Brooklyn Physical Therapy News- Evolve NY
Healing in Brooklyn: Rehab Centers That Get You Back on Track
Finding Your Path to Recovery in Brooklyn

If you're looking for a Brooklyn rehabilitation center, here's what you need to know:
- Top-rated facilities: Leading rehabilitation centers with excellent reputations for quality care
- Treatment types: Physical therapy, neurological rehab, substance abuse treatment, short and long-term care
- Therapy intensity: Leading centers provide minimum 3 hours daily therapy (15 hours weekly)
- Specializations: Stroke recovery, orthopedic injuries, cardiac rehab, substance abuse, geriatric psychiatry
- Cultural services: Many centers offer multilingual care for Brooklyn's diverse population
Brooklyn rehabilitation centers offer comprehensive care pathways designed to help you regain function, mobility, and independence after injury, surgery, or illness. Whether you're recovering from a sports injury, managing a chronic condition, or seeking specialized rehabilitation services, Brooklyn's diverse healthcare landscape provides options custom to your unique needs.
The borough is home to world-class facilities ranging from boutique recovery centers with rooftop lounges to cutting-edge medical complexes equipped with aquatic therapy pools and robotics suites. What sets Brooklyn's rehabilitation ecosystem apart is the combination of clinical excellence, cultural competence, and innovative approaches to recovery.
As Lou Ezrick, I've spent nearly two decades helping patients steer Brooklyn's rehabilitation landscape, specializing in manual therapy and movement optimization at Evolve Physical Therapy + Sports Rehabilitation, a Brooklyn rehabilitation center known for its patient-first approach and specialized treatment for complex conditions like chronic pain and post-surgical rehabilitation.

Mapping the Rehabilitation Landscape in Brooklyn
Brooklyn's rehabilitation landscape is as colorful and diverse as the borough itself. From waterfront facilities with breathtaking views in DUMBO to welcoming community clinics nestled in Midwood, finding your way through the rehabilitation options can feel like navigating a new neighborhood for the first time.

At Evolve Physical Therapy + Sports Rehabilitation, we've seen how overwhelming this journey can be. Many of our patients initially come to us confused about where to turn for their specific recovery needs. Think of this guide as your local friend, helping you find the perfect spot in Brooklyn's rehabilitation community that feels just right for you.
Key Service Categories
When looking for a Brooklyn rehabilitation center, understanding the different types of care available will help you make the best choice for your recovery journey.
Physical rehabilitation centers form the backbone of Brooklyn's recovery landscape, offering therapeutic exercise, hands-on manual therapy, and specialized equipment to help you regain function after injury or surgery. Whether you're recovering from a knee replacement or working through chronic back pain, these centers provide the expertise to get you moving again.
For those recovering from neurological challenges like stroke or traumatic brain injury, specialized neurological rehabilitation programs offer hope and progress. These centers employ experts who understand the brain's remarkable ability to rewire itself and create new pathways for movement and function.
Cardiac rehabilitation programs provide a safe environment for heart patients to rebuild strength and confidence under careful monitoring. These specialized programs combine exercise, education, and emotional support to help patients recover from cardiac events and prevent future ones.
Many Brooklyn rehabilitation centers also address substance abuse recovery, offering comprehensive programs from detoxification through outpatient care. These facilities recognize addiction as a health condition requiring compassionate, evidence-based treatment.
