tension in the muscles at the base of the skull as well as increased pressure on the first three segments of the cervical spine. Over time, this poor sitting posture can cause cervicogenic headaches. Adjusting one’s desk setup to ensure prevention of this situation can be as simple moving the keyboard closer to you. If the keyboard is placed too far away, you will have to slump forward to reach it, which will lead us to the forward head posture discussed above in order to ensure that you can see what is on your screen. Check out the picture below to get a better idea of what your desk setup should look like.
How can PT help?
Your physical therapist will create a program for you that includes manual therapy, therapeutic exercise, postural training, and stability training. Your program will also include education on how to adjust your desk setup or information on how to alter your current lifestyle in order to help your condition. Manual joint mobilization of the upper cervical spine, soft tissue mobilization of tense muscle tissue, and manual stretching of the region will help soothe the muscles and decrease pressure in the neck region. You will also be given specific exercises to target the muscles that are weak as well as the muscles that need to be lengthened. While heating modalities can feel good, they should not be the main intervention used in the treatment of cervicogenic headaches.
Check out this video that demonstrates 3 simple exercises that can help with your cervicogenic headaches:
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Cervicogenic Headaches. (2016, March 09). Retrieved from http://www.getactivephysio.com.au/cervicogenic-headaches/
Desk posture photo retrieved from https://sinicropispine.com/tips-improve-posture/
Main photo retrieved from http://yoffielife.com/sweat-dictionary/cervicogenic-headaches/
Manual therapy photo retrieved from https://learnmuscles.com/blog/2017/11/10/treat-spinal-joint-dysfunction-manual-therapy/
Whiplash photo retrieved from https://www.bouldercentre.com/news/whiplash-diagnosis-and-treatment
A cervicogenic headache is caused by dysfunction in the neck, whether it be from stiff joints in the upper cervical spine or from tension in the muscles near the base of the skull. Pain from this type of headache is typically felt around the skull, temple regions, and eye sockets. The origin of this condition can be traumatic, as in a whiplash injury from a motor vehicle accident, or it could be due to prolonged abnormal load on the joints and muscles of the neck (getactivephysio.com.au).
ACL Tears: Do They Always Require Surgery?
What is the ACL?
The anterior cruciate ligament (ACL) is a crucial stabilizing structure at the knee joint. When intact, it will prevent the lower leg (tibia) from moving forward on the thigh bone (femur). The ACL is commonly torn in athletes and may require surgical intervention in order to repair it. This structure does not heal on its own mainly due to its poor blood supply and twisted structure of collagen fibers. This twisted structure leads to frayed ends and therefore, cannot heal without assistance (surgery in this case)…
By Nick Mazzone PT, DPT, CSCS
What is the ACL?
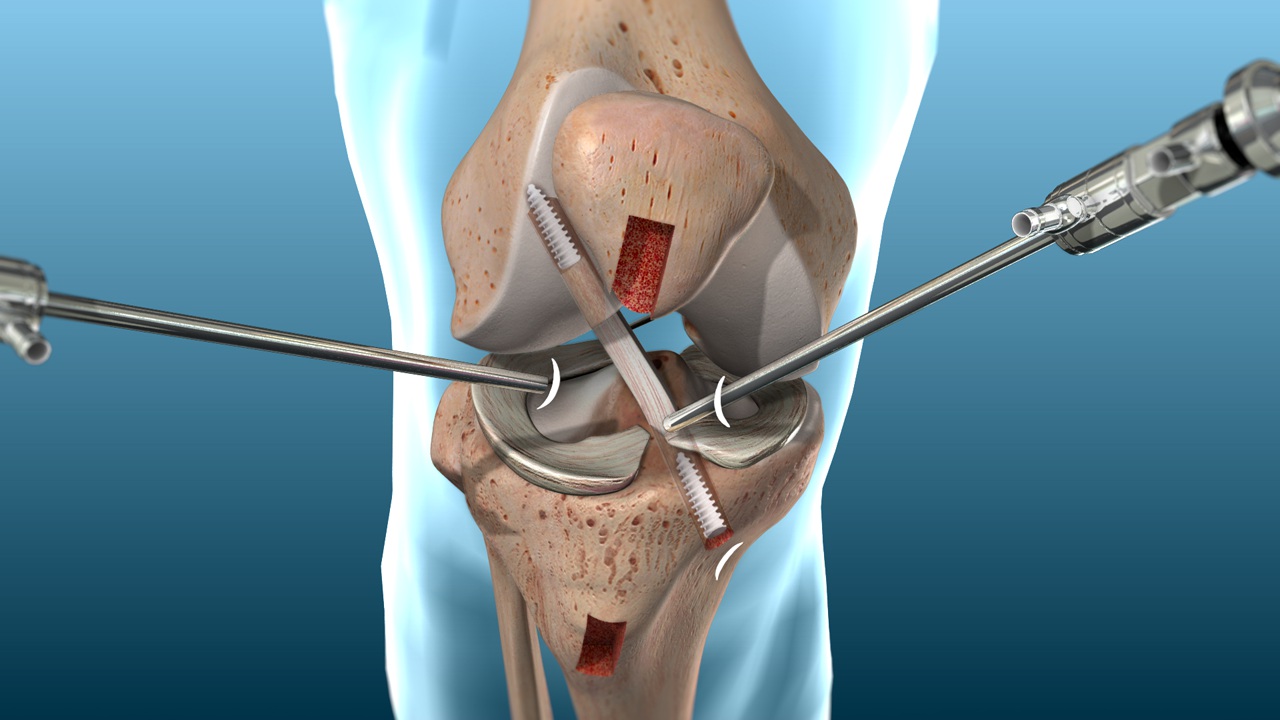
The anterior cruciate ligament (ACL) is a crucial stabilizing structure at the knee joint. When intact, it will prevent the lower leg (tibia) from moving forward on the thigh bone (femur). The ACL is commonly torn in athletes and may require surgical intervention in order to repair it. This structure does not heal on its own mainly due to its poor blood supply and twisted structure of collagen fibers. This twisted structure leads to frayed ends and therefore, cannot heal without assistance (surgery in this case).
How does someone typically tear their ACL?
ACL tears typically occur while the foot is planted and the femur twists over the tibia (or vice versa). Sometimes this happens because an athlete’s footwear gets caught on a grass surface, for instance. An ACL tear may also occur when an athlete lands on a straight knee on a hard surface such as a basketball court.
Can surgery be avoided?
Surgery is not necessary in all cases of an ACL tear. It would be highly suggested that an athlete who plans on returning to that same level of function receive surgical treatment to ensure that they return to their sport at the same level they were at before they got injured. For a person who tore their ACL but does not plan to partake in athletics or any activities that would require high level stability of the knee, a thorough and specific rehab program can help them return to their normal activities.
What might a non-surgical ACL rehab protocol consist of?
In the early stages, it is important to address the swelling and help strengthen the muscles around the knee in a gentle way in order to help normalize muscle activation patterns (acute swelling tends to turn these muscles off!). Once these issues have improved, we can move on to more functional exercises. A program aimed at rehabilitating someone after a torn ACL must address the limitation in the knee that is now missing one of its major stabilizing structures. While we no longer have the static stability that the ACL was providing to the knee, we can absolutely improve its dynamic stability by targeting the muscles around the knee joint. It is important to ensure that we are strengthening the hamstrings since they will act to prevent the forward movement of the tibia on the femur (which is one of the main functions of the ACL!). We must also ensure that we are challenging the stability of the knee in functional positions. This will teach the muscles around the knee joint to act together to keep the knee joint stable (co-contraction).
