
Brooklyn Physical Therapy News- Evolve NY
Parkinson's Disease Support: What's Out There and How to Get It
Understanding the Support Landscape for Parkinson's Disease

What support is available for parkinson's disease encompasses medical care, therapies, financial aid, emotional counseling, and community programs. Here's a quick overview:
Core Support Categories:
- Medical Treatment: Neurologists, medications (levodopa), surgery (Deep Brain Stimulation)
- Therapeutic Services: Physical, occupational, and speech therapy; specialized exercise
- Financial Aid: Insurance navigation, copay assistance, grants, welfare benefits
- Emotional Support: Counseling, support groups, helplines
- Caregiver Resources: Respite care, dedicated support groups, educational programs
- National Organizations: Parkinson's Foundation (1-800-4PD-INFO), APDA (800-223-2732), Michael J. Fox Foundation
Parkinson's disease is a progressive neurological disorder affecting movement with symptoms like tremors and balance problems. However, about 50% of people with Parkinson's also face non-motor symptoms such as anxiety, depression, and pain.
The good news is you don't have to face it alone. A comprehensive support system exists to manage these challenges, from medication and surgery to specialized exercise like Rock Steady Boxing and financial aid. Accessing the right resources can dramatically improve quality of life.
I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy in Brooklyn with experience in neurological rehabilitation. I've helped many individuals steer what support is available for parkinson's disease to regain function and independence. This guide will walk you through the major support avenues to help you build a comprehensive care plan.

Medical and Therapeutic Support for Managing Symptoms
Proper medical care begins with a diagnosis from a neurologist. Since there's no single definitive test, a diagnosis is based on your medical history, symptoms, and a neurological exam. Your doctor may order blood tests or imaging like an MRI or a dopamine transporter (DAT) scan to rule out other conditions. A promising new development is the alpha-synuclein seed amplification assay, which accurately identified Parkinson's in 87.7% of cases using spinal fluid and may lead to a future blood test.
Once diagnosed, medication is the cornerstone of symptom management, working to increase or substitute for dopamine.
- Levodopa (often with Carbidopa) is the most effective medication, converted by the brain into dopamine. It can be taken as a pill, inhaled powder (Inbrija), or continuous infusion (Duopa).
- Dopamine agonists (e.g., Pramipexole) mimic dopamine's effects and are often used in earlier stages.
- MAO-B inhibitors (e.g., Selegiline) block an enzyme that breaks down dopamine, making it last longer.
- COMT inhibitors (e.g., Entacapone) are sometimes added to extend the effectiveness of levodopa.
When medications become less effective or cause side effects like dyskinesia (involuntary movements), surgical options can offer relief.
- Deep Brain Stimulation (DBS) involves implanting electrodes in the brain that send electrical pulses to reduce tremors and dyskinesia.
- MRI-guided focused ultrasound is a less invasive option that uses ultrasound waves to treat severe tremors. You can learn more about clinical trials for MRI-guided focused ultrasound for Parkinson's disease.
The Crucial Role of Supportive Therapies
Supportive therapies are essential for maintaining independence. Think of them as a coaching team to help you thrive.
- Physiotherapy addresses movement difficulties like stiffness and poor balance through targeted exercises. At Evolve Physical Therapy, our specialized Parkinson's Physical Therapy Brooklyn program uses a hands-on approach to help you move better.
- Occupational therapy helps you find safer ways to perform daily tasks like dressing and cooking, often recommending home modifications and assistive devices.
- Speech and language therapy strengthens your voice, improves articulation, and addresses swallowing difficulties to ensure you can eat and drink safely.
- Diet and nutrition advice from a dietitian can help manage issues like constipation and optimize medication absorption.
Engaging in these therapies is fundamental to effective disease management and is proven to maintain better function and quality of life, as emphasized by organizations like Parkinson's UK and their information on the role of therapies in Parkinson's care.
Specialized Exercise and Lifestyle Programs
Regular exercise is powerful medicine for Parkinson's, shown to slow motor decline and improve symptoms.
- Beneficial Activities: Aerobic exercises like walking and swimming, Tai Chi for balance, Yoga for flexibility, and dance for movement and mood are all excellent choices.
- Rock Steady Boxing: We are passionate about this non-contact, boxing-inspired fitness program created for people with Parkinson's. It improves balance, gait, agility, and strength in a supportive group setting. We're proud to offer it at Rock Steady Boxing Brooklyn NYC, and our program's transformative impact was even featured on NBC Nightly News Covers Rock Steady Boxing at Evolve Physical Therapy.
Fall prevention is critical. Simple strategies like using handrails, installing night-lights, and removing throw rugs make a big difference. A physical therapist can teach you safer walking techniques and recommend assistive devices.
Lifestyle adjustments like a high-fiber diet, adequate hydration, and good sleep also support overall health. Always discuss these changes with your healthcare team. Understanding what support is available for parkinson's disease means recognizing that medical treatment and therapeutic support work hand-in-hand.
What Support is Available for Parkinson's Disease: Financial and Practical Aid
The financial side of living with Parkinson's can be daunting, but what support is available for parkinson's disease includes significant financial and practical assistance.
Navigating insurance and healthcare costs is often overwhelming. A smart first step is a care and support needs assessment from your local authority. This assessment creates a personalized care plan and can open doors to practical help, such as home modifications and assistive devices. An occupational therapist can recommend items like grab bars or walking aids to improve safety and independence.
How can individuals access financial assistance for Parkinson's disease?
No one should have to skip medication due to cost. Several resources exist to provide financial relief.
The PAN Foundation offers grants and copay assistance programs to help people manage medication costs, removing financial barriers to treatment. You can learn more or contribute by visiting their page on giving now to help patients afford medication.
Additionally, local authority support and welfare benefits can offer broader financial aid. Many people are eligible for benefits they aren't claiming. National organizations are experts in this area. For example, Parkinson's UK provides detailed information on financial support, including welfare benefits, grants, and loans.
Don't hesitate to explore these options. These programs are designed to help you manage the costs of Parkinson's. Reaching out is a smart strategy for managing your condition effectively. Access to financial grants, home modifications, and assistive devices is a fundamental part of living well with Parkinson's.
Finding Emotional, Community, and Caregiver Support
Living with Parkinson's involves more than physical symptoms. The emotional impact is significant, with a 2022 study showing that roughly 50% of people with Parkinson's experience anxiety, depression, or pain. These feelings are valid, and addressing them is a critical part of your care.
Mental health professionals who specialize in chronic illness can provide crucial support. However, sometimes the most powerful help comes from connecting with peers who understand your journey. Sharing your story can be incredibly relieving. That's why we created spaces like our Parkinson's Disease Online Support Group, offering comfort and friendship from home.
Primary Organizations and Their Resources
Three major organizations serve as resource headquarters for the Parkinson's community.
- The Parkinson's Foundation is a lifeline for many. Their Helpline at 1-800-4PD-INFO offers support in English and Spanish. They also provide educational materials, webinars, local chapters, and the PD GENEration program for no-cost genetic testing. Explore their offerings at the Parkinson's Foundation.
- The American Parkinson Disease Association (APDA) provides support wherever you are. Their Helpline at 800-223-2732 offers assistance in English, Spanish, and Mandarin. They host free webinars, virtual fitness classes, and offer a vast Resource Library. Learn more at the American Parkinson Disease Association.
- The Michael J. Fox Foundation focuses on accelerating research but also provides extensive educational resources to keep you informed about the latest developments. Visit the Michael J. Fox Foundation to learn more.
How can caregivers receive support and education?
If you're a caregiver, you deserve support, too. Caregiving is a demanding role, and caregiver stress is real and common. It's okay to feel overwhelmed.
Education can empower you. Johns Hopkins Medicine offers practical guides for caregivers, and we've developed our own resources, including Caregiver Support for Parkinson's, to address your unique challenges.
Connecting with other caregivers is transformative. In a support group, you'll find people who understand the fatigue, guilt, and small victories. Our Parkinson's Caregiver Support Group provides a welcoming space for these connections.
Finally, consider respite care. Taking breaks is essential for your own well-being and allows you to continue providing loving support.
Where can I find local and specialized support groups?
Finding your community can change your entire experience with Parkinson's.
- Local chapters of organizations like the Parkinson's Foundation offer face-to-face meetings, exercise classes, and social events. You can find your local chapter to connect with people in your area.
- Online groups provide convenient connection, especially if you have mobility challenges or live in a rural area.
- For the newly diagnosed, targeted programs like Parkinson's UK's "First Steps" can help you make sense of your diagnosis and start living well from day one.
If you can't find a group that fits, consider starting one. We offer a guide on how to form a support group for Parkinson's to help you bring people together.
The Future of Parkinson's Care: Research and Advocacy
Parkinson's research is advancing rapidly, bringing hope for better treatments, earlier detection, and a cure.
A major breakthrough is the alpha-synuclein seed amplification assay, a test that can detect Parkinson's before symptoms begin, with work underway to develop it into a simple blood test. Clinical trials are the backbone of this progress, offering participants access to cutting-edge treatments while advancing science.
The Parkinson's Foundation's PD GENEration program provides no-cost genetic testing, contributing to a massive database that helps researchers identify genetic links to the disease. Meanwhile, care standards are continuously updated through resources like the NICE guidelines on Parkinson's disease, ensuring patients know what care to expect.
How to Get Involved and Make a Difference
You have the power to make a difference, even without a scientific background. Here’s how you can contribute:
- Participate in Research: Your experience is invaluable. Parkinson's UK makes it easy to get involved in research through trials, surveys, and other studies.
- Volunteer: Give your time to a local support group or fundraising event to make an immediate impact.
- Fundraise: Every dollar helps accelerate the search for a cure. You can donate to support research and know you're making a difference.
- Advocate: Use your voice to campaign for better care, fair benefits, and increased awareness.
- Spread Awareness: Talk openly about Parkinson's to correct misconceptions and build a more supportive community.
By getting involved, you can help change what it means to live with Parkinson's.
Frequently Asked Questions about Parkinson's Support
Here are answers to some common questions about what support is available for parkinson's disease.
What is the first step after a Parkinson's diagnosis?
After a diagnosis, focus on these key actions:
- Consult a movement disorder specialist: This neurologist has expert knowledge of Parkinson's treatments.
- Build your healthcare team: Include a physical therapist, occupational therapist, and speech therapist to help maintain your quality of life.
- Seek trusted information: Use resources from the Parkinson's Foundation and the American Parkinson Disease Association (APDA).
- Find a support group: Connecting with peers provides emotional comfort and practical advice.
Can exercise really help with Parkinson's symptoms?
Yes, absolutely. Exercise is one of the most powerful tools for managing Parkinson's. Research shows that regular, targeted exercise can improve balance, flexibility, and strength, and may even slow motor decline.
Programs like Rock Steady Boxing, which we offer at Evolve Physical Therapy, are specifically designed to combat symptoms like poor balance, gait issues, and rigidity. Other beneficial activities include Tai Chi, yoga, dance, and swimming. The key is consistency and finding an activity you enjoy.
Are there support options available in different languages?
Yes. Accessibility is a priority for major Parkinson's organizations.
- The American Parkinson Disease Association (APDA) helpline (800-223-2732) offers support in English, Spanish, and Mandarin.
- The Parkinson's Foundation helpline (1-800-4PD-INFO) provides assistance in English and Spanish.
Many organizations also offer educational materials and resources in multiple languages and accessible formats. If you need support in a specific language, contact these foundations directly for guidance.
Conclusion
Living with Parkinson's disease is a journey, but you are not alone. As we've explored, what support is available for parkinson's disease is extensive and built on several key pillars:
- Medical Support: Your neurologist, effective medications, and advanced surgical options.
- Therapeutic Support: Physical, occupational, and speech therapists who help you maintain independence. Programs like Rock Steady Boxing empower you to fight back against symptoms.
- Financial & Practical Help: Assistance from organizations like the PAN Foundation to manage costs.
- Emotional & Community Support: Helplines, support groups, and caregiver resources that connect you with a community that understands.
Research is also providing new hope through genetic testing, earlier diagnosis, and innovative treatments. By getting involved, you can help shape a better future.
Taking the first step can feel daunting, but it can be as simple as calling a helpline or trying a new exercise class. Each action is a move toward living well with Parkinson's.
If you're in the Brooklyn area and ready to see how specialized physical therapy can improve your quality of life, we invite you to connect with us. Learn more about specialized Parkinson's physical therapy in Brooklyn and find how the hands-on approach at Evolve Physical Therapy can support your journey. We're here for you.
On Pointe Recovery – Physical Therapy for Dance Injuries
Why Dance Demands More Than Standard Physical Therapy

Physical therapy for dancers is a specialized discipline that addresses the unique biomechanical demands of dance while supporting both injury recovery and performance improvement. Here's what makes it essential:
- Treats dance-specific injuries like patellofemoral pain syndrome, ankle sprains, stress fractures, and snapping hip syndrome
- Addresses the root causes of pain through hands-on manual therapy, alignment correction, and movement retraining
- Improves performance by improving technique, turnout, stability, and movement efficiency
- Prevents future injuries through targeted strengthening, flexibility work, and biomechanical analysis
- Speaks your language using dance terminology and understanding the artistic demands of your craft
Dance is an extraordinary blend of art and athleticism. As one physical therapist who works extensively with dancers noted, "Dancers are incredible athletes with control and grace like no other." But this beauty comes at a cost. Research shows that 67-95% of professional dancers experience injuries annually, with 87.7% of those injuries occurring from the hip down. The repetitive nature of ballet movements, high training volumes averaging 20 hours per week, and the need to push beyond normal anatomical limits make dancers particularly vulnerable to overuse injuries.
Unlike standard physical therapy, dance rehabilitation requires a deep understanding of dance technique, biomechanics, and the specific movements that define your art form. A therapist who understands the difference between a plié and a relevé, who can assess your turnout mechanics, and who recognizes that your body is your instrument can make the difference between simply healing and returning stronger than before.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and over nearly two decades, I've specialized in treating complex musculoskeletal conditions and helping artistic athletes optimize their movement patterns. Physical therapy for dancers requires a holistic, hands-on approach that addresses not just the injury site but the entire kinetic chain—from how you initiate movement to how you land from a jump.
The Dancer's Body: Common Injuries and Their Causes
Your body is your instrument, and the high training volume of dance—often 20 hours or more per week—leads to overuse injuries from repetitive strain. Dancers push beyond normal anatomical limits, creating a perfect storm for injury. Research shows injury rates spike during peak rehearsal and performance seasons (typically October, November, March, and April), highlighting the need for specialized physical therapy for dancers that understands the art form's unique demands.
The Lower Body Under Pressure: Foot, Ankle, and Knee Injuries
Over 50% of all dance injuries occur in the foot and ankle, with another 16.1% affecting the knee. Your lower body absorbs tremendous force with every movement.
- Patellofemoral Pain Syndrome ("Dancer's Knee"): Pain around or behind the kneecap, often from inflammation of the cartilage. It's aggravated by turning, jumping, poor posture, or hard studio floors.
- Ankle Sprains: Common during turns and leaps, these happen when ligaments are overstretched or torn.
- Achilles Tendonitis: A burning pain in the back of the lower leg from the inflammation caused by repetitive jumping and push-offs.
- Sesamoiditis: Inflammation of the small bones under the big toe joint, creating sharp pain. It is particularly common for dancers en pointe due to constant pressure.
- Stress Fractures: Tiny cracks in the bone that develop gradually from repetitive impact without adequate recovery time. They often start as a whisper and can become a major injury if ignored. A study on ballet injury incidence emphasizes how common these injuries are.
Core and Control: Hip and Back Injuries
Your hips and back are your body's control center, accounting for 21.6% and 9.4% of dance injuries, respectively. These injuries can be limiting as they affect your core stability.
- Snapping Hip Syndrome: A palpable or audible "snap" around the hip when tendons glide over bone during movements like développés. While not always painful, it signals improper mechanics.
- Femoral Acetabular Impingement (FAI): Painful pinching in the hip joint caused by extra bone growth, which can limit your range of motion during extensions.
- Spondylolisthesis: A stress fracture in a vertebra, causing it to slip forward. This can be caused by the repeated hyperextension of the spine in movements like arabesques.
- Lower Back Pain & Sciatica: Lower back pain is often a red flag for poor core control or muscle imbalances. It can lead to sciatica, which causes shooting pain down one or both legs.
Key risk factors for all dance injuries include poor technique, muscle imbalances, inadequate rest, and nutritional deficits. Understanding these risks is the first step toward prevention and where specialized physical therapy for dancers becomes invaluable.
The Role of Specialized Physical Therapy for Dancers
Specialized physical therapy for dancers recognizes that your body is your instrument. At Evolve Physical Therapy, our holistic approach goes beyond treating an injury to improve your technique and build career-long resilience. We create custom treatment plans that address how you move, your performance goals, and what your body needs to thrive in the demanding world of dance.
The Initial Assessment: A Dance-Specific Evaluation
The foundation of effective treatment is a thorough, dance-specific evaluation. After listening to your dance history and goals, we perform a comprehensive assessment including:
- Posture and Gait Analysis: Examining your alignment both standing still and in motion to find compensatory patterns.
- Joint Range of Motion & Muscle Symmetry: Identifying areas of restriction, hypermobility, and strength imbalances between sides of the body.
- Biomechanical Analysis of Dance Movements: We watch you perform pliés, relevés, and jumps to find subtle technique flaws that may contribute to injury, such as "rolling in" at the ankles.
- Pointe-Readiness Screens: For younger ballet dancers, we conduct specialized tests of ankle strength, foot mobility, and core stability to ensure the body is ready for the demands of pointe work and to prevent serious injury.
This detailed evaluation allows us to create a treatment plan that addresses the root cause of your problem, not just the symptoms.
Custom Rehabilitation: Beyond Standard Exercises
Standard physical therapy exercises are not enough for dancers. Our custom rehabilitation programs use specialized interventions that are proven to be more effective, as supported by research on the effectiveness of physiotherapy for ballet dancers. Key components of our treatment include:
- Manual Therapy: We use hands-on techniques like joint mobilization and soft tissue massage to restore mobility, release muscle tension, and reduce pain.
- Alignment Correction & Neuromuscular Re-education: We retrain your body for optimal positioning and improve the brain-muscle connection for better coordination, balance, and proprioception (your body's awareness in space).
- Dance Modification Strategies: Instead of just telling you to rest, we work with you to modify movements—like adjusting jump height or plié depth—so you can continue training safely while you recover.
- Using Dance Terminology: We speak your language. When we talk about your turnout, développé, or épaulement, you know exactly what we mean, making our instructions immediately applicable to your training.

Communication is Key: Speaking the Language of Dance
The relationship between a dancer and physical therapist is a partnership built on clear communication. We start with collaborative goal setting to align your recovery with your artistic aspirations. We provide dancer education on anatomy and biomechanics, empowering you to understand the "why" behind your treatment. By speaking your language and demonstrating a deep knowledge of your art form, we build trust and create a space for honest conversations. Our ultimate goal is to empower you with the tools and confidence to manage your body proactively, supporting your longevity as a dancer.
From Rehabilitation to Resilience: Injury Prevention and Performance Improvement
At Evolve Physical Therapy, our approach to physical therapy for dancers extends beyond recovery to building resilience and enhancing performance. We encourage a proactive mindset, where injury prevention is woven into your training routine—like regular maintenance for your body, your most valuable instrument.
Building a Stronger Foundation: Proactive Physical therapy for dancers
Proactive physical therapy is about training smarter, not just harder. We help you build a stronger foundation for dance through:
- Cross-training: Activities like swimming, cycling, or targeted strength work build overall fitness and balance muscle development, giving your dance-specific muscles a much-needed break.
- Core Strengthening: We focus on the deep stabilizing muscles that support your pelvis and spine, providing a stable foundation for every movement you make.
- Gluteal Muscle Activation: Strong glutes are your secret weapon for knee health, powerful jumps, and safe, effective turnout. Correctly firing these muscles helps prevent conditions like patellofemoral pain syndrome.
- Proprioception and Balance Training: These exercises heighten your body's spatial awareness, leading to more precise footwork, steadier balances, and better mid-movement adjustments.
- Differentiating Flexibility vs. Hypermobility: Many dancers have extraordinary flexibility, but without adequate strength to control it, this can increase injury risk. We teach you how to identify and stabilize hypermobile joints to keep them safe.
We also emphasize daily practices like proper warm-ups, cool-downs, hydration, and listening to your body's early warning signs.

Integrating Holistic Methods for Peak Performance
We integrate specialized movement modalities to accelerate recovery and transform how you move and perform. Pilates develops precise core control and body awareness. Gyrotonic training uses three-dimensional, spiraling movements to improve spinal mobility and build strength. Yoga connects breath with movement, improving flexibility, balance, and mind-body awareness.
| Method | Primary Benefits for Dancers |
|---|---|
| Pilates | Deep core control, precise alignment, strengthening without bulk, improved stability for turns and balances |
| Gyrotonic | Improved spinal mobility and articulation, three-dimensional strength, fluid movement patterns, joint decompression |
| Yoga | Mind-body awareness, breath control, flexibility with stability, mental focus, stress reduction |
The Ultimate Goal: Enhancing Artistry and Career Longevity
Proactive physical therapy helps you dance better, longer, and with more joy. The benefits include:
- Improved Technique: With proper alignment and conditioning, movements become more efficient and lines become cleaner.
- Improved Stability: A strong foundation leads to softer landings from jumps and more confident balances.
- Greater Movement Efficiency: You conserve energy for artistry and expression, which improves your endurance.
- Increased Confidence: Trusting your strong, resilient body allows you to take artistic risks without fear.
- Reduced Re-injury Risk: By addressing the root causes of injury, we help you achieve fewer setbacks and a more sustainable career.
Why Dance Demands More Than Standard Physical Therapy
Physical therapy for dancers is a specialized discipline that addresses the unique biomechanical demands of dance while supporting both injury recovery and performance improvement. Here's what makes it essential:
- Treats dance-specific injuries such as patellofemoral pain syndrome, ankle sprains, stress fractures, and snapping hip syndrome
- Addresses root causes with manual therapy, alignment correction, and movement retraining
- Improves performance by refining technique, turnout, stability, and movement efficiency
- Prevents future injuries through targeted strengthening, flexibility work, and biomechanical analysis
- Speaks your language with dance terminology and an understanding of artistic demands
Dance blends art and athleticism, but the physical cost is high. Research shows that 67-95% of professional dancers experience injuries annually, with 87.7% occurring from the hip down. High training volumes (often ~20 hours/week), repetitive movements, and extreme ranges of motion increase overuse risk.
Unlike standard physical therapy, dance rehabilitation requires deep knowledge of technique and biomechanics. A therapist who understands a plié versus a relevé, can assess turnout mechanics, and recognizes that your body is your instrument can be the difference between simply healing and returning stronger.
I'm Lou Ezrick, founder of Evolve Physical Therapy. For nearly two decades I've helped artistic athletes resolve complex musculoskeletal issues. Effective physical therapy for dancers treats the whole kinetic chain—from initiation to landing—so you can recover and perform at your best.
The Dancer's Body: Common Injuries and Their Causes
Dancers are artistic athletes training at high volumes, often 20+ hours per week. Repetition, extreme ranges, and hard floors create overuse and biomechanical stress that demand targeted care.
The Lower Body Under Pressure: Foot, Ankle, and Knee Injuries
Over 50% of dance injuries involve the foot and ankle; another 16.1% affect the knee.
- Patellofemoral Pain Syndrome ("Dancer's Knee"): Pain around or behind the kneecap, aggravated by turning, jumping, poor posture, or hard floors.
- Ankle Sprains: Ligament overstretch/tear during turns, leaps, and quick direction changes.
- Achilles Tendonitis: Burning pain from repetitive push-offs and landings.
- Sesamoiditis: Sharp pain under the big toe joint, common en pointe due to constant pressure.
- Stress Fractures: Tiny bone cracks from repetitive impact and inadequate recovery. A study on ballet injury incidence highlights how common these are.

Core and Control: Hip and Back Injuries
Hips and back account for 21.6% and 9.4% of injuries, affecting stability and control.
- Snapping Hip Syndrome: Audible/palpable snap when tendons glide over bone during développés; signals mechanics to address.
- Femoral Acetabular Impingement (FAI): Painful pinching from extra bone growth, limiting high extensions.
- Spondylolisthesis: Vertebral stress fracture and forward slip, exacerbated by repeated hyperextension.
- Lower Back Pain & Sciatica: Often from core control deficits or imbalances; may radiate down a leg.
Key risk factors:
- Poor technique
- Muscle imbalances
- Inadequate rest
- Nutritional deficits
Understanding these patterns is step one; specialized physical therapy for dancers addresses root causes to keep you dancing.
The Role of Specialized Physical Therapy for Dancers
At Evolve Physical Therapy, we treat dancers as artists and athletes. Our holistic approach looks beyond the painful area to your technique, goals, and the specific demands of your style, building a plan that heals, improves performance, and supports longevity.
The Initial Assessment: A Dance-Specific Evaluation
- Posture and Gait Analysis: Identify static/dynamic alignment issues and compensations.
- Joint Range of Motion & Muscle Symmetry: Flag restrictions, hypermobility, and side-to-side imbalances.
- Biomechanical Analysis of Dance Movements: Observe pliés, relevés, turns, and jumps to find subtle flaws (e.g., ankle rolling in turnout).
- Pointe-Readiness Screens: Assess ankle/foot strength, mobility, balance, and core stability before going en pointe.
Custom Rehabilitation: Beyond Standard Exercises
We blend PT fundamentals with dance-specific strategies shown to help dancers. See Effectiveness of physiotherapy for ballet dancers.
- Manual Therapy: Joint mobilization and soft-tissue techniques to restore mobility and reduce pain.
- Alignment Correction & Neuromuscular Re-education: Rebuild optimal positioning, balance, and proprioception.
- Dance Modification Strategies: Adjust jump height, plié depth, or rotation so you can keep training safely.
- Using Dance Terminology: Clear cues in your language (turnout, développé, épaulement).
Communication is Key: Speaking the Language of Dance
We partner with you through:
- Collaborative goal setting aligned with training and performance schedules
- Education on body mechanics so you understand the "why" behind your plan
- Trust and empowerment that support honest dialogue and long-term self-management
From Rehabilitation to Resilience: Injury Prevention and Performance Improvement
Our goal is not just recovery but resilience. We integrate proactive care into your routine so you can perform more consistently and avoid setbacks.
Building a Stronger Foundation: Proactive Physical therapy for dancers
- Cross-training benefits: Add swimming, cycling, or strength work to balance high dance volumes without overloading the same tissues.
- Core strengthening: Train deep stabilizers for stable turns, controlled extensions, and powerful jumps.
- Gluteal activation: Protect knees, support turnout, and improve propulsion.
- Proprioception and balance training: Sharpen spatial awareness for precise footwork and steadier balances.
- Flexibility vs. hypermobility: Maintain range while stabilizing hypermobile joints.
Integrating Holistic Methods for Peak Performance
A truly holistic approach to physical therapy for dancers often incorporates specialized movement modalities that complement traditional PT. These methods not only aid in recovery but also significantly improve a dancer's technique and overall physical intelligence.
| Method | Primary Benefits for Dancers |
|---|---|
| Pilates | Focuses on core strength, stability, precision, and breath. It builds balanced musculature and improves body awareness, crucial for controlled dance movements and injury prevention. Excellent for strengthening deep stabilizers and achieving efficient movement patterns. |
| Gyrotonic Method | Emphasizes circular, flowing movements and spinal articulation. It improves spinal mobility, joint articulation, and functional strength, promoting a sense of freedom and fluidity in movement. Ideal for improving range of motion and neuromuscular coordination. |
| Yoga | Cultivates flexibility, strength, balance, and mental focus through various poses and breathwork. It improves body awareness, reduces stress, and improves overall physical and mental well-being, complementing the mental and physical demands of dance. |
The Ultimate Goal: Enhancing Artistry and Career Longevity
- Improved technique and control through alignment and conditioning
- Greater stability for softer landings and confident balances
- More efficient movement to conserve energy for artistry
- Increased confidence to take risks safely
- Lower re-injury risk by correcting root causes and building durable habits
Frequently Asked Questions about Dance Physical Therapy
What are the primary goals of physical therapy for dancers?
The primary goals extend beyond immediate pain relief. We aim to:
- Heal and Get You Back to Dancing: Address the current injury so you can return to the studio safely.
- Prevent Future Injuries: Identify and correct the root causes of the injury, such as muscle imbalances or alignment issues.
- Improve Performance: Improve your technique by strengthening specific support muscles for cleaner lines, better turnout, and more controlled movements.
- Educate and Empower: Give you the knowledge to understand your body, recognize warning signs, and manage your health for a long, successful dance career.
It's a partnership to build a more resilient and aware artist.
How does physical therapy improve a dancer's technique, not just heal an injury?
Physical therapy improves technique by identifying and correcting hidden physical limitations that may be holding you back. For example, if you struggle with your arabesque height, a therapist will analyze if tight hip flexors or inactive glutes are the true cause.
By using targeted strengthening, mobility work, and neuromuscular re-education, we correct these underlying biomechanical issues. When you learn to activate the right muscles in the right sequence, movements like balances and turns become more stable and controlled with less effort. By making your body move more efficiently, we free you to focus on your artistry.
When is it safe for a dancer to return to pointe work after an injury?
A safe return to pointe work is determined by a physical therapist through a thorough, progressive assessment, not just by the absence of pain. We evaluate multiple factors:
- Strength: We test the intrinsic foot muscles, ankles, calves, and glutes to ensure they can provide adequate support.
- Stability and Control: You must be able to perform foundational movements like single-leg relevés with perfect alignment and without pain or compensation.
- Range of Motion: You need sufficient ankle plantarflexion and foot articulation to rise onto pointe correctly.
Once these criteria are met, the return is always gradual. We start with short periods at the barre and slowly progress to more complex work, always in close communication with you and your dance instructor. This methodical approach is the best way to prevent re-injury and ensure a long-term return to dancing.
Conclusion: Take the Next Step in Your Dance Journey
Your body is your instrument, and like any finely tuned instrument, it deserves specialized care. Throughout your dance journey—from your first plié to your hundredth performance—the physical demands never let up. The beauty you create on stage comes from dedication, artistry, and yes, an extraordinary amount of physical stress.
We understand this at Evolve Physical Therapy in Brooklyn, where we serve dancers throughout Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin. Physical therapy for dancers isn't something you should only think about when you're injured. It's a partnership that supports you through every stage of your career—whether you're recovering from a stress fracture, working to prevent dancer's knee, or simply looking to refine your technique and perform at your peak.
Our approach is different because we see the whole picture. We use hands-on manual therapy to address the root causes of your pain, not just mask the symptoms. We speak your language, understanding the difference between a développé and a dégagé, and we know what it takes to safely return to pointe work. We integrate holistic methods like Pilates and Gyrotonic that complement your training rather than compete with it.
Most importantly, we empower you. We teach you about your body's unique mechanics, help you build strength where you need it most, and give you the tools to stay healthy for the long haul. Because dance isn't just about getting through today's rehearsal—it's about sustaining a lifelong passion.
Whether you're dealing with an injury right now or you're ready to take a proactive approach to your physical health, we're here to help you move with greater freedom, confidence, and artistry. Your dance journey deserves a partner who truly understands what you do and what you need.
Ready to dance stronger, safer, and longer? Take control of your dance health with physical therapy.
Mobilizations with Movement: Your Joints Will Thank You
Why Your Joints Need Mobilizations with Movement

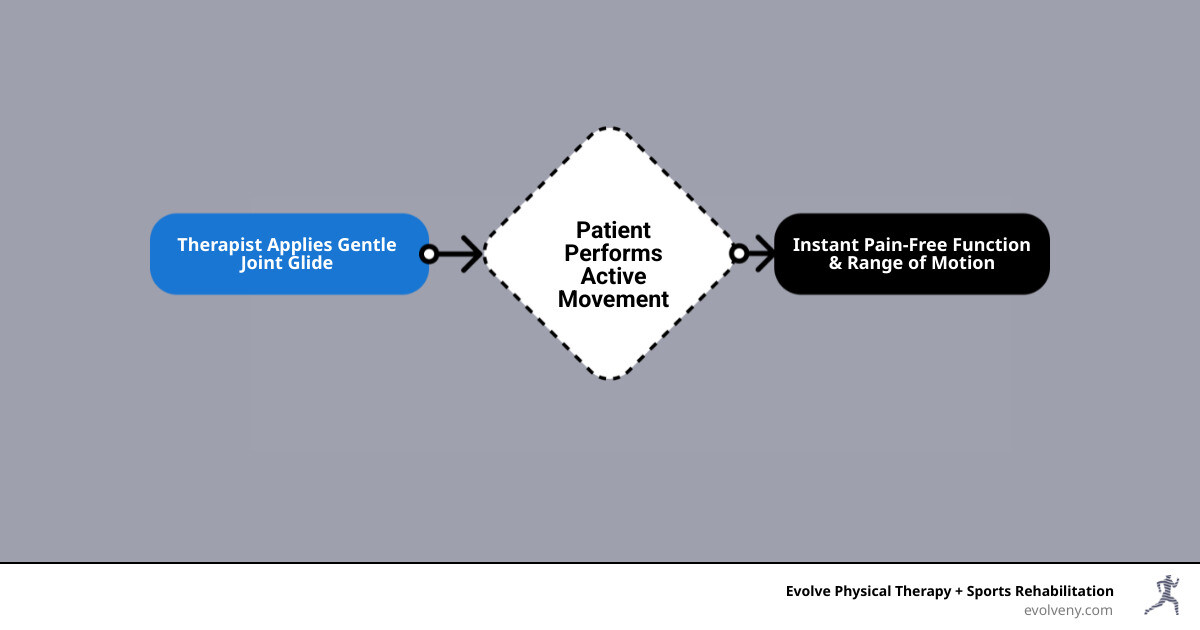
Mobilizations with Movement is a manual therapy technique that combines gentle joint gliding with active movement to restore pain-free function instantly. Developed by New Zealand physiotherapist Brian Mulligan in the 1980s, this approach has transformed how we treat joint dysfunction and movement restrictions.
Key Features of Mobilizations with Movement:
- Pain-free technique - No discomfort during treatment
- Instant results - Immediate improvement in movement and pain
- Long-lasting effects - Benefits persist after treatment
- Active participation - You move while the therapist guides your joint
- Self-treatment options - Learn techniques to maintain progress at home
Unlike traditional joint mobilization where you lie passively, MWM requires your active participation. The therapist applies a specific glide to your joint while you perform the previously painful or restricted movement. When done correctly, pain disappears and full range of motion returns immediately.
This technique works on the principle that many joint problems stem from minor "positional faults" - small misalignments that disrupt normal joint mechanics. By correcting these faults during movement, MWM restores proper joint tracking and eliminates pain.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've used mobilizations with movement techniques for nearly two decades to help patients overcome chronic pain and movement restrictions that traditional approaches couldn't resolve. My experience treating complex cases in Tel Aviv and Brooklyn has shown me the remarkable power of MWM to restore function when other treatments fall short.
Unpacking the Mulligan Concept: Core Principles and Theories
When Brian Mulligan first developed his approach back in the 1980s, he revolutionized how we think about joint problems. Instead of just pushing and pulling on stiff joints, he finded something remarkable: many of our aches and pains come from tiny misalignments that we can fix while we're actually moving.
Think of it like this - your joints are supposed to glide smoothly like a well-oiled machine. But sometimes, after an injury or from poor posture, they get slightly "off track." Traditional therapy often tries to fix this by moving your joint for you while you lie still. Mobilizations with movement takes a completely different approach - we guide your joint back into its proper path while you actively use it.
This isn't just theory anymore. After decades of use across five continents, we know that MWM works through multiple pathways. It corrects mechanical problems, calms down irritated nerves, and gives patients that incredible "aha!" moment when pain-free movement returns instantly. There's something deeply empowering about feeling your body work properly again after months or years of limitations.
At Evolve Physical Therapy, we've seen countless patients light up when they experience their first pain-free shoulder raise or effortless neck turn. It's these moments that remind us why we love what we do. More info about our hands-on approach explains how we integrate these powerful techniques into comprehensive care.
The 'Positional Fault' Theory Explained
Picture trying to slide a drawer that's slightly crooked in its frame. It catches, it sticks, and sometimes it just won't budge. Your joints can develop similar problems - what we call positional faults.
These aren't the dramatic dislocations you might see in emergency rooms. We're talking about subtle shifts that might not even show up on X-rays. Maybe your shoulder blade isn't sitting quite right, or your wrist bones aren't tracking perfectly when you bend your hand. These tiny misalignments can create big problems.
The beauty of understanding positional faults is realizing they're fixable. When we apply mobilizations with movement, we're essentially helping that "crooked drawer" slide smoothly again. We gently guide your joint back into its happy place while you move it through the motion that was causing trouble.
What's amazing is how quickly your body responds. Once we find the right direction and amount of guidance, that painful movement often becomes completely comfortable - sometimes within seconds. Your joint remembers how it's supposed to move, and the pain simply melts away.
The Guiding Principles: PILL and CROCKS
Every effective treatment approach needs clear guidelines, and mobilizations with movement follows two essential frameworks that keep both therapists and patients on track.
The PILL response is our gold standard for success. If we don't see all three components, we know this particular approach isn't the right fit for your specific problem. No forcing, no "working through the pain" - we simply try a different strategy. The criteria are:
- Pain-free: The movement must be completely pain-free. If it hurts, we're not doing it right.
- Instant: You should feel the difference immediately, not days later.
- Long-lasting: The positive changes should stick around after we finish the technique.
For therapists applying these techniques, the CROCKS principles ensure safe, effective treatment:
- Contraindications: We always check for conditions that would make this technique unsuitable.
- Repetitions: Repetitions help your nervous system learn the new, pain-free movement pattern.
- Overpressure: Gentle overpressure at the end of your available range can boost the lasting effects.
- Communication: Your feedback is crucial every step of the way.
- Knowledge: Our knowledge of anatomy and biomechanics guides precise application.
- Sustained mobilization: We maintain that gentle guidance throughout your entire movement.
These aren't just academic concepts - they're practical tools that help us deliver the remarkable results MWM is known for.
How MWM Differs from Traditional Mobilization
The difference between mobilizations with movement and traditional joint mobilization is like comparing learning to ride a bike with training wheels versus having someone push your bike while you sit on it. While both can be helpful, they operate on fundamentally different principles.
Here's a quick comparison:
| Feature | Mobilizations with Movement (MWM) | Traditional Mobilization |
|---|---|---|
| Patient Involvement | Active - You perform the movement. | Passive - The therapist moves your joint for you. |
| Application | During active, functional movement. | On a static, resting joint. |
| Goal | Restore immediate, pain-free function. | Reduce stiffness and improve passive range. |
| Feedback | Instant functional change (e.g., increased motion). | Gradual symptom response over time. |
| Pain Principle | Strictly pain-free; pain indicates incorrect technique. | May involve some discomfort to achieve tissue changes. |
In MWM, you're the star of the show, actively participating in your recovery by performing the very movement that was causing trouble, now made pain-free. This real-time correction of movement patterns is not only more comfortable but also more functionally relevant to your daily life, as your nervous system learns the new, correct way to move without protective responses.
The Power of Mobilizations with Movement in Action
When you're dealing with pain or movement restrictions, you want results - and you want them fast. That's exactly what mobilizations with movement delivers. This powerful technique has transformed countless lives at our clinic, helping people overcome musculoskeletal disorders that seemed impossible to resolve.
What makes MWM so remarkable is its versatility. Whether you're struggling with chronic shoulder pain, can't grip a coffee cup without wincing, or find yourself limping after an ankle sprain, mobilizations with movement offers a path forward. The technique works by addressing the root cause of your movement dysfunction, not just masking the symptoms.
The research backing MWM continues to grow stronger each year. Studies consistently show that when applied correctly, this approach leads to immediate pain relief and lasting functional improvements. What used to take weeks or months of traditional therapy can often be achieved in a single session - though we always follow up to ensure those gains stick around.
One of the most empowering aspects of mobilizations with movement is how it teaches you to become an active participant in your recovery. Many techniques can be adapted for self-treatment, giving you tools to maintain your progress at home. It's like learning to tune your own instrument instead of always needing someone else to do it for you.
For those who love diving deep into the science, you can explore A comprehensive list of supporting research that supports these techniques.
Applying mobilizations with movement for Shoulder Pain
Your shoulder is an incredible joint - it can move in more directions than almost any other joint in your body. But when something goes wrong, that same complexity can make shoulder problems particularly frustrating. Simple tasks like reaching into a high cabinet or putting on a shirt can become painful reminders of what you've lost.
Shoulder impingement syndrome is one of the most common culprits behind shoulder pain. It feels like something is getting pinched or squeezed inside your shoulder every time you lift your arm. With mobilizations with movement, we apply a gentle lateral glide to your upper arm bone while you perform the exact movement that usually causes pain. It's like creating a little extra space in a crowded elevator - suddenly everything moves smoothly again.
Frozen shoulder, or adhesive capsulitis, presents a different challenge. Your shoulder capsule becomes thick and tight, making even small movements feel like you're fighting against invisible restraints. MWM techniques help us gently coax your shoulder back to life, particularly improving flexion and abduction - those crucial movements that let you reach forward and out to the side.
The change can be dramatic. I've watched patients walk into our clinic barely able to lift their arm to shoulder height, then leave the same day reaching overhead pain-free. It never gets old seeing that look of amazement on someone's face when they realize their shoulder works again.