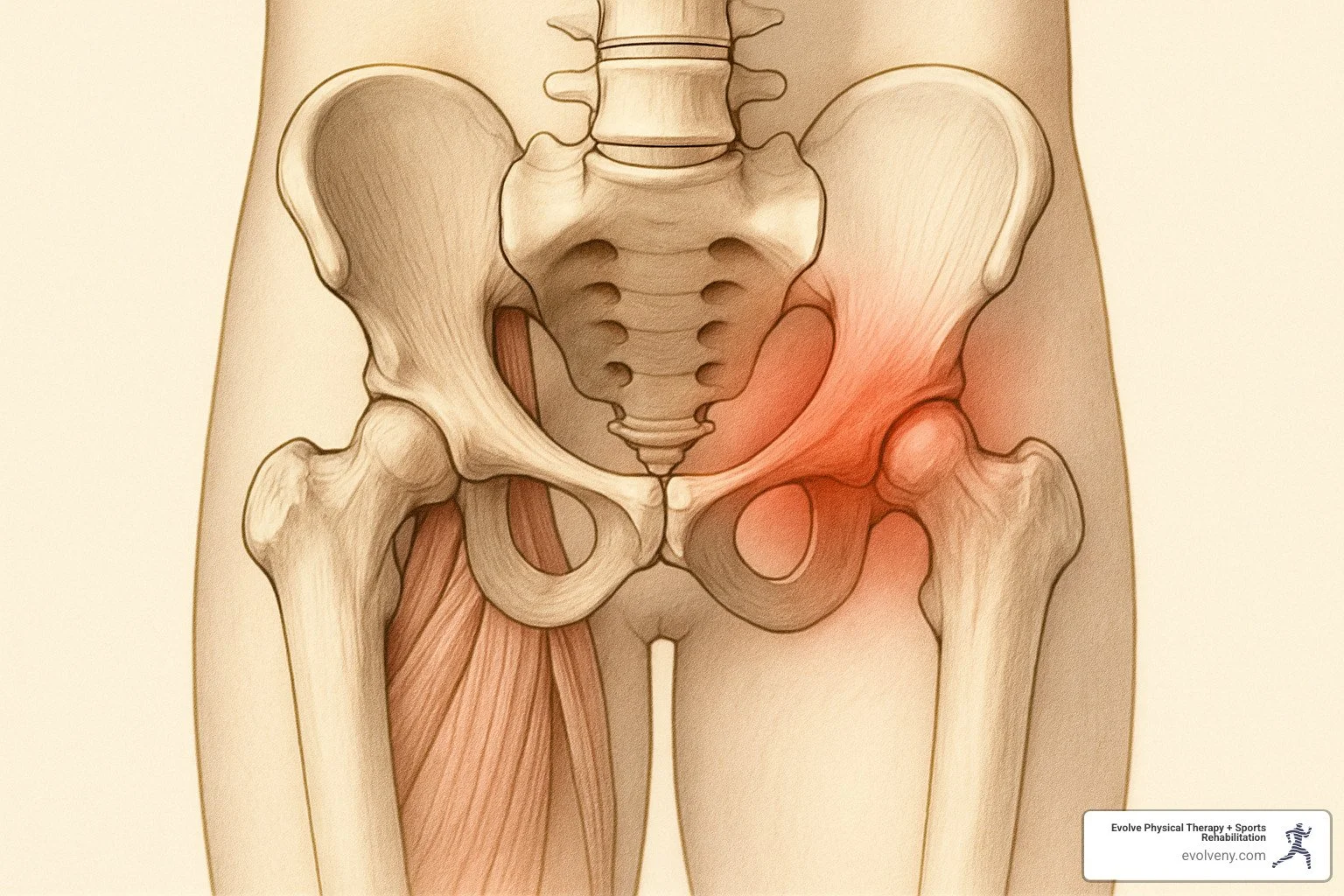
Orthopedic rehabilitation specialists focus on bones, joints, and muscles, helping patients recover from surgeries, sports injuries, and conditions like arthritis. Their expertise ensures proper healing and prevents future injuries through education and targeted strengthening.
For more information about specialized physical therapy services, visit our Physical Therapy in Brooklyn, NY page.
Patient Populations Served
The beauty of Brooklyn's rehabilitation landscape lies in its ability to serve everyone who calls this borough home.
Seniors find specialized care at facilities with geriatric specialists who understand the unique challenges of aging bodies and minds. These highly-rated facilities offer comprehensive programs to help older adults maintain independence and quality of life.
Athletes—from weekend warriors to professional competitors—benefit from sports-specific rehabilitation that addresses not just recovery but performance improvement and injury prevention. These specialized programs understand the demands of different sports and tailor treatment accordingly.