Check out this video that shows 3 simple exercises to help normalize the knee after a torn ACL that did not require surgery:
Click here for more information about physical therapy for ACL injuries or call 1-718-258-3300
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Main Photo retrieved from http://www.stack.com/a/a-new-type-of-acl-surgery-could-have-athletes-back-on-the-field-faster-than-ever
Photo of ACL tear retrieved from https://www.reddit.com/r/nba/comments/2ws4zu/science_and_the_nba_digging_in_to_the_anatomy_of/
Photo of twisting of knee retrieved from https://www.parisischool.com/acl-what-why-and-how/
Photo of ACL repair retrieved from https://www.mocnyc.com/acl-reconstruction/
Photo of squat on bosu ball retrieved from http://www.ctialatest.org/lab/lab-equipment-diagram
What is Achilles Tendinitis and How Can Physical Therapy Help It?
What is Achilles tendinitis?
The Achilles tendon is the thick band that connects the rear calf muscles to the heel. Achilles tendinitis is considered an overuse injury and may be caused by a sudden increase in physical activity and is commonly seen in the running population. Some risk factors for the development of this condition may be improperly fitting footwear, a stiff ankle and foot, weakness of the muscles that act on this region, and over-pronation of the foot during walking or running.
By Nick Mazzone PT, DPT, CSCS
What is Achilles tendinitis?
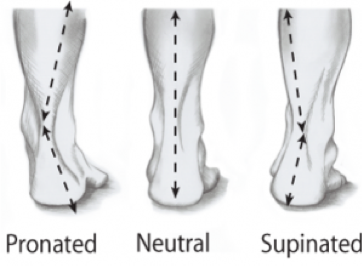
The Achilles tendon is the thick band that connects the rear calf muscles to the heel. Achilles tendinitis is considered an overuse injury and may be caused by a sudden increase in physical activity and is commonly seen in the running population. Some risk factors for the development of this condition may be improperly fitting footwear, a stiff ankle and foot, weakness of the muscles that act on this region, and over-pronation of the foot during walking or running. If left untreated, this condition can lead to degenerative changes in the makeup of the tendon itself, which will further exacerbate the symptoms. At this point, the condition would be considered a tendinosis.
What should be done in the early stages of this condition?
In the early stages of the condition it may be wise to combine active rest with techniques that help decrease swelling. This would mean refraining from running, long distance walking, or any other higher intensity activity that may have led to this issue in the first place. The active part of this equation would include gentle strengthening and range of motion exercises for the region to help improve blood flow for healing and address some of the issues that may have contributed to the condition in the first place. It is important to elevate the leg above chest level so that gravity can assist in decreasing swelling. If desired, ice can be used in combination with these methods as well.
What can PT do for me in later stages of this condition?
Once the acute stages of the condition have passed, it is important to restore normal function of the muscles in this region. Your physical therapist will prescribe a specific program based on your flexibility and strength assessments. Foot posture and stability will also be addressed after screening is completed. Stretching of the Achilles tendon is important; however, it is more important that we gradually reintroduce normal activities to the foot and ankle. Progressive loading of the Achilles tendon combined with eccentric exercise is the gold standard method for healing this condition.
What does progressive loading and eccentric exercise mean?
Progressive loading of the Achilles tendon simply means that we will be using specific exercises to gradually increase the amount of pressure that the Achilles tendon is under. For example, early exercises may include an activity performed with a resistance band while the foot is off the ground and later stage exercises may include activities on one leg.
Eccentric exercise simply means that we are strengthening the muscle’s ability to contract while it moves from a shortened position to a lengthened position. Most functional activities require eccentric strength. An example of an eccentric-focused exercise would be standing on your toes and then slowly lowering the heel to the ground. The eccentric portion of the exercise is the part where you focus on slowly lowering the heel to the ground (muscle is lengthening).
Check out this video that shows an example of a program that utilizes eccentric activity with progressive loading of the Achilles tendon:
For more information about foot physical therapy or ankle physical therapy, or call: 1-718-258-3300
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Main photo (green background) retrieved from http://www.achillestendonitis.co.uk/
Photo of anatomy of Achilles region retrieved from https://www.researchgate.net/figure/The-anatomy-of-the-Achilles-tendon-and-the-suralis-muscle_fig1_262230849
Photo of “RICE” retrieved from https://www.quora.com/How-do-I-heal-my-Achilles-tendon
Photo of foot posture retrieved from http://okanaganpeakperformance.com/knee-solution-seminar-recap
Photo of heel raise retrieved from https://fitness.stackexchange.com/questions/14976/is-this-a-good-at-home-exercise-routine-for-a-beginner
How Can Physical Therapy Help My Sciatica?
What is Sciatica?
Sciatica is one of the most common symptoms associated with lower back pain. It refers to the sensation of burning pain that tends to radiate from the buttock down the leg. The distance the pain travels is typically correlated to the extent of the irritation effecting the nerves. The name “sciatica” comes from the sciatic nerve, which is one of the largest nerves in the body…
By Nick Mazzone, PT, DPT, CSCS
What is Sciatica?
Sciatica is one of the most common symptoms associated with lower back pain. It refers to the sensation of burning pain that tends to radiate from the buttock down the leg. The distance the pain travels is typically correlated to the extent of the irritation effecting the nerves. The name “sciatica” comes from the sciatic nerve, which is one of the largest nerves in the body. The spinal nerves that become irritated are typically those that eventually come together to form the sciatic nerve (from spinal level L4 to S3). Sciatica is not a permanent condition and does not typically require surgical intervention.
What causes sciatica?
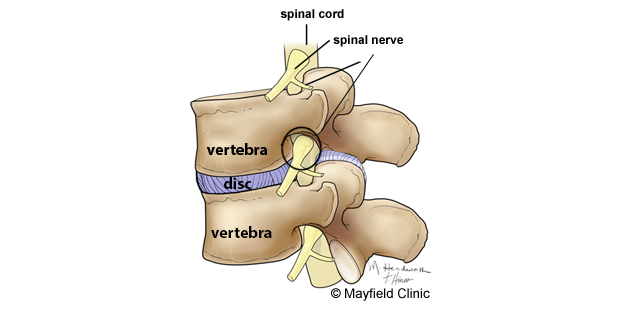
These symptoms are typically caused by excess pressure on a nerve after it exits the lumbar spine (lower spine). This pressure can come from a herniated disc, arthritis in the lumbar region, and other conditions in which the space that the spinal nerve travels becomes compressed or shrinks.
How can physical therapy help improve this condition?
This condition is relieved by decompressing the region in which these spinal nerves travel. This can be achieved through a specific mobility and strengthening program that includes postural education and awareness training. These specific exercises will depend on the location at which the nerve is being irritated. Generally speaking, in order to decrease pressure in the lumbar region of the spine, you must be mobile in not only the lumbar spine but the thoracic region (mid back) and hips. This will help take pressure off the low back by allowing a more even distribution of movement. Think about it this way: If you are lacking proper mobility in your thoracic spine, your lumbar spine will have to make up for this lack of mobility. This can lead to increased stress and strain in this area. The same idea works for the hips.