At Evolve Physical Therapy, we've helped hundreds of people reclaim their shoulder function. Learn more about our specialized approach with Physical Therapy for Shoulder Pain and find How does mobilization with movement improve shoulder flexion.
A Solution for Tennis Elbow (Lateral Epicondylitis)
Don't let the name fool you - you don't need to play tennis to get tennis elbow. This frustrating condition, officially called lateral epicondylitis, can strike anyone who uses their hands and arms repetitively. Office workers, gardeners, painters, and yes, tennis players all know the distinctive ache along the outside of their elbow.
The real kicker with tennis elbow is how it affects your grip strength. Suddenly, simple tasks like opening a jar or shaking hands become painful reminders of your condition. You might find yourself avoiding certain movements altogether, which only makes things worse over time.
Here's where mobilizations with movement truly shines. We apply a specific lateral glide of the ulna - that's one of your forearm bones - while you actively grip or extend your wrist. The combination of our gentle guidance and your active movement often produces immediate pain relief that seems almost magical.
I've had patients who couldn't shake my hand without grimacing at the start of a session, then grip firmly and pain-free by the end. The technique works by correcting the subtle tracking problems in your elbow joint that develop with repetitive stress. It's like realigning the wheels on your car - suddenly everything runs smoothly again.
The beauty of this approach is that we can often teach you a modified version to use at home, helping you maintain those gains between sessions. It puts you back in control of your recovery.
If elbow pain is limiting your daily activities, we're here to help. Explore our comprehensive Physical Therapy for Elbow Pain services.
Easing Wrist, Hand, and Ankle Issues
Sometimes the smallest joints cause the biggest problems. Your wrists, hands, and ankles might be compact, but when they're not working properly, they can turn everyday activities into major challenges. Fortunately, mobilizations with movement works beautifully on these intricate joints too.
Carpal tunnel syndrome affects millions of people, causing that distinctive numbness, tingling, and pain in your hand and fingers. Traditional treatments often focus on rest and splinting, but MWM takes a different approach. We apply gentle glides to your wrist bones while you perform movements that typically trigger your symptoms. This helps improve median nerve mobility and reduces the compression that's causing your problems.
The results can be remarkable. Patients often notice their fingers feel more normal and their grip becomes stronger within just a few sessions. It's incredibly rewarding to see someone regain the ability to type comfortably or sleep through the night without waking up with numb hands.
Wrist pain from other causes responds well too. Whether you're dealing with a old injury that never quite healed right or developing stiffness from repetitive work, MWM can help restore that smooth, pain-free movement you've been missing.
Don't overlook your ankles either. These hardworking joints take a beating every day, supporting your entire body weight with each step. Ankle sprains are incredibly common, but the stiffness that lingers afterward doesn't have to be permanent. MWM techniques can quickly restore lost motion and get you walking, running, or dancing without that nagging stiffness. For comprehensive ankle and foot care, visit our Physical Therapy for Ankle Pain page.
The MWM Toolkit: Understanding SNAGs and NAGs
When it comes to spinal problems, mobilizations with movement takes on a special form through two powerful techniques: SNAGs and NAGs. These approaches are specifically designed for your spine and can work wonders for neck pain, back stiffness, and even those stubborn headaches that seem to come from nowhere.
Your spine is incredibly complex - it's not just one joint, but dozens working together. When even one segment isn't moving quite right, it can throw off your entire system. That's where SNAGs and NAGs come in. They help us address these spinal hiccups with the same pain-free philosophy that makes all mobilizations with movement so effective.
What makes spinal MWM techniques particularly exciting is their ability to tackle problems that often leave people feeling frustrated. You know that nagging neck pain that flares up when you turn to check your blind spot? Or that morning stiffness that makes getting out of bed feel like you're 90 years old? SNAGs and NAGs can often provide immediate relief for these exact issues.

What are SNAGs (Sustained Natural Apophyseal Glides)?
Think of SNAGs as the "active partner" in spinal mobilizations with movement. The name might sound technical, but the concept is beautifully simple: we apply a sustained glide to a specific spinal segment while you actively move in a way that was previously painful or restricted.
Here's how it works in real life. Let's say you can't turn your head to the right without sharp pain - maybe it happened after sleeping funny or sitting at your computer too long. During a SNAG, I'll place my hands on a specific vertebra in your neck and apply a gentle, sustained pressure in just the right direction. While I maintain that pressure, you slowly turn your head to the right.
The magic happens when that painful movement suddenly becomes pain-free. It's like we've found the perfect key to open up your stuck joint. This technique is particularly effective because it happens in weight-bearing positions - meaning you're sitting or standing normally, which helps your body learn the corrected movement pattern for real-world activities.
SNAGs work beautifully for restoring spinal mobility in all regions of your spine. Whether it's neck rotation, looking up at the ceiling, or bending forward to tie your shoes, SNAGs can often restore these movements instantly and comfortably.
One of my favorite applications is for headaches that originate from the upper neck. These cervical headaches often respond dramatically to the right SNAG technique. I've seen patients walk in with splitting headaches and leave completely pain-free after just one session.
If you're struggling with persistent neck or back pain, our specialized approach can make all the difference. Learn more about our Physical Therapy for Neck Pain and Physical Therapy for Back Pain services.
What are NAGs (Natural Apophyseal Glides)?
While SNAGs are all about sustained pressure during active movement, NAGs take a different approach. These are oscillatory mobilizations - think of them as gentle, rhythmic waves of movement applied to your spinal joints.
NAGs work primarily on the neck and upper back, and they're particularly good at addressing that general stiffness and achiness that doesn't have one specific painful movement. Instead of the sustained pressure of a SNAG, we apply rhythmic, repetitive glides to the spinal segment in mid-to-end range positions.
These techniques are usually performed while you're lying down in non-weight-bearing positions, making them perfect for when movement is too uncomfortable or when we need to focus on reducing pain and stiffness before progressing to more active techniques.
The gentle oscillations work by stimulating the nerve receptors in your joints, which can help block pain signals and improve how your tissues move. It's like giving your spine a gentle massage from the inside out. While NAGs still follow our pain-free principles, they're often the technique of choice when you're dealing with more diffuse discomfort rather than sharp, movement-specific pain.
Both SNAGs and NAGs are powerful tools in our toolkit, and the beauty is that we can often teach you modified versions to use at home. This means you're not dependent on coming to the clinic every time your symptoms flare up - you have the power to maintain your progress independently.
Frequently Asked Questions about Mobilizations with Movement
When patients first hear about mobilizations with movement, they naturally have questions. After nearly two decades of using these techniques, I've found that understanding what to expect makes the experience much more comfortable and effective. Let me address the most common concerns we hear at Evolve Physical Therapy.
Is Mobilization with Movement painful?
This is the question I hear most often, and I'm always excited to answer it: absolutely not! The beauty of mobilizations with movement lies in its core principle - if it hurts, we're not doing it right.
Pain-free movement is the foundation of everything we do with MWM. When I apply a mobilization glide to your joint, you should feel immediate relief, not discomfort. If you experience any pain during the technique, it tells me we haven't found the correct angle or direction of glide yet, or perhaps MWM isn't the right approach for your specific issue.
I constantly communicate with my patients during treatment. "How does that feel?" and "Any pain with that movement?" are questions you'll hear repeatedly. Your feedback guides everything I do. The absence of pain isn't just nice to have - it's our primary indicator that the technique is working correctly.
This approach is completely different from the "no pain, no gain" mentality you might expect. We're not working through pain; we're eliminating it entirely while you move.
How quickly will I see results from MWM?
Here's where mobilizations with movement truly shines - the results are often instantaneous. The "I" in our PILL principle stands for "Instant," and that's exactly what we aim for in every session.
I've had patients walk into my clinic barely able to lift their arm overhead due to shoulder pain, and within minutes of applying the right MWM technique, they're reaching toward the ceiling with a huge smile on their face. It's one of the most rewarding aspects of what I do.
You should notice an immediate improvement in your range of motion during the first application. If we don't see that instant change, we adjust our approach until we find what works for your specific joint dysfunction. The goal isn't just temporary relief either - these improvements should persist after I remove my hands from your joint.
While dramatic changes often happen in the first session, most patients benefit from a series of treatments to fully resolve the underlying issue and learn self-treatment techniques to maintain their progress at home.
Who is qualified to perform Mobilizations with Movement?
This is a crucial question for your safety and treatment success. Mobilizations with movement requires specialized training beyond basic physical therapy education. Not every therapist is qualified to perform these techniques safely and effectively.
At Evolve Physical Therapy, our licensed physical therapists have completed advanced manual therapy training, including specific education in the Mulligan Concept. This specialized knowledge is essential because MWM isn't just about applying pressure - it requires a deep understanding of joint biomechanics, anatomy, and the ability to assess exactly where and how each joint needs to be guided.
Proper assessment comes first. We need to identify potential "positional faults" in your joints and determine whether MWM is appropriate for your specific condition. The precision required to find the exact angle and direction of mobilization that eliminates your pain takes years of training and practice to master.
Our expertise allows us to recognize immediately when a technique is working and when we need to try a different approach. This knowledge and experience ensures you get the safest, most effective treatment possible.
Conclusion
When you're struggling with joint pain or movement restrictions, mobilizations with movement offers something truly special – a path back to pain-free function that feels almost magical in its simplicity. This remarkable approach doesn't just mask your symptoms; it addresses the root cause by gently correcting those subtle "positional faults" that can turn everyday movements into painful ordeals.
What makes MWM so powerful is how it empowers you to take an active role in your recovery. Instead of lying passively while treatment happens to you, you become a partner in the healing process. You move while we guide your joints back to their happy place – and the results speak for themselves.
The pain-free restoration of function isn't just a nice idea; it's the fundamental promise of this technique. When we see patients walk in unable to lift their arm overhead or grip a coffee cup without wincing, then watch them perform these movements effortlessly just minutes later, it never gets old. These aren't temporary fixes either – the long-lasting results mean you can return to your daily activities with confidence.
Perhaps most importantly, MWM teaches you self-treatment techniques that put the power of healing literally in your own hands. You'll learn how to maintain your progress and even prevent future flare-ups, giving you tools that last a lifetime.
At Evolve Physical Therapy + Sports Rehabilitation, our skilled therapists have mastered these advanced mobilizations with movement techniques through years of specialized training and hands-on experience. We've witnessed countless "impossible" cases turn around, from frozen shoulders that suddenly move freely to tennis elbows that stop aching overnight.
Our approach goes beyond just applying techniques – we believe in truly understanding your unique situation and creating a treatment plan that makes sense for your life. Whether you're dealing with a nagging shoulder issue, stubborn elbow pain, or chronic neck stiffness, we're here to help you move better and live pain-free.
Ready to experience what it feels like when your joints work the way they're supposed to? Learn more about our physical therapy services and find how mobilizations with movement can transform your relationship with movement itself.
Awkward Postures at Work? Here's Your Ergonomic Survival Guide
Why Your Body Is Screaming for Better Workplace Ergonomics

Awkward posture ergonomics is the science of designing work environments to minimize harmful body positions and reduce the risk of musculoskeletal disorders. Here's what you need to know:
- Neutral posture: The body is positioned with minimal strain.
- Awkward posture: Any deviation from neutral, like bending or twisting.
- Key risks: Muscle fatigue, reduced force, and compressed nerves.
- Prevention: Ergonomic tools, proper workstation design, and regular breaks.
- Assessment methods: REBA and OWAS evaluation systems.
If you've ever felt neck ache from hunching over a computer or back pain from lifting boxes, you've experienced the effects of awkward postures. These aren't minor inconveniences; they're warning signs of potential injury.
Statistics show that more than half of all workers have neck problems, 30% suffer from shoulder tension, and 26% experience wrist and arm pain. Awkward postures are a leading cause of sick leave and workplace absenteeism.
An "awkward" posture forces your body from its natural alignment, making muscles work harder and less efficiently. This leads to faster fatigue and stress on your joints, tendons, and nerves.
The path to chronic injury often starts with pain during work that vanishes with rest (Stage 1). It progresses to symptoms that persist after work, disrupting sleep (Stage 2), and can end in constant, debilitating pain that impacts your quality of life (Stage 3).
As the founder of Evolve Physical Therapy, I've seen how proper awkward posture ergonomics can prevent these injuries. My approach combines manual therapy with workplace modifications to address both symptoms and root causes.
Defining Awkward Postures vs. Neutral Alignment
Understanding the difference between neutral and awkward postures is the foundation of awkward posture ergonomics. It can mean the difference between ending your workday energized or exhausted.
What is a Neutral Posture?
Neutral posture is when your body parts are positioned at their natural, mid-range of motion with minimal strain. Your muscles are at their resting length, joints are aligned, and no conscious effort is needed to hold the position. In neutral alignment, your muscles work with maximum efficiency. Your proper alignment of the spine maintains its natural curves, distributing weight evenly and minimizing stress.
This is why good posture for office workers is so important. A workstation that supports a neutral position allows you to work longer with less fatigue because your muscles aren't fighting gravity or awkward angles.
What Makes a Posture "Awkward"?
Awkward postures are positions that force your body away from its neutral alignment. This includes bending, twisting, reaching far from your body, squatting for extended periods, or kneeling. When a joint is pushed toward the end of its range of motion, you've entered awkward territory.
In these positions, your muscles must work much harder, leading to inefficiency and exhaustion. Static postures—holding any position for too long—are also problematic. They cause muscle fatigue, decrease blood flow, and can lead to compressed nerves and tendons sending pain signals.
The result is increased exertion, faster fatigue, and discomfort. Unfortunately, many of us develop habits that lead to bad office posture without realizing it. Understanding these concepts is the first step toward creating a healthier work environment. Listening to your body's signals puts you in control of your long-term health.
The High Cost of Poor Posture: Health Risks and MSDs
That nagging neck pain or shoulder tension isn't just an annoyance; it's your body signaling that something needs to change.

Musculoskeletal disorders (MSDs), which affect muscles, bones, and nerves, are among the most common workplace injuries, with poor awkward posture ergonomics as a major cause. Over half of all workers deal with neck problems, 30% have shoulder tension, and 26% experience wrist and arm pain. The economic impact is also staggering, with awkward postures causing significant sick leave, lost productivity, and healthcare costs.
Continuous exposure to awkward postures can lead to fatigue failure in the spine, causing chronic pain. This is why we focus on treatments like physical therapy for back pain Brooklyn and physical therapy for neck pain Brooklyn. Research confirms that good posture is key to the reduction of musculoskeletal disorders.
Key Risk Factors for Injury
Understanding risk factors helps you take action before an injury occurs.
- Duration: The longer you hold an awkward position, the more strain it places on your tissues. Static postures are especially harmful as they restrict blood flow.
- Frequency: Repeating an awkward position, even briefly, creates cumulative trauma as your body doesn't have time to recover.
- Degree of deviation from neutral: The further you move from your body's natural alignment, the harder your muscles must work.
- Forceful exertions: Combining an awkward posture with lifting or pushing creates a perfect storm for injury, as muscles can't generate force efficiently.
- Static loading: Maintaining muscle contractions for long periods without relaxation leads to rapid fatigue.
- Repetitive motions: Performing the same motions in an awkward position can lead to overuse injuries like tendinitis.
The Three Stages of Musculoskeletal Injury
Most workplace injuries develop gradually through three stages. Recognizing them is key to preventing chronic disability.
- Stage 1: Pain and fatigue appear during work but disappear with rest. It's easy to dismiss these early warning signs, but your body is asking for attention.
- Stage 2: Symptoms persist after work, disturbing sleep and reducing your work capacity. The problem is getting worse.
- Stage 3: Pain becomes chronic and persistent, significantly impacting your quality of life and daily activities.
The progression through these stages in the development of injuries isn't inevitable. Intervention in Stage 1 or early Stage 2, through ergonomic changes and physical therapy for posture training, can prevent chronic pain. Listen to your body's early signals; pain is valuable information.
Proactive Prevention: Your Guide to Awkward Posture Ergonomics
Most health risks from poor posture are preventable. With the right approach to awkward posture ergonomics, you can transform your workspace and habits to protect your body. It's about working smarter, not harder, by redesigning how you work to support your body's natural alignment. Our approach to physical therapy for posture training emphasizes prevention alongside treatment.

The Hierarchy of Ergonomic Controls
Ergonomics experts use a hierarchy of controls to tackle awkward postures, prioritizing the most effective solutions first.
- Elimination: The most effective solution. Can you completely avoid the awkward posture, such as by storing items at waist height instead of on the floor?
- Substitution: If elimination isn't possible, swap out tools or change processes. Use a headset instead of cradling a phone.
- Engineering controls: Modify the physical environment with adjustable desks, ergonomic chairs, and monitor arms.
- Administrative controls: Change how work is done through job rotation, mandatory breaks, and training on proper body mechanics.
- Personal Protective Equipment (PPE): Items like knee pads can provide cushioning but don't eliminate the awkward posture. They are best used with higher-level controls.
Recommended Time Limits for Awkward Postures
Even with a good workspace, some awkward postures may be unavoidable. Knowing your limits is crucial. Prolonged exposure is what causes problems.
Research suggests limiting certain postures to about 2 hours total per shift. This includes:
- Neck bent more than 30 degrees
- Back bent more than 30 degrees
- Working with hands above your head or elbows above shoulders
- Kneeling
Squatting should be limited as much as possible due to the stress on the knees and back. These limits are based on research into tissue breakdown. The key is variety and movement. Take regular breaks, change positions, and listen to your body's signals.
Designing a Safer Workspace: Practical Ergonomic Solutions
Creating a workspace that supports your body's natural alignment is practical and simple with awkward posture ergonomics. Your workspace should adapt to you, not the other way around. This is crucial for both office settings and when dealing with home office ergonomics or achieving correct computer posture.
Common Awkward Postures and How to Fix Them
Let's tackle common positions that gradually wear down your body.
- Working overhead: This strains your neck and shoulders. The fix: Use step stools, ladders, or tool extenders to bring your body to the work.
- Bending forward: Compresses your spine and overworks back muscles. The fix: Raise the work surface using adjustable-height desks, lifting devices, or proper monitor positioning.
- Reaching and over-reaching: Creates cumulative strain. The fix: Rearrange your workspace to keep frequently used items within arm's length.
- Twisting your torso: Happens with poor workspace layout. The fix: Turn your whole body to face what you need. Ensure your chair swivels easily.
- Kneeling and squatting: Strains knees and back. The fix: Use comfortable knee pads, adjustable stools, or lifting aids.
- Forward head posture ("tech neck"): Caused by craning your neck toward screens. The fix: Bring screens to eye level. Hold handheld devices higher.
- Bent wrists: Caused by poor keyboard and mouse placement. The fix: Keep wrists straight and neutral, with forearms parallel to the floor, by adjusting your chair or using a keyboard tray.
If you're working from home and experiencing back pain, these adjustments can provide immediate relief.
Applying Awkward Posture Ergonomics to Tool Selection
Smart tool selection is a game-changer for maintaining neutral postures.
- Grip Type: Use a power grip (whole hand) for forceful tasks. Reserve pinch grips (thumb and fingers) for light, brief tasks.
- Handle Size and Shape: Handles should fit your hand comfortably. For power grips, a diameter between 1.75 and 3.75 inches is ideal. Contoured, textured handles are best.
- Tool Weight: Heavy tools cause fatigue up the entire arm. Choose lighter tools or those with dual-handle options to distribute weight.
- Adjustable Handles: Tools with adjustable handles (e.g., inline vs. pistol grip) help you maintain a neutral wrist position for different tasks.
- Force Reduction Features: Look for spring-loaded handles, ratcheting mechanisms, or counterbalances to reduce the effort you need to apply.
The goal is to apply effort efficiently, with your body in positions that support strength, not strain.
Taking Action: How to Identify, Assess, and Report Risks
Understanding awkward posture ergonomics is the first step; taking action is next. This requires a collaborative effort to identify, assess, and report ergonomic risks.
Understanding the Basics of Awkward Posture Ergonomics Assessment
Ergonomic assessments provide systematic ways to evaluate tasks and identify hazards.
- Observation: Watching how a job is performed can reveal repeated bending, twisting, or static positions.
- Employee Feedback: Workers are the best source of information on discomfort and strenuous tasks. Encourage them to report issues.
- Checklists: Standardized checklists help identify common risk factors.
- Formal Assessment Methods: For a scientific approach, tools like REBA (Rapid Entire Body Assessment) and OWAS (Ovako Working Analysis System) are used. REBA assesses specific postures to determine MSD risk, while OWAS evaluates a sample of postures over time to assess cumulative load.
These methods help quantify risks objectively, guiding effective solutions. The OSHA website offers resources on how to identify ergonomic problems.
Creating a Collaborative Safety Culture
Effective ergonomics requires a collaborative safety culture where everyone works together.
- Open Communication: Employees should feel empowered to report risks without fear of reprisal through clear reporting channels.
- Employee Training: Educating employees on proper body mechanics, neutral posture, and ergonomic benefits increases awareness and compliance.
- Management Commitment: Employers must commit resources for assessments, implement changes, and provide proper equipment.
- Joint Health and Safety Committees: Committees with both management and employee representatives can oversee ergonomics programs.
- Continuous Improvement: Ergonomics is an ongoing process. Regularly reassess, gather feedback, and adapt solutions for long-term success.
A collaborative spirit creates workplaces that reduce injuries and improve productivity and morale.
Frequently Asked Questions about Awkward Posture Ergonomics
Here are answers to common questions about awkward posture ergonomics based on my experience at Evolve Physical Therapy.
How do I know if my posture is awkward?
An awkward posture forces your joints away from their comfortable, neutral middle ground. Telltale signs include bending your neck, twisting your spine, hunching your shoulders, or reaching far from your body. The real test is to listen to your body. If you feel strain, fatigue, or nagging discomfort, your posture is likely awkward. If a position requires conscious effort or leaves you sore, it's time for a change.
Can stretching during breaks really help?
Yes, absolutely. When you hold static or awkward postures, muscles get tight and blood flow decreases. Frequent, short stretching breaks relieve muscle tension, restore circulation, and reduce fatigue. Even a few minutes of gentle stretching or walking around can reset your body, improve flexibility, and prevent the cumulative strain that leads to injury. Your body needs movement and variety.
Is a standing desk a good solution for awkward postures?
A standing desk can be a fantastic tool against the negative effects of prolonged sitting, but it's not a magic bullet. The key to awkward posture ergonomics is movement and variety, not just finding one "perfect" position. A standing desk is most effective when you maintain a neutral standing posture (ears over shoulders, shoulders over hips) and, most importantly, alternate between sitting and standing throughout the day. Trading eight hours of sitting for eight hours of standing just swaps one static posture for another.
Conclusion
After diving into awkward posture ergonomics, it's clear your body isn't meant to suffer through workdays in uncomfortable positions. The evidence is overwhelming, but the good news is that most of these injuries are preventable. Understanding neutral postures and recognizing early warning signs allows you to take meaningful action. Every ergonomic adjustment is an investment in your long-term health.
The stages of injury are not inevitable; they are warning signs. That afternoon neck ache is your body asking for help. The beauty of awkward posture ergonomics is that small changes—like adjusting your monitor, taking breaks, and using the right tools—yield big results.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach combines manual therapy with practical workplace modifications to address both symptoms and root causes. We help patients reclaim their active lifestyles by taking control of their environment.
Pain shouldn't be your daily companion. Taking a proactive approach to ergonomics can make all the difference. Your body is sending signals; it's time to listen.
Ready to transform how you feel? Find out how personalized ergonomic physical therapy Brooklyn services can help you achieve lasting comfort and peak performance.
Breaking the Pain Cycle – Physical Therapy Strategies for Chronic Pain
Why Physical Therapy for Chronic Pain is Your Path to Recovery

Physical therapy for chronic pain offers a proven, drug-free approach to breaking the cycle of persistent discomfort and reclaiming your active lifestyle. Here's what physical therapy can do for your chronic pain:
Key Benefits:
- Pain reduction through targeted manual therapy and therapeutic exercises
- Improved mobility and strength without relying on medications
- Education about pain science to reduce fear and anxiety around movement
- Personalized treatment plans addressing your specific condition and goals
- Long-term solutions rather than temporary symptom masking
Chronic pain affects nearly 51.6 million Americans, making it the leading cause of disability with an economic impact of over $560 billion annually. But there is hope—chronic pain doesn't have to control your life.
Unlike acute pain (a temporary alarm), chronic pain persists after tissues have healed because the nervous system becomes hypersensitive. Physical therapy excels at retraining your brain and body to break these faulty pain patterns.
Physical therapy addresses chronic pain through a biopsychosocial approach, recognizing that your pain experience involves biological, psychological, and social factors. Rather than simply masking symptoms, skilled physical therapists identify and treat the root causes of your discomfort while teaching you strategies to prevent future flare-ups.
I'm Lou Ezrick, founder of Evolve Physical Therapy. With nearly two decades specializing in physical therapy for chronic pain management, I've helped thousands of patients find lasting relief. My experience with complex cases confirms that with the right approach, recovery is achievable.

Understanding Chronic Pain: More Than Just an Ache
Acute pain is your body's alarm system, like the sharp pain from a burn that fades as you heal. It's a protective signal that typically resolves within 12 weeks.
Chronic pain is different. It's pain that lasts more than three months, persisting long after an injury has healed, as the nervous system continues to send pain signals. As the National Institute of Neurological Disorders and Stroke explains, while acute pain alerts you to injury, "chronic pain persists. Pain signals keep firing in the nervous system long after the injury has healed."
For example, ankle sprain pain that lasts six months instead of a few weeks is chronic pain, even if the original injury has healed completely.
This persistence is often due to central sensitization, where the nervous system's 'volume control' gets stuck on high. Your brain and spinal cord become hypersensitive, turning normal sensations like a gentle touch into pain.
The brain's role in pain is complex. Your brain actively creates your pain experience based on factors like past experiences, emotions, and stress. This is why stress can often worsen pain.
This is why we use the biopsychosocial model in physical therapy for chronic pain. We consider the biological (tissues), psychological (thoughts, emotions), and social (work, relationships) factors contributing to your pain. For instance, a person with chronic back pain may also have a fear of movement and anxiety about work, all of which are part of their pain experience.
Common Causes and Conditions
Chronic pain can develop from various sources, and understanding your specific situation helps us create the right treatment approach.
Previous injuries are common culprits. If an injury like a sprain or post-surgical recovery isn't fully rehabilitated, the nervous system can remain sensitized, turning acute pain into a chronic problem.
Arthritis affects millions with ongoing joint pain from inflammation and wear-and-tear. Physical therapy is proven to help people with osteoarthritis or rheumatoid arthritis improve movement and reduce pain. More info about Physical Therapy for Arthritis.
Fibromyalgia creates widespread pain, fatigue, and amplified pain signals in the brain. Our gentle, educational approach helps patients gradually and safely increase their activity levels. More info about Physical Therapy for Fibromyalgia.
Neuropathic pain results from nerve damage and creates sensations like burning, tingling, or shooting pain. Conditions like sciatica or diabetic neuropathy fall into this category.
Back and neck issues are among the most common chronic pain conditions we treat. Chronic low back pain was identified as the single greatest cause of "years lived with disability" worldwide, making effective treatment crucial.
How Chronic Pain Impacts Your Life
Living with chronic pain touches every corner of your life.
Physical effects create a frustrating cycle. Pain makes you move less, leading to deconditioning (weaker muscles, stiffer joints). This unfortunately can make you more susceptible to pain.
The emotional toll is immense, with about 67% of people with chronic pain also struggling with anxiety and depression. It's exhausting to hurt every day, and it's understandable to feel hopeless or irritable.
Social withdrawal often follows. You might cancel plans or avoid activities for fear of worsening the pain. This isolation can increase feelings of depression and anxiety.
The impact on work and daily activities can be devastating. Chronic pain is a leading cause of disability, affecting your ability to work, care for your home, or enjoy hobbies. According to a CDC study, over 20% of U.S. adults experience these challenges.
Physical therapy for chronic pain addresses all these impacts, helping you break the pain cycle and regain your life.
The Role of Physical Therapy for Chronic Pain
At Evolve Physical Therapy, we empower you to take control of your pain. Our approach to physical therapy for chronic pain begins with a comprehensive initial evaluation to understand not just where it hurts, but why.
During this diagnostic process, we'll discuss your history and daily routines, then perform a hands-on assessment of your posture, flexibility, and movement to find imbalances contributing to your pain. Unlike imaging like MRIs (which often show abnormalities in pain-free people), our evaluation focuses on your functional movement.
Together, we'll set functional goals that matter to you, whether it's sleeping through the night or hiking again. Your goals drive your treatment plan.
A powerful benefit of physical therapy is reducing your reliance on medication. By addressing root causes and teaching self-management strategies, we help you need fewer pain medications, avoiding their potential side effects and dependency risks.
Our ultimate goal is a genuine improvement in your quality of life. We want to help you reclaim the activities, relationships, and experiences that chronic pain may have stolen from you.

Goals of Physical Therapy for Chronic Pain
We partner with you to achieve several interconnected goals for lasting change.
Pain reduction is a primary goal. We use various techniques to calm overactive pain signals and provide significant relief.
Improved mobility follows as pain decreases. We work to restore fluid, easy movement in your joints and muscles.
Building increased strength and endurance is crucial. We safely help you rebuild physical capacity so daily activities become less taxing.
Restored function means getting back to what matters most, like playing with your grandchildren or working without constant discomfort.
We foster patient independence by teaching you to become your own best therapist, understanding your body and knowing how to manage flare-ups.
Finally, we focus on preventing future pain episodes. By correcting underlying issues and teaching proper body mechanics, we help break the cycle of recurring pain.
Key Interventions and Techniques
Our physical therapy for chronic pain toolkit includes a variety of evidence-based treatments personalized for you.
Manual therapy is a cornerstone of our approach. These hands-on techniques, including skilled joint mobilization and soft tissue massage, restore movement and release tension. This therapeutic touch helps retrain the nervous system's response to sensation. Research on manual physical therapy for chronic pain
Therapeutic exercise is medicine for chronic pain. We use graded exposure, starting with comfortable movements and gradually progressing. This desensitizes your nervous system and helps you overcome the fear of movement.
Our strengthening and flexibility programs blend low-impact cardio with targeted strengthening and stretching to address your specific needs. For those with back issues, these exercises can be life-changing. More info about Physical Therapy for Back Pain Brooklyn
We may also use modalities as supportive treatments. TENS units can help block pain signals, while heat and ice therapy relax muscles and reduce inflammation.
The key to our success is combining these approaches into a personalized treatment plan that evolves as you progress.
Your Partnership in Healing: Education and Active Participation
True healing from chronic pain is a partnership. We build a strong therapeutic alliance with you, based on trust and shared decision-making, where your goals and preferences shape your treatment plan. This collaboration is a powerful predictor of successful outcomes [Ferreira et al. 2013, Therapeutic alliance].
Your active role is paramount. Physical therapy for chronic pain is a process you actively participate in. Consistency with your home exercise programs is crucial for progress. Think of us as your coaches; we provide the roadmap and tools, but you're in the driver's seat.