Trauma survivors receive compassionate care addressing both physical and emotional aspects of recovery. These programs recognize that healing involves the whole person, not just the injured body part.
Post-surgical patients follow carefully designed protocols to ensure proper healing and optimal outcomes. From joint replacements to cardiac procedures, rehabilitation plays a crucial role in successful surgical recovery.
The Brooklyn rehabilitation center landscape also accepts our borough's incredible diversity. Many facilities offer multilingual services and culturally sensitive care for Spanish-speaking residents and other communities. Programs designed for specific cultural communities ensure that language and cultural differences never stand in the way of quality care.
At Evolve Physical Therapy + Sports Rehabilitation, we're proud to be part of this rich mix, serving patients across Brooklyn's diverse neighborhoods including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin with personalized, compassionate care that respects each individual's unique background and needs.
Choosing a Brooklyn Rehabilitation Center: 10 Factors That Matter
Finding the right Brooklyn rehabilitation center is a bit like finding the perfect apartment in the borough – location matters, but so do the amenities, the people, and that special feeling when you walk through the door. After helping thousands of Brooklyn residents find their path to recovery, I've seen how the right choice can make all the difference in your healing journey.
When you're evaluating your options, keep these ten essential factors in mind:

Your recovery deserves thoughtful consideration of therapy intensity – look for centers that provide at least 3 hours of daily therapy. The center's specialization should align with your specific condition, whether it's stroke recovery, sports injury, or post-surgical rehabilitation. Don't overlook proper accreditation (like Joint Commission or CARF), which serves as your quality assurance.
The expertise of your rehabilitation team will directly impact your progress, so ask about their qualifications and experience with your condition. And while fancy amenities aren't everything, innovative technologies like aquatic therapy pools and robotics can significantly improve your recovery experience.
Insurance acceptance is practical but crucial – make sure to understand what's covered and any potential out-of-pocket costs before you begin. The center's location should be convenient not just for you but for family members who'll be supporting your journey. The best Brooklyn rehabilitation centers offer a seamless continuum of care, allowing you to transition between levels as you progress.
For Brooklyn's wonderfully diverse communities, cultural competence matters – from staff who speak your language to understanding cultural nuances that affect your care. Finally, don't hesitate to research patient outcomes and reviews for your specific condition – real experiences tell you what brochures can't.
Brooklyn rehabilitation center Accreditation & Expertise
When it comes to rehabilitation, credentials matter. Think of accreditation as Brooklyn's version of the health department's letter grade system for restaurants – it tells you someone's been checking the quality.
The best Brooklyn rehabilitation centers proudly display their Commission on Accreditation of Rehabilitation Facilities (CARF) certification, which specifically evaluates rehabilitation services. The Joint Commission accreditation offers another gold standard for overall healthcare quality and safety. And just like you might look for that perfect 5-star review on Yelp, many facilities highlight their 5-Star CMS rating from the Centers for Medicare & Medicaid Services.
But buildings don't heal people – people do. The expertise of your rehabilitation team is where the magic happens. Leading centers assemble multidisciplinary teams that work together like a well-rehearsed Brooklyn band. Your recovery orchestra might include board-certified physiatrists conducting the overall medical management, physical therapists helping you regain strength and mobility, occupational therapists guiding you back to daily activities, and speech-language pathologists improving communication skills.
Some conditions require specialized players like neuropsychologists, rehabilitation nurses, respiratory therapists, and social workers who help coordinate your return to community life. At Evolve Physical Therapy + Sports Rehabilitation, we believe that ongoing education keeps our clinical team sharp and current with the latest rehabilitation science – because your recovery deserves nothing less than the best.
Brooklyn rehabilitation center Amenities & Technology
Brooklyn has always been at the forefront of innovation, and our rehabilitation centers are no exception. The technology and amenities available at a Brooklyn rehabilitation center can transform your recovery from good to exceptional.