Postural training is important in helping to decrease pain and inflammation in the low back. The pelvis and lower spine are anatomically connected (the lower spine actually sits in the pelvis), and therefore movement between the two will be interrelated. The position of the pelvis will dictate the posture in our lumbar spine during all activities (including at rest!). Depending on where the nerve irritation is occurring, this positioning of the pelvis will either increase or decrease pressure on the nerve. If the irritation is occurring at the point where the nerve exits the spinal canal (at the nerve root), extension of the lumbar spine should help alleviate the pressure by “opening” the region where the spinal nerves exit, while flexion of the lumbar spine may increase pressure due to “closing” of the region. Refer to the picture above for a visual of this phenomenon. “Lordosis” is known as lumbar spine extension, while “flat” spine refers to a flexed spine. The picture below demonstrates these movements.
Click here to find out more information about physical therapy for sciatica or call 1-718-258-3300
Check out this video that demonstrates a simple mobility exercise for the sciatic nerve to help alleviate your symptoms of sciatica:
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Main photo of sciatica pain in leg retrieved from https://www.magnilife.com/blog/5-effective-ways-for-dealing-with-sciatica-pain/
Photo of irritated nerve retrieved from http://arizonapaintreatmentcenters.com/from-dr-craig-peterson-mva-sciatica
Photo of lumbar flexion and extension retrieved from https://b-reddy.org/making-pull-ups-and-burpees-more-shoulder-and-lower-back-friendly/
Photo of pelvis position and lumbar spine retrieved from https://body-motion.co.uk/injuries/postural-pain/improve-your-sitting-posture/
What is Tennis Elbow and How Can Physical Therapy Help?
What does tennis elbow mean?
“Tennis elbow” is the nickname given to a condition known to the medical community as lateral epicondylitis (also seen ending in -osis or -algia). This name describes the region from which the pain originates on the outside of the elbow…
By Nick Mazzone, PT, DPT, CSCS
What does tennis elbow mean?
“Tennis elbow” is the nickname given to a condition known to the medical community as lateral epicondylitis (also seen ending in -osis or -algia). This name describes the region from which the pain originates on the outside of the elbow. The lateral epicondyle is the part of the upper arm bone that serves as the origin for all of the muscles that extend the wrist.
What causes tennis elbow?
Tennis elbow is considered an overuse injury. It typically occurs after repetitive stress to the involved region over time, however one traumatic incident such as a fall or work accident may also cause inflammation in this region. Tennis elbow got its name because it is a common overuse injury seen in those who play the sport. Tennis players tend to hold a tight grip on their racquets while producing powerful forces with their wrist extensor muscles. In certain cases, this may be a recipe for inflammation. Another common population that tends to get tennis elbow is the office worker. Being in a position of wrist extension while typing for prolonged periods may cause repetitive stress to the outside of the elbow.
Here is an example of what your posture should look like while in front of your computer:
How Will Physical Therapy help me?
Your physical therapist will design a specific treatment plan tailored to your needs based on your background and activity level. The program will consist of soft tissue mobilization to assist in the healing process, stretching/mobility training, functional strengthening of eccentrics (the muscle’s ability to control movement from wrist extension to wrist flexion) and grip strengthening, training of ergonomics and posture, and education on how to prevent the condition from reoccurring.
Your specific program will depend on how you acquired the condition in the first place. An office worker will be trained to alter their desk setup in order to decrease the stress on the wrist extensors. A tennis player may be prompted to consider changing the thickness of their racquet handle or the tightness of the strings. Both of these variables may help contribute to the repetitive stress that occurs during the sport since more force production is necessary to produce the desired effect when these conditions are not optimal.
This picture shows one way to stretch the wrist extensor muscles.
Click here to find out more information about physical therapy for tennis elbow
Check out this video for 3 simple exercises to help with your tennis elbow:
About-
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn, NY. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources
Main photo retrieved from https://www.mayoclinic.org/diseases-conditions/tennis-elbow/symptoms-causes/syc-20351987
Photo of bones of arm retrieved from http://cruxcrush.com/2014/06/26/climber-problems-elbow-injury/
Picture of wrist and finger extension retrieved from http://www.militarydisabilitymadeeasy.com/images/handmuscles/
Picture of ideal desk posture retrieved from xhttps://www.microsoft.com/accessories/en-us/support/ergonomic-comfort
Photo of wrist extensor stretch retrieved from https://www.therapeuticassociates.com/athletic-performance/golf/stretching-for-golfers/
What is Assisted Stretching and How can it help me?
What is Assisted Stretching?
Assisted Stretching is a hands-on method of stretching in which a person is gently supported through a series of stretches by a trained practitioner. Assisted Stretching is more effective than stretching by yourself because the practitioner stabilizes your joints in positions that allow you both to isolate and stretch one muscle at a time while expanding your fullest range of motion.
Nick Macaluso
Stretching is kind of like flossing... everyone knows they should be doing it, but who really does it? It’s one of those things that we’re all going to start making into a habit tomorrow, but somehow tomorrow never comes. To our credit though, when we get that cramp in our thigh, or piece of spinach in between our teeth, we know exactly what we need to do. But how do we identify the exact muscles that tend to cramp or spasm, and prevent it from happening? How can we isolate and stretch the muscles we hold the most tension in to prevent and alleviate pain? How can we most effectively just enhance our mobility for a higher quality of life? The answer, Assisted Stretching.
What is Assisted Stretching?
Assisted Stretching is a hands-on method of stretching in which a person is gently supported through a series of stretches by a trained practitioner. Assisted Stretching is more effective than stretching by yourself because the practitioner stabilizes your joints in positions that allow you both to isolate and stretch one muscle at a time while expanding your fullest range of motion. The benefit to being able to isolate and stretch individual muscles is to give both you and the practitioner a better understanding of where exactly your body may be out of alignment. Perhaps your low-back pain is just a result of tight hamstrings, or your sciatica is just a result of tight glutes. Both of which can be relieved from general stretching, but without the assistance of a trained practitioner, it is nearly impossible to isolate the exact muscle and relieve its tension.
Why is Assisted Stretching so productive?
Aside from being able to realign your body by isolating the muscles being stretched, Assisted Stretching is an opportunity for you to relax and repair your body and mind while still using your time constructively. Many of us after long days or weeks want nothing more than a massage to take the tension out of our backs, necks, shoulders, or hips, but aside from the relaxation, what is the massage doing to prevent that tension from returning? Most of the time, tension builds in areas of our bodies that are either overactive or misaligned due to habitual poor posture. While massages are great, if you’d rather spend your time relaxing AND simultaneously preventing the tension from returning, Assisted Stretching is for you.
Stretching is one of those things that people spend their lifetime studying and writing about because of its incredible complexity and near infinite amount of benefits. But instead of wasting your time with all that, experience the hype for yourself by scheduling a 20 minute Assisted Stretching session with Nick Macaluso at Evolve Physical Therapy. Sessions run in 20 minute increments and can last anywhere from 20 minutes to 2 hours depending on how long you would like to be stretched. While this service is open to the public, all active patients of Evolve must first speak to their therapist to ensure an Assisted Stretch is right for them.