Pain Neuroscience Education (PNE)
Pain Neuroscience Education (PNE) is a transformative tool where we teach you the biology of pain. Understanding that "pain does not always mean harm" is a crucial first step [Physiopedia]. Learning how your brain produces pain helps reduce fear of movement. This knowledge empowers you to re-engage in activities and change pain beliefs from "my body is broken" to "my nervous system is overprotective, and I can retrain it." PNE is a cornerstone of our approach to pain management and can greatly improve manual therapy effects Louw et al. 2017, A clinical perspective on a pain neuroscience education approach. More info about Pain Management in Brooklyn NY.
Behavioral Strategies for Managing Pain
We also equip you with behavioral strategies to gain control over your pain experience:
- Pacing Activities: Learn to balance activity and rest to avoid the "boom-bust" cycle. We teach you to break down tasks and take regular breaks to prevent pain flares.
- Goal Setting: We help you set realistic short-term and long-term goals, providing motivation and a clear path to recovery.
- Relaxation Techniques: Techniques like diaphragmatic breathing and progressive muscle relaxation help calm your nervous system and reduce muscle tension.
- Mindfulness: Mindfulness practices can help you observe pain without judgment, reducing the emotional distress associated with it and improving coping Hill et al. 2017, Changes in psychosocial well-being after mindfulness-based stress reduction.
- Improving Sleep Hygiene: We provide strategies to improve your sleep habits, as restorative rest is crucial for pain management.
- Stress Management: Since stress amplifies pain, we explore coping strategies to help you manage life's challenges without triggering flare-ups.
Integrating these strategies empowers you to become an active manager of your own pain, leading to greater independence and a better quality of life.
Advanced and Integrated Approaches to Pain Management
The best results in physical therapy for chronic pain come from a team approach. Each professional brings unique expertise to tackle different aspects of your pain.
At Evolve Physical Therapy, we regularly engage in collaboration with doctors and psychologists. This multidisciplinary care ensures we're addressing the physical, emotional, and social factors of your pain, not just the symptoms.
One of our most important roles is preventing the transition from acute to chronic pain. Early intervention with physical therapy can stop pain from becoming a long-term problem. By teaching proper movement and addressing fears about activity, we can interrupt the cycle that leads to chronic pain.
The shift in how we treat chronic pain represents a major breakthrough. We've moved from a purely biomedical model to a more effective biopsychosocial one.
| Feature | Biomedical Approach (Outdated) | Biopsychosocial Approach (Modern & Comprehensive) |
|---|---|---|
| View of Pain | Primarily a direct result of tissue damage or structural issue. | A complex experience influenced by biological, psychological, and social factors. |
| Focus of Treatment | Fixing the "problem" tissue; symptom suppression (e.g., surgery, medication). | Restoring function, reducing sensitivity, empowering self-management. |
| Patient Role | Passive recipient of treatment. | Active participant in their recovery. |
| Key Interventions | Medication, injections, surgery, passive modalities. | Exercise, education, manual therapy, psychological strategies, lifestyle changes. |
| Understanding of Healing | Pain resolves when tissue heals. | Pain can persist even after tissue healing; involves nervous system changes. |
This modern approach recognizes that you are an active participant in your recovery, and we are here to guide and support you.
The Impact of Technology in Physical Therapy
Technology is revolutionizing physical therapy for chronic pain, making treatment more accessible and effective.
Telehealth appointments offer incredible flexibility, eliminating travel stress and allowing us to see how you move in your own environment. This is particularly valuable for our patients with mobility challenges. More info about Physical Therapy for Neurological Disorders.
Virtual Reality (VR) for pain distraction is a powerful tool for pain management. By immersing you in a virtual world during exercises, it can redirect your brain's attention away from pain signals.
Wearable technology and app-based exercise programs help us track your activity, sleep, and response to exercises between visits. This data allows us to fine-tune your treatment plan and celebrate your progress.
Technology improves our partnership, empowering you to manage your pain while strengthening the crucial human connection in your healing journey.
Frequently Asked Questions about Chronic Pain and PT
We understand you have questions about chronic pain. Here are some honest, reassuring answers based on our experience.
How is chronic pain diagnosed by a physical therapist?
A physical therapist diagnoses chronic pain through a thorough evaluation. We start by listening to your story—your health history, the nature of your pain, and how it affects your daily life, sleep, and mood. Next, a physical exam assesses your strength and movement to identify patterns or imbalances contributing to your pain. These functional findings are often more revealing than an MRI. We don't rely heavily on imaging; instead, detailed questions about your symptoms and our physical assessment guide us to the factors crucial for your recovery.
Will physical therapy hurt?
This is a valid concern. The goal of physical therapy is to work within your comfort levels to reduce pain, not cause it. You might feel mild muscle soreness after some exercises—similar to after a good workout—but this is productive soreness, not harmful pain. We'll teach you the difference. We start slowly and progress gradually, never pushing you into sharp pain. Constant communication with your therapist is key. We are your partners in movement, and our goal is to build your confidence, not fear.
How long will I need physical therapy?
The duration varies for each individual based on their condition, the severity of the pain, and their personal goals. After your initial evaluation, your therapist will create a customized plan and timeline. Some patients feel better in a few weeks, while those with more complex conditions may need several months. Our ultimate goal is to empower you with self-management strategies. As you progress, you'll learn to handle flare-ups independently, and your visit frequency will decrease. The tools you gain will last a lifetime.
Take Control of Your Pain and Reclaim Your Life
I know how overwhelming chronic pain can be, making you feel trapped in your own body. But you have more power than you realize.
Physical therapy for chronic pain is about empowerment through movement and education. By understanding your pain and learning to retrain your body's responses, you become an active participant in your recovery.
I've watched thousands of patients reduce their pain levels, improve their mobility, and return to activities they thought were lost forever. These victories, big and small, are what matter.
Our approach is personalized, not cookie-cutter. We create personalized treatment plans that address your specific goals and work with your body's natural healing ability.
The importance of seeking expert care cannot be overstated. Chronic pain is complex, and you deserve guidance from professionals who understand the intricate relationship between your nervous system, movement, and pain experience.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach is designed to help you break the pain cycle and return to the activities you love. We combine evidence-based treatments with genuine care, giving you the tools and confidence for long-term success.
Your journey to better pain management starts with a single step. Relief is possible, and we're here to help you find it.
Begin your journey to a pain-free life with our physical therapy services.
Mobility Movement Training: Unlock Your Body's Potential
Why Your Body Needs More Than Just Flexibility
Mobility movement training is actively moving your joints through their full range of motion with strength and control. It combines flexibility, stability, and coordination to improve how your body functions daily.
What Mobility Movement Training Includes:
- Active range of motion - moving joints under your own muscle power
- Dynamic stretching - controlled movements that prepare muscles for activity
- Strength through range - building stability at different joint positions
- Functional patterns - movements that translate to real-world activities
- Joint health focus - keeping joints lubricated and properly aligned
Waking up stiff and tight is a sign your body needs more than occasional stretching—it needs mobility movement training.
Unlike passive stretching, mobility training challenges you to control your body through movement. Research shows that better mobility scores correlate with a six times lower injury risk. It's not just about touching your toes; it's about moving well in all directions.
As we age, joints can become stiff and our range of motion can decrease. The good news is that mobility movement training can combat these effects, helping you move with confidence.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience. I've seen how mobility movement training is the foundation for pain-free movement and long-term joint health for everyone from trauma victims to active professionals.
Mobility vs. Flexibility: Understanding the Key Difference
Imagine someone who can easily pull their leg to their ear but stumbles when trying to kick a ball. That's the difference between flexibility and mobility movement training in action.
Most people confuse the two, but they are quite different. Flexibility is passive—it's how far your muscles can stretch with assistance, like holding a toe touch. Mobility movement training, on the other hand, is active—it's the ability to move through that range of motion with your own strength and control.
Here's how they stack up against each other:
| Feature | Mobility | Flexibility |
|---|---|---|
| Movement Type | Active (requires muscle engagement) | Passive (often assisted or static) |
| Focus | Joint health, control, stability, strength | Muscle lengthening, tissue extensibility |
| Primary Goal | How well you can move through a full range | How far you can stretch or be stretched |
| Application | Functional movements, athletic performance | Reaching passive end ranges, relaxation |
The key difference is that mobility is active, while flexibility is passive. Mobility requires your muscles, joints, and nervous system to work together in a coordinated effort.
What is Mobility Movement Training?
Mobility movement training takes a whole-body approach, teaching your muscles, joints, and nervous system to work together smoothly. It improves coordination and your body's awareness of its position in space.
This training focuses on real-life movement patterns like squatting, reaching, and twisting. These are life skills, not just gym exercises. At Evolve Physical Therapy, we see how this integrated approach helps people move more efficiently. For more insight, check out our article on the Difference Between Mobility and Movement.
Why Flexibility Isn't Enough
Ever wonder why you can touch your toes but still feel stiff or get injured? The problem is that passive flexibility alone doesn't prepare your body for active movement.
If your muscles aren't strong through their full range, your body compensates. For example, a lack of hamstring control can lead to an overworked lower back or tight hips, causing nagging pain.
Mobility movement training builds strength and control within your available range. It's the difference between passively doing the splits and actively kicking a soccer ball—one requires control, the other doesn't. Dancers and gymnasts don't just stretch; they practice controlled movements. They need both strength and control, which is what mobility movement training brings to everyday life.
The Core Benefits of Mobility Movement Training
Imagine waking up without stiffness, reaching for a high shelf without wincing, or tying your shoes with ease. These are the real-world benefits that mobility movement training delivers.

You'll quickly notice reduced pain and stiffness and improved posture. Mobility work addresses daily discomforts by teaching your joints to move freely with proper muscle support.
For regular exercisers, mobility training transforms workouts by improving efficiency, balance, and agility. Crucially, it reduces injury risk. Research shows that better mobility scores correlate with a six times lower likelihood of injury. The long-term benefits are an investment in longevity and quality of life, paving the way for decades of pain-free activity.
Injury Prevention and Improved Performance
Most injuries occur not where you feel tight, but where your body compensates. A stiff mid-back can lead to an overworked lower back; restricted hips can strain your knees.
Mobility movement training breaks this compensation cycle by ensuring each joint does its part, leading to improved movement efficiency. It's the ultimate warm-up, preparing your body for workouts by increasing blood flow, activating the nervous system, and lubricating joints.
This preparation significantly decreases overuse injuries because no single area is overwhelmed. Paired with practices like Dynamic Balance Training, it's your best defense against common injuries. Better mobility also means deeper squats and effortless overhead movements, making your workouts more effective.
Better Daily Life and Healthy Aging
Aging and modern lifestyles—like hours of sitting—naturally lead to stiffer, achier bodies. The empowering truth is that mobility movement training can slow or even reverse many of these changes.
It combats the effects of sitting by restoring hip flexibility and postural strength, and it eases everyday tasks like reaching or dressing, ensuring these activities remain natural and joyful.
The National Institute on Aging confirms that maintaining mobility is key to living independently as we age. Mobility training directly supports this by keeping you capable and confident. It's never too late to start. By mitigating age-related stiffness, you invest in an active future and the independence to live life on your terms.
Essential Mobility Exercises for the Whole Body
Ready to move better? The beauty of mobility movement training is its simplicity. These exercises target common problem areas to build a foundation for fluid, pain-free movement. Think of them as daily maintenance for your joints. For more ideas, see our guide to the Best Mobility Movements.
Hip Mobility Exercises
Tight hips can cause lower back and knee pain. These exercises help restore mobility.

- 90/90 Hip Switch: Seated with knees bent at 90 degrees (one forward, one to the side), keep your back straight and smoothly switch your legs to the opposite side. This improves internal and external hip rotation.
- Spider Lunge: From a plank, step one foot outside your hand. Keep the back leg straight or drop the knee to the ground. This opens tight hip flexors.
- Cossack Squats: Stand with feet wide apart. Shift your weight to one side, bending that knee into a squat while keeping the other leg straight.
- Seated Figure-4 Stretch: Sit with knees bent, cross one ankle over the opposite knee, and gently pull the bottom knee toward your chest to target deep hip rotators.
For a deeper dive, check out our guide on Hip Mobility Movements.
Spine and Back Mobility Exercises
Our spines are meant to move in all directions, but modern life makes them stiff. These exercises help restore that motion.

- Cat-Cow: On your hands and knees, alternate between arching your back (cow) and rounding it (cat) to warm up the spine and counteract sitting.
- Thoracic Rotations (Open Books): Lie on your side with knees bent. Slowly open your top arm like a book, allowing your upper back to rotate. This targets mid-back stiffness.
- World's Greatest Stretch: From a lunge, this stretch combines hip mobility, thoracic rotation, and a hamstring stretch, making it a highly efficient movement.
- Lumbar Windshield Wipers: Lie on your back with knees bent and gently drop them from side to side. This soothes the lower back and maintains rotational mobility.
These movements complement the approach we use in Therapeutic Exercise Brooklyn to restore healthy spinal function.
Shoulder and Ankle Mobility
Shoulder and ankle mobility are crucial. Stiff shoulders can cause neck pain, while tight ankles affect your entire movement chain.

- Shoulder CARs (Controlled Articular Rotations): Stand tall and slowly make the largest possible circle with one arm, keeping your body still. This teaches controlled shoulder movement.
- Dead Hangs: Hang from a pull-up bar for 10-15 seconds, letting gravity stretch your shoulders and decompress your spine. Build up time gradually.
- Wall Ankle Mobilization: Face a wall, place one foot a few inches away, and drive your knee toward it while keeping your heel down. This mobilizes the ankle.
- Downward-Facing Dog: This classic yoga pose stretches the calves, hamstrings, spine, and shoulders simultaneously, making it great for counteracting 'tech neck'.
For more targeted ankle work, explore our article on Ankle Mobility Movements.
How to Create Your Mobility Routine
Creating a mobility routine is about consistency over intensity. Like brushing your teeth, it's the daily habit that counts. Listen to your body, start slow, and progress gradually to build sustainable habits and avoid injury. Always prioritize proper form over range of motion; forcing movements leads to setbacks. For personalized guidance, explore our Therapeutic Exercise Programs.
Getting Started with Mobility Movement Training
- Frequency and Duration: Start with two to four sessions per week for 10 to 20 minutes. Consistency is more important than duration; even five-minute "movement snacks" throughout the day are effective.
- Timing: Use dynamic mobility as a warm-up to prepare for workouts. Use deeper stretches for cool-downs or on rest days for active recovery.
- Tracking Progress: Keep a journal or film yourself monthly to stay motivated and see how far you've come. For more ideas, see our tips for Balance Exercises at Home.
Safety and When to See a Professional
Always prioritize proper form over range of motion. A gentle stretch is good; sharp pain is not. If it hurts, stop.
Use caution with acute injuries, post-surgery recovery, or hypermobility. In these cases, professional guidance is key.
If you have chronic pain or specific concerns, consult a physical therapist. At Evolve Physical Therapy, we can design a personalized program to help you regain pain-free movement. This is crucial for complex issues like balance problems. Learn more about our Physical Therapy for Balance Disorders and how we can help.
Frequently Asked Questions about Mobility Training
As a physical therapist, I get these questions about mobility movement training almost daily. Here are the most common answers.
How long does it take to see results from mobility training?
You may feel some immediate relief after your first few sessions. With consistent practice (2-4 times per week), you can expect noticeable improvements in range of motion and daily comfort within 3-6 weeks. Lasting changes, like sustained joint health and reduced injury risk, build over several months. Consistency is the key to long-term benefits.
Can mobility training replace stretching?
Think of them as complementary. Traditional stretching is typically passive (holding a stretch), which is great for cooling down. Mobility movement training is active (controlling your body through a range of motion), making it ideal for warm-ups. Dynamic stretching is a form of mobility. A balanced routine includes both.
Is mobility training suitable for all ages and fitness levels?
Absolutely. Mobility movement training is adaptable for everyone, from beginners and athletes to seniors. For beginners, it builds a solid movement foundation. For athletes, it improves performance and prevents injury. For older adults, it combats stiffness and improves balance, which is why we offer programs like Balance Training for Seniors. Exercises can be modified for any fitness level or physical limitation, making it a truly universal practice.
Open up Your Potential with a Hands-On Approach
Movement should feel effortless. As we've covered, mobility movement training delivers powerful benefits: injury prevention, improved daily function, and long-term joint health. But knowing what to do isn't the same as doing it effectively. The right guidance is key.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach gets results. We don't just give you an exercise list; we evaluate your unique movement patterns to find the root cause of your limitations. Then, we guide you through a personalized mobility movement training program.
Whether you're dealing with nagging pain or want to improve athletic performance, we meet you where you are. Our convenient Brooklyn locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin are ready to help you start.
We focus on both healing current problems and strengthening your body to prevent future ones. Our goal is to empower you with the tools for long-term independence.
Taking the first step is simple. Schedule an evaluation to assess your movement and create a roadmap to your goals. Don't let stiffness or discomfort limit you another day. Ready to open up your body's potential? Learn more about our physical therapy services and find the freedom of moving well.
How to Nail Your Sitting Posture at Work
Why Sitting Posture at Work Matters More Than You Think

Sitting posture at work directly impacts your health, productivity, and comfort. With many employees spending up to 9 hours a day at a desk, this sedentary reality has earned sitting the nickname "the new smoking."
Quick Answer: The Basics of Correct Sitting Posture at Work
- Feet flat on the floor or footrest
- Knees at 90 degrees, level with or slightly below your hips
- Back supported by your chair, maintaining the natural curve of your lower back
- Shoulders relaxed, not hunched or raised
- Elbows at 90 degrees, close to your body
- Monitor at eye level, about an arm's length away
- Head aligned over your spine, not jutting forward
Poor posture leads to more than just discomfort; it causes significant health problems. The British Chiropractic Association reports that 73% of people struggle with daily back pain, often linked to how they sit. The damage can also include neck pain, digestive issues, reduced lung capacity, and an increased risk of diabetes and cardiovascular disease.
The good news is that small adjustments make a huge difference. Proper sitting posture at work can reduce pain, boost energy, and protect your long-term health.
I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy with nearly two decades of experience. I've helped countless office workers find lasting relief from pain caused by poor posture through ergonomics and targeted exercises.
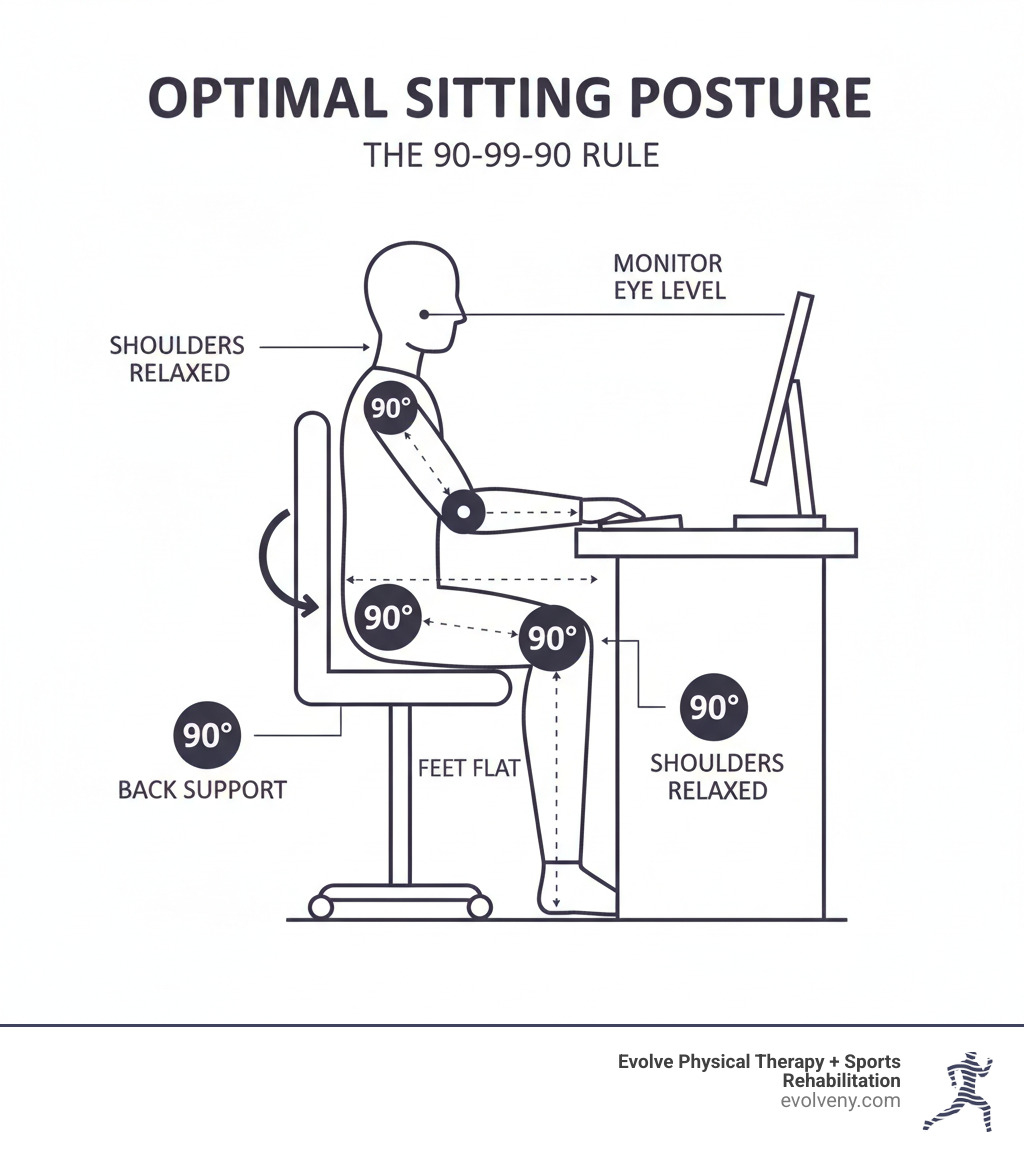
Why Good Posture Is More Than Just Looking Good
Good posture isn't just about looking professional; it's about protecting your body from long-term damage. When you consistently sit with poor posture, you're setting yourself up for chronic pain, digestive problems, and even mood changes. Sitting posture at work directly affects nearly every system in your body.
Health Risks Associated with Poor Sitting Posture at Work
Every hour of slouching adds up. Here’s what’s at stake:
- Chronic Back and Neck Pain: Incorrect sitting puts excess pressure on your spine, leading to premature disc degeneration. A 2020 survey found 41% of remote workers reported new lower back pain. The toll on our bodies from prolonged sitting is significant.
- Digestive Issues: Slouching compresses your abdominal organs, slowing digestion and causing discomfort.
- Reduced Lung Capacity: Hunching forward makes it physically difficult to take deep breaths, reducing oxygen flow to your brain and muscles.
- Increased Disease Risk: Prolonged sitting is linked to a higher risk of type 2 diabetes and heart disease.
- Widespread Joint Pain: A misaligned spine creates a domino effect of pain and stiffness in your hips, knees, and ankles.
- Fatigue and Headaches: Muscles working overtime to support an imbalanced body lead to exhaustion and tension headaches.
Benefits of Maintaining Good Posture While Working
The benefits of good sitting posture at work are immediate and substantial:
- Pain Reduction: Proper spinal alignment takes pressure off your discs, ligaments, and muscles. More on the benefits of good posture highlights this significant relief.
- Increased Energy: An aligned spine allows muscles to work efficiently, conserving energy for your tasks.
- Improved Focus: Without the distraction of nagging pain, you can concentrate better on your work.
- Better Organ Function: Good posture prevents compression of blood vessels and organs, improving circulation and allowing your lungs to expand fully.
- Mood Boost: Research shows that sitting upright can positively influence your emotional state.
- Long-Term Health: You're protecting your joints and muscles from excessive wear and tear, investing in future mobility.
Signs You Have Poor Posture
Are you listening to your body's warning signs? Here’s what to look for:
- Chronic Back, Neck, and Shoulder Pain: Persistent soreness or knots that never loosen are classic signs of overworked muscles.
- Frequent Headaches: Tension headaches starting at the base of your skull often trace back to neck strain.
- General Body Aches: Discomfort in your hips, knees, or ankles can stem from spinal misalignment.
- Muscle Fatigue: If your back and neck muscles feel constantly tired, they're overcompensating for poor alignment.
- Visible Changes: Look for rounded shoulders or a potbelly appearance, which can occur when your core muscles disengage.
Common Mistakes That Ruin Your Sitting Posture at Work
These common habits can sabotage your posture. Avoid:
- Slouching or Hunching: This strains your neck and spine, restricts breathing, and compresses organs.
- Crossing Your Legs: This misaligns your pelvis and spine and can restrict blood flow. Keep both feet flat on the floor.
- Perching on the Edge of Your Chair: This forces your back muscles to work constantly. Use your chair's backrest for support.
- Cradling Your Phone: Use a headset or speakerphone to avoid neck strain.
- 'Tech Neck': This forward head posture occurs when your screen is too low. As one expert explains: "When your spine is aligned correctly, your muscles can support you with minimal strain. But if you slouch or hunch, muscles have to work harder, leading to fatigue and pain."
- Dangling Feet: Use a footrest if your feet don't reach the floor to ensure proper support and pelvic alignment.
- Sitting Too Rigidly: Aim to maintain your spine's natural curves, not a stiff, military-style posture.
- Ignoring Breaks: Your body needs to move. No single position is healthy for hours on end.
How to Achieve the Ideal Sitting Posture at Work: Your Ergonomic Setup Guide
Achieving ideal sitting posture at work isn't about holding a single "perfect" position. It's about creating an ergonomic workspace that supports your body and encourages movement. This concept is known as "dynamic sitting"—the idea that "the next posture is the best posture." Regularly shifting and stretching is key.
An ergonomic setup is your foundation. For a comprehensive overview, see this office ergonomics how-to guide. Let's build your setup, and for more details, see our guide on Ideal Computer Posture.
Your Chair: The Foundation of Good Posture
Your chair is the foundation of good posture. Adjust it correctly:

- Chair Height: Adjust the height so your feet rest flat on the floor (use a footrest if needed). Your knees should be at or slightly below hip level (a 90-degree angle). This usually means a seat height of 16-21 inches.
- Lumbar Support: Sit all the way back in your chair so your lower back's natural inward curve is supported. If your chair lacks support, use a small cushion or rolled-up towel.
- Backrest: Keep your back against the chair. Don't perch on the edge, which forces your back muscles to work overtime.
- Armrest Height: Adjust armrests so your elbows are close to your body at a 90-degree angle, with shoulders relaxed and low.
- Seat Depth: You should be able to fit about three fingers between the back of your knees and the seat's edge. This prevents pressure and ensures good circulation.
Your Monitor: Positioning for a Neutral Neck
Incorrect monitor placement is a common cause of neck pain. Follow these steps:

- Distance: Position your monitor about an arm's length away (typically 20-40 inches).
- Height: The top of your screen should be at or slightly below eye level. This keeps your head balanced over your spine. If you wear bifocals, you may need to lower it an inch or two.
- Position: Center the monitor directly in front of you. If using dual monitors, place the primary one in the center or center both if used equally.
- Adjustments: Use monitor risers or sturdy books to achieve the correct height. For laptops, an external keyboard, mouse, and laptop stand are essential for good posture.
For more screen setup advice, see our guide on Correct Computer Posture.
Your Keyboard and Mouse: Protecting Your Wrists
Protect your wrists from repetitive strain with these adjustments:
- Wrist Position: Keep wrists straight and neutral, not bent up, down, or sideways.
- Keyboard Height: Position your keyboard so your forearms are parallel to the floor, with elbows at a 90-degree angle and close to your body.
- Mouse Placement: Keep your mouse close to your keyboard at the same level to avoid reaching.
- Shoulders: Keep your shoulders relaxed and low, not hunched.
Consider using keyboard shortcuts to reduce mouse use. For more on workstation setup, explore our guide on Home Office Ergonomics.
Beyond the Setup: Maintaining Good Posture All Day
An ergonomic setup is only half the battle. Movement is medicine. Our bodies aren't designed for static positions, so even perfect posture becomes strained over time. Prolonged sitting shortens hip flexors, which can pull on your hips and cause lower back pain.
The solution is "dynamic sitting"—the idea that your next posture is your best posture. Shift, stretch, and change positions regularly. The Canadian Centre for Occupational Health and Safety recommends moving every 50 minutes, but even a micro-break every 30 minutes helps.
- Use the Pomodoro Technique: Work for 25 minutes, then take a 5-minute break to stand or walk.
- Use a Standing Desk: Alternate between sitting and standing, aiming to stand for 5-10 minutes every hour.
Regular movement improves blood flow, reduces stiffness, and prevents the cumulative strain that leads to chronic pain. For personalized guidance, consider Physical Therapy for Posture Training.
The Checklist for Correct Sitting Posture at Work
Run through this quick mental checklist a few times during your workday. The NHS sitting posture tips echo many of these same principles.
Start from the ground up. Your feet should be flat on the floor or a stable footrest—never crossed. Your knees should bend at roughly 90 degrees, positioned level with or slightly below your hips. Moving up, your back needs full support from your chair's backrest, especially maintaining that natural curve in your lower back. Sit all the way back in your seat rather than perching on the edge.
Keep your shoulders relaxed and down—not hunched up toward your ears. Your elbows should stay close to your sides, bent at about 90 degrees. Finally, check that your head is aligned directly over your spine with your chin slightly tucked. This prevents that all-too-common forward head posture that causes so much neck strain.
Simple Stretches and Exercises You Can Do at Your Desk
Incorporate these simple desk stretches to counteract the effects of sitting:

- Chin Tucks: To combat forward head posture, gently pull your chin straight back (making a double chin). Hold for 5 seconds and repeat 10-15 times.
- Shoulder Blade Squeezes: Sit tall and squeeze your shoulder blades together as if holding a pencil between them. Hold for 5-10 seconds and repeat 10-15 times.
- Chest Stretch: In a doorway, place your forearms on the frame and gently step forward until you feel a stretch across your chest. Hold for 20-30 seconds.
- Seated Spinal Twist: Sit tall with feet flat on the floor and gently twist your torso to one side, using the chair for light support. Hold for 15-30 seconds per side.
- Hip Flexor Stretch: Stand and lunge forward with one leg, keeping your back straight. You should feel a stretch in the front of the hip of your back leg. Hold for 20-30 seconds per side.
These movements take just a few minutes. For more targeted exercises, see our guide on Physical Therapy for Neck Pain and Neck Injuries.
Frequently Asked Questions about Desk Posture
Let's tackle the most common questions about sitting posture at work.
Is it bad to cross my legs while sitting?
Yes. While it may feel comfortable, crossing your legs tilts your pelvis and pulls your spine out of alignment, stressing your lower back. It can also compress nerves, causing a "pins-and-needles" sensation, and restrict blood flow. The best practice is to keep both feet flat on the floor or a footrest, with your weight evenly distributed.
How often should I take a break from sitting?
Even with perfect posture, you need to move. Aim to stand and move for a few minutes every 30-50 minutes. Set a timer or use a productivity method like the Pomodoro Technique (work 25 minutes, break 5 minutes) to build the habit. These breaks don't need to be long—a quick walk to the water cooler or a simple stretch is enough to improve blood flow, reduce muscle stiffness, and prevent the strain that leads to chronic pain.
Can a special cushion or posture corrector fix my posture?
They can be helpful tools, but they are not magic fixes. A lumbar cushion can provide needed support if your chair lacks it. Posture correctors (braces or wearables) can serve as temporary reminders, but over-reliance can weaken the core muscles you need to strengthen.
The most effective solution is a combination of a proper ergonomic setup, regular movement, and targeted strengthening exercises. This approach builds lasting strength and muscle memory. For a personalized plan that addresses the root cause of your issues, consult a physical therapist at Evolve Physical Therapy.
Conclusion
Your sitting posture at work is crucial for your long-term health, energy, and focus. As we've covered, poor posture can lead to chronic pain, digestive issues, and more, while good posture offers reduced pain, increased energy, and better overall health.
Good posture is a dynamic habit, not a static position. The goal is to create a supportive environment, move regularly, and stay aware of your body. Small adjustments—like raising your monitor or taking stretch breaks—make a huge impact. Start with one or two changes today.
If pain persists, professional help is key. Sometimes, you need expert guidance to address underlying muscle imbalances or long-standing postural habits.
At Evolve Physical Therapy + Sports Rehabilitation, we specialize in helping people throughout Brooklyn—from Marine Park to Park Slope, Gravesend to Mill Basin—overcome chronic pain. Our hands-on approach focuses on the root causes of your discomfort, with personalized treatment plans to heal your body and build lasting strength. Don't let poor posture hold you back from feeling your best.
Learn how ergonomic physical therapy in Brooklyn can help you build lasting posture habits
Don't Fall for It – Physical Therapy Exercises for Better Balance
Why Balance Problems Affect More People Than You Think

Physical therapy for balance is a specialized approach that helps millions regain stability, reduce fall risk, and restore confidence. It's proven to reduce fall risk in older adults by improving strength, coordination, and reaction time. Physical therapists use targeted exercises and vestibular rehabilitation therapy (VRT) to address root causes like inner ear problems, muscle weakness, and even medication side effects.
A physical therapist conducts a comprehensive balance assessment to create a personalized treatment plan. This involves hands-on therapy, strengthening exercises, and education on fall prevention.
Every second, a senior falls in the United States, but the good news is that falls are largely preventable. Balance is a skill you can improve at any age. Whether you're dealing with instability from an injury or just noticing you're not as steady as you used to be, physical therapy can help. It offers a proven path to rebuild the strength, coordination, and confidence needed to stay active.
I'm Lou Ezrick, founder of Evolve Physical Therapy. With nearly two decades of experience, I've seen that a personalized, hands-on approach to physical therapy for balance is the most effective way to help people overcome these challenges and address the whole person, not just the symptoms.
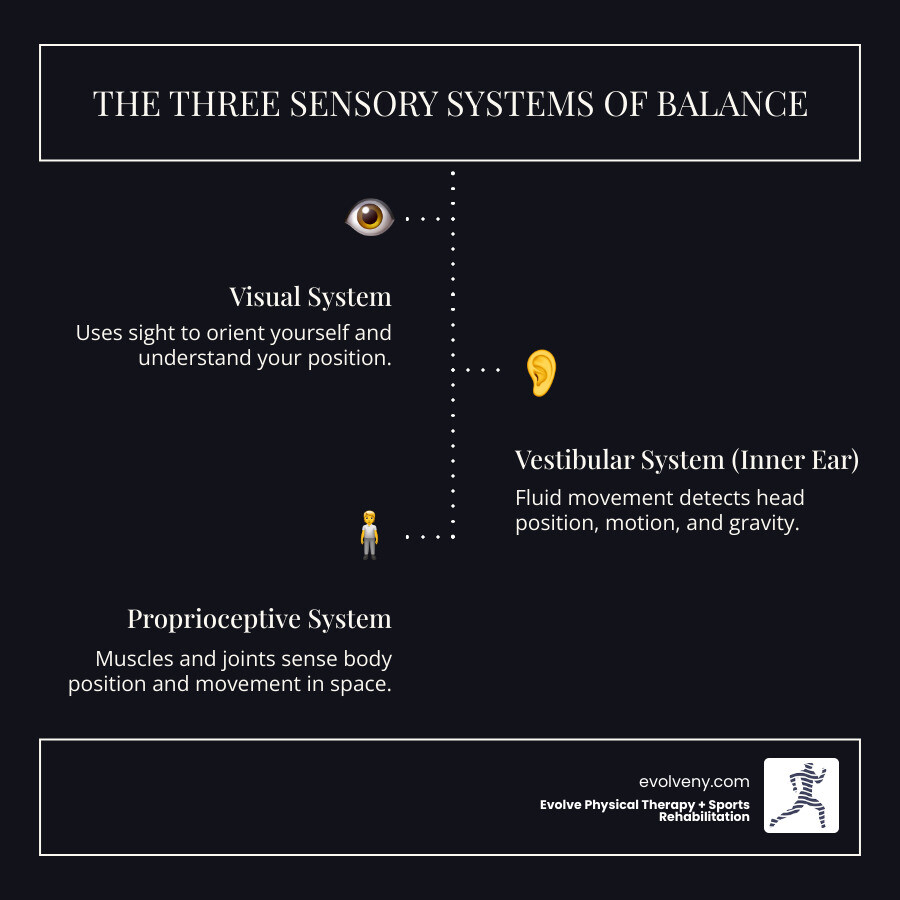
Why Am I Unsteady? Understanding the Root Causes of Balance Problems
Feeling a sudden wobble or a shift in the room when you stand up are common signs of a balance issue. Balance is your body's ability to stay upright and stable. It has two main components: static balance for when you're still (like standing in line) and dynamic balance for when you're moving (like walking or turning). When this system is disrupted, you might feel unsteady, dizzy, or experience vertigo—the sensation that the world is spinning. Staggering or swaying, especially when changing positions, are also common symptoms.