Imagine doing your rehabilitation exercises while floating in water, where gravity's effects are minimized and movement becomes possible again. Many centers offer this experience with dedicated Aqua Therapy Pools, providing the perfect environment for gentle, resistance-based healing.
For patients relearning to walk after a stroke or spinal cord injury, robotics-assisted therapy has been a game-changer. These sophisticated exoskeletons and gait trainers provide just the right amount of support while your brain and body rebuild those crucial connections. For those battling chronic pain, specialized centers offer Scrambler Therapy – an FDA-approved technique that essentially "rewires" how your brain interprets pain signals.
Some forward-thinking facilities have acceptd virtual reality, turning rehabilitation exercises into engaging activities that feel more like play than therapy – particularly helpful for balance training and cognitive rehabilitation. And recovery doesn't have to feel clinical; some facilities prove this with boutique settings featuring stunning rooftop lounges overlooking the NYC skyline, where healing happens with a view.
Even the small comforts matter – like personal bedside tablets loaded with entertainment and communication features to keep you connected and engaged during your stay. After all, healing happens best when both body and spirit are nurtured. Learn more about our specialized Sports Rehab Physical Therapy Brooklyn and Neuromuscular Physical Therapy Brooklyn programs that incorporate many of these innovative approaches.
Admissions & Insurance Made Simple
Let's face it – paperwork is nobody's favorite part of healthcare. Fortunately, most Brooklyn rehabilitation centers have streamlined their admissions process to get you focused on healing rather than forms.
The journey typically begins with a referral – often from your hospital or physician, though many outpatient services accept self-referrals too. Next comes the pre-admission screening, where the facility assesses your medical needs and verifies your insurance coverage. Based on this information, they'll develop a personalized care plan with specific rehabilitation goals custom to your situation. Finally, you'll be formally admitted to the program and can begin your recovery journey.
Understanding insurance coverage can feel like deciphering the Brooklyn subway map during construction season. Most centers accept Medicare (Parts A and B), Medicaid, and a variety of private health insurance plans. If your injury happened at work, workers' compensation might cover your rehabilitation. Many facilities also offer self-pay options and sliding scale fees for those without comprehensive coverage, and some programs qualify for state-funded plans.
If the financial aspects feel overwhelming, you're not alone. Many centers provide dedicated financial counselors to help you understand your coverage and steer potential out-of-pocket expenses. For those interested in specialized rehabilitation for surgical recovery, check out our detailed guide to Physical Therapy for Surgery & Post-Op Rehab.
The right Brooklyn rehabilitation center will make you feel supported not just physically, but through every aspect of your recovery journey – including the paperwork.
Innovations Fueling Faster Recovery
Brooklyn has become a true hotspot for rehabilitation innovation, where forward-thinking centers are embracing cutting-edge approaches that help patients recover faster and achieve better outcomes.
Advanced Therapies in Action
When you visit a Brooklyn rehabilitation center today, you'll find technologies and approaches that seemed like science fiction just a decade ago. These innovations aren't just flashy additions – they're changing real patients' lives every day.
Take robotics-assisted rehabilitation, for instance. At advanced robotics suites, patients recovering from strokes or spinal injuries work with devices that guide their movements with incredible precision. These robots don't replace therapists – they improve what's possible by allowing for hundreds more repetitions than traditional therapy, with adjustable assistance that decreases as you get stronger. Many patients tell us the immediate feedback these machines provide gives them a motivational boost too.
Water has always been healing, but today's aquatic therapy takes this to new levels. Dedicated Aqua Therapy Pools create an environment where gravity seems to disappear. I've seen patients who can barely move on land walk confidently in water. The natural resistance builds strength while the buoyancy reduces joint stress – a perfect combination, especially for those managing arthritis or recovering from joint replacements.
Neuromuscular re-education might sound complicated, but it's actually about retraining your body to move correctly again. At Evolve Physical Therapy + Sports Rehabilitation, we incorporate biofeedback systems that show you in real-time how your muscles are firing. Imagine seeing on a screen exactly which muscles are working during an exercise – it's like having a window into your body! This approach is particularly valuable for patients with complex neurological conditions who need to rebuild those brain-to-muscle connections.