For more information or any questions, give us a call at 718-258-3300 or contact us today!
How Can Physical Therapy Help My Plantar Fasciitis?
What is the plantar fascia?
The plantar fascia is a thick band of connective tissue that runs from the lower surface of the heel to the beginning of the toes. This fibrous band of tissue is placed under tension during walking and other activities in which you place weight onto the feet. This tension creates support and stabilization of the arch of foot, which will help stabilize the entire lower extremity during these types of activities…
By Nick Mazzone, PT, DPT, CSCS
What is the plantar fascia?
The plantar fascia is a thick band of connective tissue that runs from the lower surface of the heel to the beginning of the toes. This fibrous band of tissue is placed under tension during walking and other activities in which you place weight onto the feet. This tension creates support and stabilization of the arch of foot, which will help stabilize the entire lower extremity during these types of activities.
What causes this structure to become inflamed?
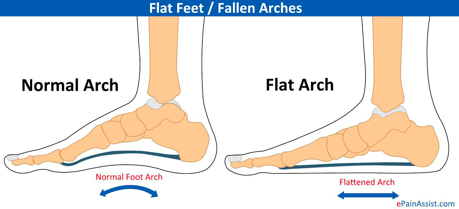
While the exact mechanisms behind the causes of plantar fasciitis are not completely understood, the condition has been correlated with some mechanical issues at the foot and ankle. One of the more common impairments associated with this condition is inadequate dorsiflexion of the foot. Dorsiflexion is the movement performed when the top surface of the foot comes closer to the front of the leg.
Another impairment that is commonly associated with plantar fasciitis is weakness of the posterior tibialis muscle. This muscle helps to increase arch height during activities in which weight is placed on the feet.
This condition can also be considered an overuse injury. For instance, a running athlete may progress their running program too quickly without allowing their body to adapt. This can cause inflammation and pain in the plantar fascia.
What can PT do to help?
Your physical therapist will create a specific foot physical therapy treatment plan tailored to your needs and impairments. Most commonly, the treatment will consist of mobility drills and functional stabilization techniques to help support the arch of the foot. These exercises are more effective when performed with weight on the legs in a standing position, as this is more closely related to the way in which these structures actually function in the real world. Your program may start more conservatively depending on your pain and activity tolerance.
The ultimate goal of the treatment is to progressively load these structures so that they become adapted to increased stress. This will ensure that the plantar fascia can handle the demands placed on it during our daily endeavors, whatever they may be. In some cases, a physical therapist will recommend orthotics to help provide support to the arch of the foot.
Click here for more information about physical therapy for plantar fasciitis
Check out this video depicting 3 simple exercises that can be performed to help improve your plantar fasciitis:
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources:
Picture of painful foot retrieved from https://www.tcpaindoctor.com/can-prp-help-treat-plantar-fasciitis/
Picture of plantar fascia function during weight bearing retrieved from https://painphysiotherapist.com/2016/05/25/plantar-fascia-rupture/
Picture depicting dorsiflexion of ankle retrieved from http://www.militarydisabilitymadeeasy.com/
Picture of posterior tibialis retrieved from https://www.fixpodiatry.com.au/podiatry-conditions/tibialis-posterior-tendinopathy/
Picture of collapsed arch retrieved from https://www.epainassist.com/sports-injuries/foot-and-heel-injuries/flat-feet-or-pes-planus-or-fallen-arches
Photo of orthotic placement retrieved from https://bestwalkingfeet.com/good-shoes-for-flat-feet/insoles-and-inserts/
Wheeless' Textbook of Orthopaedics. (n.d.). Retrieved from http://www.wheelessonline.com/ortho/Plantar_fascia
What is the Rotator Cuff and What Does It Do?
What is the rotator cuff?
The rotator cuff is the name given to the group of 4 muscles that originate from different positions on the shoulder blade and connect to the humerus (upper arm). These muscles all work together to ensure stability of the shoulder joint during movement (dynamic stability). When isolated, each of these muscles acts on the humerus and moves the shoulder joint in different directions…
By Nick Mazzone, PT, DPT, CSCS
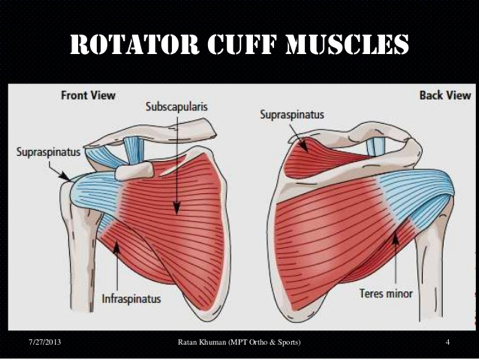
What is the rotator cuff?
The rotator cuff is the name given to the group of 4 muscles that originate from different positions on the shoulder blade and connect to the humerus (upper arm). These muscles all work together to ensure stability of the shoulder joint during movement (dynamic stability). When isolated, each of these muscles acts on the humerus and moves the shoulder joint in different directions. These muscles are named supraspinatus, infraspinatus, teres minor, and subscapularis.
Why do we need this dynamic stability?
As we move the arm, these rotator cuff muscles will contract together to help keep the humerus centered nicely inside the cup of the shoulder joint (think ball and socket). If there is an asymmetry in strength among these muscles, the positioning of the shoulder inside the socket may be altered while you move your arm. Over time, this can cause irritation of other tendons, ligaments, and bone in the shoulder region. Some of the common diagnoses associated with rotator cuff muscle weakness are shoulder impingement syndrome and non-traumatic rotator cuff tears.
What happens if the rotator cuff is torn?
The most commonly torn rotator cuff muscle is the supraspinatus. People with supraspinatus tears typically have trouble elevating the arm and may exhibit a compensatory shrugging of the shoulder in order to assist in raising the arm.
If a partial tear is present, the muscle and tendon have the ability to heal without surgical intervention. In order for proper healing to occur, we must provide an ideal environment for the muscle and tendon to recover. This would include intervention aimed at decompressing the region where the muscle attaches to the humerus, which would be achieved through range of motion exercise and strengthening of all 4 rotator cuff muscles to help produce more efficient movement of the shoulder (to put it briefly).
If a complete tear is present, there are two options that one may follow. The non-surgical route would include strengthening other muscles around the shoulder joint that will help to compensate and act as a substitute for the torn rotator cuff muscle. Fortunately, the shoulder joint was designed to be able to withstand this type of injury and with the right rehab protocol, may return to normal functioning. In cases where this method does not help, surgical intervention is typically indicated. After surgery, patients will be sent to a physical therapist in order to help them return to their prior level of functioning.
What does physical therapy typically consist of for rotator cuff injuries?
The plan of care will consist of manual stretching and soft tissue mobilization of tense muscles, specific strength and stability exercise to improve the function of the shoulder, range of motion exercises to help normalize joint movement, and movement re-education to ensure pain-free use of the arm.