Common Causes of Imbalance
Balance problems often stem from a combination of factors. Age-related changes are significant, as muscles weaken, joints stiffen, and sensory systems become less sharp. Our team has extensive experience helping older adults maintain independence through targeted physical therapy for seniors.
Muscle weakness and joint stiffness are major contributors. A strong core and legs are essential for stability. Your inner ear's vestibular system also plays a key role, and conditions like vertigo, Meniere's disease, or ear infections can disrupt it. Neurological conditions like stroke or Parkinson's disease can interfere with the brain-body communication needed for balance. Finally, don't overlook medication side effects, as many common drugs can cause dizziness or drowsiness.
How a Physical Therapist Diagnoses Balance Issues
At Evolve Physical Therapy, we focus on finding the root cause. We start with a comprehensive health history to understand your symptoms and how they affect your life. Our movement screening involves observing how you walk, stand, and move. We use standardized balance tests, like the Timed Up and Go test, to get objective measurements of your stability.
By systematically testing your vision, vestibular system (inner ear), and proprioception (body awareness), we can identify which systems are struggling. This allows us to create a treatment plan designed for your unique situation, which is why physical therapy for balance is so effective. You can learn more about our personalized PT plans and how we tailor each treatment.
The Professional Approach: How Physical Therapy for Balance Restores Stability
Working with a movement expert for physical therapy for balance means you get a scientific approach, not a generic set of exercises. After our assessment identifies the root cause of your issues, we create a personalized treatment plan. Our goal is to dramatically reduce your fall risk and restore your confidence, which is crucial. Fear of falling can lead to a less active, more isolated life. We help people break that cycle.
For more specialized vestibular issues, we offer comprehensive vestibular physical therapy in Brooklyn to address inner ear-related balance problems.
Types of Specialized Balance Training
If inner ear problems are the cause, we use Vestibular Rehabilitation Therapy (VRT) to retrain your brain to better process signals from your inner ear, eyes, and body. This includes:
- Gaze stabilization exercises: To help you see clearly when your head is moving.
- Habituation exercises: To gradually reduce dizziness triggered by specific movements or busy environments.
- Repositioning maneuvers: For conditions like BPPV, these precise movements can provide immediate relief by repositioning inner ear crystals.
Strength, Coordination, and Reaction Training
Balance also requires physical strength and coordination. We focus on:
- Core strengthening: A strong core is the foundation for safe movement.
- Lower body exercises: Strong hips, thighs, and calves are your pillars of support.
- Proprioceptive training: This sharpens your body's internal awareness, or "sixth sense," often by using unstable surfaces or having you close your eyes. You can learn more about dynamic balance training and how we incorporate these challenging movements.
- Perturbation-Based Training (PBT): This advanced technique uses small, controlled pushes or shifts to improve your reaction time. Research shows this can reduce fall rates significantly and builds trust in your body's ability to recover from unexpected disturbances.
Your At-Home Balance Workout: 6 Essential Exercises
Consistent home practice is where the real magic of physical therapy for balance happens, building the muscle memory and confidence you need. Safety first: Always check with your healthcare provider before starting a new routine. Perform these exercises near a sturdy support like a kitchen counter or wall. Listen to your body and aim for practice at least twice a week. For additional guidance on creating your home routine, check out our comprehensive guide on balance exercises at home.

Foundational Physical Therapy for Balance Exercises
These exercises build static balance - your ability to stay steady when you're not moving.
- Sit-to-Stands: From a sturdy chair, stand up without using your hands, then slowly lower yourself back down. This builds essential leg strength for daily activities.
- Weight Shifts: Standing with feet hip-width apart, slowly shift your weight from one foot to the other. This improves your body's ability to make small, stabilizing adjustments.
- Single-Leg Stance: Holding onto support, lift one leg and hold for 5-10 seconds, working up to 30. This strengthens key stabilizing muscles in your ankles, knees, and hips.
Dynamic Physical Therapy for Balance Exercises
Now we move into dynamic balance - staying steady while you're moving.

- Heel-to-Toe Walk: Walk in a straight line, placing the heel of one foot directly in front of the toes of the other. Look forward, not down, to improve your body's spatial awareness.
- Sidestepping: Step sideways for 10 steps, then return. This improves lateral stability, which is crucial for preventing falls.
- Step-Ups: Use a low, sturdy step or the bottom stair. Step up with one leg, then the other, and step back down. This builds strength and coordination for stairs and curbs.
Consistent practice is key. Some days will be better than others, but with regular effort, you'll feel much steadier and more confident.
Making Stability a Habit: Progression and Lifestyle Tips
Once you're comfortable with the basic physical therapy for balance exercises, it's time to challenge yourself. Progressing exercises safely means gently pushing your boundaries. Try reducing your hand support, performing exercises with your eyes closed (always near a wall for safety), adding head turns, or balancing on unstable surfaces like a folded towel or pillow. These progressions force your balance systems to work harder and adapt. As your balance improves, so will your gait. Learn more info on balance and gait training to see how these systems connect.
Lifestyle Changes for Lasting Balance
Creating a balance-friendly lifestyle is key. Make simple home safety modifications like securing loose rugs and adding nightlights. Wear proper footwear with good support and grip. Schedule a medication review with your doctor to see if any prescriptions are causing dizziness. Finally, don't skip annual vision and hearing exams, as both senses are vital for balance.
Integrating Balance into Daily Life
You can sneak balance training into your daily routine. Try one-leg stands while brushing your teeth or tandem (heel-to-toe) walking in hallways. Whenever possible, take the stairs to build strength and coordination. You might also enjoy balance-focused group classes like Tai Chi, which is proven to improve postural stability.
The evidence supporting exercise for fall prevention is overwhelming. Research shows that physical activity, especially programs that include balance and strength training, can significantly reduce falls in older adults. Every small improvement you make builds toward a more stable and confident future.
Frequently Asked Questions About Balance Therapy
Here are answers to some common questions about physical therapy for balance.
How long does it take to improve my balance with physical therapy?
The timeline varies by individual and depends on the cause of your issues, your overall health, and your consistency with exercises. Many patients notice improvements within a few weeks, with more significant gains over weeks to months. For some vestibular conditions like BPPV, relief can come after just one session. Consistency is key to achieving the best results, and we'll help you set realistic goals.
Can physical therapy help with dizziness and vertigo?
Yes, absolutely. Vestibular Rehabilitation Therapy (VRT) is specifically designed to treat dizziness and vertigo, especially when caused by inner ear problems. We use targeted exercises and specific maneuvers to retrain your brain and sensory systems, often leading to a significant reduction in symptoms.
When should I see a physical therapist for balance problems?
You should consider seeing a physical therapist if you:
- Have had a fall, even a minor one.
- Feel unsteady on a regular basis.
- Experience dizziness or vertigo.
- Have difficulty with daily activities like walking or climbing stairs.
Proactive fall prevention is also a smart reason to see a PT, especially if you are over 65 or have risk factors. In New York, you can contact us directly for an evaluation without a doctor's referral.
Take the First Step Towards a More Stable Future
You now know that falls are preventable and that balance is a skill you can improve at any age. We've seen how factors from muscle weakness to inner ear problems can affect stability, and how physical therapy for balance offers targeted, evidence-based solutions.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach is designed to find and treat the root cause of your unsteadiness. We create personalized plans for everyone, from active Brooklyn professionals to those seeking proactive fall prevention. Our expertise in vestibular rehabilitation and strength training can help you regain stability and confidence.
You don't have to accept unsteadiness or live with the fear of falling. With professional guidance and consistent practice, you can build a more stable, confident future.
Schedule a personalized physical therapy evaluation today and take the first step. Let us help you create a plan to get back on solid ground. Your journey to better balance starts now.
Mobility Moves: Exercises to Boost Your Range of Motion
Why Mobility and Movement Exercises Are Essential for Pain-Free Living

Mobility and movement exercises are targeted movements that improve your joints' ability to move freely through their full range of motion while maintaining control and stability.
Key Types of Mobility Exercises:
- Hip mobility: 90/90 stretches, hip circles, spider lunges
- Shoulder mobility: Arm circles, wall angels, overhead reaches
- Spine mobility: Cat-cow stretches, thoracic rotations, twists
- Ankle mobility: Circles, calf stretches, dorsiflexion drills
Primary Benefits:
- Reduce injury risk by up to 6 times
- Improve athletic performance and daily movement
- Decrease muscle stiffness and soreness
- Support healthy aging and independence
Feeling stiff is common, especially since Americans sit an average of 8 hours every day. This sedentary lifestyle makes muscles stiff and sore, limiting free movement. Fortunately, even five minutes of mobility work a few times a week can have a positive benefit. The right movements can restore your body's natural range of motion.
Research shows that subjects with higher mobility scores were six times less likely to get injured. This isn't just for athletic performance—it's about maintaining your quality of life as you age.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience. At Evolve Physical Therapy, I've seen how targeted mobility and movement exercises transform lives, helping everyone from weekend warriors to desk-bound professionals move better and feel stronger.
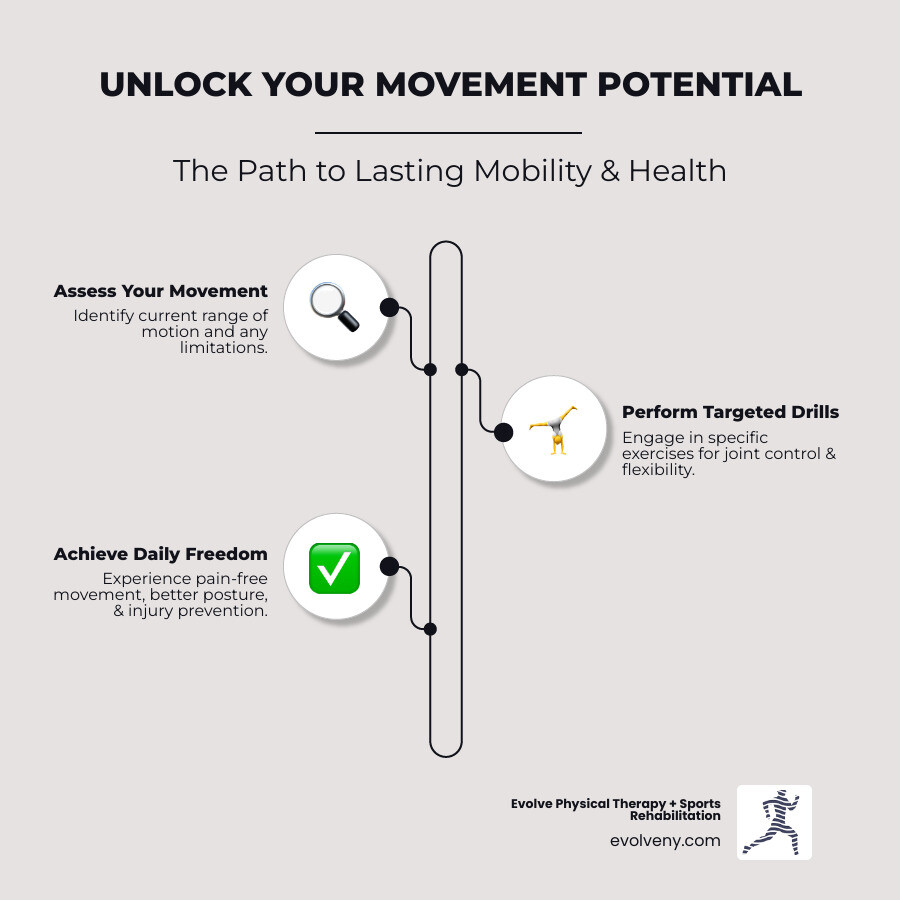
Understanding Mobility: More Than Just Flexibility
If you've ever wondered why some people seem to move effortlessly while others struggle with basic movements, the answer often lies in understanding mobility. At Evolve Physical Therapy, we see this distinction every day - and it's more important than you might think.
Most people use "flexible" and "mobile" as if they mean the same thing. But here's the truth: you can be incredibly flexible yet still move poorly, or have amazing mobility without being able to do the splits. Understanding this difference is your first step toward pain-free movement.
What Makes Mobility Different
Think of mobility as your body's ability to move freely and easily through its full range of motion while staying in complete control. It's not just about how far you can stretch - it's about how well your joints, muscles, and nervous system work together to create smooth, controlled movement.
When you walk up stairs, reach for something on a high shelf, or simply get out of bed in the morning, you're using mobility. It combines joint health, muscle strength, and your brain's ability to coordinate movement - what we call motor control.
The Flexibility vs. Mobility Breakdown
Here's where it gets interesting. Flexibility is passive - it's how far someone else can move your leg if you're completely relaxed. Maybe you can lie on your back and have someone push your leg toward your chest until it touches.
Mobility, on the other hand, is active. It's how high you can lift that same leg using your own muscles while maintaining control and stability. You might be surprised to find there's a big difference between the two.
This is why some yoga enthusiasts can fold themselves into pretzel-like poses but struggle with basic squats. They have flexibility but lack the strength and control needed for functional mobility.
Why Stability Matters Just as Much
Here's something that might surprise you: mobility without stability is actually dangerous. Think of stability as your body's ability to keep joints secure and supported while you're moving. It's what keeps your knee from buckling when you step off a curb or prevents your shoulder from sliding around when you reach overhead.
Motor control ties it all together. This is your nervous system's ability to sequence movements properly and control where they start and stop. Without good motor control, even simple movements become clunky and inefficient.
At Evolve Physical Therapy, we often tell patients that mobility without stability leads to injury-prone joints, while stability without mobility creates stiffness. You need both working together.
The Role of Body Awareness
There's another piece to this puzzle: body awareness, or what we call proprioception. This is your body's built-in GPS system - it tells you where your limbs are in space without having to look.
Good proprioception is why you can walk in the dark without falling over or catch yourself when you start to slip. Mobility and movement exercises naturally improve this body awareness, making you move more confidently in all activities.
| Feature | Mobility | Flexibility | Stability |
|---|---|---|---|
| Definition | Controlled movement through full range of motion | Passive range of motion or muscle length | Ability to maintain position or control movement |
| Focus | Joints, muscles, nervous system, and control | Muscle and tendon lengthening | Joint integrity and postural control |
| Components | Strength, flexibility, coordination, motor control | Muscle elasticity | Muscle strength, balance, coordination |
| Example | Actively lifting leg high with control | Passively holding leg high (assisted) | Holding a single-leg stance without wobbling |
| Benefit | Functional movement, injury prevention, performance | Improved range of motion, reduced muscle stiffness | Injury prevention, efficient movement, balance |
The bottom line? True mobility training addresses all these elements together. It's not enough to just stretch - you need to build strength, control, and awareness throughout your entire range of motion. That's what creates lasting change and keeps you moving well for life.
The Life-Changing Benefits of Daily Mobility Work
Here's something that might surprise you: while everyone talks about hitting the gym for strength training or logging miles for cardio, mobility and movement exercises might just be the most important thing you're not doing. At Evolve Physical Therapy, we've seen how these simple movements can completely transform someone's quality of life.
Think about it this way - what good is being able to bench press 200 pounds if you can't reach overhead to put a dish away without pain? Or what's the point of running marathons if your tight hips leave you hobbling around the house every morning?
Your Body's Best Insurance Policy Against Injury
Let's start with the most compelling reason to make mobility a priority: it's like having incredible insurance for your body. Subjects who scored higher on a screening test that measured mobility were found to be six times less likely to get injured.
Six times! That's not a small improvement - that's life-changing.
When your joints can move through their full, intended range of motion, something beautiful happens. The stress gets distributed properly across all your tissues instead of building up in one spot. No more compensating with your lower back because your hips are tight. No more shoulder pain because your thoracic spine won't rotate. Your body works as the integrated system it was designed to be.
Open up Your Body's True Performance Potential
Whether you're chasing your kids around the playground, playing weekend tennis, or just want to feel strong and capable in your daily life, improved mobility is your secret weapon. When your joints move freely, everything else follows.
Better hip and ankle mobility means you can squat deeper, which means stronger glutes and legs. Improved shoulder mobility means you can reach, lift, and throw without that nagging ache. Even simple activities like getting out of bed or climbing stairs become effortless when your body moves the way it should.
Stand Taller, Feel Better, Move With Confidence
Here's the reality: Americans sit for about 8 hours every day. Our hip flexors get tight, our shoulders round forward, and our spines forget how to extend. The result? That stiff, achy feeling that's become so "normal" we forget what it's like to feel good.
Mobility and movement exercises directly counteract these effects. They wake up sleepy muscles, restore proper joint alignment, and help you refind what it feels like to stand tall and move with confidence. The morning stiffness starts to fade. That afternoon shoulder tension becomes a thing of the past.
Your Investment in a Vibrant Future
Here's what really motivates us at Evolve Physical Therapy: helping people age with grace and independence. Maintaining mobility is critical to staying independent as you age, according to the National Institutes of Health.
As we get older, joints naturally become less lubricated, cartilage thins, and tendons lose their elasticity. Muscles get weaker, bones become less dense, and our nervous system slows down. Add in conditions like arthritis, and it's easy to see how mobility can decline rapidly.
But here's the exciting part: it doesn't have to be this way. Regular mobility work keeps your joints well-oiled, your muscles engaged, and your movement patterns sharp. This means continuing to tie your own shoes, reaching items on high shelves, and walking up stairs without thinking twice about it.
We've worked with patients in their 70s and 80s who move better than some 40-year-olds, and the difference is almost always consistent attention to mobility. It's never too late to start, and it's never too early to begin investing in your future self.
The Ultimate Guide to Mobility and Movement Exercises
Now that we understand the profound benefits of mobility and movement exercises, let's dive into some practical movements you can start using today. The beauty of mobility work is its simplicity; you don't need fancy equipment or hours to see real improvements.
At Evolve Physical Therapy, we emphasize that consistency beats intensity. Think of these exercises as daily maintenance for your body, like brushing your teeth. A few minutes each day can prevent bigger problems down the road.
Controlled movements are always better than fast or forced ones. Listen to your body. These exercises work wonderfully as dynamic warm-ups before a workout, as gentle cool-downs, or as part of your morning routine.
Essential Hip Mobility and Movement Exercises
Your hips are the body's central hub, connecting your upper and lower body. Unfortunately, they're often the first casualty of our desk-bound lives. When you sit for hours, your hip flexors tighten, pulling on your lower back and creating stiffness.
Targeted mobility and movement exercises can open up your hips and restore that natural freedom of movement.

The 90/90 Hip Switch addresses both internal and external hip rotation. Sit on the floor with both knees bent at 90 degrees—one leg externally rotated in front of you, the other internally rotated to your side. Keep your chest proud and slowly switch your knees from one side to the other, rotating through your hips while keeping your feet planted. Aim for 5-10 smooth transitions per side. Don't worry if it feels awkward at first; that's your body learning new movement patterns.
The Cat-Cow stretch is fantastic for your hips and spine. Start on all fours with hands under shoulders and knees under hips. As you inhale, drop your belly, lift your tailbone, and look up (Cow). Exhale as you round your spine, tuck your tailbone, and bring your chin to your chest (Cat). The magic is in the pelvic movement, teaching your hips and spine to work together.
For a full-body opener, try the World's Greatest Stretch. Start in a lunge with your right foot forward, placing both hands inside your front foot. Keep your left hand down and rotate your chest to the right, reaching your right arm toward the ceiling. You'll feel this through your hip flexors, thoracic spine, and hamstrings. Five reps per side is plenty.
Hip Circles are simple but effective for lubricating your hip joint. Stand tall, holding a wall for balance if needed, and lift one knee. Make small circles with your knee, gradually increasing the size. Ten to fifteen circles in each direction will get your hips feeling more fluid.
The Spider-Man Lunge targets stubborn hip flexors. Start in a high plank, then step your right foot to the outside of your right hand, lowering your hips. Hold for a few deep breaths. For an extra challenge, lift the arm that matches your front leg for some thoracic rotation.
Key Shoulder Mobility and Movement Exercises
Our shoulders are the most mobile joints in our body. But modern life isn't kind to them. Hours hunched over computers and phones leave us with rounded shoulders and limited overhead reach.

Shoulder CARs (Controlled Articular Rotations) are the gold standard. They take your shoulder joint through its full range of motion in slow motion. Stand tall with your arm extended, thumb up. Slowly rotate your arm outward, upward, then backward, making the largest circle possible while keeping your torso still. Your thumb should point down when your arm is behind you. Reverse the motion. Three to five slow rotations in each direction will improve your shoulder's capabilities.
The Thoracic Extension on Foam Roller addresses a root cause of shoulder problems: a stiff mid-back. Lie on your back with the foam roller horizontally under your mid-back. Support your neck and gently extend your upper back over the roller. Five to ten gentle extensions will help restore your spine's natural curve.
Wall Angels improve posture and teach your shoulder blades to move properly. Stand with your back against a wall, feet about six inches away. Press your lower back, head, and arms against the wall, then slowly slide your arms up and down like a snow angel. The challenge is keeping everything pressed against the wall.
Simple Arm Circles are effective for lubricating your shoulder joints. Extend your arms to your sides and make small circles forward, gradually increasing the size. After 10-15 circles, reverse direction. Keep your shoulders down and back.
These mobility and movement exercises are crucial for maintaining healthy overhead reach.
Foundational Spine and Ankle Drills
Your spine is your central support, and your ankles are your foundation. Stiffness in either area can cause a ripple effect of problems. A stiff ankle can cause knee pain, while a rigid mid-back can lead to neck and lower back issues.

Thoracic Spine Rotations ("Thread the Needle") are fantastic for your mid-back. Start on all fours and thread your right arm under your left armpit, resting your right shoulder and ear on the floor. Feel the gentle twist through your mid-back. Hold for 30 seconds or perform 5-10 gentle rotations before switching sides. This is valuable for anyone who needs rotational power.
We've covered Cat-Cow for hips, but it's equally important for spinal health. Focus on articulating each segment of your spine as you move between the two positions.
Downward-Facing Dog is a yoga classic that benefits your hamstrings, calves, and ankles. Push your hips up and back to form an inverted V, then press your heels toward the floor. A small bend in your knees is fine to keep your spine straight. Hold for 30-60 seconds, or gently "pedal" your feet to deepen the calf stretch.
Ankle Circles are essential for ankle joint health. Sit or stand, lift one foot, and slowly make circles with your ankle in both directions. Ten to fifteen circles each way will help lubricate the joint.
Calf Stretches with a focus on dorsiflexion (toes toward shin) are crucial for proper squat depth and walking. Stand facing a wall, step one foot back, and lean forward while keeping both heels down. For a deeper stretch, bend your back knee slightly. Hold for 30 seconds per side.
These foundational exercises are the building blocks of good movement. When your spine and ankles are mobile, your whole body works better.
How to Build Your Own Mobility Routine
The question I hear most often at Evolve Physical Therapy is simple: "How much do I actually need to do?" Here's the truth that might surprise you: consistency beats intensity every single time. You don't need to become a yoga master or spend hours stretching. Even five minutes a few times a week can have a positive benefit.
The Magic of Frequency Over Duration
Think of mobility and movement exercises like brushing your teeth. You wouldn't brush for an hour once a week and expect great results, right? The same principle applies here. It's far more beneficial to practice mobility for 5 to 10 minutes five times a week than cramming an hour-long session into your Sunday.
If you're just starting out, aim for two to three sessions per week and gradually build up to four times weekly. The beautiful thing about mobility work is that you can do it pretty much every day without overdoing it. Your joints actually thrive on regular, gentle movement.
When to Fit It In
The beauty of mobility work is its flexibility (pun intended!). You can weave it into different parts of your day:
Pre-workout warm-ups using dynamic mobility drills prepare your body for action. Post-workout cool-downs with gentle movements help your body transition back to rest while maintaining that newfound range of motion. On rest days, a dedicated mobility session works as perfect active recovery, reducing soreness and keeping your joints happy.
My favorite approach? Daily "movement snacks" - short bursts throughout the day, especially if you're one of those Americans sitting for 8 hours daily. A few hip circles between meetings or shoulder rolls while waiting for coffee can work wonders.
Tracking Your Progress (It's Easier Than You Think)
Nothing motivates like seeing real progress. Here are two simple ways we recommend to our patients:
Film yourself performing key movements like a deep squat or overhead reach before starting your routine. Re-film every few weeks and compare - the visual progress is incredibly powerful and often surprising. Keep a workout journal noting how movements feel, whether you can go deeper into stretches, or if previously stiff areas feel more fluid. This subjective feedback is just as valuable as any measurement.
At Evolve Physical Therapy, we use professional assessment tools to measure your improvements objectively, but you can absolutely track meaningful progress at home.
Tailoring for Your Life
Mobility and movement exercises absolutely can be customized for specific sports or activities. Runners benefit tremendously from ankle, hip, and hamstring mobility to improve stride efficiency. Desk workers need focused hip flexor and thoracic spine work to counteract prolonged sitting. We regularly work with athletes and everyday people to identify their unique movement demands and design targeted programs.
Here's a sample 5-minute daily mobility routine that hits the major areas:
- Cat-Cow: 10 repetitions, focusing on smooth spinal movement
- Thoracic Spine Rotations: 5-8 repetitions per side
- Hip Circles: 5-8 large circles each direction per leg
- Ankle Circles: 10 circles each direction per ankle
- World's Greatest Stretch: 2-3 repetitions per side, holding for a few breaths
This quick routine touches on your spine, hips, and ankles - the areas that need the most attention for most people. It easily fits into your morning routine or evening wind-down, and you'll be amazed at how much better you feel with just this small investment in your body.
Conclusion
Throughout this guide, we've explored the transformative world of mobility and movement exercises - from understanding what true mobility means (and how it's different from simple flexibility) to finding the incredible benefits these exercises can bring to your daily life.
The research speaks for itself: people with better mobility are six times less likely to get injured. But beyond the statistics, we've seen how these exercises can help you wake up without that morning stiffness, move through your day with confidence, and maintain your independence as you age.
Your body truly is designed to move. After nearly two decades of helping patients overcome pain and movement limitations, I can tell you that maintaining your full range of motion isn't just about feeling good today - it's about protecting your future self. Whether you're battling the effects of sitting at a desk all day, working to prevent injuries, or simply wanting to feel more comfortable in your own skin, dedicated mobility work is one of the most powerful investments you can make in your health.
The beauty of mobility and movement exercises lies in their accessibility. You don't need expensive equipment or hours of free time. Just five to ten minutes of consistent daily practice can create meaningful changes in how you feel and move. It's consistency over intensity that wins the day.
At Evolve Physical Therapy + Sports Rehabilitation, we've witnessed countless changes right here in Brooklyn. Our patients from Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin have finded what it feels like to move without pain, to reach overhead without restriction, and to trust their bodies again. Our hands-on approach means we don't just give you exercises - we work with you to understand your unique movement patterns and create a personalized plan that fits your lifestyle and goals.
Taking control of your health doesn't have to be overwhelming. Sometimes the most profound changes come from the simplest actions - like dedicating a few minutes each day to helping your body remember how to move well.
If you're ready to experience what it feels like to move with freedom and confidence again, we're here to help you take that first step.
Sit Right, Feel Bright: Mastering Office Work Posture
Why Office Work Posture Matters More Than You Think
Office work posture affects millions of workers who spend much of their day seated, leading to health issues beyond simple back pain.
Key Elements of Proper Office Work Posture:
- Head: Level and aligned with spine, not tilted forward
- Shoulders: Relaxed and even, not hunched or rolled forward
- Elbows: Bent at 90-120 degrees, close to your body
- Wrists: Straight and neutral, not bent up or down
- Back: Supported with natural lumbar curve maintained
- Hips and Knees: At 90-degree angles or slightly higher
- Feet: Flat on floor or footrest, not dangling
The statistics are sobering: for every inch your head moves forward from proper alignment, your neck bears an additional 10 pounds of stress. Poor posture doesn't just cause neck and back pain; it can reduce lung capacity, disrupt digestion, and increase your risk of diabetes and cardiovascular disease.
The good news is that good posture is within your control. Sitting correctly reduces unnecessary strain on muscles and joints, boosts your energy levels, and can improve your focus and productivity.
As Lou Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades helping patients overcome chronic pain rooted in poor office work posture habits. Through my work with hundreds of desk workers, I've developed practical strategies that address the root causes of postural dysfunction, not just the symptoms.

The Hidden Dangers of Your Desk Job
Poor office work posture creates a domino effect of health problems. Spending hours hunched over a keyboard or slumped in a chair takes a toll on your body in ways you might not realize.
Back pain is often the first warning sign. Slouching flattens your spine's natural curves, putting immense pressure on discs and ligaments. This can lead to disc degeneration and chronic discomfort.
Your neck also suffers. For every inch your head juts forward, your neck muscles work 10 pounds harder, leading to "tech neck." This persistent ache and stiffness from looking at screens can cause chronic neck strain and trigger tension headaches.
Poor posture affects more than muscles and joints. Slouching compresses abdominal organs, causing digestion issues and slowing metabolism. It also reduces lung capacity by shortening frontal muscles, making deep breaths difficult. Less oxygen means lower energy and reduced brain function.
Most concerning is the increased risk of chronic disease. Prolonged sitting and poor posture are linked to a higher risk of diabetes and cardiovascular disease. Our bodies are designed for movement, and a sedentary lifestyle works against our biology.
The science behind these risks is eye-opening. You can explore more about the health risks of sitting to understand just how serious these issues can become. And if you're wondering about the state of your own neck alignment, take a moment to consider Have You Checked Out Your Neck Curvature Lately.

Common Mistakes That Ruin Your Office Work Posture
It's easy to slip into habits that wreck our office work posture. These mistakes gradually become your new normal.
Slouching is the most common mistake. Collapsing your spine into a C-shape stresses discs and ligaments and can compress nerves, causing radiating pain.
Forward head posture ("tech neck") occurs when you lean forward to see your screen. This strains your neck and upper back muscles and is extremely common among office workers.
Crossing your legs feels comfortable but can cause problems. It can compress nerves, leading to numbness, misalign your hips, and restrict blood flow.
Dangling feet put pressure on the backs of your thighs and disrupt alignment up your entire body. Proper support for hips and knees is essential.
Reaching for your mouse or keyboard due to an improper setup leads to shoulder shrugging, leaning, and can cause repetitive strain injuries.
Cradling your phone between your ear and shoulder is a direct cause of neck and upper back pain, as the muscles aren't meant to hold that position.
The good news is that recognizing these patterns is the first step toward fixing them. For a deeper dive into identifying and correcting these common issues, check out our detailed guide on Bad Office Posture.
The Ultimate Guide to Proper Office Work Posture
Let's focus on what proper office work posture should look like. It's your body's natural sweet spot, where everything aligns without strain. The goal isn't a rigid, military-straight spine. Instead, we aim to maintain its natural curves with balance and support.

Your head should be level and balanced directly over your shoulders, not jutting forward. Imagine a string pulling your head upward, aligning your ears, shoulders, and hips.
Your shoulders should be relaxed and even, not hunched. Roll them back and let them settle naturally.
Keep your elbows close to your body, bent at 90 to 120 degrees. This supported position allows your forearms to rest gently on your desk.
Wrists and hands must stay in a straight line, not bent up, down, or sideways. Your hands, wrists, and forearms should form one continuous unit.
For your back, sit all the way back in your chair to maintain the natural curve in your lower back. Good lumbar support is crucial and should feel like a gentle pressure in the small of your back.
The 90-90-90 rule applies to your lower body: aim for 90-degree angles at your hips, knees, and ankles. Your thighs should be parallel to the floor.
Finally, your feet should rest flat on the floor or a footrest. This stable base supports your entire posture.
Proper alignment makes sitting feel effortless, as your muscles aren't fighting gravity. For a deeper dive into achieving this ideal setup, check out our comprehensive guide on Ideal Desk Posture.
Perfect posture isn't about being rigid—it's about finding a balanced, supported position where your body can work comfortably for hours.
Building Your Ergonomic Oasis: A Step-by-Step Setup
An ergonomic workspace isn't about fancy equipment; it's about setting up your environment to support your body's natural alignment. A correct setup means less strain, more comfort, and better focus.
Proper office work posture requires the right foundation. Your workspace should work with you, not against you. When everything is positioned correctly, you'll notice less strain, more comfort, and the ability to focus on your work instead of constantly shifting positions.

The Mayo Clinic provides excellent guidance in their comprehensive office ergonomics how-to guide, and if you're working from home, our dedicated insights on Home Office Ergonomics can help you create an ideal setup in any space.
Chair Adjustments for Optimal Support
Your office chair is your foundation. Most ergonomic issues can be solved with a few simple adjustments.
- Seat height: Adjust so your feet are flat on the floor and knees are at a 90-degree angle. Your knees shouldn't be higher than your hips. A height of 16-21 inches works for most.
- Lumbar support: It should maintain your lower back's natural inward curve. If your chair lacks support, use a cushion or rolled towel.
- Armrests: Set them so your shoulders are relaxed, with elbows close to your body and bent at 90-120 degrees. If they're too high you'll hunch; too low and you'll lean.
- Seat depth: Sit all the way back and ensure a two-finger gap between the seat edge and the back of your knees for good circulation.
Desk, Keyboard, and Mouse Placement
With your chair adjusted, set your desk height so your forearms are parallel to the floor when typing. If your desk isn't adjustable, raise your chair and use a footrest.
Place your keyboard directly in front of you, 4-6 inches from the desk edge, to keep wrists straight. The mouse should be right next to it to avoid reaching.
Use wrist rests only for breaks, not while typing. Let your wrists float to prevent pressure on nerves that can lead to carpal tunnel syndrome. For detailed guidance, our article on Correct Computer Posture walks you through the specifics.
Monitor Positioning to Prevent Neck Strain
Your monitor position is critical for good office work posture and preventing neck pain.
- Position: Place your monitor arm's length away (20-40 inches).
- Height: The top of the screen should be at or just below eye level.
- Centering: Center the monitor directly in front of your keyboard to avoid twisting your neck.
- Bifocals: If you wear them, lower your monitor an extra inch or two to avoid tilting your head back.
- Laptops: The screen is too low and the keyboard is cramped. Use an external keyboard, mouse, and a laptop stand or separate monitor.
Accessories like footrests, back cushions, and monitor stands are problem-solvers that help ensure proper foot placement, lumbar support, and screen height.
Maintaining Good Habits for Lasting Comfort
A perfect ergonomic workspace is just the start of improving your office work posture. Real change comes from weaving healthy movement into your daily routine. Your body is designed for movement. Staying static for hours, even in an ideal setup, creates tension, reduces circulation, and encourages slouching.
Adopt the 30-minute rule: every half hour, take a brief break to stand, walk, or stretch. This regular movement prevents stiffness, improves blood flow, and resets postural muscles. Find a consistent rhythm that works for you.
A sit-stand desk is a great tool for alternating between sitting and standing. This reduces the static load on your spine, but variation is key—don't just stand all day.
Micro-movements also help. While seated, shift your weight, adjust your chair, or stretch your fingers and wrists to prevent your body from getting locked into one position.
For more comprehensive strategies on building these habits into your routine, check out our guide on Good Posture for Office Workers.
Simple Stretches to Improve Your Office Work Posture
Regular stretching resets your office work posture. These desk-friendly movements counteract the effects of prolonged sitting.