Pain management has seen remarkable innovations too. Scrambler therapy represents a breakthrough for many suffering from stubborn neuropathic pain. Rather than just masking pain with medications, this FDA-approved treatment actually "scrambles" the pain signals your nerves send to your brain. Several Brooklyn rehabilitation centers now offer this non-invasive option, providing relief for conditions that were previously difficult to treat, from diabetic neuropathy to post-surgical discomfort.
For those seeking substance use treatment, modern centers have reimagined what rehabilitation can feel like. Their treatment approaches take place in settings that feel more like wellness retreats than clinical facilities. This approach recognizes that healing happens best when dignity and comfort accompany evidence-based practices.
These innovations reflect Brooklyn's position at the forefront of rehabilitation science. When you choose a Brooklyn rehabilitation center, you're gaining access to treatments that might not be available elsewhere, delivered by professionals passionate about incorporating the latest advances into your recovery journey. At Evolve Physical Therapy + Sports Rehabilitation, we're proud to be part of this forward-thinking community, always seeking better ways to help our patients regain function and return to the activities they love.
For patients with neuromuscular conditions, we offer specialized treatments at our center. More info about Neuromuscular Physical Therapy Brooklyn is available on our dedicated page.
To learn more about evidence-based rehabilitation approaches, visit the American Physical Therapy Association's resource center for comprehensive information on the latest research and best practices in physical therapy and rehabilitation.
From Admission to Independence: The Patient Journey

Your journey begins with a comprehensive evaluation—think of this as creating your personal recovery roadmap. At Evolve Physical Therapy + Sports Rehabilitation, we take extra time with these initial assessments because we know they're the foundation of your success. During this evaluation, our therapists will examine your strength and movement abilities, assess any pain you're experiencing, review your medical history, and most importantly, listen to your personal goals. What activities do you want to return to? What matters most in your daily life?
With this information in hand, we develop your personalized treatment plan. This isn't a one-size-fits-all approach—it's custom specifically to your needs, with clear, measurable goals and timeframes. Leading Brooklyn rehabilitation centers ensure patients receive at least 3 hours of therapy daily (that's 15 hours weekly) of individualized care. Your plan will outline exactly which therapies you'll receive, how often, and what we're working to achieve together.
Then comes the heart of your recovery—the active rehabilitation phase. This is where the real work happens through structured therapy sessions, whether that's physical therapy, occupational therapy, speech therapy, or a combination. During this phase, your therapy team meets regularly to discuss your progress and adjust your treatment as needed. We also begin training family members who might be helping with your care and providing emotional support for what can sometimes be a challenging journey.
As you progress, we shift focus to transition planning. This critical phase is all about preparing you for the next step, whether that's returning home or moving to a different level of care. We'll conduct home safety assessments, train your caregivers, practice community reintegration activities, help you get any equipment you might need, and set you up with outpatient services to continue your progress.
But your journey doesn't end when you leave our facility. The follow-up and continued recovery phase ensures you maintain your gains and continue improving. Most Brooklyn rehabilitation centers provide scheduled follow-up appointments, home exercise programs, connections to community resources, support groups, and even telehealth check-ins to monitor your progress remotely.
Throughout this entire journey, we pay special attention to cultural and linguistic needs—particularly important in Brooklyn's wonderfully diverse communities. Interpreter services and culturally competent care are standard at quality rehabilitation centers across the borough.
Coordinating Care Across Settings
One of Brooklyn's rehabilitation strengths is the seamless coordination between different care settings. This coordination looks like:
Hospital to rehabilitation transitions that happen smoothly, with minimal paperwork and stress for you and your family. Many hospital-affiliated rehabilitation units maintain direct connections with acute care hospitals, allowing for seamless transfers when you're ready.
Inpatient to outpatient continuity where you often work with the same clinical team throughout your journey, maintaining relationships with the therapists who know your case best.