Click here to find out more information about physical therapy for rotator cuff injuries
Check out this brief video for 3 exercises that will strengthen the rotator cuff muscles:
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
Resources
Photo depicting widespread shoulder pain (top photo) retrieved from https://www.myanthemhealth.com/blog/shoulder-paincould-it-be-my-rotator-cuff
Photo depicting different muscles of the rotator cuff retrieved from https://www.slideshare.net/prkhuman/shoulder-impingement-syndrome-24685952
Photo depicting a rotator cuff tear retrieved from https://www.vivehealth.com/blogs/resources/rotator-cuff-tear
Photo depicting the compensatory shoulder shrug during shoulder elevation retrieved from https://healtheappointments.com/chapter-16-the-musculoskeletal-system-essays/5/
How Can PT Help My Carpal Tunnel Syndrome?
What is carpal tunnel syndrome?
The carpal tunnel is the space formed by the bones of the wrist and hand that allows passage of the median nerve along with tendons of muscles that move the joints of the hand. This space is typically about an inch wide, however it can be made narrower in the presence of irritation and swelling of any of these structures.
By Nick Mazzone PT, DPT, CSCS
What is carpal tunnel syndrome?
The carpal tunnel is the space formed by the bones of the wrist and hand that allows passage of the median nerve along with tendons of muscles that move the joints of the hand. This space is typically about an inch wide, however it can be made narrower in the presence of irritation and swelling of any of these structures. Narrowing of this passageway can lead to pressure on the median nerve, which may lead to symptoms such as tingling, burning, weakness, and pain in the hand and fingers.
How do I know it is carpal tunnel syndrome?
Symptoms from carpal tunnel syndrome such as numbness and tingling typically present themselves at the thumb, index finger, middle finger, and half of the ring finger. This is because sensation to these areas is supplied by the median nerve. If the median nerve is being compressed, these areas may become numb or painful. You may also find weakness of the muscles that move the thumb, first two fingers, and wrist. The picture below shows what the hand may look like when a person with long-standing carpal tunnel syndrome attempts to make a fist. It is known as the “Hand of Benediction Sign”.
What is the traditional treatment for carpal tunnel?
Typically, people suffering with the symptoms of carpal tunnel syndrome receive anti-inflammatory medications or are suggested to have surgery. This surgery involves a “release” of the transverse carpal ligament, meaning that the surgeon cuts this ligament to help decrease pressure on the tunnel and, therefore, the median nerve. The issue is that this does not always solve the problem. If the tendons are still inflamed and swollen, we may still be feeling these symptoms after the post-surgical healing process is complete. For this reason, physical therapy should be a patient’s first option. Many people find that PT alone helps them return to normal, pain-free functioning during daily tasks.
How do we improve these symptoms in PT?
The symptoms from carpal tunnel syndrome can be resolved by decreasing pressure on the median nerve at the level of the wrist and hand. This can be accomplished by improving flexibility of the muscles and connective tissues at the wrist and hand, especially those on the front of the forearm. Your physical therapist will perform mobilization and stretching techniques, postural training and education, nerve gliding techniques, and soft tissue mobilization. Once the tissues are of proper flexibility, we must ensure that the muscles surrounding the hand and wrist are strong to help stabilize the joints. A home exercise program with specific exercises to help your condition will also be prescribed.
Check out the video below for a demonstration on how to perform median nerve gliding to help alleviate symptoms of carpal tunnel syndrome:
Click here to find out more information about physical therapy for carpal tunnel syndrome
Resources:
Our knowledge of orthopedics. Your best health. (n.d.). Retrieved April 05, 2018, from https://orthoinfo.aaos.org/en/diseases--conditions/carpal-tunnel-syndrome/
“Hand of Benediction” photo retrieved from http://slideplayer.com/slide/9418409/
Photo depicting carpal tunnel release surgery retrieved from http://www.korshjafarniamd.com/treatment/minimally-invasive/endoscopic-carpal-tunnel-release.php
Photo depicting median nerve compression retrieved from http://nursinglink.monster.com/training/articles/814-carpal-tunnel-syndrome
Photo used at top of page depicting painful wrist retrieved from http://www.pipmchealth.com/conditions/carpal-tunnel-syndrome/
“Tips for preventing and treating carpal tunnel syndrome”photo retrieved from https://www.mispinerelief.com/blog/carpal-tunnel-treatment-and-preventing-for-carpal-tunnel-syndrome/
Nick Mazzone received his Doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn. To view some of his other content, visit drnickmazzonedpt.wordpress.com.
How Can PT Help My Spinal Stenosis?
What is Spinal Stenosis?
Spinal stenosis is one of the most commonly diagnosed conditions that affects the lumbar spine (lower back). It is common for people with stenosis to feel tightness and pain that radiates from the low back and buttocks down into both legs.
It is estimated that only about 5% of people with spinal disorders actually require surgery (Eidelson, 2018). So, what are the other 95% of people expected to do? This is where physical therapy comes into play. There are many methods your PT will use in order to help address the issue causing your pain and discomfort.
By Nick Mazzone, PT, DPT, CSCS
Spinal stenosis is one of the most commonly diagnosed conditions that affects the lumbar spine (lower back). It is common for people with stenosis to feel tightness and pain that radiates from the low back and buttocks down into both legs.
It is estimated that only about 5% of people with spinal disorders actually require surgery (Eidelson, 2018). So, what are the other 95% of people expected to do? This is where physical therapy comes into play. There are many methods your PT will use in order to help address the issue causing your pain and discomfort. This includes but is not limited to therapeutic exercise, soft tissue mobilization, manual stretching of the hips and spine, and postural re-education.
What is spinal stenosis of the lumbar region?
As you can see from the picture above, stenosis of the spine involves a narrowing of the canal in which the spinal cord sits. This leads to increased pressure on the spinal cord as well as the nerves that branch from it. This is the reason why people feel pain in the buttocks and legs; the region of pain stems from a specific section of the spinal cord that is under pressure. For this reason, two people with the same condition will present with different symptoms.
How can physical therapy help with this problem?
The treatment plan will be specifically tailored to each patient with stenosis. The main objective is to help decompress the spinal cord and its nerve branches by using techniques that create more space in the spinal canal. Bending backward, also known as extension of the lumbar spine, will decrease the space in the spinal canal due to the way the joints of the spine are oriented. This may increase pain and symptoms in a person with spinal stenosis. For this reason, the treatment plan will be focused on utilizing and improving spinal flexion, more commonly known as bending forward. This will help to widen the canal and decompress the inflamed structures, effectively providing relief of symptoms.
A comprehensive treatment plan will help you find positions of maximal comfort and give you more drug-free and surgery-free options for taking care of your lumbar spine and preventing pain in the future.
Please check out this brief video that provides 3 simple exercises to help decrease symptoms due to lumbar spinal stenosis, or click here to find out more information about physical therapy for spinal stenosis.
Resources
Eidelson, S. G., & An, H. S. (February 2018). Spinal Stenosis Center | Lumbar, Cervical, Symptoms, Exercise, Surgery. Retrieved March 18, 2018, from https://www.spineuniverse.com/conditions/spinal-stenosis
Picture of person with low back pain retrieved from http://www.omegapainclinic.com/spinal-stenosis-pain-treatment-utah
Pictures of stenosis in lumbar region retrieved from https://www.spineuniverse.com/conditions/spinal-stenosis
Nick Mazzone received his doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn.