- Neck rolls: Relieve tension from screen time. Gently bring your ear toward each shoulder and do chin tucks to combat "tech neck."
- Shoulder shrugs: Release tension in your upper back. Lift your shoulders to your ears, hold, and then release.
- Torso twists: Improve spinal mobility. While seated, gently rotate your upper body to one side, using the chair for support, then repeat on the other side.
- Wrist stretches: Help prevent repetitive strain injuries. Extend your arm and gently pull your fingers back, first with the palm up, then down.
- Upper back stretch: Counteracts hunching. Clasp your hands and push forward, rounding your upper back. You can also interlace fingers behind your head and open your elbows to stretch your chest.
These stretches improve flexibility, boost blood flow, and remind your body what good alignment feels like.
The Role of Professional Guidance
Sometimes, despite your best efforts, you may need professional support for your long-term comfort and health.
When should you see a specialist? Seek professional guidance for persistent pain, numbness, tingling, or weakness that doesn't improve with self-care or interferes with your daily life.
How can physical therapy help? At Evolve Physical Therapy + Sports Rehabilitation, we go beyond symptoms. We start with a thorough posture assessment to find the root cause of your discomfort. Our physical therapists use hands-on techniques, targeted exercises, and education to correct imbalances. We focus on core stability, spinal alignment, and muscle re-education to retrain your body.
Our goal is lasting relief. We teach you custom corrective exercises and help you understand how your daily habits contribute to your discomfort. Physical therapy for posture training can be a game-changer. To learn more, explore our guide on Physical Therapy for Posture Training.
Frequently Asked Questions about Office Posture
Here are answers to common questions about improving office work posture.
How long does it take to correct years of bad posture?
Correcting years of poor office work posture takes time and patience. Consistency is key; daily practice is more effective than infrequent, longer sessions. Most people feel some relief within a few weeks. However, re-training neuromuscular patterns that have developed over years takes time. The gradual process involves becoming aware of your posture, strengthening supportive muscles, and stretching tight ones until good posture feels natural. With consistent effort, most people see significant improvements in 6-12 weeks.
Can a standing desk solve all my posture problems?
Standing desks are useful tools, but not a magic bullet. It's easy to adopt poor standing posture, such as leaning on one hip or hunching. The real benefit is alternating positions, as your body needs movement. Proper standing posture is just as important as proper sitting posture: distribute weight evenly, keep knees soft, shoulders relaxed, and core engaged.
Is it normal to feel some discomfort when first correcting my posture?
Yes. When you start correcting your office work posture, you're activating muscles that have been underused, which can cause some initial discomfort. Think of it like the soreness after a new workout. It's important to differentiate between good and bad pain. Good discomfort is mild muscle fatigue or soreness. Bad pain is sharp, shooting, or involves numbness and tingling.
When should you seek help? If discomfort persists for weeks, worsens, or feels sharp, consult a physical therapist to ensure you're making changes safely and effectively.
Take Control of Your Comfort and Health
Improving your office work posture is about more than sitting up straight; it's about reclaiming your energy, comfort, and quality of life. Prioritizing posture is an investment in feeling better every day.
The change can be remarkable: no more backaches or tension headaches, and more energy to enjoy your evenings instead of feeling drained. The benefits include reduced pain in your back, neck, and shoulders. You'll also experience increased energy levels as your body works more efficiently, and improved focus without the distraction of discomfort.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we've seen these changes firsthand. Our approach is not about quick fixes; we empower you with the knowledge and tools for lasting change.
We meet you where you are, assessing your posture, workstation, habits, and pain patterns to understand your unique situation. We don't just treat symptoms; we help you understand the why behind your discomfort and provide practical, real-world strategies you can stick with.
Ready to finally feel comfortable at your desk? Learn more about how ergonomic physical therapy in Brooklyn can transform your workday. Your future self will thank you for taking this step today.
Joint Effort – Physical Therapy Tips for Arthritis Management
Why Physical Therapy is Essential for Managing Arthritis Pain

Physical therapy for arthritis is an evidence-based approach that helps reduce pain, improve joint function, and restore mobility. It strengthens muscles around affected joints, reduces stiffness, and teaches you safe movement to prevent further damage, often without relying on medication or surgery.
Quick Overview: How Physical Therapy Helps Arthritis
- Pain Relief: Manual therapy and targeted exercises reduce joint pain and inflammation
- Improved Mobility: Gentle stretching and movement restore range of motion
- Stronger Support: Strengthening exercises build muscle around joints for better stability
- Better Function: Learn proper body mechanics for daily activities
- Reduced Medication: Studies show PT can be more effective than steroid injections for knee arthritis
- Delayed Surgery: Many patients avoid or postpone joint replacement with consistent therapy
Research confirms that exercise and physical therapy can ease rheumatoid arthritis symptoms. A 2020 study even found that PT was more effective than steroid injections for reducing pain and disability in people with knee osteoarthritis.
Arthritis doesn't have to control your life. With the right approach, you can maintain an active lifestyle and continue doing the things you love.
I'm Lou Ezrick, founder of Evolve Physical Therapy. With nearly two decades of experience in manual therapy and chronic pain management, I've helped thousands use physical therapy for arthritis to regain active lifestyles without surgery or long-term medication.
Understanding Arthritis: More Than Just Joint Pain
Arthritis is more than just achy joints. It's an umbrella term for over 100 conditions that cause joint inflammation and pain. What they all share is their ability to make your joints hurt, swell, and feel stiff.
The impact of chronic joint pain extends beyond physical discomfort, affecting mood, sleep, and quality of life. The CDC notes a strong link between arthritis and mental health issues like anxiety and depression.
This is why physical therapy for arthritis takes a comprehensive approach—we're not just treating your joints, we're helping you reclaim your whole quality of life.
The Two Most Common Types of Arthritis
Understanding which of the two most common types of arthritis you have helps determine the best treatment approach.
Osteoarthritis (OA) is the common "wear and tear" type. Over time, the protective cartilage in joints breaks down, causing bones to rub together. This results in pain, stiffness, and a grinding sensation. It typically affects weight-bearing joints like knees and hips, plus hands and spine.
Rheumatoid arthritis (RA) is an autoimmune disease. The body's immune system mistakenly attacks the joint lining (synovium), causing widespread inflammation and damage. RA often affects the same joints on both sides of your body and can impact other organs too.
Recognizing the Symptoms
Arthritis symptoms vary, but there are some telltale signs to watch for.
Morning stiffness is a classic sign, especially if it lasts over 30 minutes. Joints can feel immobile upon waking.
Pain with activity (or at rest) is common, along with joint tenderness where even light pressure hurts.
Other symptoms include swelling, redness, warmth, reduced flexibility, and a grating sensation during movement.
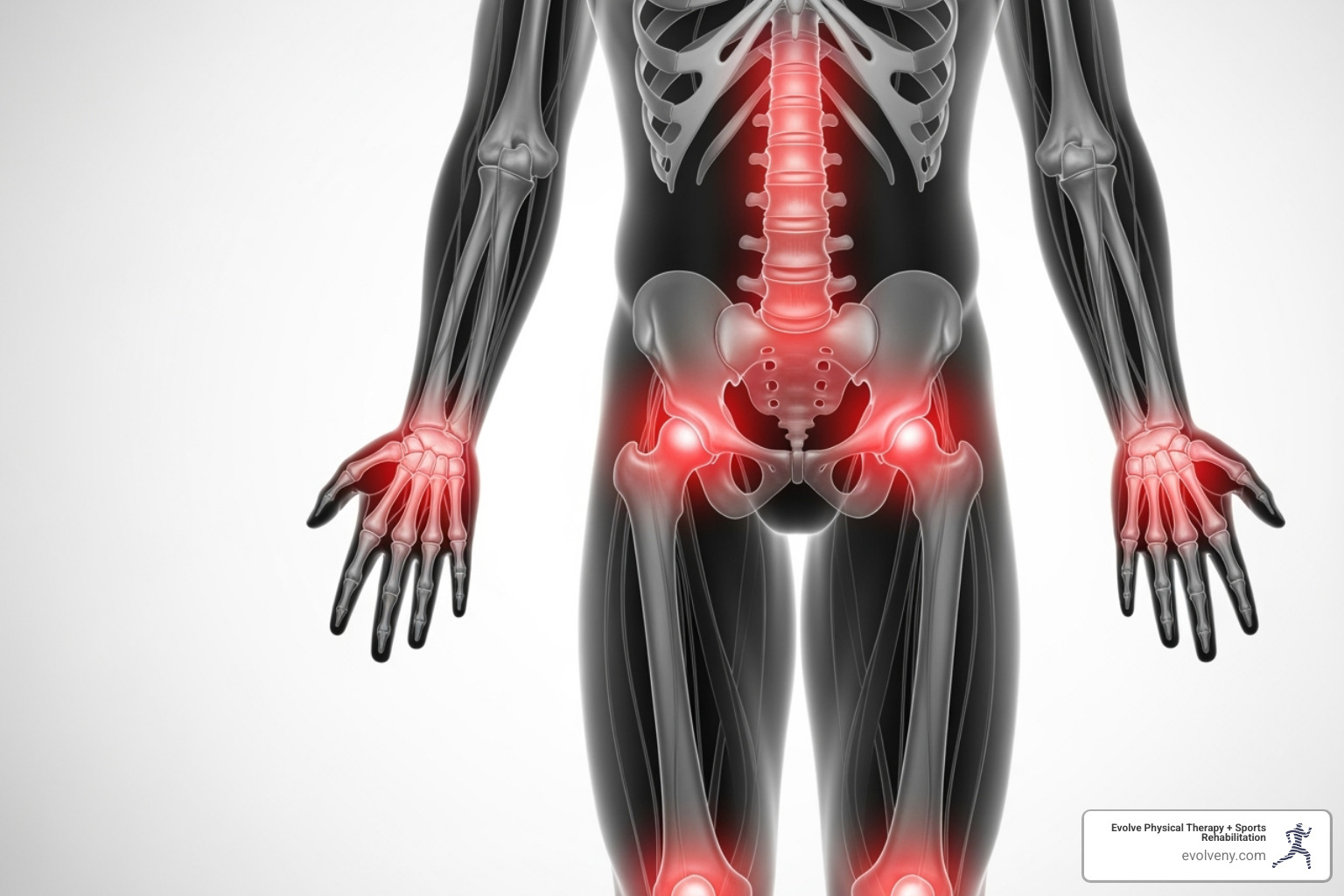
These symptoms can turn simple daily tasks into major challenges. But you don't have to accept this as your new normal. Physical therapy for arthritis can help you regain control and get back to doing the things you love.
The Role of Physical Therapy for Arthritis: A Proven Approach
When arthritis affects your daily life, physical therapy for arthritis offers a proven, hands-on approach to tackle pain at its source. It helps you regain the activities you love, often without relying on medication or surgery.
At Evolve Physical Therapy, we've seen countless patients learn to move with confidence again. Our approach focuses on pain reduction, improved function, and increased strength, helping you delay or avoid surgery.
Like fixing a car's alignment to prevent further damage, physical therapy addresses the root causes of your pain, such as movement patterns, muscle imbalances, and joint restrictions.

Primary Goals of a PT Program
When you start working with us, our primary goals are to restore joint use, strengthen supporting muscles, maintain your fitness, and preserve your ability to do daily activities. Through patient education and self-management strategies, we empower you to protect your joints while staying active.
How PT Complements Other Approaches
Research shows that physical therapy is a first-line, evidence-based treatment for hip and knee osteoarthritis, meaning it should often be the first treatment you try.
A 2019 study found that supervised, active treatment—including physical and exercise therapy—is the most effective initial approach for knee and hip osteoarthritis. This doesn't mean we ignore other treatments, but rather that physical therapy for arthritis works alongside your medical care to improve its effectiveness.
While pain medication might offer temporary relief, physical therapy addresses why you're having pain in the first place. We improve how your body moves, strengthen weak areas, and teach you strategies for long-term success. Many of our patients find they need fewer medications as their strength and function improve.
The beauty of this approach is that it puts you in control. Instead of just managing symptoms, you're actively working toward long-term improvement.
What to Expect from Your Arthritis Physical Therapy Plan
Starting physical therapy for arthritis can feel daunting, but we make the process straightforward. Your first visit is the beginning of a partnership focused on helping you move better and feel stronger.
Initial Evaluation
Your journey begins with a comprehensive evaluation. We'll conduct a posture assessment to find imbalances, perform strength testing on muscles around the joints, and use range of motion measurement to identify stiffness. A balance evaluation and movement analysis of daily tasks like walking help us spot problematic patterns. Based on these findings, we create a personalized treatment plan custom to your condition and goals.
What a Typical Physical Therapy for Arthritis Plan Involves
Your plan will combine several proven techniques. Manual therapy uses hands-on methods like joint mobilization to restore movement. Therapeutic exercises are selected to strengthen supporting muscles and improve flexibility. We may use modalities like heat and cold therapy for relief. Crucially, we provide education on proper body mechanics to protect your joints during daily tasks and a home exercise program to ensure your progress continues outside the clinic.
The PT's Role in Assistive Devices and Home Modifications
Our therapists can recommend assistive devices to make life easier and safer. This might include a walker or cane for stability, shoe inserts for better alignment, or splints or braces for joint support.

Beyond devices, we also provide ergonomic setup advice, suggesting simple home modifications like grab bars in the bathroom, cushioned mats in the kitchen, or an ergonomic chair at your desk to reduce daily joint stress.
Finding the Right Specialist for Physical Therapy for Arthritis
Choosing the right physical therapist is key. Look for a licensed professional with experience treating arthritis and good communication skills. At Evolve Physical Therapy, our one-on-one approach ensures you receive individualized, hands-on care. With locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, quality arthritis care is convenient. Ready to start? Find a qualified physical therapist at Evolve Physical Therapy and learn how we can help you reclaim your active lifestyle.
Safe and Effective Exercises for Arthritis Relief
Movement is medicine for arthritis, but exercising with joint pain can feel daunting. The right physical therapy for arthritis exercises are designed to reduce pain and stiffness, not worsen them.
The key is consistent, low-impact exercise that's gentle on your joints. Even 10-15 minutes of daily movement can make a huge difference. Before starting, always warm up properly for 5-10 minutes, and don't skip the cool-down period with gentle stretches afterward.
Can Physical Therapy Make Arthritis Worse? Safety First!
A common concern is whether PT can worsen arthritis. When done correctly under professional guidance, physical therapy for arthritis is designed to improve your symptoms. You may feel mild muscle soreness, which is normal, but sharp pain or increased swelling is a sign to stop. The "no pain, no gain" mantra is a myth for arthritis; your safety is the priority.
During arthritis flare-ups, we modify your routine to focus on gentle movements. Rest days are also essential for recovery. A physical therapist provides professional guidance to ensure you exercise safely and effectively, and the CDC offers excellent general exercise safety tips.
Exercises for Specific Joints
Your physical therapist will create a customized plan. Here are some examples of gentle exercises:
- For knee pain: Sit-to-stand exercises (rising from a chair without using hands) and leg lifts while lying down strengthen the muscles supporting the knee.
- For hip pain: Clamshells (lying on your side, lifting your top knee) and standing kickbacks help engage the glutes and improve hip strength.
- For hands and fingers: A 2015 study showed daily hand exercises improve function. Try making gentle fists, doing individual finger bends, and making small thumb circles.
- For neck stiffness: Shoulder rolls and gentle head tilts (ear toward shoulder) can release tension and ease discomfort.
General Activities to Ease Arthritis Pain
Incorporating enjoyable low-impact activities into your routine is key.
- Walking is highly accessible and keeps joints moving.
- Bicycling (stationary or outdoor) promotes joint lubrication without impact.
- Tai Chi improves balance and flexibility with slow, meditative movements.
- Gentle yoga can improve flexibility, strength, and balance; look for arthritis-specific classes.
- Aquatic therapy and water aerobics are game-changers. The water's buoyancy supports your body, reducing stress on joints and allowing for pain-free movement.
Working with an experienced physical therapist is valuable because we help you find the right combination of exercises and activities that fit your lifestyle and goals.
Frequently Asked Questions About Arthritis Management
We want to address common questions to help you feel more confident about starting physical therapy for arthritis.
How often should I see a physical therapist for arthritis?
The frequency of your visits is personalized. During the initial phase, most patients visit two to three times per week for close monitoring, hands-on therapy, and proper exercise instruction. Our goal is to transition you to a home program, so visits will decrease as you gain confidence and independence.
Periodic check-ins every few months are valuable for updating your program and addressing new concerns. During flare-ups, we can quickly modify your plan to help you manage symptoms. Consistency with your home program is the key to long-term success.
How is physical therapy for arthritis covered by insurance or Medicare?
Most insurance plans recognize physical therapy for arthritis as a medically necessary treatment.
- Private insurance typically covers PT, but plans may have session limits, co-pays, or deductibles. It's best to call your provider to understand your specific benefits.
- Medicare coverage varies. As detailed by sources like AARP, Medicare Part A and Part B coverage details show Part A covers inpatient therapy, while Part B covers outpatient services like ours. Part B usually pays 80% after your deductible is met.
Across all plans, treatment must be deemed a medical necessity. Our administrative team can help you steer your coverage.
What is the difference between physical therapy and occupational therapy?
This is a great question, as both are helpful for arthritis. The main difference is their focus:
- Physical Therapy (PT) focuses on how your body moves. We work to improve strength, range of motion, and mobility to reduce pain and improve overall function. A PT helps your knee move better so you can walk without pain.
- Occupational Therapy (OT) focuses on how you perform daily tasks. An OT helps you adapt activities and environments, often using assistive devices or improving fine motor skills. An OT might teach you how to get dressed more easily or recommend ergonomic kitchen tools.
While we focus on PT at Evolve, we work closely with OTs to provide comprehensive care.
Take Control of Your Joints and Your Life
Living with arthritis doesn't mean accepting a life of pain or giving up activities you enjoy. Physical therapy for arthritis offers a path to proactive management, empowering you to take control.
The benefits are real: pain reduction, improved function, increased strength, and empowerment through movement. By understanding your body's needs, you can break free from the cycle of pain and stiffness.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach ensures your treatment is as unique as you are. We don't use cookie-cutter solutions; our therapists work with you to guide and adjust your plan as you improve.
Long-term success in managing arthritis is a marathon, not a sprint. It requires consistency and a partnership with your physical therapist. We're here to support you through every step of your health journey.
Whether it's stiffness in your hands or pain in your knees or hips, there is hope. Our team across Brooklyn—in Marine Park, Park Slope, Gravesend, Mill Basin, and Midwood—is ready to help you write a new chapter.
Ready to take the next step? Learn more about our physical therapy services and find how we can help you move better, feel stronger, and live the life you want. Your joints—and your future self—will thank you.
Mobilize Your Shoulder Like a Pro – Mobilization with Movement Explained
Why Shoulder Pain Doesn't Have to Limit Your Active Life

How to do mobilization with movement for the shoulder is a pain-free manual therapy technique that combines therapist-applied joint glides with your active movement to restore normal shoulder function. Here's the quick answer:
Basic MWM Steps:
- Assessment - Therapist identifies your painful shoulder movement
- Glide Selection - Usually a posterior or posteroinferior glide of the humeral head
- Application - Therapist applies sustained glide while you actively move your arm
- Pain-Free Rule - Movement must remain completely pain-free
- Repetitions - Multiple pain-free repetitions to "reset" your nervous system
If shoulder stiffness is keeping you from your active life, you're not alone. Research shows MWM can improve flexion by nearly 12 degrees for frozen shoulder and over 18 degrees for general shoulder pain.
The beauty of MWM is its immediate effects; many patients experience less pain and better movement right after their first session. It works by gently correcting subtle joint alignment issues while calming your nervous system's pain response.
I'm Lou Ezrick, founder of Evolve Physical Therapy. I've spent nearly two decades helping active professionals overcome shoulder limitations using advanced manual therapy. My experience in Tel Aviv and Brooklyn has shown me how to do mobilization with movement for the shoulder effectively to get people back to their active lifestyles without medications or surgery.
What is Mobilization with Movement (MWM) and How Does It Work?
When shoulder pain stops you from reaching for a high shelf, Mobilization with Movement (MWM) can be a game-changer. Developed by Brian Mulligan, MWM is a manual therapy technique where your therapist applies a gentle, sustained glide to your shoulder joint while you actively move your arm.
Think of your shoulder as a ball in a shallow cup. Tiny misalignments, or "positional faults," can disrupt smooth movement, like a sticking door hinge. MWM corrects this by guiding the humeral head (the ball) back into its proper position as you move.
Beyond mechanics, MWM calms an overactive nervous system. When you're in pain, your brain guards the area, making things worse. The gentle pressure of MWM can override pain signals (Pain Gate Theory), activate your body's natural pain relief (descending pain inhibition), and reduce the fear that keeps you from moving. This is why MWM provides immediate relief—it resets your nervous system's alarm. If you're dealing with shoulder issues in Brooklyn, our team specializes in these advanced techniques at Shoulder Physical Therapy Brooklyn.
The Core Principles of MWM
The effectiveness of MWM lies in its core principles, which guide every session at Evolve Physical Therapy + Sports Rehabilitation.
- The Pain-Free Rule: This is non-negotiable. If you feel any discomfort, we stop and adjust. This works with your nervous system, not against it.
- Functional Movement: We focus on restoring actions you need for daily life, from reaching for a coffee mug to throwing a ball.
- Communication: Your feedback is crucial for us to fine-tune the glide, pressure, and speed. We listen to what your body tells us.
- Repetitions: Repeating the pain-free movement reinforces the correct pattern and teaches your nervous system that the movement is safe.
- Long-Lasting Results: While immediate relief is common, our goal is lasting change that enables more effective exercise and long-term improvement.
The Science Behind the Relief: Correcting Faults and Calming Nerves
MWM addresses both the mechanical and neurological aspects of shoulder problems. Mechanically, it corrects faulty humeral head alignment within the glenoid fossa (the socket). During a normal arm lift, the humeral head should glide downward and backward. If it doesn't, tissues get pinched, causing pain. MWM provides a biomechanical correction by applying an external force to guide the joint correctly as you move.
Neurologically, MWM calms an overactive sympathetic nervous system. Pain can cause your brain to treat normal movements as threats, creating a cycle of fear and guarding. By demonstrating that movement can be pain-free, MWM achieves fear-avoidance reduction. This combination of mechanical correction and nervous system reset is supported by research, with studies like this Efficacy of MWM for shoulder conditions: a systematic review showing significant improvements in pain and range of motion.
How to Do Mobilization with Movement for the Shoulder to Improve Flexion

If lifting your arm overhead is painful or stiff, how to do mobilization with movement for the shoulder can restore that smooth, pain-free reach. Your highly mobile shoulder joint requires precise coordination. For proper shoulder flexion, the humeral head (the ball) must glide downward and backward in the socket. When this movement, known as arthrokinematics, is disrupted, pain and struggle result. At Evolve, our hands-on approach identifies this breakdown and applies the precise correction needed.
Step 1: Finding the Right Glide for Your Shoulder
MWM begins with detective work to identify your specific movement fault. We'll ask you to perform the movement that causes trouble, noting where pain or limitation occurs. The next step is determining the optimal glide direction. For most shoulder flexion issues, a posterior or posteroinferior glide of the humeral head is effective.
Precise hand placement over your humeral head is crucial for applying the sustained, gentle force needed to correct the fault. This is not a one-size-fits-all approach; finding the specific "positional fault" requires skill and careful attention to your body's response.
Step 2: A Step-by-Step Guide on How to Do Mobilization with Movement for the Shoulder
The how to do mobilization with movement for the shoulder technique is a partnership between you and your therapist. While the therapist maintains a sustained glide on your humeral head, you actively lift your arm. The movement must be completely pain-free; if you feel any discomfort, the glide is adjusted immediately.
We guide you through 6 to 10 pain-free repetitions. Each one helps your nervous system learn that the movement is safe, relaxing its protective guarding. This nervous system reset can happen quickly, with many patients experiencing improved range and less pain after just one set. You can see a demonstration of a Posterior Glide to increase flexion here.
Can You Do This at Home? A Guide to Self-MWM

The benefits of MWM can often be continued at home with self-treatment techniques, but only after learning from a qualified therapist. A common method uses a mobilization belt secured to a sturdy object to replicate the therapist's glide. You position the belt around your upper arm near the shoulder joint to create a gentle pull.
While maintaining belt tension, you actively lift your arm, ensuring the movement remains pain-free. If you feel discomfort, adjust the belt's tension or angle. Performing these gentle repetitions multiple times throughout the day reinforces correct movement patterns and helps you maintain your progress.
However, professional guidance is essential to learn the correct setup and force. Safety first is our rule, especially for those in our Prehab for Shoulder Surgery Brooklyn program. Self-MWM extends professional care, it doesn't replace it, giving you tools to accelerate recovery between sessions.
The Evidence: Why MWM is a Top Choice for Shoulder Recovery
Patients often ask if MWM actually works. The answer is a resounding yes, backed by both clinical experience and solid research. At Evolve Physical Therapy, we use MWM because of its consistent, proven results.
The evidence is strong for common conditions like frozen shoulder, shoulder impingement syndrome, and rotator cuff pain. For rotator cuff issues, MWM is a cornerstone of our approach at Physical Therapy for Rotator Cuff.
What sets MWM apart are its immediate effects. Many patients experience significant improvement in range of motion and pain relief in a single session, as their nervous system gets the 'all clear' signal to move freely.
What the Research Says About MWM
The research is compelling. For frozen shoulder, MWM improved flexion by an average of nearly 12 degrees—a clinically significant change that makes a real difference in daily life. For general shoulder pain, the improvement was even more impressive at over 18 degrees.
Beyond the numbers, patients report significant pain reduction and functional improvement. These changes often occur within a single session, as the nervous system learns it can move without pain. This evidence is why how to do mobilization with movement for the shoulder is central to our philosophy of helping you recover as quickly and safely as possible.
Who Benefits Most from MWM?
MWM is particularly effective for certain individuals and conditions:
- Reproducible Pain: If your pain occurs with a specific movement, MWM can target the exact fault.
- Shoulder Stiffness: It works well for frozen shoulder, post-injury recovery, or general tightness.
- Athletes and Active Individuals: They benefit from the quick gains that help them return to their sport.
- Older Adults: The gentle, non-aggressive nature of the technique is highly appreciated.
- Plateaued Progress: If exercise alone isn't working, MWM can provide a breakthrough, making your exercises more effective.
MWM is versatile and can restore smooth, pain-free movement for a wide range of issues. Our team has extensive experience with various shoulder problems, as detailed in our guide on Physical Therapy for Shoulder Injuries.
Comparing MWM to Other Shoulder Therapies
How does MWM compare to other therapies?
- vs. Passive Mobilizations: Traditional mobilizations can involve pushing into discomfort. MWM's pain-free rule makes it unique and more comfortable.
- vs. Passive Treatment: The active component of MWM, where you move your own arm, creates a powerful neurological reset that passive techniques can't match.
- vs. Therapeutic Exercise Alone: MWM can be a precursor to exercise. By restoring pain-free range of motion first, it makes strengthening exercises more effective and less painful.
The speed of results is also a key advantage. MWM provides immediate improvements that boost motivation, and research shows combining MWM with exercise is more effective than exercise alone. At Evolve, we use MWM to provide immediate gains, while targeted exercises build long-term strength and stability for the best possible outcome.
Frequently Asked Questions About Shoulder MWM
After nearly two decades of helping patients with shoulder issues, I've noticed that people often have similar concerns when they first hear about how to do mobilization with movement for the shoulder. Let me address the questions that come up most often in our Brooklyn clinic.
Does MWM for the shoulder hurt?
This is the most common question, and the answer is a firm NO. If MWM causes any pain, it's not being done correctly. The pain-free principle is the golden rule. We stop and adjust at the slightest discomfort, as our goal is to work with your nervous system, not against it.
Adding pain would reinforce your brain's fear of movement. By guiding your shoulder through a pain-free range, we're resetting its pain response. Your feedback is crucial for us to fine-tune the technique, so we encourage you to speak up. Your comfort is our guide.
What are the safety considerations and contraindications?
MWM is very safe when performed by a qualified therapist after a thorough evaluation. However, it may not be appropriate for everyone.
Contraindications or conditions requiring caution include:
- Joint hypermobility or significant shoulder instability
- Recent fractures
- Active cancer in the shoulder region
- Acute inflammatory arthritis
- Severe osteoporosis (requires a modified, gentle approach)
We always conduct a comprehensive hands-on evaluation to ensure MWM is both safe and effective for you. This assessment is our first step, whether you have a new injury or are considering Rehab for Shoulder Surgery.
How many sessions are typically needed to see results?
One of MWM's biggest advantages is that most people experience noticeable improvement in their very first session, with less pain and better movement.
While this immediate improvement is encouraging, the total number of sessions for lasting change depends on your specific situation. Newer problems may resolve in a few sessions, while chronic issues take longer. Your active participation with home exercises also significantly impacts your recovery speed.
Typically, patients need 4-8 sessions to solidify their gains and learn long-term management strategies. The immediate relief from the first session is just the beginning. Our goal is to address the root cause of your dysfunction and teach you how to maintain a healthy shoulder for life.
Take Control of Your Shoulder Health Today
You don't have to accept shoulder pain as your new normal. MWM is your pathway to reclaiming an active life, offering a gentle, powerful solution that works with your body.
At Evolve Physical Therapy + Sports Rehabilitation, we combine evidence-based MWM with personalized, comprehensive care. Our approach goes beyond just the technique; we take a holistic view, examining how posture, habits, and daily movements contribute to your pain. Our hands-on philosophy means we take the time to understand your unique story and craft a treatment plan that fits your goals.
During your first session, you'll likely experience the immediate relief of pain-free movement as your nervous system learns that it's safe to move again. Our team serves the vibrant communities of Brooklyn NY, Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, and we're committed to getting you back to the activities you love.
Don't let another day pass. Your shoulder health is an investment in your future. Schedule your comprehensive shoulder evaluation today and let our expert care restore your freedom of movement. Your journey back to pain-free living starts now.
Straight Talk on Proper Posture at Work
Why Your Desk Job Might Be a Pain in the Neck

Proper posture at work is more important than ever. Here's what you need to know:
Key Elements of Proper Workplace Posture:
- Feet flat on floor or footrest
- Knees at 90 degrees, level with or below hips
- Back fully supported with lumbar curve maintained
- Shoulders relaxed, not rounded or hunched
- Elbows at 90-120 degrees, close to body
- Monitor at eye level, arm's length away
- Wrists straight and neutral while typing
With over 80% of U.S. jobs being sedentary, we're spending more time than ever at desks. This has led to a rise in neck pain, back strain, and headaches.
Your body isn't designed to sit in one position for 8+ hours. Poor posture adds stress to your spine; for every inch your head moves forward, an additional 10 pounds of weight is placed on your neck. That's like carrying a bowling ball on your shoulders all day.
The good news is that small adjustments to your workspace and habits can make a huge difference. Proper posture aligns your bones and joints, reduces muscle fatigue, and can boost your energy.
I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy in Brooklyn. With nearly two decades of experience, I specialize in helping patients overcome chronic pain through ergonomic solutions and a focus on proper posture at work. I've seen how simple workspace modifications can eliminate years of discomfort and prevent future injuries.
The High Cost of Slouching: Understanding the Risks and Rewards
If you're sitting with rounded shoulders and your head jutting forward, you're not alone—and you're likely feeling the effects. Poor posture creates real damage, setting you up for chronic back pain, persistent neck strain, and tension headaches.
Internally, your lung capacity decreases when you slouch, and your digestive system gets compressed, hindering its function. The health risks of prolonged sitting are significant.
The good news is that proper posture at work can reverse this. Sitting tall with an aligned spine gives your body increased energy, improved confidence, and reduced wear and tear on your joints. Everything simply works better.
If you're dealing with persistent headaches, know that physical therapy can help with headaches, often more effectively than you might expect.
The Domino Effect of Poor Posture
Poor posture creates a cascade of problems. Forward head posture is the most common issue I see in my Brooklyn practice. When your head moves forward just one inch, it adds 10 pounds of extra weight for your neck muscles to support. Over an 8-hour workday, that's like carrying a bowling ball on your shoulders.
This forward head position leads to rounded shoulders. Your chest muscles tighten while your upper back muscles become stretched and weak. This misalignment affects your entire spine, flattening its natural curves and putting excessive pressure on your spinal discs. These cushions between your vertebrae can break down under constant compression, leading to nerve compression and even sciatica—that sharp pain that travels down your leg.
If you're experiencing this, physical therapy for upper back pain can help break the cycle and restore proper alignment.
The Surprising Benefits of Sitting Tall
When you correct your posture, the benefits go beyond pain avoidance. Your muscles work efficiently, leading to less fatigue and more energy to focus on your work. Good posture also decreases stress on your ligaments, the tough tissues that hold your joints together.
Proper posture also improves your circulation and digestion. When you're not slouched, blood flows more freely, and your internal organs have the space they need to function properly. Many of my patients report feeling more alert and having better digestion after improving their workplace posture.
Finally, good posture makes you look more professional and feel more self-assured. Research shows that people who sit up straight feel more confident and perform better in challenging situations. Every minute you spend in good posture is an investment in your long-term health and daily comfort.
The Ergonomic Blueprint for Proper Posture at Work
Creating an ergonomic workspace that supports proper posture at work doesn't require a complete overhaul. It's about making smart adjustments that work with your body.
Workplace ergonomics is the science of making your workspace fit you. Instead of contorting your body to a desk setup, your environment should adapt to support your natural alignment. This approach prevents the nagging aches that develop from years of poor positioning.
The goal is to achieve neutral body positioning, where your joints are aligned and stress on your tissues is minimized. This allows you to work with less fatigue and a lower risk of musculoskeletal problems. Since every body is different, your ideal setup will be unique. Customizing your space is key, a topic we explore in our article on Ergonomics and Physical Therapy explained.

Achieving Proper Posture at Work with Your Chair
Your office chair is the foundation of good posture. Start with chair height: your feet should rest flat on the floor or a footrest. Your knees should be at or slightly below hip level, creating about a 90-degree angle. This keeps your hips open and prevents pressure on your thighs.
Next, focus on lumbar support. Your chair's backrest should cradle the natural inward curve of your lower back. If your chair lacks this feature, a small pillow or a rolled towel can provide the necessary support.
Position your buttocks all the way back against the chair, with your weight distributed evenly across both sitz bones. This neutral pelvis position supports your spine's natural curves. Adjust your armrests so your arms rest gently, keeping your shoulders relaxed and elbows close to your body. Finally, ensure there are two to three finger-widths of space between the front of the seat and the back of your knees to promote good circulation.