Rehabilitation to home support including thorough home safety evaluations and hands-on training for anyone who'll be helping with your care at home.
Community integration assistance connecting you with local resources, support groups, and adaptive recreation programs that help you continue your recovery while resuming normal life activities.
At Evolve Physical Therapy + Sports Rehabilitation, we prioritize communication with your entire healthcare team. We work closely with your referring physicians, surgeons, and other specialists, sharing progress notes and treatment plans through our secure electronic medical record system. This team approach ensures everyone involved in your care is on the same page, working toward your best possible outcome.

For patients recovering from surgery, our specialized approach ensures you regain function quickly and safely. Learn more about our Physical Therapy for Surgery & Post-Op Rehab program designed specifically for surgical recovery.
Frequently Asked Questions about Brooklyn Rehab
What conditions qualify me for inpatient vs. outpatient rehab?
When you're facing rehabilitation needs, understanding whether you need inpatient or outpatient care is often the first big question. The difference really comes down to the intensity of care you require.
Inpatient rehabilitation makes sense when you need round-the-clock medical attention. If you've experienced a significant stroke, spinal cord injury, or traumatic brain injury, this level of care provides the intensive therapy (typically three or more hours daily) that can jumpstart your recovery. It's also appropriate after complex orthopedic surgeries, multiple trauma situations, or severe burns when you simply aren't safe to return home yet.
On the flip side, outpatient rehabilitation works well when you can safely live at home but still need specialized therapy. Many of our patients at Evolve Physical Therapy + Sports Rehabilitation come to us as they're transitioning from inpatient care or when their conditions don't require 24-hour supervision. The key is having reliable transportation to attend your scheduled sessions.
Think of it as a continuum – inpatient care provides the foundation for recovery when you're at your most vulnerable, while outpatient therapy helps you build on that foundation as you regain independence.
How long does recovery take at a Brooklyn rehabilitation center?
I wish I could give you a simple answer about recovery timelines, but the truth is that healing follows its own schedule for each person. Your recovery journey at a Brooklyn rehabilitation center depends on several factors that make your situation unique.
The nature and severity of your condition naturally plays the biggest role – recovering from a joint replacement differs dramatically from rehabilitating after a major stroke. Your age, overall health, and whether you have other medical conditions also influence your timeline. Even factors like your home support system and how consistently you follow your therapy program make a significant difference.
For those in inpatient settings, typical stays range from 1-3 weeks for straightforward recoveries like joint replacements, to 2-4 weeks for comprehensive rehabilitation after events like strokes, and 4-8 weeks or longer for complex conditions like spinal cord injuries.
For our outpatient patients at Evolve Physical Therapy + Sports Rehabilitation, we generally see treatment spanning 4-6 weeks for uncomplicated conditions, 8-12 weeks for moderately complex situations, and sometimes 3-6 months for neurological conditions requiring extensive rehabilitation.
What's most important is that we establish clear milestones during your initial evaluation and regularly reassess your progress, adjusting both treatment and expectations as you move forward.
Which insurance plans are commonly accepted?
Navigating insurance coverage shouldn't add stress to your recovery journey. Most Brooklyn rehabilitation centers work with a broad spectrum of insurance providers to make quality care accessible.
The major insurance plans typically accepted throughout Brooklyn include Medicare Parts A and B, Medicaid, Blue Cross Blue Shield, UnitedHealthcare, Aetna, Cigna, and the Empire Plan. If your injury resulted from a workplace incident or auto accident, Workers' Compensation and no-fault insurance are generally covered as well.
At Evolve Physical Therapy + Sports Rehabilitation, we understand that insurance verification can feel overwhelming when you're already dealing with health challenges. That's why we verify your benefits before your first appointment and provide a clear explanation of any potential out-of-pocket costs you might face.
For those with limited or no insurance coverage, many Brooklyn rehabilitation centers offer alternatives like sliding scale fees based on income, manageable payment plans, financial assistance programs, or straightforward self-pay options. The goal is always to ensure that financial concerns don't prevent you from receiving the care you need to recover fully.