What Does Foam Rolling Do for Me?
Foam Rolling has become one of the more popular health and fitness topics over the past few years or so. These tools can be found in many different shapes, sizes, and colors with varying textures and firmness to fit everybody’s apparent need. If you google this, you will find claims that foam rolling can help you improve range of motion, muscle strength and performance, and decrease pain…
By Nick Mazzone, PT, DPT, CSCS
Foam Rolling has become one of the more popular health and fitness topics over the past few years or so. These tools can be found in many different shapes, sizes, and colors with varying textures and firmness to fit everybody’s apparent need. If you google this, you will find claims that foam rolling can help you improve range of motion, muscle strength and performance, and decrease pain. It is also often used as part of a warm-up and cool-down within an exercise program.
Who do I believe?
Well, unfortunately there are very few studies on foam rolling and its effects on our muscles and connective tissues. The following bullet points can be used as a summary of the current body of research on this topic:
Positive Effects of Using a Foam Roller
· Increased blood flow
· Increased tissue temperature
· Better short-term improvements in range of motion versus static or dynamic stretching
· Decreased sensation of pain
What Foam Rolling Will NOT do for You
· Increase strength or power output
· Give lasting improvements in range of motion when used as a stand-alone treatment
· Lead to complete resolution of pain/symptoms when used as a stand-alone treatment
Let’s Discuss these findings…
As you can see, there are some benefits to using a foam roller, however I feel it is important that we clear up some of the common misconceptions on the topic…
Many people who use a foam roller use it in isolation as a method of improving their mobility. I understand why people want this to be true; foam rolling is much easier and less strenuous than stretching. Unfortunately, you will not receive lasting effects from foam rolling alone. While foam rolling will only provide temporary improvements in range of motion, we can take advantage of this temporary improvement by proceeding to perform static or dynamic stretching. With consistency, this can help to improve range of motion on a more permanent basis (although more studies are needed on this topic).
There is also no evidence that foam rolling increases strength or explosiveness during your workout, however one may argue that by utilizing a foam roller you are increasing blood flow to the area, and therefore, helping to facilitate contraction of specific muscles during exercise.
Foam Rolling may also help decrease pain by working to desensitize the area through repetitive stimulation and can help promote tissue healing by improving local blood flow.
How do you suggest I use the foam roller in my daily life?
· In conjunction with a stretching program for improving range of motion
· As part of a warmup routine, especially for activities that have high mobility requirements
· As an alternative to pain killers for temporary pain relief
· As a method of soothing sore, painful muscles after a physically demanding workout
Check out this video for a brief introduction on how to use a foam roller:
For more information or any questions, give us a call at 718-258-3300 or contact us today!
Resources:
Su, H., Chang, N., Wu, W., Guo, L., & Chu, I. (2017). Acute Effects of Foam Rolling, Static Stretching, and Dynamic Stretching During Warm-ups on Muscular Flexibility and Strength in Young Adults. Journal of Sport Rehabilitation,26(6), 469-477. doi:10.1123/jsr.2016-0102
Cartoon depicting man foam rolling retrieved from https://www.gq.com/story/foam-roller-tips
Nick Mazzone received his doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn.
How Do I Warmup Prior to Lifting Weights?
The warmup phase is easily one of the most forgotten components of an exercise program these days. Would you intentionally leave it out if I told you that it could lead to increased performance and results during your workout?
By Nick Mazzone, PT, DPT, CSCS
The warmup phase is easily one of the most forgotten components of an exercise program these days. Would you intentionally leave it out if I told you that it could lead to increased performance and results during your workout?
Traditionally, people have used static stretching (long holds in a position that lengthens a muscle) before workouts to help decrease their risk of injury, however there is no evidence that this is the case. Static stretching before exercise has actually been shown to decrease maximal force production, jump height, and sprint speed while increasing reaction time and impairing balance (Perrier et. al).
Rather than static, long holds in the lengthened position of a muscle, dynamic movement involves actively moving through a joint’s range of motion without holding at the end point. A study by Perrier et. al found that dynamic movement including skipping, shuffling, and calisthenics of increasing intensity that were chosen based on the movements that would be performed during training led to improved athletic performance versus static stretching and no stretching at all.
Dynamic movements that mimic the exercises you will be performing help to prepare the central nervous system for physical activity. By activating specific muscles prior to exercising, we are facilitating proper muscle activation patterns and therefore, “priming” the nervous system.
Suggestions for a proper warmup routine
· 15-20 minutes of dynamic movement
· Must make an effort to mimic the activities that will be performed in the exercise program
· Must include enough intensity to elevate heart rate
· Should not approach more than 30% of your maximal effort to prevent muscle fatigue
Example of warmup routine prior to squatting or deadlifting
· Bridging with a resistance band 3 sets of 15-20 reps
· Marching with a resistance band 3 sets of 15-20 reps
· Body weight squatting with a resistance band 3 sets of 15-20 reps
· Lateral Band Stepping with resistance band 3 sets of 10 steps in each direction
Example of warmup routine prior to overhead pressing or bench pressing
· Banded shoulder external rotation with retraction 3 sets of 12-15 reps
· Wall Angels 3 sets of 10-15 reps
· Overhead Arm Raise at Wall 3 sets of 10-15 reps
· Banded Wall Climbs 3 sets of 8-12 reps
For a preview of upper and lower body warmup routines, check out these videos:
For more information or any questions, give us a call at 718-258-3300 or contact us today!
Click here for more information about sports physical therapy and how a personalized physical therapy program may just be your best bet…
Resources
Perrier, E. T., Pavol, M. J., & Hoffman, M. A. (2011). The Acute Effects of a Warm-Up Including Static or Dynamic Stretching on Countermovement Jump Height, Reaction Time, and Flexibility. Journal of Strength and Conditioning Research,25(7), 1925-1931. doi:10.1519/jsc.0b013e3181e73959
Warmup picture retrieved from https://www.hosmerchiropractic.com/blog/7-ultimate-dynamic-stretching-exercises/
Nick Mazzone received his doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn.
How Can Physical Therapy Help My Arthritis?
What is Osteoarthritis?
Osteoarthritis is a major cause of chronic pain and disability in our society today. People with arthritis typically report deep, aching pain in the joints affected as well as stiffness and inability to get up and get right out of bed in the morning. The most common treatments for this painful condition include cortisone injections aimed at decreasing inflammation, over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs), and knee replacement surgery once the condition significantly worsens…
By Nick Mazzone, PT, DPT, CSCS
What is Osteoarthritis?
Osteoarthritis is a major cause of chronic pain and disability in our society today. People with arthritis typically report deep, aching pain in the joints affected as well as stiffness and inability to get up and get right out of bed in the morning. The most common treatments for this painful condition include cortisone injections aimed at decreasing inflammation, over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs), and knee replacement surgery once the condition significantly worsens.
What is going on in my joints that causes this pain?
Osteoarthritis is a degenerative condition that leads to wearing away of the outer layers of cartilage and bone as you can see in the image above. This causes an inflammatory process to be induced by the body which leads to swelling, increased sensitivity to touch and pressure, and pain. On an X-ray, you will see decreased space between the bones and potentially bone spurs, which the body lays down in response to excess pressure in the area. This inflammatory condition typically leads to inactivity, which then leads to decreased range of motion along with muscle weakness.