Monitor and Screen Placement
Poor monitor placement is a major cause of neck pain and headaches. Your monitor should be directly in front of you, an arm's length away (about 20-40 inches). The top of the screen should be at or slightly below eye level, encouraging a natural, slightly downward gaze.
If you wear bifocals, you may need to lower your monitor slightly to avoid tilting your head back. Position your monitor to avoid glare from windows or lights, using an anti-glare screen if needed. For laptop users, the solution is to use a laptop stand to raise the screen to eye level and add an external keyboard and mouse. This setup is crucial for preventing neck strain. For more details, see our article on ideal computer posture.
Keyboard and Mouse Positioning
Proper keyboard and mouse placement prevents wrist pain and shoulder tension. When typing, your wrists should be straight and neutral, not bent. Your forearms should be parallel to the floor, with elbows at a 90- to 120-degree angle and close to your sides. Position the keyboard 4-6 inches from the desk edge to give your wrists a place to rest during breaks, but let your hands float above the keyboard while actively typing.
Your mouse should be next to your keyboard, easily reachable without stretching. Keep your wrist straight and your upper arm relaxed. Avoid resting your elbow on hard surfaces to prevent nerve compression. If you're on the phone frequently, use a headset or speakerphone instead of cradling the phone between your ear and shoulder. Keep frequently used items within easy reach to minimize twisting and stretching.
Beyond the Setup: Habits and Stretches for All-Day Comfort
An ergonomic setup is only half the battle; your body is designed to move. At Evolve Physical Therapy, we often say movement is medicine. Staying in any single position for too long—even with perfect posture—causes muscles to tighten and blood flow to slow.
The solution is to take frequent breaks. Get up and move for one to two minutes every 30 minutes, or for 10 minutes every hour. These mini-breaks are essential for preventing muscle shortening and energy crashes. A quick walk, standing up to stretch, or chatting with a colleague can work wonders. Also, try the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds to rest your eyes and neck.
Consider taking phone calls while standing or walking. The goal is to change positions frequently throughout the day to maintain proper posture at work.
Simple Stretches to Relieve Tension
Try these desk-friendly stretches to reset your posture and release tension:
Shoulder Blade Squeeze is a great way to strengthen muscles that fight rounded shoulders. Sit tall and squeeze your shoulder blades together as if holding a pencil between them. Hold for 5-10 seconds and repeat 5-10 times. You can find detailed instructions for this Shoulder Blade Squeeze exercise.
Neck tilts relieve stiffness from screen time. Gently tilt your head, bringing your ear toward your shoulder. Hold for 15-20 seconds on each side. Follow with gentle up-and-down nods and side-to-side turns.
The chin tuck is highly effective for forward head posture. Pull your chin straight back as if making a double chin, keeping your head level. You should feel a stretch at the base of your skull. Hold for 5 seconds and repeat 10-15 times.
Torso twists mobilize your spine. While seated with feet flat, gently twist your upper body to one side, using the chair for support. Hold for 15-20 seconds, then switch sides.
Wrist and finger stretches are crucial for typists. Extend one arm, palm down, and use your other hand to gently pull your fingers back. Hold for 15-20 seconds. Flip your palm up and repeat. Finish by rotating your wrists.
These movements, done regularly, prevent tension buildup. If you have persistent neck issues, our team specializes in physical therapy for neck pain and injuries.
Habits for Maintaining Proper Posture at Work
Building good postural habits requires consistency. These daily practices will help make proper posture at work feel natural.
- Regular posture checks: Set a reminder to check your posture hourly. Are your feet flat? Shoulders relaxed? Head balanced?
- Avoid crossing your legs: This throws off spinal alignment and can reduce blood flow. Keep both feet flat on the floor or a footrest.
- Ensure even weight distribution: Sit evenly on both hips to keep your pelvis neutral and balanced.
- Keep items within easy reach: Arrange your desk so you don't have to constantly stretch or twist for frequently used items.
- Stay hydrated: Dehydration can lead to fatigue and slumping. Plus, trips to get water provide natural movement breaks.
Frequently Asked Questions about Workplace Posture
At Evolve Physical Therapy, we hear many questions about workplace posture. Here are answers to the most common concerns.
What if my desk and chair aren't adjustable?
Many people work with basic furniture, but you don't need an expensive setup to achieve proper posture at work. Simple solutions can be very effective.
- For height issues: If your chair is too low, use a sturdy box or stack of books as a footrest to get your knees to a 90-degree angle. If your chair is too high, a firm cushion can lift you up.
- For lumbar support: A rolled-up towel or a small pillow placed in your lower back's curve works wonders.
- For monitor height: Stack books or paper reams under your monitor to bring it to eye level. For laptop users, a laptop stand paired with an external keyboard and mouse is critical for neck health.
Even small adjustments can significantly improve how you feel at the end of the day.
Is a standing desk a better option?
Standing isn't automatically better than sitting; what matters most is variety. Your body needs to change positions. Staying in any single posture for too long, whether sitting or standing, creates problems. The key is to alternate between sitting and standing throughout the day.
When you stand, maintain proper posture: keep shoulders relaxed, engage your core, and distribute your weight on the balls of your feet. Your monitor still needs to be at eye level. Standing all day can cause its own issues like leg fatigue and back pain, so an anti-fatigue mat can help. Listen to your body and switch positions when you feel uncomfortable.
A standing desk is a tool to introduce variety, not a cure-all to replace one static position with another.
How long does it take to correct bad posture?
The timeline for correcting posture is unique to each individual and depends on consistency. You are re-training your muscle memory and strengthening muscles that have been underused for years. When you've slouched for a long time, your tissues adapt, so sitting with proper alignment might feel strange or cause mild muscle fatigue at first. This is a normal sign that your muscles are adapting.
With consistent effort—workspace adjustments, movement breaks, and stretches—you can feel improvements within a few weeks. More significant changes in muscle strength and habits typically take a few months to solidify.
If you have persistent pain or feel you're not making progress, professional help is recommended. At Evolve Physical Therapy, we can assess your specific imbalances and create a personalized plan. An expert evaluation of your workspace and movement patterns can accelerate your progress. You didn't develop poor posture overnight, so be patient as you work toward lasting change.
Conclusion: Make Good Posture Your New Habit
Achieving proper posture at work is a journey of small, simple changes that create a big impact. You don't need to overhaul your office overnight. Start with one adjustment, like raising your monitor, and once it becomes a habit, add another.
The benefits extend beyond avoiding neck aches. Proper alignment leads to increased energy, improved confidence, and reduced joint wear over the years. These long-term health advantages, from better circulation to a lower risk of chronic pain, make every effort an investment in your future self.
Think of good posture as a skill. At first, it requires conscious effort, but with consistent practice, it becomes automatic. Your body will start to prefer an aligned position.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we understand that everyone's body and workspace are unique. Our hands-on approach helps you implement proper mechanics in your daily life. We've helped countless professionals transform their work experience with targeted ergonomic solutions and personalized plans.
Whether you're dealing with pain or aiming for prevention, we're here to help. For a personalized plan to improve your workspace, explore our ergonomic physical therapy services in Brooklyn. Let us help you make proper posture at work your new, healthy habit.
Move It or Lose It – Physical Therapy Solutions for Adults
Why Physical Therapy is Essential for Adult Health and Recovery

Physical therapy for adults helps people recover from injuries, manage chronic conditions, and maintain optimal physical function. Whether you're dealing with persistent pain, recovering from surgery, or looking to prevent future injuries, physical therapy offers evidence-based solutions custom to your specific needs.
Physical therapy for adults addresses:
- Pain management - Natural relief without relying on medications
- Injury recovery - Faster healing from accidents, surgeries, or overuse
- Chronic conditions - Managing arthritis, neurological disorders, and age-related issues
- Prevention - Strengthening weak areas before they become problems
- Mobility improvement - Restoring range of motion and functional movement
- Balance training - Reducing fall risk, especially important as one in four adults over 65 falls annually
As movement specialists, physical therapists use their advanced training to create personalized plans combining hands-on therapy, targeted exercises, and patient education. The recovery process typically follows five phases: pain relief, introducing movement, strengthening, functional retraining, and long-term prevention. Most treatment plans last four to 12 weeks, with one to three sessions per week.
I'm Lou Ezrick, founder of Evolve Physical Therapy. With nearly two decades of experience, my approach to physical therapy for adults emphasizes hands-on manual therapy and individualized care plans that address the root cause of your symptoms for lasting relief.
Why Consider Physical Therapy for Adults? Opening Up Core Benefits
As adults, we often accept aches and stiffness as a normal part of aging. But physical therapy for adults offers a better way to live. It's not just for injury recovery; it's about reclaiming your life from chronic pain or physical limitations. Physical therapy can help you move freely and confidently again, without being constantly reminded of pain in your back, knees, or shoulders.
The benefits reach far beyond simply "fixing what's broken." Pain management becomes possible without relying on medications. Improved mobility means you can bend down to pick up your grandchild without wincing. Injury prevention helps you stay active, while avoiding surgery can save you from invasive procedures. Many adults also build improved strength and endurance, and better balance becomes crucial as we age—the CDC reports that falls are the leading cause of injury deaths in older adults. For those recovering from surgery, post-surgery recovery through physical therapy can mean the difference between a good outcome and a great one.

Pain Management Without Opioids
Chronic pain affects every part of your life, from sleep to relationships. Physical therapy offers a powerful alternative to managing pain without a reliance on prescription medications. Instead of masking symptoms, we focus on treating the source of pain. A tight hip might be causing your back pain, or weak glutes could be the real culprit behind your knee discomfort.
Chronic pain relief and acute pain reduction happen through natural therapies that work with your body's healing processes. We use targeted exercises to strengthen weak muscles and improve flexibility, while manual therapy techniques like massage and joint mobilization reduce stiffness. Research supports this approach; a study found PT as effective as surgery for lumbar stenosis pain. We also use modalities like heat, ice, and e-stim to reduce inflammation and promote healing, teaching you how to manage pain for the long term.
Improved Mobility, Balance, and Injury Prevention
Physical therapy can help you regain the effortless movement you once had. Restoring function is about getting back to the activities that matter to you. We work on increasing range of motion in stiff joints and strengthening muscles that have weakened from disuse or injury.
Fall prevention strategies are vital for adults of all ages. We improve your coordination and balance through targeted training, helping you feel more confident and steady. We also focus on pre-habilitation to prevent injuries, identifying and addressing weak spots before they become problems. This is especially valuable if you're planning surgery or starting a new exercise program. We also provide home safety education, as simple changes like securing rugs or improving lighting can prevent accidents.
A Spectrum of Care: Conditions Treated and Types of PT
Physical therapy for adults is incredibly adaptable, offering solutions for everything from a weekend sports injury to the complex challenges of a neurological condition. We treat adults from all walks of life, whether it's an executive with chronic neck pain, a grandparent with arthritis, or a stroke survivor working to regain independence.
Our goal is to optimize how your body moves and functions. We address a full spectrum of adult health challenges, including musculoskeletal injuries, neurological conditions, age-related issues, post-operative care, and sports injuries.

Common Conditions Physical Therapy Can Treat in Adults
Our philosophy is simple: if it affects how you move, we can likely help. Some of the most common conditions we treat include:
- Back and neck pain: Often from poor posture, injury, or daily wear and tear.
- Arthritis: We help manage joint pain and stiffness to keep you active.
- Rotator cuff tears: Common in active adults, these injuries respond well to manual therapy and targeted exercises.
- Neurological conditions: We offer specialized care for stroke recovery and Multiple Sclerosis. Our Parkinson's disease program includes Rock Steady Boxing, a unique approach featured on NBC News for its effectiveness.
- Joint replacements: We guide you through recovery after a hip, knee, or shoulder replacement, helping you return to activities with less pain.
- Other conditions: We also treat carpal tunnel syndrome, COPD, vertigo, fibromyalgia, osteoporosis, and various sports injuries.
Because every condition affects each person differently, our approach is always personalized to your specific needs and goals.
Specialized Types of Physical Therapy
Different types of physical therapy focus on specific areas of expertise, ensuring you receive care from a specialist who understands your condition.
- Orthopedic PT: Focuses on the musculoskeletal system—bones, muscles, and joints. It's the starting point for back pain, sports injuries, and post-surgical recovery.
- Geriatric PT: Addresses the unique challenges of aging, focusing on maintaining independence through balance training, strength work, and managing chronic conditions.
- Neurological PT: Requires specialized knowledge of how the brain and nervous system affect movement, helping patients recovering from a stroke or managing Parkinson's disease.
- Sports PT: Keeps you in the game by helping you recover from and prevent injuries related to your specific sport or activity.
- Cardiovascular and pulmonary PT: Helps when heart or lung conditions, like COPD or recovery from a heart attack, limit your activity.
- Pelvic floor rehabilitation: Addresses common but sensitive issues like incontinence or pelvic pain.
- Vestibular therapy: Tackles dizziness and balance problems caused by inner ear issues.
You don't have to figure out which type you need. We'll assess your situation and create a comprehensive care plan, often combining approaches to meet your needs.
Your Path to Recovery: What to Expect and How to Choose a Therapist
Starting physical therapy can feel overwhelming, but at Evolve Physical Therapy, we make the process straightforward. We partner with you on your recovery journey, guiding you every step of the way.
Your journey begins with a thorough initial evaluation where we listen to your concerns and create a personalized treatment plan. During sessions, you'll experience our signature hands-on therapy approach, where we work directly with you using manual techniques. Patient education is a key component; we want you to understand your condition. You'll also receive a customized home exercise program with carefully chosen movements to accelerate your progress.
Preparing for Your First Visit
A little preparation for your first visit can go a long way.
- Gather your medical history: Bring any doctor's notes, imaging reports (X-rays, MRIs), and a current list of medications.
- Wear comfortable clothing: Choose loose-fitting clothes that allow you to move freely and give us access to the area we need to examine.
- List your symptoms and goals: Note when your symptoms started, what makes them better or worse, and how they affect your daily life. Think about what you want to achieve, like walking without pain or returning to a favorite sport.
- Ask questions: We encourage you to be curious and engaged. The more you understand, the better your results will be.
How to Choose the Right Physical Therapist for Adults
Choosing the right physical therapist is a critical decision for your recovery.
- Check credentials and licensing: Ensure your therapist has a Doctor of Physical Therapy (DPT) degree and is licensed in your state. You can use the APTA's Find a PT tool for a list of qualified therapists.
- Look for experience with your condition: A therapist specializing in your specific issue, whether it's a neurological condition or a sports injury, can provide more targeted care.
- Seek a hands-on approach: A therapist who uses manual techniques to assess and treat your condition can often achieve better results than one who only supervises exercises.
- Evaluate communication style: A great therapist listens carefully, explains things clearly, and makes you feel comfortable asking questions.
- Insist on personalized care plans: Avoid clinics with cookie-cutter programs. Your treatment should be built around your specific condition and goals.
Physical therapy for adults works best as a partnership. We bring the expertise, but your active participation is what makes the magic happen.
Empowering Your Recovery: Common At-Home Exercises
Your physical therapy sessions are just the beginning. Real progress happens when you continue with a personalized home exercise program, which helps maintain and build on the work we do in the clinic. You don't need fancy equipment—just a comfortable space and commitment. Consistency is your secret weapon; even 10-15 minutes daily can make a remarkable difference.
Your program will include stretching for flexibility, strengthening exercises for stability, and posture correction techniques. We'll teach you proper form and provide modifications for your needs.

Simple Stretches for Flexibility
Stretching releases tension, reduces stiffness, and keeps joints moving freely. Hold each stretch for 30-45 seconds, feeling a gentle pull, not pain.
- Hamstring Stretch: Ideal for those who sit frequently. Lie on your back with knees bent. Raise one leg, clasping behind the knee. Gently pull it toward your chest, then slowly straighten the knee until you feel a stretch in the back of your thigh.
- Piriformis Stretch: Helpful for sciatica-like symptoms. On your back with knees bent, cross one ankle over the opposite knee. Gently pull that thigh toward your chest to feel a stretch deep in your glute.
- Standing Hip Flexor Stretch: Targets the front of the hip. Facing a sturdy surface, place one foot on it with your knee bent. Shift your weight forward to feel the stretch in the front of your hip.
Foundational Strengthening Exercises
Building strength supports your body during daily activities. Aim for 10-20 repetitions, focusing on quality over quantity.
- Bridges: Strengthens glutes, hamstrings, and core. Lie on your back with knees bent, feet flat. Squeeze your glutes and lift your pelvis to form a straight line from shoulders to knees. Hold for 3-5 seconds, then lower slowly, keeping knees aligned over ankles.
- Clamshells: Excellent for hip stability. Lie on your side with knees bent and stacked. Keeping your ankles touching, lift your top knee toward the ceiling without letting your pelvis roll back.
- Straight Leg Raises: Builds hip flexor and quad strength. Lie on your back with one knee bent. Keeping the other leg straight, lift it to about 45 degrees, then lower slowly.
To add variety, consider using resistance bands for added challenge. These affordable tools are perfect for home workouts. Combining these exercises with good posture habits will make every movement more efficient and less likely to cause pain.
Frequently Asked Questions about Adult Physical Therapy
Starting physical therapy for adults can bring up many questions. Here are answers to the ones we hear most often at our Brooklyn clinics.
Do I need a doctor's referral to see a physical therapist?
In most cases, you don't. Thanks to direct access laws, you can seek physical therapy directly. In New York State, experienced licensed physical therapists (like our team at Evolve) can evaluate and treat you for up to 10 visits or 30 days without a referral. This allows you to save both time and money by getting help sooner.
If your condition requires extended care or is outside our scope of practice, we will guide you to the right medical professional. Your safety and recovery always come first.
How long does a typical physical therapy plan last?
The length of a treatment plan varies for each person. Most adult plans last between four to 12 weeks, with one to three sessions per week. Each session is about an hour to an hour and a half, including hands-on therapy, guided exercises, and education.
The duration depends on several factors:
- The severity of your condition
- Your adherence to your home exercise program
- Your personal goals
- Your body's individual response to treatment
We'll provide a clear timeline during your first visit and adjust it as you progress.
Is physical therapy supposed to be painful?
A common concern is whether therapy will be painful. Our primary goal is to reduce your pain, not add to it. It's important to distinguish between different types of discomfort.
- Therapeutic discomfort is the mild soreness or muscle fatigue you feel as your body heals and strengthens. This is a normal and positive sign of progress.
- Harmful pain is sharp, shooting, or increasing pain. You should tell your therapist immediately if you feel this, as we never want to aggravate your condition.
Communication with your therapist is key. We need to know how you're feeling so we can modify your treatment to keep you comfortable while still making progress. We use various pain-relieving techniques to minimize discomfort and ensure your therapy is a positive experience.
Conclusion
Your journey to better health can start now. As we've explored, physical therapy for adults offers a proven path to pain relief without medications, improved mobility and balance, and the prevention of future injuries.
Physical therapy is proactive. Instead of just managing symptoms, we help you build a stronger, more resilient body. This approach helps you maintain your independence, stay active in the hobbies you love, and feel confident in your body's ability to support you.
At Evolve Physical Therapy + Sports Rehabilitation, we believe in hands-on, individualized treatment that addresses the root cause of your concerns. Our holistic approach ensures we're treating you as a whole person, utilizing specialized programs and manual therapy techniques to provide the personalized care you deserve.
Long-term wellness starts with a single step. You don't have to accept pain or limited mobility as a normal part of life. With the right support, you can regain control over your physical health and enjoy a more active, fulfilling life.
Ready to start your recovery journey? We're here to help you every step of the way.
Take control of your health and book a physical therapy consultation today.
Unlocking Shoulder Mobility Through Scapular Movement
Why Your Shoulder Blade is the Key to Pain-Free Movement

How much of shoulder mobility is due to scapular movement is a critical question for anyone with shoulder pain. The answer is significant:
The scapula (shoulder blade) contributes approximately 60 degrees out of 180 degrees of total arm elevation—that's one-third of your shoulder's mobility.
- Total shoulder elevation: 180 degrees
- Glenohumeral joint (ball-and-socket): 120 degrees (67%)
- Scapulothoracic joint (shoulder blade): 60 degrees (33%)
- Movement ratio: 2:1 (glenohumeral to scapular movement)
Your shoulder is a complex system where the scapula acts as a moving platform for your arm. When this coordination breaks down, pain and stiffness follow. Research shows that scapular dyskinesis (altered shoulder blade movement) occurs in 68-100% of people with shoulder injuries. If you have shoulder problems, your scapula is likely involved.
I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy. With nearly two decades of experience, I've helped thousands of patients restore proper function by focusing on scapular movement, open uping pain-free mobility they thought was gone forever.
The Scapulohumeral Rhythm: A Coordinated Dance for Shoulder Movement
The relationship between your shoulder blade and arm bone is like a coordinated dance, crucial for understanding how much of shoulder mobility is due to scapular movement.
This partnership is the scapulohumeral rhythm. Your humerus (arm bone) and scapula (shoulder blade) move together in a precise 2:1 ratio. For every 3 degrees your arm lifts, 2 degrees come from your ball-and-socket (glenohumeral) joint, and 1 degree comes from your shoulder blade gliding across your ribcage. This allows for a full 150-180 degrees of motion.
Behind the scenes, your rotator cuff muscles work to keep your arm bone centered in the socket, preventing pinched tissues and pain.
The Three Phases of Arm Elevation
Lifting your arm occurs in three distinct phases:
The Setting Phase (0-30 degrees) is the warm-up. Your shoulder blade moves very little as the ball-and-socket joint initiates the movement.
The Mid-Range (30-90 degrees) is where the 2:1 rhythm is most prominent. Your shoulder blade rotates upward and tilts back, creating space for the arm to move freely and avoid pinching.
The Final Phase (90-180 degrees) is the finale. The shoulder blade's rotation becomes more significant, and your collarbone (via the acromioclavicular joint) contributes to achieve full overhead motion.
Why This Rhythm is Crucial for Shoulder Health
This coordinated rhythm is essential for a healthy, pain-free shoulder. It:
- Maintains stability: Proper scapular movement creates a stable platform for the arm bone in its socket.
- Prevents impingement syndrome: As your arm lifts, the scapula moves to increase the space between the arm bone and the acromion (a part of the shoulder blade), preventing painful pinching of rotator cuff tendons.
- Optimizes muscle function: It positions the deltoid and rotator cuff muscles to work at their ideal length and angle for maximum efficiency.
- Protects the rotator cuff: When the rhythm is correct, the rotator cuff isn't overworked, reducing the risk of fatigue, pain, and injury.
How Much of Shoulder Mobility is Due to Scapular Movement? The Numbers Explained
When patients ask me how much of shoulder mobility is due to scapular movement, the research-backed answer is clear.
Your shoulder blade contributes approximately one-third of your total arm elevation—about 60 degrees out of 180. This contribution is crucial for pain-free movement.
Let's break down the 180 degrees of motion you need for everyday activities:
The glenohumeral joint—your main ball-and-socket joint—provides 120 degrees of elevation.
The scapulothoracic joint contributes the remaining 60 degrees through upward rotation. Without those 60 degrees, your arm would get stuck at about 120 degrees, making it impossible to reach a high shelf or comb your hair.
This one-third contribution represents what we call dynamic stability. Your shoulder blade actively repositions your arm socket, creating a stable platform for your humerus to move freely.
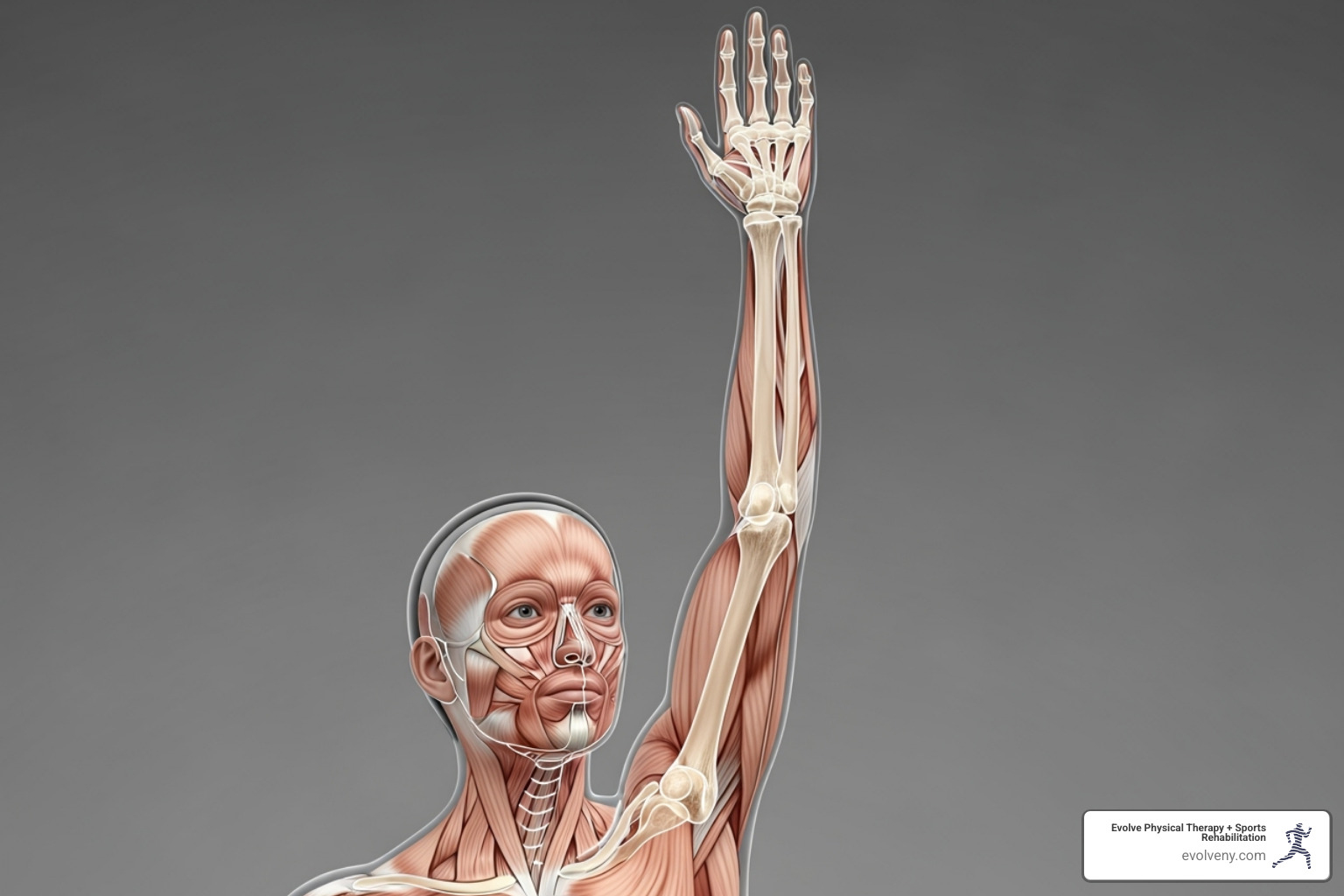
The Critical Role of Scapular Upward Rotation
As your arm rises, the scapula rotates upward, clearing the acromion (the bony roof over your shoulder). This movement increases the subacromial space, preventing your rotator cuff tendons from getting pinched between bones—a common and painful condition we see in our Brooklyn clinics.
When your scapula moves correctly, it's also maintaining rotator cuff effectiveness. These muscles work best when positioned properly, and your shoulder blade's movement keeps them in their optimal zone. The research backs this up: a scientific review of scapular dyskinesis shows that altered shoulder blade movement is present in the vast majority of shoulder injuries.
How much of shoulder mobility is due to scapular movement in different planes?
While that 2:1 ratio holds true generally, your scapula's contribution varies slightly depending on how you move your arm.
- Frontal plane abduction—lifting your arm straight out to the side—shows the classic 2:1 ratio most consistently.
- Sagittal plane flexion involves lifting your arm forward. Your scapula still upwardly rotates and tilts backward.
- Scapular plane movement, or "scaption," happens about 30 degrees forward from pure side-lifting. Many consider this the most natural way your shoulder moves, and the scapula's contribution remains essential.
Research shows variable ratios depending on the movement. That's why at our Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin locations, we assess shoulders during dynamic, functional movement patterns, not just static positions. This variability highlights that your shoulder is a complex system where the scapula always plays a starring role.
When the Rhythm is Off: Understanding Scapular Dyskinesis
Picture this: you're trying to reach for something on a high shelf, and suddenly your shoulder feels like it's grinding, catching, or just plain stuck. What you're experiencing might be scapular dyskinesis - a fancy term for when your shoulder blade has forgotten how to dance properly with your arm.
When we talk about how much of shoulder mobility is due to scapular movement, we're really highlighting how critical that coordinated rhythm is. When it breaks down, the effects ripple through your entire shoulder system like a domino effect.
Scapular dyskinesis is essentially any noticeable disruption in how your shoulder blade moves or sits on your ribcage. Think of it as your shoulder blade going rogue - instead of gliding smoothly and rotating upward as your arm lifts, it might stick out like a wing, barely move at all, or move in all the wrong directions.
The consequences can be frustrating and painful. Shoulder impingement becomes almost inevitable when your scapula can't create that crucial space for your arm to move freely. Your rotator cuff muscles end up working overtime, trying to compensate for the poor positioning, which often leads to strain or even tears.
You might also experience glenohumeral instability, where your arm bone doesn't sit properly in its socket because the scapula isn't providing a stable platform. It's like trying to shoot a basketball while standing on a wobbly stool - everything becomes harder and less reliable.

Common Causes of Impaired Scapular Movement
So what makes a perfectly good shoulder blade go off track? In my years of practice, I've seen some patterns emerge time and again.
Muscle imbalances are the biggest culprit by far. Your serratus anterior - that "boxer's muscle" that hugs your ribs and keeps your shoulder blade flat against your back - often becomes weak from poor posture or lack of use. When it's not doing its job, your shoulder blade can stick out like a wing, especially when you try to push or reach forward.
Meanwhile, your upper trapezius (the muscle that runs from your neck to your shoulder) often becomes overactive, trying to help with every shoulder movement. It's like having an overeager teammate who tries to do everyone else's job - well-intentioned but ultimately counterproductive.
The pectoralis minor, a small but mighty muscle in your chest, frequently becomes tight from hunching over computers or phones. When it's tight, it pulls your shoulder blade forward and down, setting up a poor starting position for any arm movement.
Poor posture is another major player, especially in our screen-dominated world. That forward head, rounded shoulder position doesn't just look tired - it actually changes how your shoulder blade sits and moves. Your thoracic spine (upper back) gets stiff and rounded, creating a bumpy, restricted surface for your shoulder blade to glide on.
Sometimes the cause is more specific: clavicle fractures, AC joint injuries, or even nerve damage can directly disrupt the delicate coordination your shoulder blade needs to function properly.
What happens when the scapula's contribution to shoulder mobility is impaired?
When your shoulder blade can't contribute its vital one-third of shoulder mobility, the whole system suffers. You'll likely notice reduced range of motion first - that frustrating feeling when your arm just won't go where you want it to go, often getting stuck around 120 degrees instead of reaching the full 180.
Many of my patients describe a painful arc of motion - certain parts of lifting their arm hurt more than others. This usually happens when tissues get pinched because the scapula isn't creating enough space.
Decreased strength follows naturally because your muscles can't work efficiently when the bones they're attached to aren't positioned properly. It's like trying to use a wrench when the bolt is at the wrong angle - you just can't get good leverage.
Perhaps most concerning is the increased risk of injury that comes with compensatory movement patterns. When your shoulder blade isn't doing its job, other structures have to work harder, making rotator cuff tears, labral injuries, and even frozen shoulder more likely.
Some patients develop what we call "SICK" Scapula Syndrome - an acronym that describes Scapular malposition, Inferior medial border prominence (the bottom inside edge sticking out), Coracoid pain and malposition, and dysKinesis of scapular movement. It sounds dramatic, but it perfectly captures how one problem can cascade into multiple issues.
The good news? Once we understand what's gone wrong, we can usually get that rhythm back on track. That's where proper assessment and targeted treatment come in - but more on that in the next section.
Restoring the Rhythm: How Physical Therapy Can Help
Here's the encouraging news: most cases of scapular dyskinesis respond beautifully to physical therapy. Think of it like learning to dance again - your shoulder just needs the right teacher and some practice to get back in rhythm.
At Evolve Physical Therapy + Sports Rehabilitation, we take a hands-on approach to getting your shoulder blade moving properly again. Our experienced physical therapists serve Brooklyn communities including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, and we know exactly what it takes to restore that crucial scapular contribution to your shoulder mobility.
Professional assessment is where everything begins. We don't just peek at your shoulder and call it a day. Instead, we examine your entire upper body like detectives solving a movement mystery. This comprehensive evaluation helps us understand not just what's wrong, but why it went wrong in the first place.
Visual observation reveals so much about how your scapula behaves. We'll watch closely as you move your arm through different motions, looking for telltale signs like winging, excessive shrugging, or that awkward "hitching" movement that signals something's not quite right.
Clinical tests give us the specific information we need to create your treatment plan. The Scapular Assistance Test (SAT) is particularly revealing - we manually guide your scapula into better position as you lift your arm. If your pain decreases or your range improves with our help, it confirms your scapula needs some coaching to move correctly on its own.
The Scapular Retraction Test (SRT) works similarly. We stabilize your shoulder blade while you perform movements, and if this makes you stronger or more comfortable, it tells us your periscapular muscles need attention.

This thorough evaluation allows us to pinpoint exactly why how much of shoulder mobility is due to scapular movement has become compromised in your case. You can find more info about our shoulder rehabilitation services to learn how we can help restore your shoulder function.
Physical Therapy Goals for Scapular Dyskinesis
Our mission is simple: get your scapula dancing in perfect rhythm with your arm again. This means restoring pain-free, full shoulder function through a targeted approach that addresses your specific needs.
Strengthening stabilizers forms the foundation of most treatment plans. The serratus anterior often needs the most attention - this "boxer's muscle" is crucial for preventing winging and promoting proper upward rotation. We use exercises like wall slides, push-up plus movements, and serratus punches to wake this muscle up. Sometimes we even use special biofeedback equipment to help you feel exactly how to activate it correctly.
Lower trapezius activation is equally important. This muscle helps your scapula rotate upward and stay stable during arm movements. Prone "Y" raises and specific rowing variations become your new best friends. We focus on teaching these muscles to work in real-world patterns, not just isolated gym exercises.
Stretching tight muscles addresses the other side of the equation. Your pectoralis minor often becomes tight from poor posture, pulling your scapula forward and down like an anchor. Targeted stretching releases this tension, allowing your shoulder blade to move freely again.
Upper trapezius and levator scapulae stretches help reduce that compensatory shrugging pattern many people develop. When these muscles relax, your scapula can focus on its proper job instead of being hijacked by overactive helpers.
Improving thoracic mobility creates a better foundation for scapular movement. If your upper back is stiff, your scapula can't glide smoothly across your ribcage. We use hands-on techniques and specific exercises to restore that essential thoracic extension and rotation.
Neuromuscular re-education might sound fancy, but it's really about retraining your brain and muscles to work as a team again. We teach you to consciously control your scapula through slow, controlled movements. You'll learn to feel the difference between good and poor movement patterns.
This process often starts with simple awareness - learning to pull your shoulder blades back and down into a healthy resting position. We then progress to more complex, automatic movements that carry over into your daily activities.
Our individualized approach at Evolve Physical Therapy + Sports Rehabilitation means your treatment plan is designed specifically for you. We don't just fix the immediate problem - we establish a maintenance program to prevent future issues, especially important if you're active or have demanding physical activities. Whether you're dealing with everyday shoulder stiffness or athletic performance issues, we're here to help you open up your shoulder's full potential.
Frequently Asked Questions about Scapular Movement
After treating thousands of patients with shoulder issues at Evolve Physical Therapy, I've noticed the same questions come up again and again. Let me address the most common concerns about how much of shoulder mobility is due to scapular movement and what it means for your shoulder health.
What is the 2:1 scapulohumeral rhythm?
Think of the 2:1 scapulohumeral rhythm as your shoulder's secret handshake - a perfectly coordinated movement pattern that happens every time you lift your arm. Here's how it works: for every 3 degrees your arm rises, 2 degrees come from your glenohumeral joint (that ball-and-socket joint) and 1 degree comes from your scapula gliding across your ribcage.
This might sound like technical jargon, but it's actually quite beautiful when you think about it. Your body has developed this intricate dance to ensure smooth, pain-free overhead motion. The rhythm optimizes how your muscles work together and prevents that painful pinching sensation (impingement) that many people experience when reaching overhead.
When this rhythm is working properly, you don't even think about it - your arm just flows upward effortlessly. But when it's disrupted, every overhead reach becomes a reminder that something isn't right.
Can I fix scapular winging on my own?
I understand the appeal of trying to fix things yourself - we live in a DIY world, after all. While improving your posture and doing some general strengthening exercises might help a little, scapular winging usually stems from complex muscle imbalances or even nerve issues that aren't easily addressed with generic exercises.
Here's the thing: what looks like a simple "muscle weakness" problem could actually be caused by nerve damage, specific muscle inhibition, or compensation patterns that have developed over months or years. Simple home exercises might not target the root cause, and worse, they could reinforce the wrong movement patterns.
A professional evaluation by a physical therapist is crucial to identify exactly what's causing your scapular winging. Is it a weak serratus anterior muscle? Nerve involvement? An underlying joint restriction? Each cause requires a different approach. We need to create a safe, effective, and targeted exercise program based on your specific situation.
Trying to "fix" it on your own without a proper diagnosis is a bit like trying to repair a car engine when you're not sure if the problem is the spark plugs, the fuel pump, or something else entirely. You might get lucky, but you're more likely to create new problems or waste precious time.
How does my posture affect my shoulder mobility?
Your posture is like the foundation of a house - if it's off, everything built on top of it will have problems. A slouched, forward-head posture creates a cascade of issues that directly impacts how much of shoulder mobility is due to scapular movement.
When you slouch, your thoracic spine rounds into that familiar "hunched" position, and your shoulder blades tilt forward and downward. This isn't just an aesthetic issue - it fundamentally changes how your shoulder works. The altered resting position reduces the subacromial space (that crucial area where your rotator cuff tendons need to glide freely) and completely changes the starting point for your shoulder's normal movement pattern.
Think of it this way: if your scapula starts in the wrong position, it can't perform its proper upward rotation and backward tilt when you lift your arm. This limitation significantly restricts your overhead reach and forces your shoulder muscles to work much harder and less efficiently.
Poor posture essentially sets your shoulder up for failure before you even start moving. It's like trying to throw a ball while standing on uneven ground - you might be able to do it, but it won't be smooth, powerful, or sustainable. The good news? Posture is something we can definitely work on together, and the improvements in shoulder function can be dramatic once we restore that solid foundation.
Conclusion
Your shoulder blade plays a starring role in every reach, lift, and throw you make. How much of shoulder mobility is due to scapular movement? As we've explored together, it's a crucial one-third of your total arm elevation - those vital 60 degrees that make the difference between getting stuck at shoulder height and reaching freely overhead.
Think of your scapula as the unsung hero of shoulder movement. While your ball-and-socket joint gets most of the credit for big movements, your shoulder blade is working behind the scenes as a moving platform, constantly adjusting its position to keep everything running smoothly. When this coordinated dance breaks down, even simple tasks like putting dishes away or throwing a ball become painful reminders that something isn't right.
The beauty of understanding scapular movement is that knowledge leads to solutions. Most scapular problems aren't permanent fixtures - they're puzzles waiting to be solved. Whether you're dealing with that telltale shoulder blade winging, struggling with overhead reach, or experiencing that frustrating shoulder pain that just won't quit, there's hope.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen countless patients refind pain-free shoulder movement by addressing their scapular rhythm. Our hands-on approach goes beyond just treating symptoms - we look at the whole picture, from your posture at your desk to the way you sleep at night. We understand that your shoulder doesn't exist in isolation; it's part of a beautiful, complex system that deserves comprehensive care.
Your journey back to healthy shoulders starts with understanding, and now you have that foundation. The next step is getting the personalized assessment and treatment your unique situation deserves. Our experienced team across Brooklyn - whether you're in Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin - is ready to help you open up your shoulder's full potential.
Don't let shoulder pain write the story of your daily life. Get a professional assessment for your shoulder pain and let us help you refind what pain-free movement feels like. Your shoulders - and your quality of life - are worth the investment.
How to Sit Pretty—The Best Posture for Desk Work
Why Perfect Desk Posture Is Your Secret Weapon Against Pain