It's always best to contact your chosen facility directly for the most up-to-date information about accepted insurance plans, as coverage options can change.
Conclusion
Brooklyn's rehabilitation landscape truly shines as a guide of hope for those on their recovery journey. From cutting-edge physical therapy techniques to comprehensive addiction treatment programs, the borough offers an impressive array of healing options. What makes Brooklyn rehabilitation centers truly special isn't just their clinical excellence—it's how they weave cultural competence into care, creating environments that heal the whole person, not just the injury or condition.
Here at Evolve Physical Therapy + Sports Rehabilitation, we take immense pride in being part of Brooklyn's vibrant rehabilitation community. Our approach to physical therapy isn't about following a cookie-cutter protocol—it's about putting our hands on you, understanding your unique needs, and creating a personalized path forward. We've developed specialized programs like our Rock Steady Boxing for Parkinson's patients (which caught the attention of NBC News) because we believe in meeting specific needs with targeted solutions.
Recovery isn't always a straight line forward—sometimes it zigzags, sometimes it plateaus. Whether you're bouncing back from surgery, managing a chronic condition that flares and fades, or working to reach your peak physical performance, Brooklyn offers rehabilitation options as diverse as its neighborhoods. The secret to success lies in finding your perfect match—a Brooklyn rehabilitation center where the expertise, philosophy, and environment feel right for you.
Throughout your rehabilitation journey, healing takes time, patience, and the right team in your corner. Brooklyn's rehabilitation professionals aren't just clinicians—we're neighbors, community members, and advocates committed to walking alongside you every step of the way. Our goal isn't just to help you recover; it's to help you thrive beyond what you thought possible.
Ready to take the next step in your healing journey? For more information about our approach at Evolve Physical Therapy + Sports Rehabilitation, visit our website or reach out to one of our convenient locations throughout Brooklyn, including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin. Your comeback story starts here—and we'd be honored to be part of it.
From Benchwarmer to MVP – Understanding Sports Performance Coaching
The Transformative Power of Sports Performance Coaching

Sports performance coaching is a specialized approach to athletic development that combines physical training, mental conditioning, nutrition guidance, and recovery strategies to help athletes reach their peak potential. Unlike traditional coaching that often focuses primarily on sport-specific skills, sports performance coaching takes a holistic view of the athlete as a complete system.
What is Sports Performance Coaching?
- A multi-disciplinary approach focusing on total athlete development
- Combines physical training with mental skills, nutrition, and recovery
- Uses evidence-based methods and technologies to track progress
- Tailors programs to specific sports and individual athlete needs
- Delivered by professionals with specialized education and certifications
Sports performance coaching has evolved significantly over the past decades, moving from generalized strength and conditioning to sophisticated, science-backed programming that addresses every aspect of athletic development. What was once reserved for elite professional athletes is now accessible across all levels of competition, from youth sports to weekend warriors looking to improve their game.
The International Coaching Federation reports that coaching has seen tremendous growth, with the number of coaches worldwide increasing by 33% between 2015 and 2022. This surge reflects the growing recognition of coaching's value in helping athletes break through plateaus and achieve consistent performance improvements.
At its core, effective sports performance coaching is about building a bridge between where an athlete currently stands and where they want to be. It's not just about getting stronger or faster—it's about developing a complete athletic foundation that supports long-term success and prevents career-derailing injuries.
My name is Lou Ezrick, and as a physical therapist specializing in sports rehabilitation, I've incorporated sports performance coaching principles into my practice to help athletes not just recover from injuries but return to competition stronger than before. My experience with rehabilitation techniques and movement optimization provides a unique perspective on how proper coaching can transform an athlete's career trajectory.

What Is Sports Performance Coaching?
Sports performance coaching is so much more than traditional training—it's a complete approach to athlete development that considers the whole person, not just their physical abilities. Think of it as the difference between having a single tool and owning an entire workshop. This comprehensive method addresses everything that impacts how you perform, from strength and conditioning to mental toughness, nutrition, and recovery.