What will physical therapy accomplish?
The hallmarks of arthritis include joint stiffness, swelling, muscular weakness, and pain. In physical therapy, your therapist will prescribe specific exercises that will help improve range of motion, and therefore, stiffness, as well as exercises for strengthening the surrounding muscle groups. These exercises will also act to help decrease the central nervous system’s hypersensitivity to pressure and touch, which will allow you to perform your daily tasks with much greater ease. Your therapist will also work on improving your patterns of movement in order to ensure that you are decreasing the pressure on your arthritic joints and using the most efficient pattern available to your body. There are also modalities and other methods used that will help to decrease the amount of swelling in the joint, which then leads to decreased pain.
Great. Stronger muscles, improved range of motion. How exactly is this helping my condition?
Good question. I would like to start by saying that there is currently no way to reverse the arthritic condition. That being said, I would like you to consider this example. Think about a stiff and swollen knee joint. When a person bends their knee, the stiffness in the muscles and fibers of the joint force the bones to glide along a smaller surface area. This will eventually lead to more breakdown of the cartilage and outer layers of bone, which means progression of the osteoarthritis. Now imagine we have a knee joint that has been sufficiently stretched and has less swelling. These bones glide in a smoother manner across a larger surface area (due to less range of motion restrictions). Now that the force can be spread evenly across the bony surfaces, there is a much less chance of increasing breakdown of the cartilage and bone.
Strengthening the muscles helps to ensure that while walking or performing other functional daily tasks, the joint is kept in a position that ensures proper alignment and efficiency of muscle function. This formula along with a prescribed home exercise program will prevent progression of the condition and assist in avoiding knee replacement surgery.
Check out this brief video which shows how to utilize a “hip-first pattern” to help offset pressure on the knee joint when bending down and squatting.
For more information or any questions, give us a call at 718-258-3300 or contact us today!
or click here to find out more about physical therapy for arthritis
Nick Mazzone received his doctorate in Physical Therapy from Stony Brook University. He has a strong background in strength and conditioning and aims to bridge the gap between strength training and physical therapy. Nick believes that a lifestyle centered around physical fitness and mental well-being are vital to one’s successes and happiness. For this reason, he educates his patients on pain science and helps empower them and motivate them to reach their goals every day. You can find him at Evolve Physical Therapy in Mill Basin, Brooklyn.
Anterior Hip Pain and How to Manage It
What is Anterior Hip Pain and what are it's causes?
Anterior hip pain is most often caused by a strain in the hip flexor muscles which are located at the front of the hip. A strain, which is a injury to a muscle or tendon, causes a painful sensation to the hip which heavily contributes while walking, running or squatting. These strains are common with overtraining, strength imbalances, poor technique, inflexibility and forceful contractions such as kicking and sprinting.
How does the hip work?
The hip is a ball-and-socket joint that comprises the top of the thigh. The femur, which is your thigh bone, sits into the acetabulum, which is the socket that allows it to remain both stable and mobile, and to allow for movement without dislocation.
What is Anterior Hip Pain and what are it's causes?
Anterior hip pain is most often caused by a strain in the hip flexor muscles which are located at the front of the hip. A strain, which is a injury to a muscle or tendon, causes a painful sensation to the hip which heavily contributes while walking, running or squatting. These strains are common with overtraining, strength imbalances, poor technique, inflexibility and forceful contractions such as kicking and sprinting. The most common and impactful of these is overtraining which includes insufficient rest and difficult training sessions. Consistent overtraining sessions will result in micro trauma which accumulate and result in a possible hip flexor strain or tendonitis.
Myofascial Release of the Anterior Hip
In this video, Chris Desiderio, DPT will explain how to release some tension that may be in the front of the hip in order to help the hip flexors function optimally.
Posterior Mobilization
In this video, Chris will demonstrate a mobilization of the hip in a posterior direction to help release the front of the joint capsule.
Standing External Rotations
In this video, Chris will demonstrate a standing external rotation, which can help strengthen the gluteus medius to prevent anterior hip pain.
Click here to find out more information about hip physical therapy in Brooklyn or give Evolve Physical Therapy in Brooklyn a call today! 1-718-258-3300
Physical Therapy and Your Insurance
Is Physical Therapy Covered by Health Insurance?
Though your insurance company may allow many physical therapy visits per year, they usually also reserve the right to do a pre-check to ensure that the treatment you’ll be receiving will be medically necessary or able to make a positive change.
Authorization
Though your insurance company may allow many physical therapy visits per year, they usually also reserve the right to do a pre-check to ensure that the treatment you’ll be receiving will be medically necessary or able to make a positive change.
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment is medically necessary. Sometimes called prior authorization, prior approval or pre-certification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization isn’t a promise your health insurance or plan will cover the cost.
In and Out of Network
Some insurance companies have in-network providers, which means that they have pre-negotiated rates with those doctors or physical therapists, but insurance companies may also restrict the patient to the in-network providers. Some insurance providers that have in-network providers will also have out-of-network providers, although they may cover less of the expense of the treatment and have the patient pay the remainder of the bill.
Knowing your rights when it comes to your insurance
First, you should know that your insurance company is there to help you, you are not subject to their demands
You have a right to go out of network if your provider doesn’t have any in-network providers
If you are denied for authorization, you have your right to have your voice heard and to request more visits. If you are entitled to more visits than you were authorized for, you can speak to your insurance along with you physical therapists and doctor to be granted more visits
You are never locked into a healthcare provider, whether it is a doctor or a physical therapist. If you are unhappy with the care you are receiving, you are entitled to finding a care provider that you feel is good for you
For some more detailed info concerning healthcare laws in New York, please visit: http://www.dfs.ny.gov/consumer/hrights.htm
If you have any questions, give us a call at 718-258-3300 or contact us today!
What Is Direct Access and How Can It Help You?
What is direct access?
Direct access is the legal term that states that patients can go straight to a physical therapist to receive treatment, and do not have to get referrals from physicians, which can cause delays and be costly. The term has different conditions in every state, but direct access is available in all 50 states in the US, which means that patients are put at the focus of the treatment plan, and are allowed to receive faster and cheaper services than when required to go through a physician.
What is direct access?
Direct access is the legal term that states that patients can go straight to a physical therapist to receive treatment, and do not have to get referrals from physicians, which can cause delays and be costly. The term has different conditions in every state, but direct access is available in all 50 states in the US, which means that patients are put at the focus of the treatment plan, and are allowed to receive faster and cheaper services than when required to go through a physician.
Are physical therapists qualified to deliver services independent of referral?
Absolutely. Physical therapists are educated at the post-baccalaureate level and receive extensive education and clinical training in the examination, evaluation, diagnosis, prognosis, and intervention of patient/clients with functional limitations, impairments and disabilities. All accredited entry-level physical therapist education programs currently culminate in a Doctor of Physical Therapy (DPT) degree. Physical therapists are qualified to recognize when a patient presents with signs and symptoms inconsistent or outside the scope and expertise of the physical therapist and when the patient should be referred to a physician. APTA's Guide of Professional Conduct advocates that physical therapists should assist patients in receiving appropriate medical care when the physical therapist's examination and evaluation reveals signs and symptoms inconsistent with a condition that can be appropriately treated with physical therapy or needs a physician's care and expertise.