Best posture for desk work is your first line of defense against the pain that plagues modern workers. With many spending over half their workday seated, the health stakes are high. A 2020 survey found 41% of remote workers reported new lower back pain. Prolonged sitting also increases the risk of diabetes and cardiovascular disease.
The best posture for desk work includes:
- Feet flat on the floor with knees at 90 degrees
- Back against chair with lumbar support
- Monitor at eye level, arm's length away
- Elbows at 90 degrees with relaxed shoulders
- Wrists straight while typing
The good news? Proper posture can boost energy, improve focus, and prevent the damaging "cashew" posture. I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy in Brooklyn. With nearly two decades of experience, I've seen how mastering desk posture transforms my patients' quality of life.
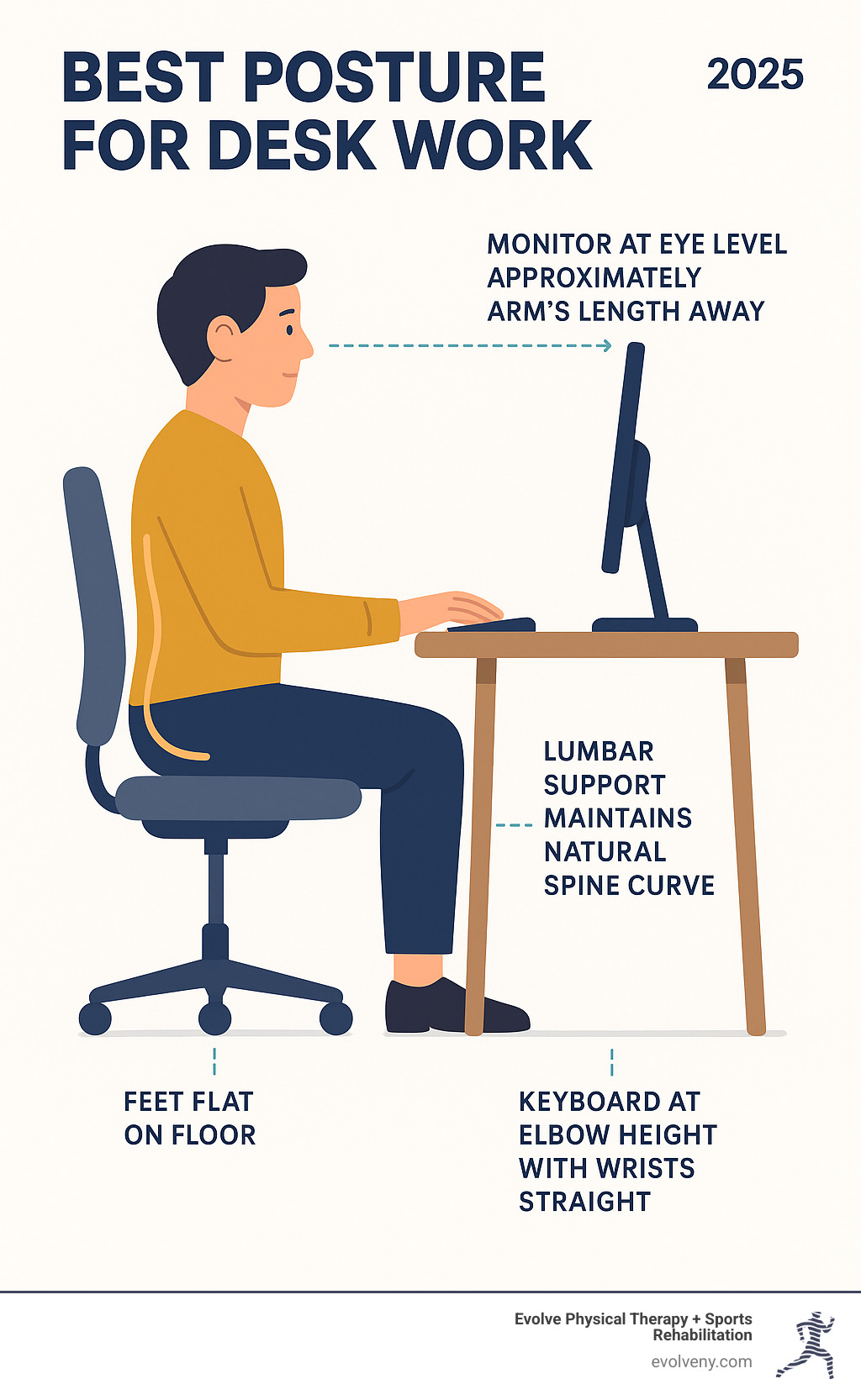
Why Your Desk Posture Matters: The Risks and Rewards
The phrase "sitting is the new smoking" might sound dramatic, but our bodies were designed for movement, not to be folded into a chair for 8+ hours. Ignoring the best posture for desk work has serious consequences beyond end-of-day stiffness, including an increased risk of diabetes, cardiovascular disease, and chronic pain. At Evolve Physical Therapy, we see the aftermath daily: weak glutes, tight hip flexors, and aching backs. These problems are largely preventable.
For a deeper dive into the health risks, check out the risks of prolonged sitting. And if you're curious about common postural mistakes, our article on bad office posture covers the most frequent culprits we see.
The Hidden Dangers of Slouching
Slouching creates the "cashew posture"—your spine curves, your head juts forward, and your shoulders round inward. This seemingly comfortable slump has a high cost:
- Spinal Stress: Your spinal discs compress unevenly, which can lead to conditions like kyphosis (a hunched back) and herniated discs.
- Neck and Shoulder Pain: A forward head position adds significant strain to your cervical spine, leading to "tech neck," headaches, and shoulder tension.
- Back Pain: The natural S-curve of your spine flattens, forcing lower back muscles to overwork, causing chronic aches.
- Wrist and Hand Issues: Awkward wrist angles while typing can lead to pain and carpal tunnel syndrome.
- Poor Circulation & Digestion: Crossing your legs or slouching can reduce blood flow and compress abdominal organs, leading to fatigue and digestive issues.
The Benefits of Sitting Up Straight
Mastering the best posture for desk work offers immediate and long-term rewards. When your body is properly aligned, you'll experience:
- Reduced pain and discomfort
- Increased energy and focus
- Better breathing and oxygen flow
- Improved mood and confidence
- Protection for your long-term spinal health
Good posture isn't just about looking professional—it's about feeling great, thinking clearly, and setting yourself up for long-term health. For more insights, check out our article on perfect posture.
The Ultimate Ergonomic Workstation Setup
Ergonomics is the science of designing your workspace to fit you, preventing your body from adapting to an uncomfortable setup. A proper ergonomic environment supports 'neutral body positioning,' where your body maintains its natural alignment without strain. This is the key to mastering the best posture for desk work.
For comprehensive guidance, the Mayo Clinic's ergonomics guide offers excellent advice. For home setups, see our article on Home Office Ergonomics.

Achieving 'Neutral Body Positioning'
Neutral positioning means aligning your joints so your muscles aren't fighting gravity. Your spine should maintain its natural S-curve—not be poker-straight. The foundation is your pelvis; sit with your weight centered on your "sitz bones" (the pointy bones in your buttocks) to maintain your lower back's natural curve. From there, let your shoulders relax down, keep your head balanced over your shoulders, and bend your elbows comfortably near your sides. Even in a good position, your body needs to move. OSHA's guide emphasizes this balance between alignment and regular movement.
Choosing and Adjusting Your Office Chair
Your chair should be your biggest supporter. Look for these key adjustments:
- Height: Adjust so your feet are flat on the floor, with knees level with or slightly below your hips.
- Lumbar Support: Position the support to fit the natural curve of your lower back. A rolled-up towel is a great substitute.
- Armrests: Set them so your shoulders are relaxed and your forearms are parallel to the floor.
- Seat Depth: Ensure a 2-3 finger gap between the front of the seat and the back of your knees.
- Recline: A slight recline of 90-110 degrees can reduce spinal pressure.
For more details, see our guide on Correct Computer Posture.
Positioning Your Monitor, Keyboard, and Mouse
Your tech setup is critical for preventing "tech neck" and wrist strain.
- Monitor: Place the top of the screen at or slightly below eye level, about an arm's length away. Center it directly in front of you.
- Keyboard: Position it to allow for relaxed shoulders and straight wrists. Consider a negative tilt (angling it away from you) for a more natural wrist position.
- Mouse: Keep it close to the keyboard at the same height.
- Laptop Users: To avoid hunching, use a laptop stand to raise the screen to eye level and use an external keyboard and mouse.
The Best Posture for Desk Work: Feet and Legs
Your lower body is your foundation.
- Feet: Keep them flat on the floor. Use a footrest if they don't reach.
- Knees: Bend them at approximately 90 degrees.
- Legs: Avoid crossing them to maintain good circulation and hip alignment.
- Legroom: Ensure you have enough space under your desk to move freely.
How to Maintain the Best Posture for Desk Work All Day Long
An ergonomic chair won't help if you're still slouching. The best posture for desk work is a daily practice, not a one-time setup. Your muscles have memory from years of hunching, and breaking those patterns requires consistent effort and movement. Your body wasn't designed to stay frozen in any position, even a perfect one.
For more insights on maintaining proper alignment, check out our article on Ideal Computer Posture.
The Power of Movement: Breaks and Stretches
Static posture, even good posture, creates stiffness and slows circulation. Movement is the antidote.

- Take Breaks: Move every 30-60 minutes. Set a timer.
- Use the 20-20-20 Rule: Every 20 minutes, look at something 20 feet away for 20 seconds to rest your eyes and reset your posture.
- Stand and Walk: Take calls while standing or walk to a colleague's desk.
- Stretch at Your Desk:
- Chin Tucks: Gently pull your chin back to stretch the back of your neck.
- Shoulder Blade Squeezes: Squeeze your shoulder blades together to open your chest.
- Chest Stretch: Use a doorway to lean forward and stretch your chest muscles.
- Hip Flexor Stretch: Stand and step into a gentle lunge to stretch the front of your hip.
Common Posture Mistakes and How to Fix Them
Watch out for these common posture saboteurs:
- Hunching Forward: Raise your monitor to eye level and sit back in your chair.
- 'Tech Neck': Bring your phone/screen up to your eyes, not your eyes down to the screen.
- Cradling the Phone: Use a headset or speakerphone.
- Reaching for Items: Keep frequently used items within easy arm's reach.
- Dangling Feet: Use a footrest if your feet don't touch the floor.
- Not Using Back Support: Scoot your chair in and let the backrest support your spine.
Building Habits for Lasting Posture Improvement
Turn good posture into an automatic habit.
- Do Regular Posture Checks: Set a timer to do a quick body scan every hour.
- Strengthen Your Core: A strong core supports your spine effortlessly. Simple exercises like planks and glute bridges are highly effective.
- Listen to Your Body: Pain is a signal to change something. Don't ignore it.
- Get Professional Help: If pain persists despite your best efforts, it's time to see a professional. Underlying issues may need to be addressed.
At Evolve Physical Therapy, we help people build these habits and address the root causes of postural problems. Learn more about Physical Therapy for Posture Training.
Frequently Asked Questions about Desk Posture
Here are answers to the most common questions I hear at Evolve Physical Therapy about achieving the best posture for desk work.
How can I tell if my chair is at the right height?
Your chair height is the foundation of your posture. Use this quick checklist:
- Your feet should be flat on the floor (use a footrest if needed).
- Your knees should be level with or slightly below your hips.
- Your thighs should be parallel to the floor.
- There should be a 2-3 finger gap between the seat edge and the back of your knees to ensure good circulation.
Is a standing desk better than sitting?
Neither sitting nor standing all day is ideal. The real benefit comes from alternating between sitting and standing. This variety engages different muscles, improves blood flow, and boosts energy. When you stand, maintain good posture (eye-level monitor, relaxed shoulders) and consider an anti-fatigue mat. Movement trumps any single static position.
What if I still have pain after improving my posture?
If you've improved your ergonomics but still have persistent pain, your body is signaling a deeper issue. Muscle imbalances, joint restrictions, or nerve compression may have developed over time and won't be fixed by a better chair alone. Don't try to tough it out.
Persistent pain, stiffness, or tingling is your cue to seek professional help. At Evolve Physical Therapy, serving Brooklyn communities from Marine Park to Park Slope, we can identify the root cause of your discomfort. A physical therapy evaluation provides targeted exercises and hands-on treatment that go beyond ergonomics. Learn more about how we combine Ergonomics and Physical Therapy.
Conclusion: Your Path to a Pain-Free Workday
You now have the knowledge to trade desk-related aches for a pain-free workday. The key takeaway is that discomfort is not inevitable. By creating an ergonomic workspace and practicing good posture, you can reduce pain, increase energy, and improve focus.
Your ergonomic setup—a properly adjusted chair, an eye-level monitor, and supported feet—is your foundation. But the real change comes from building mindful habits. Regular movement is the most critical piece of the puzzle. Getting up frequently to stretch and walk is like hitting a reset button for your body.
Posture is an ongoing practice, not a one-time fix. Some days will be better than others; what matters is your commitment to getting back on track.
At Evolve Physical Therapy, we see the incredible changes that happen when people in Brooklyn, from Marine Park to Park Slope, commit to better posture. If you've tried these strategies but still face persistent pain, don't ignore it. Underlying issues often need professional attention. Our hands-on approach can identify the root cause and give you the tools to finally break free from chronic discomfort.
Your workday doesn't have to be a battle against pain. Take the next step. Get a professional ergonomic assessment with physical therapy in Brooklyn and start your journey to truly pain-free days.
Steady Steps Ahead – Physical Therapy for Parkinson's Disease
Why Physical Therapy is Essential for Parkinson's Management

Physical therapy for Parkinson's is a cornerstone treatment that helps manage symptoms, improve mobility, and improve the quality of life for the over 1 million Americans living with this progressive neurological condition.
Key Benefits of Physical Therapy for Parkinson's:
- Improved Balance & Gait - Reduces fall risk and improves walking confidence
- Increased Strength & Flexibility - Combats muscle rigidity and weakness
- Better Daily Function - Helps maintain independence in everyday activities
- Symptom Management - Addresses tremor, stiffness, and movement difficulties
- Disease Progression - Slowing decline when exercising 2.5+ hours per week
Physical therapy isn't just for managing symptoms after they worsen—it's about taking control from the moment of diagnosis. Research shows that regular physical activity leads to a slower decline in quality of life and better long-term outcomes for people with Parkinson's.
The science is clear: exercise acts as medicine for the Parkinson's brain. It improves the release of brain-derived neurotrophic factors (BDNF), increases neuroplasticity, and helps the body use dopamine more efficiently, providing neuroprotective benefits that medication alone cannot.
As Lou Ezrick, founder of Evolve Physical Therapy, I've seen how specialized physical therapy for Parkinson's transforms lives by helping patients maintain their independence and mobility. My experience with complex neurological conditions confirms that early, consistent, hands-on care is crucial for managing this progressive disorder.
Understanding Parkinson's and How Movement is Affected
Receiving a Parkinson's diagnosis can be overwhelming. Understanding how the disease affects movement is the first step toward taking control.
Parkinson's disease is a progressive neurodegenerative disorder targeting the substantia nigra, a brain area that produces dopamine. Dopamine is a chemical messenger essential for coordinating movement. As these dopamine-producing neurons deteriorate, movement becomes less smooth and coordinated.
Over 1 million Americans live with Parkinson's, a number expected to reach 1.64 million within 20 years. Globally, it's the fastest-growing neurological disorder, affecting 6.1 million people—a figure projected to double by 2050.
Parkinson's is characterized by its four cardinal motor symptoms that emerge as dopamine levels decline. Bradykinesia (slowness of movement) makes simple tasks difficult. Rigidity causes muscle stiffness. Tremor involves involuntary shaking, often at rest. Most concerning is postural instability, which impairs balance and coordination, increasing fall risk.
Parkinson's also involves non-motor symptoms like deep fatigue, sleep problems, depression, anxiety, cognitive changes, and loss of smell. These invisible symptoms can be as impactful as the movement challenges.

The Brain-Body Connection: How Exercise Helps
Here's where the story gets hopeful. While it seems counterintuitive, the science behind using movement to help a movement disorder is one of medicine's most encouraging findings.
Your brain has an incredible ability called neuroplasticity—it can rewire itself and form new neural pathways. When Parkinson's damages dopamine pathways, targeted exercise helps your brain build detours around the damaged areas.
Exercise doesn't create more dopamine, but it helps your body use it more efficiently. This occurs through neuroprotection, where physical activity shields healthy neurons from further damage.
One exciting finding involves Brain-Derived Neurotrophic Factor (BDNF), or "fertilizer for the brain." Regular exercise boosts BDNF, promoting neuron growth and survival. Scientific research on exercise and dopamine release continues to show how physical activity optimizes the brain's neurochemical resources.
Exercise also improves corticomotor excitability, making the brain's motor cortex more responsive when sending movement signals. This improves brain-body communication.
Every intentional movement helps your brain adapt, protect itself, and optimize its resources. That's why physical therapy for Parkinson's isn't just treatment; it's hope in action.
The Transformative Role of Physical Therapy for Parkinson's
Receiving a Parkinson's diagnosis is overwhelming, but physical therapy for Parkinson's offers a way to take control. It's not just for managing symptoms as they appear; it's about building a strong foundation for the future, starting from day one.
Think of a physical therapist as your personal movement coach. We teach your brain new ways to move, help you stay independent, and provide tools for daily confidence. This proactive approach means starting therapy at diagnosis, not waiting for symptoms to worsen.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen how the right therapy program can transform someone's relationship with their diagnosis. Our hands-on approach, including specialized programs like Rock Steady Boxing for Parkinson's patients (which was even featured on NBC News), focuses on what you can do rather than what the disease might take away.

Key Benefits for Mobility and Quality of Life
Physical therapy for Parkinson's touches every aspect of daily life. Improving your gait and walking speed makes a trip to the grocery store feel less like a marathon. We work on lengthening your stride and reducing shuffling to help you walk with renewed confidence.
Better balance reduces the constant worry of falling. Targeted exercises retrain the systems that keep you steady, helping you feel more secure at home and in the community.
The reduced fall risk from improved balance and strength provides peace of mind for you and your family. We focus on improving reaction time and teaching you how to recover from a stumble.
Increased strength and flexibility combat the frustrating rigidity of Parkinson's. Stronger, more flexible muscles make everyday movements easier and less painful, so tasks like dressing or reaching for items become manageable again.
Most importantly, as your ability for daily tasks improves, so does your independence. We help you maintain the activities that matter most, from getting out of a chair to playing with grandchildren.
The improved mood and confidence from better movement is significant. Feeling more in control of your body can decrease anxiety and increase hope, leading to renewed optimism. More info about Parkinson's physical therapy benefits.
Long-Term Impact on Disease Progression
The long-term impact of physical therapy for Parkinson's is truly powerful. Research shows that committing to at least 2.5 hours of exercise per week leads to a slower decline in quality of life compared to being sedentary.
Exercise is a long-term investment in yourself. While Parkinson's is progressive, consistent physical activity can significantly slow symptom progression and help maintain function over time. This is backed by solid science.
This is a lifelong commitment to your well-being, but you're not alone. We guide you, adjust your program, and celebrate your victories. Evidence shows that staying active preserves your independence for years to come.
Research on long-term exercise benefits continues to show us just how powerful this approach can be. When you make physical therapy part of your Parkinson's management plan, you're not just treating symptoms - you're actively working to maintain the life you want to live.
What to Expect from a Parkinson's Physical Therapy Program
At Evolve Physical Therapy + Sports Rehabilitation, we start a partnership built around you. Every person with Parkinson's is unique, so we create individualized plans custom to your specific needs and goals, not a one-size-fits-all program.
We believe in collaborative goal setting. Your personal goals—whether it's playing with grandchildren, taking morning walks, or moving confidently at home—become the focus of our work together.
Your First Appointment and Evaluation
Your first visit is a comprehensive assessment where we get to know you. We'll cover your medical history, daily routines, and therapy goals. During the medical history review, we'll discuss your diagnosis, medications, and how Parkinson's affects your daily life, including your hobbies and important activities.
Next, we'll perform functional tests to assess your movement. The 6-Minute Walk Test measures endurance, while the Timed Up and Go test assesses balance and mobility. We also conduct strength and balance testing and a gait analysis to spot issues like shuffling, reduced arm swing, or freezing episodes.
This information helps us collaborate on setting realistic movement goals based on your daily life. We encourage you to prepare questions before your visit. More info on preparing for your first PT appointment.
Core Exercise Strategies in Physical Therapy for Parkinson's
Our physical therapy for Parkinson's programs use proven, targeted exercises that can be adapted as you get stronger.
- Aerobic exercise, like treadmill walking and cycling, is foundational for heart health and reducing Parkinson's symptoms.
- Resistance training with weights and resistance bands builds strength for daily activities and combats weakness.
- Balance training, sometimes incorporating Tai Chi or yoga, is essential for preventing falls and building confidence.
- Flexibility and stretching exercises address Parkinson's-related stiffness.
- Gait training with external cues, such as metronomes for rhythm or visual lines on the floor, helps overcome walking challenges.
- Task-specific training focuses on real-life activities like sit-to-stand transfers to build your skill and confidence.
Specialized Approaches in Parkinson's Physical Therapy
We also use specialized techniques like amplitude-based training. Our "Think BIG!" philosophy helps retrain your brain to counteract the smaller movements caused by Parkinson's, producing larger, more functional actions.
Task-specific movement practice and functional mobility training focus on the practical skills you need every day. We also offer adapted exercise classes and aquatic therapy to make exercise accessible and effective.
At Evolve Physical Therapy + Sports Rehabilitation, we're proud to offer specialized programs for Parkinson's including our Rock Steady Boxing program, which has been featured on NBC News for its effectiveness. All of these services are provided or coordinated through our Brooklyn locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, making expert care accessible right in your community.
Building Your Parkinson's Care Team
Managing Parkinson's disease isn't a solo journey. The most effective approach is a multidisciplinary team of healthcare professionals working together to address every aspect of your condition. Physical therapy for Parkinson's is a cornerstone of this team, working best when combined with other specialized services. This holistic care strategy ensures comprehensive symptom management and quality of life.
Finding the Right Physical Therapist
Finding the right physical therapist doesn't have to be overwhelming. The key is to start your search at the moment of diagnosis—don't wait for symptoms to worsen. Your neurologist is the best starting point for referrals to therapists specializing in movement disorders. Look for a Board-Certified Neurologic Clinical Specialist (NCS), which indicates advanced neurological training.
Ask direct questions about their Parkinson's experience, including the number of PD patients they treat and the specialized programs they offer. A good therapist will welcome these questions. The American Physical Therapy Association provides a helpful Directory to find a PT that can help you locate qualified professionals in your area.
At Evolve Physical Therapy + Sports Rehabilitation, our therapists have extensive experience with neurological conditions and offer specialized programs like Rock Steady Boxing, featured on NBC News for its effectiveness in helping people fight back against Parkinson's symptoms.
How Physical Therapy for Parkinson's Complements Other Treatments
Physical therapy for Parkinson's doesn't work in isolation; it supports your entire treatment plan. The best results come from coordinated communication among all your healthcare providers.
Your physical therapist will communicate with your neurologist to align therapy goals with your medication schedule and overall management strategy. This partnership is crucial, as timing therapy with medication can significantly impact progress.
While PT focuses on larger movements, Occupational Therapy (OT) addresses the finer details of daily living. An OT helps with hand coordination, fine motor skills, and home adaptations like special utensils or grab bars to make daily tasks safer and easier.
Speech-Language Pathology (SLP) addresses communication challenges, which affect up to 89% of people with Parkinson's. A speech therapist works on voice volume, clarity, and swallowing safety, which can greatly restore confidence.
In this team approach, everyone stays in touch. For example, your PT shares balance updates with your OT, who may then adjust home modification recommendations. This collaborative care means you're not just treating symptoms in isolation—you're addressing the whole person.
Frequently Asked Questions
Having worked with countless families navigating a Parkinson's diagnosis, I've learned that certain questions come up again and again. These are the conversations that help you make informed decisions about your care and feel more confident about the path ahead.
When is the best time to start physical therapy for Parkinson's?
My answer is always the same: start now. The perfect time to begin physical therapy for Parkinson's is right after your diagnosis. It may seem counterintuitive if your symptoms aren't severe, but that's precisely the point. Early intervention is key because it allows us to build on your current strength and capabilities.
This proactive vs. reactive care allows us to establish a baseline of your movement and strengths. This baseline is invaluable for tracking progress and adjusting your care over time. Building good habits early is powerful. Learning proper movement techniques from the start helps them become second nature, making it easier to maintain them long-term.
The research backs this up completely. People who engage in regular physical activity from the early stages experience a slower decline in both quality of life and motor function. Don't wait for a fall or significant worsening of symptoms to talk to your doctor about starting physical therapy.
Does Medicare cover physical therapy for Parkinson's?
Yes, Medicare Part B does cover physical therapy for Parkinson's when it is prescribed by your doctor and deemed medically necessary. This means if your physician determines PT will help treat your condition, improve function, or prevent decline, Medicare should provide coverage. You will need a doctor's referral, which most neurologists readily provide for their Parkinson's patients.
A significant recent change was the removal of strict therapy caps. Now, as long as your therapy remains medically necessary to maintain or improve your mobility, coverage can continue, which is crucial for chronic conditions like Parkinson's. I always recommend checking your specific plan to understand your co-pays, deductibles, and any particular requirements.
At Evolve Physical Therapy + Sports Rehabilitation, we work directly with Medicare and other insurance providers to help make sure you can access the care you need.
How often should I do my exercises?
For physical therapy for Parkinson's, consistency is crucial. It's better to make movement a regular part of your daily life than to do one long workout per week. Research recommends at least 2.5 hours of exercise per week. The key is that frequency matters most; moving for 20-30 minutes several times a week is more effective than one long, infrequent session.
Your program will combine guided PT sessions with a home exercise program. In our sessions, you'll learn and refine techniques, but your daily home program is where you'll build lasting habits. I also recommend periodic "tune-ups" every few months or once a year to reassess your progress, adjust your home program, and address any new challenges.
Research on exercise frequency consistently shows that people who maintain regular, frequent activity see the best long-term outcomes. The goal isn't perfection—it's sustained activity that fits into your life.
Conclusion
Your journey with Parkinson's doesn't have to be one of decline. As we've explored, physical therapy for Parkinson's is a powerful ally. The science is clear: targeted exercise actively rewires the brain, protects neurons, and helps you maintain the activities that matter most.
From the moment of diagnosis, physical therapy for Parkinson's offers tangible results. Consistent exercise can slow symptom progression, improve balance and walking confidence, and reduce fall risk, helping you stay engaged in life. These benefits extend to your mood, confidence, and sense of control.
The right care team, one that treats you as a whole person, makes all the difference. At Evolve Physical Therapy + Sports Rehabilitation, our hands-on approach ensures every session is customized to your specific needs and goals.
We're proud of our specialized programs like Rock Steady Boxing, featured on NBC News for its effectiveness. This program is more than just exercise; it's empowerment, giving you the tools to fight back against PD.
The best part? You don't have to travel far to access this level of specialized care. Our dedicated team is ready to support you right here in Brooklyn, with convenient locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin.
Taking the first step toward physical therapy for Parkinson's is about taking control of your future. Don't wait to start building the strength, balance, and neural pathways that will serve you for years to come.
Contact us to start your journey to better movement. The best time to begin is now, with a team that understands your journey.
Physical Therapy Unpacked: Movement and Mobility Explained
Why Movement and Mobility Matter More Than You Think

How does physical therapy deal with movement and mobility? By using a comprehensive approach that addresses pain, restores function, and prevents future injuries. Here's a quick overview:
- Assessment: Evaluating movement patterns, muscle strength, and joint function
- Manual Therapy: Using hands-on techniques to improve joint mobility and reduce muscle tension
- Therapeutic Exercise: Creating targeted strengthening and flexibility programs
- Balance Training: Prescribing exercises to improve stability and prevent falls
- Patient Education: Teaching proper body mechanics and home exercise programs
- Functional Training: Practicing activities that mirror real-life movements
Many people dismiss aches and pains as a normal part of aging, but impaired mobility affects millions worldwide, limiting their independence and quality of life. Physical therapy helps manage movement and reduce pain for various conditions, from neurological diseases to traumatic injuries.
As licensed movement experts, physical therapists evaluate and improve physical function. They improve a person's range of motion and quality of life while preventing further injury. Through targeted interventions, physical therapy can strengthen your muscles, bones, and joints, and support your cardiovascular and neurological systems.
I'm Lou Ezrick, founder of Evolve Physical Therapy. With nearly two decades of experience treating complex cases from terror attack victims in Tel Aviv to chronic pain patients in Brooklyn, I've learned that addressing the root cause of movement dysfunction leads to lasting results.
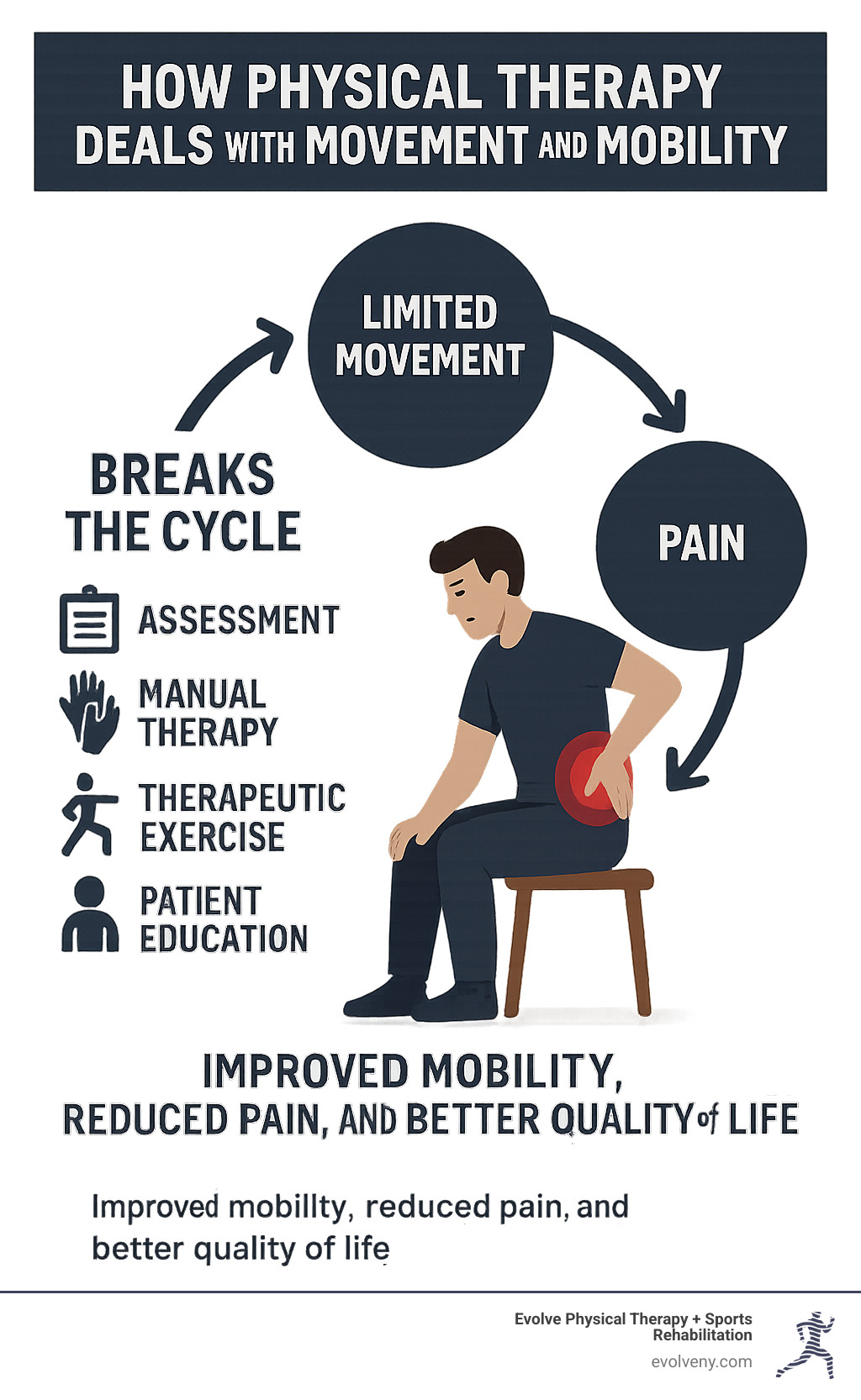
The Foundation: How Physical Therapists Assess Movement and Mobility
Your first physical therapy visit is like a detective investigation into your body's movement. At Evolve Physical Therapy, we don't just look at where it hurts; we uncover the full story of why you're struggling.

Our initial evaluation starts with your patient history, discussing your injury, lifestyle, work habits, and exercise routine. This context is crucial, as pain in one area can often stem from an issue elsewhere.
The physical examination involves analyzing your movement patterns as you walk, sit, and stand. For runners, a gait analysis can uncover subtle issues affecting performance. We use muscle strength testing to find weak links, check your joint range of motion for stiffness, and perform a posture analysis to see how your body compensates for dysfunction.
Finally, a balance assessment evaluates your stability, which is the foundation of safe movement for people of all ages. This gives us insight into how your nervous system controls your body.
What is Physical Therapy and How Does it Relate to Mobility?
What is Physical Therapy? It's a healthcare profession dedicated to restoring function and helping people move better. As licensed movement experts, we understand the body is an interconnected system.
How does physical therapy deal with movement and mobility? We work with your musculoskeletal, nervous, and cardiovascular systems to restore efficient, pain-free movement. Our approach covers everything from injury recovery to chronic condition management. The American Physical Therapy Association (APTA) definition highlights our role in diagnosing movement dysfunction and creating effective treatment plans.
What to Expect During Your First Appointment
Your first appointment begins with a conversation with your therapist. We'll focus on goal setting, whether you want to play with your grandkids or return to a sport. Your goals become our roadmap. A pain assessment helps us understand the specifics of your discomfort.
We then perform simple functional tests, like reaching or squatting, and use palpation (gentle touch) to feel muscles and joints. By the end of your visit, you'll have a personalized treatment plan and have all your questions answered. We believe that understanding your treatment makes you an active partner in your recovery.
The Core of Treatment: How Does Physical Therapy Deal with Movement and Mobility?
After your assessment, we begin treatment. How does physical therapy deal with movement and mobility? By using a comprehensive approach that targets the root causes of your problems, not just the symptoms.

Our primary goals are to reduce pain, restore function, prevent future injury, and improve your quality of life. Your treatment plan is personalized to your specific needs, lifestyle, and goals, because we know every patient is unique.
Strengthening Muscles and Joints for Better Support
Improving mobility requires building strength. We design therapeutic exercises that are carefully crafted to target your specific weaknesses. Resistance training builds muscle strength for better daily function, while strong core stability acts as a natural brace for your spine, reducing pain.
We also focus on joint protection by strengthening the muscles around them to act as shock absorbers. Endurance training ensures you can maintain these improvements throughout your day. Our therapists are experts at identifying hidden muscle weakness patterns that may be the true source of your pain. Learn more about our Therapeutic Exercise Brooklyn programs.
Enhancing Flexibility and Range of Motion with Manual Therapy
Our hands-on approach uses precise, therapeutic techniques to restore proper movement. Joint mobilization uses gentle, controlled movements to restore motion to stiff or restricted joints. We also use soft tissue massage and myofascial release to address muscle and fascial tightness that limits your movement.
We teach you specific stretching techniques that target your problem areas. These manual therapy methods improve joint mechanics and help your nervous system relearn efficient movement patterns. For more details, you can explore Manual Therapy techniques explained.
The Critical Role of Balance and Gait Training
Good balance is a complex skill that provides confidence in daily activities. Our fall prevention programs are crucial for older adults but benefit everyone by improving proprioception (your body's internal GPS). Neuromuscular re-education teaches your muscles and brain to communicate better through exercises that safely challenge your stability.
Gait training analyzes and corrects your walking pattern to eliminate issues causing pain or inefficiency. We also address the vestibular system (the balance center in your inner ear) with coordination exercises to improve stability. Our approach to Balance and Gait Training helps you move with confidence. We also offer specialized Physical Therapy for Seniors to prioritize safety and independence.
Specialized Physical Therapy for Diverse Mobility Needs
Mobility challenges are unique, so how does physical therapy deal with movement and mobility varies for each person. The approach for a runner with knee pain differs from that for a stroke survivor or a child with developmental delays.