Direct Access Laws in New York
The direct access laws in New York have three conditions:
Treatment can be rendered by a Licensed PT without a referral for 10 visits or 30 days, whichever comes first.
Licensed PT must have practiced PT on a full-time basis for no less than three years; be of at least twenty-one years of age.
PT must provide written notification that services without a referral might not be covered by the patient’s health plan or insurer; notification must state that said services might be covered by health plan or insurer with a referral. Must keep a copy of the written notification in the patient’s file.
The Bottom Line
Allowing individuals to make decisions regarding their health care is inherently good. Eliminating the referral requirement is one step to making health care more accessible to more people across the United States.
Physical therapist education supports practice without referral. Physical therapist practice in the states that allow treatment without referral has proven that it is safe. Yet consumers in many states continue to face arbitrary barriers to physical therapist services.
Direct access is about individual choice in health care decisions through the elimination of unnecessary and burdensome regulation. Direct access also puts control in the patients’ hands, and allows them to be a part of their own plan of care.
What this means for you
This means that you can come to Evolve Physical Therapy without a referral and get treated by one of our amazing physical therapists right away! Should you need more than ten visits, we’d need to get in contact with your doctor, which we’ll try to make as smooth a process as possible.
If you have any questions, give us a call at 718-258-3300 or contact us today!
Rock Steady Group Boxing Classes now in Brooklyn, NYC at Evolve Physical Therapy!
Rock Steady Boxing is a unique exercise program based on training used by boxing pros and adapted to people with Parkinson’s disease, and will now be available in Brooklyn, NY!
Rock Steady Group Boxing Classes now in Brooklyn, NYC at Evolve Physical Therapy!
What is Rock Steady Boxing?
Rock Steady Boxing is a unique exercise program based on training used by boxing pros and adapted to people with Parkinson’s disease, and will now be available in Brooklyn, NY! The program involves regular exercises, such as stretching, bicycling, running, jump-roping, push-ups, balancing and lots of non-contact boxing, led by experienced trainers and coaches. Rock Steady Boxing serves both men and women of all ages and levels of ability.
Is Rock Steady Boxing Safe?
At Evolve, training classes are taught by Physical Therapists and Certified Personal Trainers, and include an exercise program that attacks Parkinson’s at its vulnerable neurological points. Rock Steady Boxing is proven safe and effective addition to a treatment program for Parkinson's disease. It is a non-contact boxing training program led by certified trainers and physical therapists that are experienced with helping people with PD. While focusing on overall fitness, strength training, reaction time and balance, workouts include: focus mitts, heavy bags, speed bags, double-ended bags, jump rope, core work, calisthenics and circuit weight training. No boxing experience is necessary and people of all ages are invited to participate. Boxers, both male and female, range in age from mid-30s to early 90s.
Evolve Physical Therapy in Brooklyn, NY has licensed physical therapists who have been treating patients with Parkinson’s Disease in NYC for over 25 years. Evolve has teamed up with RSB to offer another truly great way to help the Parkinson’s community get stronger and better.
The History
The Rock Steady Boxing Method was developed in Indianapolis over the course of seven years by former Marion County, Indiana Prosecutor, Scott C. Newman, who is currently living with Parkinson’s. In 2012, the Training Camp was launched to share the Rock Steady Boxing Method with other people who are fighting back against Parkinson’s. Today, there are 515 Rock Steady Boxing centers around the world, initiated by certified Rock Steady Boxing coaches, and that number is constantly growing.
It is estimated that 1-1.5 million Americans have Parkinson’s disease, with as many as 60,000 people newly diagnosed with PD each year.
Rock Steady Boxing can help by moving your body in all planes of motion while continuously changing the routine as you progress through the workout. RSB classes have proven that anyone, at any level of Parkinson’s, can actually lessen their symptoms and lead a healthier/happier life.
Can Rock Steady Help You?
Classes - RSB offers four different levels of classes to accommodate varying degrees of Parkinson’s/fitness.
Support - The PTs at Evolve Physical Therapy have years of experience with patients with Parkinson’s Disease, and know how to help patients move and feel better at any degree of fitness. We strive to help patients feel strong and empowered, and work hard to reduce the progression of symptoms, which is why Evolve and Rock Steady make a great match!
Camaraderie - Friends for fighters and caregivers. Group fitness classes and positive atmosphere are proven to push fighters to work harder and will help them get better at a faster pace.
Low Back Pain: Why You Have It, and How to Fix It
The lumbar spine is what is most commonly referred to as the low back, and it is comprised of the last 5 vertebrae of the spine before the tailbone (sacrum). Low back pain can be caused by many different things, but there are a few things that can always help: proper posture, stretching, and strengthening.
How does the low back work?
The lumbar spine is what is most commonly referred to as the low back, and it is comprised of the last 5 vertebrae of the spine before the tailbone (sacrum). The vertebrae are stacked above each other, and there are intervertebral discs (IVDs), which are very tough fribrocartilaginous joints that can withstand a lot of bending and pressure, but if it is overdone, or a chronic issue, you may experience pain.
What causes back pain?
Back pain can be caused by anything that stresses the joint, whether a one-time stressor like lifting a heavy object incorrectly, or a chronic issue like sleeping on an uneven bed or having bad posture. Additionally, because our spine has many nerves running through it, it’s possible that an imbalance in the spinal structure can cause pain to radiate down the leg as well. This condition is known as sciatica, and is also very common among the older population. Low back pain is one of the most common pains among people in the US, and if it lasts longer than 72 hours, there might be a problem that needs immediate care.
How Can Physical Therapy Help?
Because of the sensitivity of the spine, physical therapy is usually recommended before other, more invasive procedures like surgeries or injections. If your back pain is affecting you from doing your daily activities, even if that means things like heavy lifting or sports, physical therapy can get you back into shape, or at the least help you get to doing most tasks pain-free. With mobilizations and strengthening exercises, our goal is to get you back to where you were and to get you stronger, and to advance with proper mechanics so that we can avoid this issue in the future.
What can I do to help myself?
Improve your posture
Posture is something that is always present, and if your back is not aligned, and your spine is out of line with your shoulders and hips, you might be experiencing pain. Align your posture by making sure your shoulders aren’t rounded, and stacking your shoulders above your spine, and above your hips, all in one vertical line. Note that this proper posture is even more important when sitting, because just having shoulders rounded can cause this system to go out of whack.
Exercise
There are many exercises that can help low back pain, but as always, don’t don’t exercise if you’re in pain. Low-impact exercises like swimming are great for keeping strong, but there are also low-back specific exercises that might help. Many people find that yoga is helpful, as this practice usually contains low-impact, slow movement, which can help improve both mobility and stability in the lower back.
Summary
Low back pain can be caused by many different things, but there are a few things that can always help: proper posture, stretching, and strengthening.
Physical therapy is one of the most common ways to relieve low back pain, and most people leave their first visit feeling better.
Try the exercises suggested here to help ease pain and prevent future symptoms.