At Evolve Physical Therapy, we tailor your care to your age, condition, and personal goals. A teen athlete's recovery plan will be different from that of someone managing Parkinson's disease.
Common Specializations in Physical Therapy
Physical therapy has many specializations to address specific needs:
- Orthopedic PT focuses on the musculoskeletal system (bones, muscles, joints), helping you recover from fractures, sprains, or surgery.
- Neurological PT addresses nervous system conditions like stroke, spinal cord injury, or Parkinson's disease, using neuroplasticity to restore function.
- Geriatric PT helps manage age-related challenges like arthritis and osteoporosis to keep you active and independent.
- Pediatric PT assists children with developmental delays or conditions like cerebral palsy to reach their full potential.
- Sports PT gets athletes back in the game safely. Our specialized physical therapy for athletes includes sport-specific training.
- Cardiopulmonary PT helps people with heart and lung conditions improve endurance. Other areas include vestibular, wound care, and pelvic floor therapy.
How Physical Therapy Supports Daily Living and Independence
Our goal is to help you feel capable and confident in your daily life. We focus on "functional mobility"—your ability to perform tasks that matter to you. This means helping you climb stairs with confidence or feel steady when reaching for high shelves.
We adapt exercises to mirror your real-world needs, whether it's standing comfortably to cook or using proper techniques for gardening. We also work on walking and running mechanics to help you move efficiently. Restoring the joy of movement and celebrating your independence is the real measure of our success.
The Long-Term Impact: Beyond the Clinic
Your physical therapy journey continues after your sessions end. We empower you with the knowledge and tools for self-management, helping you maintain your progress long-term. The goal is to integrate healthy movement principles into your daily lifestyle, making small, sustainable changes that become second nature.
How does physical therapy help individuals return to their usual activities?
Returning to the activities you love is a primary goal. How does physical therapy deal with movement and mobility for daily life? Through functional training. We focus on activities that mimic real-world movements, like practicing proper lifting for a parent or squatting patterns for a gardener.
Our rehabilitation is goal-oriented. For injured runners, our specialized return to running programs progressively prepare the body for the sport's demands. For athletes, we use sports-specific drills, and for workers, we provide work simulation exercises. The ultimate aim is regaining your independence so you can confidently engage in the activities that matter most.
How does physical therapy contribute to preventing future injuries and maintaining mobility?
Prevention is as important as treatment. We want to fix your current problem and ensure it doesn't return. Patient education is the foundation, teaching you proper body mechanics and how to modify harmful movements.
We provide ergonomic advice for your work environment and strategies for posture correction. Your home exercise program is your most valuable tool, featuring specific exercises for your needs, including the best mobility movements for your situation.
This focus on body mechanics training applies to everything you do, protecting you from future injury. Understanding how your body works empowers you to actively maintain your own physical well-being.
Frequently Asked Questions about Physical Therapy and Mobility
Starting physical therapy can bring up many questions. After helping patients for nearly two decades understand how does physical therapy deal with movement and mobility, I've heard most concerns. Here are answers to the most common ones.
How long does physical therapy take to improve mobility?
This is a common question, but the timeline is unique to each person. It depends on several factors:
- Acute conditions, like a recent sprain, may improve within a few weeks.
- Chronic conditions that have existed for months or years often take longer to address, as we need to reverse compensatory patterns.
- The severity of your injury is a major factor. A minor issue might take 4-6 weeks, while recovery from major surgery could take months.
- Patient adherence is key. Committing to your home exercise program and lifestyle changes leads to the fastest, most lasting results.
Is physical therapy painful?
This is a common fear. Physical therapy shouldn't be excessively painful, but some discomfort is normal, like the soreness from a new workout. You should not feel sharp, shooting pain.
Open communication with your therapist is vital. If something feels too intense, tell us immediately so we can adjust your treatment. There is a "good pain" that comes from working or stretching muscles, which is different from pain that signals a problem. Our ultimate goal is pain reduction, and temporary discomfort is sometimes necessary to achieve long-term relief.
Can physical therapy help with age-related mobility decline?
Absolutely! Age does not have to mean accepting a decline in mobility. Your body is adaptable at any age. We design safe exercises to manage conditions like arthritis and osteoporosis.
Our specialized programs, like elderly balance training, focus on fall prevention and building confidence. Maintaining independence is a primary goal, and we tailor treatment to help you with daily tasks like climbing stairs or getting up from a chair. By gradually building strength and confidence, we've helped clients in their 80s and 90s make remarkable improvements. It's never too late to reclaim your movement.
Take Control of Your Movement and Live Life to the Fullest
This guide has shown how does physical therapy deal with movement and mobility: through a comprehensive, patient-centered approach. From assessment to personalized treatment plans including strengthening, manual therapy, and balance training, our goal is to get you back to living without limitations.
Our holistic approach creates a treatment plan that works for your unique body, lifestyle, and goals. The power of physical therapy lies in empowering you with the knowledge and tools—like proper body mechanics and home exercises—to maintain your progress and prevent future problems.
At Evolve Physical Therapy + Sports Rehabilitation, our hands-on philosophy puts your needs first. We've seen patients go from chronic pain to completing marathons, and seniors regain the confidence to steer daily life. These stories remind us of what's possible with the right support.
Don't let pain or limited movement define your life. The path to better mobility starts with a single step. We're here to guide you on your journey back to pain-free movement and help you live life to the fullest again.
Explore our physical therapy services and let us help you evolve your movement, one session at a time.
Don't Slouch Your Way to Pain—Best Posture for Computer Work Explained
Why Proper Computer Posture Is Crucial for Your Health

The best posture for computer work involves maintaining a neutral body position with specific alignments that reduce strain on your musculoskeletal system. Here are the key elements:
Essential Computer Posture Guidelines:
- Feet: Flat on floor or footrest
- Knees: At 90° angle, at or below hip level
- Back: Fully supported with lumbar curve maintained
- Shoulders: Relaxed, not hunched forward
- Elbows: Bent between 90-120°, close to body
- Wrists: Straight and parallel to floor
- Head: Level, centered over shoulders
- Monitor: Top at or slightly below eye level, arm's length away
Spending 8-9 hours a day at a computer is common, but poor posture can lead to headaches, muscle fatigue, and widespread pain.
The stakes are high: bending your head forward just 15 degrees doubles neck pressure. Prolonged sitting also increases risks for diabetes and cardiovascular disease.
The good news is that proper ergonomics can prevent these issues. Maintaining a neutral body position—with naturally aligned joints—reduces stress on your muscles, tendons, and skeleton.
I'm Lou Ezrick, a physical therapist at Evolve Physical Therapy in Brooklyn. With nearly two decades of experience, I've helped countless professionals improve their health by adopting the best posture for computer work. Let me guide you to a pain-free work environment.
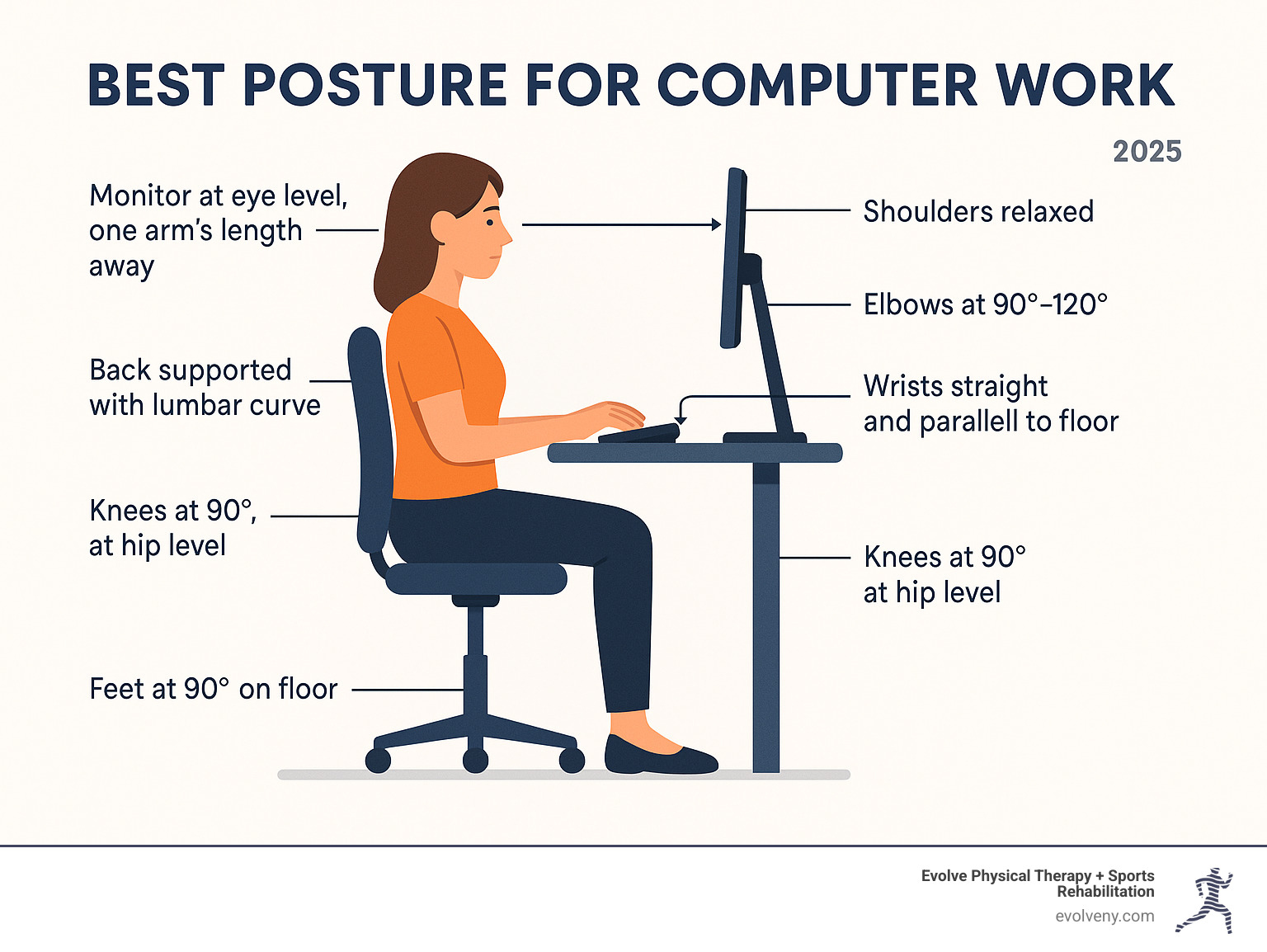
Why Poor Posture Is More Than Just a Bad Habit
Poor posture is more than just looking slouchy; it can wreak havoc on your body. Spending hours hunched over a computer can lead to serious musculoskeletal disorders (MSDs), affecting your muscles, nerves, tendons, joints, and spinal discs.
Bending your head forward just 15 degrees doubles the pressure on your neck—a significant strain over an 8-hour workday.
Poor posture also contributes to chronic neck and back pain, headaches, fatigue, and poor circulation. As research on the health risks of a sedentary lifestyle shows, prolonged sitting can even increase your risk of diabetes and cardiovascular disease.
At Evolve Physical Therapy, our specialized programs for Physical Therapy for Neck Pain Brooklyn and Physical Therapy for Back Pain Brooklyn help our community break free from chronic pain.
The good news? The best posture for computer work can prevent these issues, reducing pain, boosting energy, and improving circulation.
The Dangers of Slouching
Slouching involves forward head posture, rounded shoulders, and a compressed, C-shaped spine.
This creates spinal compression and nerve constriction, which can cause tingling or sharp pain in your arms and fingers. The ripple effects include headaches from neck tension, fatigue as your body works harder to stay upright, and even poor digestion from compressed organs.
We've written extensively about how Bad Office Posture creates these cascading health problems—and it's more serious than most people realize.
The Benefits of Sitting Tall
The benefits of proper posture go beyond pain avoidance.
Sitting tall can boost your confidence and mood. Better breathing is another benefit. An open chest allows your lungs to expand fully, increasing oxygen intake for more energy and improved focus.
Proper alignment also allows for optimal digestion by not compressing internal organs. Most importantly, it leads to reduced stress on joints and ligaments, minimizing long-term wear and tear.
The best posture for computer work helps your body function as designed, leaving you feeling significantly better.
The Ultimate Guide to the Best Posture for Computer Work
The best posture for computer work isn't a rigid stance but a relaxed, neutral position where your joints are aligned and muscles are not strained. This is achieved with neutral body positioning, where your spine keeps its natural curves and your muscles work efficiently without being overworked.
A simple guideline is the 90/90/90 rule: aim for 90-degree angles at your elbows (90-120 degrees), hips, and knees. However, your body needs variety, so slight adjustments and frequent movement are encouraged.

There's no single "perfect" posture; the goal is a comfortable, supported, and balanced position. For visual aids, see our Correct Computer Posture guide and OSHA's guide to good working positions.
Achieving the Best Posture for Computer Work: A Body-Part Breakdown
Let's build your posture from the ground up.
- Feet: Keep them flat on the floor or a footrest to create a stable base. This distributes weight evenly and reduces lower back pressure.
- Knees: Aim for a 90-degree angle, with knees at or slightly below hip level. Leave a two-inch gap between the back of your knees and the chair to ensure good circulation.
- Back: Sit all the way back in your chair, ensuring your lower back's natural curve is supported by the backrest or a lumbar cushion. A slight recline to 100-110 degrees can also reduce pressure on your spine.
- Shoulders: Keep them relaxed, low, and not hunched forward. Your upper arms should be close to your body.
- Elbows: Bend them at a 90 to 120-degree angle, close to your body. This allows your forearms to be parallel to the floor, reducing strain.
- Wrists: Keep them straight and in line with your forearms, avoiding bending them up, down, or sideways. They should feel like a natural extension of your arms.
- Head: Balance it directly over your shoulders, keeping it level. A gentle chin tuck helps align your ears over your shoulders. Avoid tilting your head forward, as even a 15-degree tilt doubles neck pressure.
When you put all these pieces together, you'll find what truly constitutes Ideal Desk Posture.
Common Mistakes to Avoid for the Best Posture for Computer Work
Avoid these common habits that can sabotage the best posture for computer work:
- Crossing your legs: This misaligns your hips and restricts blood flow.
- Dangling feet: This strains your lower back. Use the floor or a footrest for support.
- Reaching for the mouse: Keep your mouse close to the keyboard to avoid straining your shoulder and wrist. Move it with your whole arm.
- Cradling the phone: This leads to neck pain. Use a headset for frequent calls.
- Hunching forward: This common habit increases pressure on your neck and back. Consciously sit back and let your chair support you.
- Tilting your head: This often indicates your monitor is at the wrong height. Adjust your screen instead of your neck, especially if you wear bifocals.
- Slouching or sliding forward: This flattens your spine's natural curve. Keep your bottom against the back of the chair.
- Twisting your back: Center your monitor and keyboard in front of you to avoid rotational strain on your spine.
Creating Your Ergonomic Workstation: A Step-by-Step Setup
Your workstation must support the best posture for computer work. A poor setup will sabotage even the best intentions. At Evolve Physical Therapy, I've seen many patients whose workspaces were the root of their problem. A low monitor, unsupportive chair, or high desk can undo all your efforts.

The good news is that creating an ergonomic workstation is about smart adjustments, not expensive overhauls. For additional guidance, you might find our detailed article on the Best Ergonomic Way to Sit at Desk helpful, and Mayo Clinic offers an excellent A how-to guide on office ergonomics.
Your Chair: The Foundation of Good Posture
Your chair is the most important part of your workstation. It's the foundation that supports your entire body. Here's how to adjust it:
- Adjustable height: Adjust your chair so your feet are flat on the floor and thighs are parallel to it. Use a footrest if your feet dangle.
- Seat depth: Ensure a 1-2 inch gap between the back of your knees and the chair's edge when sitting all the way back. This promotes circulation and back support.
- Lumbar support: Your chair should support the natural inward curve of your lower back. Use the chair's adjustable support or a small cushion.
- Armrest height: Adjust armrests so your shoulders are relaxed and elbows are close to your body, with forearms parallel to the floor. This reduces shoulder and neck strain.
- Swivel base: A swivel base allows you to turn easily, preventing spinal twisting.
Your Desk, Monitor, and Accessories
With your chair adjusted, arrange your desk, monitor, and accessories. Monitor placement is critical for the best posture for computer work.
- Monitor at eye level: The top of your screen should be at or just below eye level. Lower it slightly if you wear bifocals to avoid tilting your head back.
- Distance: Place your monitor an arm's length away (20-40 inches) to reduce eye strain and prevent leaning.
- Laptops: Laptops are not ergonomic for long-term use because the screen and keyboard are attached. The solution is an external keyboard and mouse. This lets you use a laptop stand to raise the screen to eye level while keeping your arms in a good position.
- Frequently used items: Keep essentials within easy reach to avoid stretching or twisting. Use a headset for phone calls to prevent neck strain.
If you want personalized guidance, we offer Physical Therapy for Ergonomic Assessment services in Brooklyn to help you achieve the best posture for computer work.
Beyond the Chair: Movement and Stretches to Counteract Sitting
Even with a perfect setup and the best posture for computer work, your body needs to move. Static posture leads to stiffness, poor circulation, and muscle fatigue. The dangers are well-documented: it causes muscles to tighten and weaken, decreases blood flow, and leads to a buildup of waste products in your muscles.
Experts recommend taking a 5-10 minute movement break every 30-50 minutes. The Pomodoro Technique (25 minutes of work, 5-minute break) is an effective way to structure this. These breaks are essential. Standing and walking improve circulation, engage muscles, and decompress the spine, acting as a reset for your body.

Simple Stretches You Can Do at Your Desk
Simple desk stretches require no equipment and can transform how you feel by targeting the neck, shoulders, and wrists.
- Neck tilts and chin tucks: Gently tilt your ear toward your shoulder (hold 15-20 seconds per side). Also, perform chin tucks by pulling your chin straight back to realign your head.
- Shoulder rolls and pinches: Slowly roll your shoulders forward and backward. Then, squeeze your shoulder blades together for 5-10 seconds to release tension.
- Overhead reach: Interlace your fingers and press your palms toward the ceiling to open your chest and counteract hunching.
- Torso twist: While seated, gently rotate your torso to each side, holding for 15-20 seconds to maintain spinal mobility.
- Wrist stretches: Extend your arm and gently pull your fingers down (palm up) and then up (palm down), holding each stretch for 15-20 seconds.
For more advanced techniques, see our article on What is Assisted Stretching and How Can It Help Me?.
Integrating Movement into Your Workday
Integrate movement into your workday with a little creativity. Find and maximize existing opportunities:
- Walk during calls: If you don't need your screen, stand up and pace during phone calls.
- Take the stairs: Choose stairs over the elevator for a mini-workout that breaks up sitting.
- Set movement reminders: Use an app or alarm to remind you to move every 30-50 minutes.
- Take short walks: Aim for a short walk every hour—even a lap around the office helps improve circulation and energy.
- Stand while working: Perform tasks like reading emails or taking calls while standing. Alternate between sitting and standing if you have an adjustable desk.
These strategies, combined with proper ergonomics, support the best posture for computer work. For more structured approaches, consider our Therapeutic Exercise Programs.
Frequently Asked Questions about Computer Posture
Here are answers to common questions I hear at Evolve Physical Therapy about achieving the best posture for computer work.
How often should I take a break from sitting?
Experts recommend taking a 5-10 minute break every 30 to 50 minutes. Stand, stretch, and walk around to improve circulation and relieve muscle tension. Listen to your body—if you feel stiff, it's time to move.
What is the most important part of my workstation to adjust?
Your chair is the most critical component. It's the foundation for your entire posture. An adjustable, supportive chair allows you to position your body correctly, supporting your lumbar curve, allowing feet to rest flat, and keeping arms comfortable. Get this right before focusing on other accessories.
Are standing desks a better alternative to sitting?
Standing desks are a great tool, but the goal is to vary your posture, not just to stand all day. Standing for prolonged periods can also cause issues. The ideal setup is an adjustable desk that allows you to easily alternate between sitting and standing. Movement and variety are key to staying pain-free.
Conclusion
Achieving the best posture for computer work comes down to three key pillars:
- Maintain a neutral spine: Keep your joints naturally aligned to reduce stress and strain.
- Create an ergonomic workstation: Use an adjusted chair, properly positioned monitor, and an accessible layout to support your body.
- Move regularly: Take frequent breaks to stretch and walk. Movement is essential for preventing stiffness and maintaining circulation.
Embracing these principles is a proactive investment in your long-term health, leading to better circulation, more energy, improved focus, and a better mood.
This proactive approach to pain prevention is central to our philosophy at Evolve Physical Therapy + Sports Rehabilitation. Our holistic method focuses on evaluation, healing, and strengthening, with a hands-on approach and specialized programs like our NBC News-featured Rock Steady Boxing for Parkinson's patients.
If you're dealing with discomfort or want to optimize your workspace, we can help. A professional eye can spot issues and provide personalized solutions.
For a professional evaluation of your workspace and personalized guidance, consider an Ergonomic Physical Therapy assessment in Brooklyn. Let us help you evolve beyond pain and into a more comfortable, productive, and healthier workday.
Move Better, Feel Better – Physical Therapy Meets Wellness
Your Path to a Healthier Life: Physical Therapy and Wellness
Ready to move better, feel better, and live better? Physical therapy and wellness offers a powerful, holistic path to achieving just that. Here's a quick overview of this combined approach and its core benefits:
What is Physical Therapy and Wellness?
- It's a comprehensive approach that goes beyond just treating injuries.
- It focuses on restoring movement, reducing pain, and improving your overall quality of life.
- It empowers you to take control of your health proactively.
Key Benefits Include:
- Improved Mobility and Function: Helps you regain lost movement and move with ease.
- Effective Pain Management: Addresses the root cause of pain, often without medication or surgery.
- Increased Energy and Activity: Builds strength and stamina for a more vibrant lifestyle.
- Injury Prevention: Teaches you how to protect your body from future issues.
- Improved Mental Well-being: Contributes to a positive outlook and reduced stress.
Many think of physical therapy only after an injury or surgery. But it's much more than fixing what's broken. It's about proactive health and open uping your body's full potential.
This guide shows how integrating physical therapy with wellness principles creates a powerful, lasting approach to your health. It’s about building a strong foundation for a vibrant, active life.
As Louis Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades helping thousands achieve optimal function and quality of life through comprehensive physical therapy and wellness practices. My experience, from elite rehabilitation in Tel Aviv to pioneering a patient-first approach in Brooklyn, has shown me the profound impact of holistic, hands-on care on long-term well-being. This philosophy guides our approach to every patient's unique needs.

The Integrated Approach: Understanding Physical Therapy and Wellness
What does it truly mean to feel your best, inside and out? At Evolve Physical Therapy, we believe it's more than just fixing what hurts. It's about bringing your mind and body into harmony, helping you open up your highest physical potential and enjoy life. This is the essence of physical therapy and wellness.
So, what is physical therapy? It's a dynamic healthcare journey focused on improving how you move and function. It’s a safe, non-invasive, and drug-free way to manage pain, often offering an alternative to surgery or medications. Our expert physical therapists use movement, hands-on care, and clear explanations to help you regain mobility, boost independence, and flourish. Our goal is getting you back to the things you love, whether that's chasing grandkids or tackling a marathon.
Now, let's talk about wellness. It isn't just about 'not being sick.' It's actively pursuing a healthy, vibrant life where you feel your absolute best. It’s about being proactive with your health—preventive maintenance for your body. Wellness touches your physical health, mental clarity, emotional balance, and social connections. When we combine physical therapy and wellness, we create a holistic approach. We treat you—the whole person—not just an injury. Our commitment is to your total well-being in a compassionate environment.
Our philosophy is simple: it’s all about you. Our patient-centered approach means we listen to your unique story and personal goals. We then craft a personalized care plan that fits your life. We champion 'movement as medicine' because it's powerful. It improves strength, balance, mobility, and overall fitness, paving the way for a more active, joyful life. Did you know that moving more can reduce a person’s perception of pain by up to 28%? It’s true—movement is key!
The Core Principles of a Wellness-Focused Practice
Our practice at Evolve Physical Therapy is built on core principles that ensure you receive comprehensive and effective care:
First is Patient Education and Empowerment. We believe knowledge is power. The more you understand your body and condition, the more control you have over your healing. We'll teach you self-management strategies so you can make confident health choices.
Next is our dedication to Hands-On Care. We believe in the power of touch. This often means one-on-one sessions with our undivided attention. Techniques like Manual Therapy use skilled hands to restore function and soothe pain.
You'll also experience Personalized Treatment Plans. Your body and goals are unique, so we craft a plan specifically for you, ensuring every session brings you closer to feeling amazing.
A big part of our philosophy is Prevention Over Reaction. We don't just fix problems; we help you prevent them. We'll teach you strategies to avoid future injuries, shifting from a 'sick-care' model to a proactive, 'well-care' approach to build resilience.
Finally, our practice is grounded in Evidence-Based Practice. Our methods are rooted in solid science. We use proven treatments to help you recover quickly and achieve lasting results. You can trust you're in capable, knowledgeable hands.
Your Partner in Recovery and Rehabilitation
Think of Evolve Physical Therapy as your dedicated partner in recovery and rehabilitation. Our physical therapists are highly trained, compassionate, and knowledgeable professionals committed to your success.
Our process begins with a thorough initial evaluation to efficiently pinpoint the root cause of your discomfort or limitation. Understanding the 'why' is crucial for effective treatment.
From there, we work with you to set realistic and achievable goals. Whether it's picking up your child without pain or returning to the tennis court, your goals become our shared mission.
Then, we design custom exercise programs for your needs. These aren't generic routines; they're carefully crafted to restore mobility, regain independence, and build long-term strength. Our aim is to help you move freely and confidently again—to get you back to enjoying life without limitations. As many patients share, we're here to help you achieve renewed mobility and pain relief, guiding you back to the activities you cherish.
Ready to move better and feel stronger? Explore our Therapeutic Exercise Programs
The Comprehensive Benefits: More Than Just Pain Management
When you think of physical therapy and wellness, you might picture recovering from surgery or a sports injury. But this approach offers much more than fixing what's broken; it's about changing your relationship with your body and health.

The best part of our work is watching patients refind what their bodies can do. Improved mobility isn't just about bending or reaching; it's about regaining independence. When you can climb stairs, carry groceries, or play with your grandchildren without pain, life opens up again.
This restoration of movement creates a ripple effect. You stop planning your day around pain and start thinking about activities you want to pursue. That's what we mean by improved quality of life—getting back to being you.
A Safer Alternative for Pain Relief
Let's be honest about pain management. When pain is constant, immediate relief is a natural desire. Many face a difficult choice: live with discomfort or rely on risky medications.
Physical therapy and wellness offers a third, safer path. Whether you're dealing with chronic pain or acute pain from a recent injury, our approach focuses on understanding why you hurt, not just temporarily masking it.
Masking pain without addressing its source is like putting tape over your car's engine light. Our non-invasive treatment methods dig deeper to restore proper body function.
The beauty of this approach is that avoiding opioids doesn't mean less effective care. Research shows that moving more can reduce a person's perception of pain by up to 28%. By strengthening muscles, improving posture, and restoring natural movement, you're not just managing pain—you're eliminating its root causes.
Physical therapy as a safe alternative to opioids Physical Therapy for Back Pain
Boosting Energy and Fostering an Active Lifestyle
That afternoon slump you blame on age or stress might be your body asking for more movement, not rest. It seems counterintuitive, but combating fatigue often requires expending energy, not conserving it.
When we work to improve your energy levels naturally, we're teaching your body to be more efficient. Stronger muscles, better balance, and improved flexibility mean your body works less for daily tasks. The connection between physical health and energy is remarkable. Many patients are amazed at how much more vibrant they feel once their bodies move properly again. Some even find that treatments like acupuncture can encourage natural healing while boosting mood and energy levels.
But energy is just the start. Supporting an active lifestyle means building the foundation for activities that bring you joy. Whether it's hiking, dancing, or gardening, we're here to ensure your body is ready.
The bonus? The mental health benefits. When you feel strong and capable, your mind follows. Regular movement boosts mental awareness, improves mood, and significantly lowers the risk of anxiety and depression.
9 tips to boost your energy Physical Therapy for Wellness
What to Expect: Common Conditions and Therapies
Starting your physical therapy and wellness journey with us means finding a trusted guide. We know you want answers and relief. Your path begins with a thorough initial evaluation where we listen to your story, understand your issues, and find the root of your symptoms. Many patients are amazed at how quickly we pinpoint the source of their discomfort.
From there, we craft a personalized treatment plan for you. This isn't a one-size-fits-all approach; it's a unique blend of hands-on techniques and targeted therapeutic exercises designed to help you heal, recover, and grow stronger.

Conditions That Benefit from Physical Therapy and Wellness
Many conditions benefit from our comprehensive approach. Here's a list of common issues we address:
- Back & Neck Pain: From general discomfort to sciatica, herniated discs, whiplash, or poor posture. Spinal decompression therapy can be particularly effective for these conditions.
- Shoulder Pain: Rotator cuff injuries, frozen shoulder, bursitis, or tendonitis.
- Knee Pain: MCL tears, ligament tears, and post-total knee replacement rehabilitation.
- Arthritis: Especially osteoarthritis, we provide strategies for pain management and healthy habits.
- Sciatica: We target the root causes of this radiating pain for lasting relief.
- Sports Injuries: From sprains and strains to more complex issues, we help athletes of all levels return to their game.
- Post-surgical rehab: We offer comprehensive pre- and post-surgical rehabilitation to help you regain strength and function quickly.
- Balance and Vertigo: Our balance training improves stability and reduces fall risk.
- Parkinson's Disease: We offer specialized treatments like LSVT BIG and our unique Rock Steady Boxing program to improve movement and quality of life.
A Toolbox of Specialized Services
To treat these conditions, we use a diverse toolbox of specialized services. We often use Manual Therapy, a hands-on approach where our therapists use their touch to manipulate muscles and soft tissues, helping restore function and ease pain.
You might also experience techniques like Active Release Therapy, a system designed for muscles, tendons, ligaments, and nerves. Or the Graston Technique, which uses special instruments to address scar tissue and fascial tightness.
For ongoing support, we might use Kinesio Taping. This rehabilitative tape helps your body's natural healing process by offering gentle support to muscles and joints.
To complement your therapy, we also offer Massage Therapy to ease tension and reduce discomfort. And for those with Parkinson's disease, we're proud of our Rock Steady Boxing program, a non-contact boxing approach that improves balance, strength, and quality of life.
Choosing Your Path: What to Look for in a Physical Therapy Clinic
Choosing the right partner for your physical therapy and wellness journey is a big decision. We believe in transparency so you can make the best choice for your health.

When picking a clinic, look for qualifications and experience. You want a team with advanced training. Our founder, for example, has over two decades of experience, ensuring you're in capable hands.
Next, seek clinics that prioritize one-on-one care. This means you get the therapist's undivided attention for personalized, effective treatment. Private treatment rooms also provide a comfortable, focused environment for healing.
Also, check patient testimonials. Hearing from others provides a sense of what to expect. Our patients often share how our team helped them improve. Finally, consider insurance acceptance. Understanding your coverage is important. We accept most major insurance plans and can help you steer your benefits. We also offer cash-pay wellness visits, often covered by Health Savings Accounts (HSA), for proactive or continued care.
The Importance of a Holistic and Personalized Approach
At Evolve Physical Therapy, we treat the whole person, not just the part that hurts. Our holistic approach brings your mind and body into harmony, considering how your physical, mental, and emotional well-being are connected.
We value clear communication, listening to your story and explaining everything simply so you're an active participant in your care. Our customized plans are built for you, as a "one-size-fits-all" approach doesn't work. For example, our specialized programs for seniors help them maintain independence and quality of life.
Comparing Physical Therapy and Wellness to Other Options
When you're in pain, you have options. Here's how physical therapy and wellness compares to other choices:
| Feature | Physical Therapy and Wellness | Medication (e.g., Opioids) | Surgery |
|---|---|---|---|
| Approach | Treats the underlying source of pain; holistic. | Masks symptoms; chemical intervention. | Invasive procedure to repair or remove tissue. |
| Nature | Non-invasive, drug-free, movement-based. | Oral, injectable; systemic effects. | Invasive; requires anesthesia, incisions. |
| Goal | Long-term solution; restore function, prevent recurrence. | Temporary pain relief; often short-term fix. | Structural repair; may require long recovery. |
| Side Effects | Positive side effects: improved mobility, strength, independence. | Nausea, addiction, constipation, fatigue, cognitive issues. | Infection, bleeding, nerve damage, scarring, long recovery. |
| Cost-Effectiveness | Often more cost-effective as a first intervention; avoids long-term drug costs/surgical expenses. | Ongoing prescription costs. | High upfront costs, often significant recovery expenses. |
| Empowerment | Empowers patient with self-management strategies. | Patient reliant on medication. | Recovery largely dictated by procedure; often requires PT. |
Choosing physical therapy and wellness is often the most cost-effective first step, potentially saving you thousands compared to medication or surgery. Our focus is on empowering you to heal and build lasting strength, not just temporarily easing symptoms. We aim to help you avoid unnecessary drugs, injections, or surgery whenever possible.
Frequently Asked Questions about Physical Therapy and Wellness
Starting your physical therapy and wellness journey can feel overwhelming when you're dealing with pain. We get it. Here are answers to the most common questions we hear from patients.
Do I need a doctor's referral to see a physical therapist?
Great news: you typically don't need a doctor's referral to start physical therapy in New York State. Thanks to direct access laws from 2006, licensed physical therapists with at least three years of experience can evaluate and treat you without a referral for up to 30 days or 10 appointments, whichever comes first.
This means you can take action sooner. Physical therapy and wellness can be a safe, cost-effective first step before considering more invasive options.
That said, we always keep your overall health in mind. If you're not progressing within that 30-day window, or if your condition warrants it, we'll recommend you see your doctor. While diagnostic testing is sometimes helpful, it's often not needed right away if your discomfort developed gradually.
Is physical therapy painful?
This is a common and understandable question. You're already in discomfort and don't want more pain.
The truth is, our primary goal is pain relief. We use healing treatments like ultrasound, electrical stimulation, and heat or cold therapy to reduce your discomfort. Often, simply moving again brings significant relief.
However, as we work to restore mobility and strengthen weak areas, you might feel some discomfort. We discuss "good pain" versus "bad pain" with our patients. Good pain is the productive feeling of stretching or strengthening. Bad pain is sharp, new, or worsening discomfort that signals a problem.
Communication is key. We need you to tell us about your comfort level so we can adjust your treatment plan. We're always listening and adapting our approach based on your feedback.
How long does a typical treatment plan last?
The answer depends on several factors, but we can help you set realistic expectations.
Acute issues, like a recent injury, might resolve in a few weeks with consistent treatment. Chronic conditions typically require several months of dedicated therapy for lasting improvement.
Your personal goals also play a huge role. Returning to weekend hiking requires a different timeframe than returning to competitive sports.
Consistency is key to your success. Our appointments last about an hour and a half, allowing time for hands-on treatment, therapeutic exercises, and education. We'll also give you exercises to do at home to keep your progress moving forward.
We work collaboratively with you throughout the process, setting realistic goals, tracking progress, and adjusting the plan as needed. You're never left wondering where you stand.
Conclusion: Take the First Step Towards a Healthier You
We hope you now see how transformative physical therapy and wellness can be. It's more than mending what's broken; it's embracing a proactive way to live, move, and feel your absolute best.
Imagine moving freely with less pain, more energy, and a vibrant quality of life. That's the power of this integrated approach. By focusing on the root causes of your discomfort and empowering you with knowledge, we help you build a foundation for long-term wellness.
At Evolve Physical Therapy + Sports Rehabilitation, we're passionate about making this a reality for you. We believe in a holistic, hands-on approach that treats the whole person, not just a symptom. From our specialized programs like Rock Steady Boxing for Parkinson’s patients—highlighted on NBC News!—to our dedication to evaluation, healing, and strengthening, we're here to guide you.
Serving Brooklyn communities like Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, our mission is simple: to help you move better, feel better, and live better.
Don't let discomfort hold you back from the active, fulfilling life you deserve. Take control of your health and start on a path towards lasting wellness.




