Here at Evolve Physical Therapy + Sports Rehabilitation, we see sports performance coaching as both an art and a science. It's about understanding the unique potential in each athlete and creating pathways to excellence that are backed by evidence and custom to individual needs.
The field has come a long way from the days of simple workout routines. Today's performance coaching integrates cutting-edge sports science, psychological techniques, nutritional wisdom, and technology to create programs that truly transform athletic capability.
A modern sports performance coach rarely works alone. Instead, they often coordinate a team of specialists that might include:
- Strength and conditioning experts who build power and endurance
- Technical coaches who refine sport-specific skills
- Mental skills coaches who strengthen psychological resilience
- Nutritionists who optimize fueling strategies
- Physical therapists who prevent injuries and improve recovery
- Movement specialists who improve efficiency and technique
| Sports Performance Coach | Traditional Personal Trainer |
|---|---|
| Focuses on sport-specific performance outcomes | Primarily targets general fitness and aesthetics |
| Uses periodized training with strategic peaking | Often employs consistent weekly programming |
| Incorporates mental skills training | Typically focuses only on physical training |
| Designs programs based on competitive calendar | Programs often not aligned with competition cycles |
| Uses performance metrics and testing | Relies more on general fitness assessments |
| Integrates nutrition for performance timing | May offer basic nutrition advice for health |
| Implements advanced recovery protocols | Basic recovery recommendations |
| Often requires specialized certifications | More general fitness certifications |
Sports Performance Coaching vs Traditional Coaching
The coach who helps you perfect your tennis serve and the coach who transforms your entire athletic capacity have different approaches and goals. While traditional coaching centers on skills and game strategy, sports performance coaching takes a wider view of what makes an athlete successful.
Traditional coaching often relies on "we've always done it this way" thinking, but performance coaching is grounded in science. Rather than maintaining the same practice intensity year-round, performance coaches carefully structure training cycles to help you peak at exactly the right time for competition.
One size never fits all in performance coaching. Your program should be as unique as your fingerprint, designed around your specific needs rather than applying team-wide approaches that might work for some but not others.
"The integration of sport science principles into coaching practice represents one of the most significant advances in athletic development over the past several decades," explains Dr. Timothy Suchomel, a leading expert in the field.
Perhaps most importantly, performance coaches understand that rest isn't laziness—it's an essential part of getting stronger. Strategic recovery periods are built into programs because they recognize that improvement happens during adaptation, not just during training.
Sports Performance Coaching Across Athlete Levels
The beauty of sports performance coaching is its scalability. The core principles remain the same whether you're working with a promising 10-year-old or an Olympic medalist, but the application changes dramatically.
For young athletes between 8-14 years old, coaching focuses on building a foundation. We emphasize fun movement experiences that develop coordination and body awareness. Basic strength training with perfect technique comes before any specialized sport training. Most importantly, we nurture a positive relationship with physical activity and help build mental skills like focus that will serve them throughout life.
As athletes reach high school age, we begin to introduce more sport-specific development. Structured strength and power training becomes more important, along with basic nutritional education to fuel growing bodies. This is also when we start implementing targeted injury prevention strategies and developing the mental toughness needed for competition.
College athletes benefit from highly individualized programs that reflect their sport's specific demands. Training becomes more sophisticated, with detailed attention to nutrition timing, advanced mental performance techniques, and recovery protocols that help manage the demands of collegiate athletics.
Professional athletes require precision in every aspect of their training. At this level, we might employ cutting-edge assessment technologies, micro-periodize training variables throughout the season, and develop comprehensive recovery systems that give them the competitive edge.
We're also proud to work with adaptive athletes, modifying our approaches to accommodate different abilities while maintaining the same commitment to excellence. This might include specialized equipment adaptations, classification-specific preparation, and mental resilience training for unique challenges.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we meet you exactly where you are in your athletic journey. Whether you're taking your first steps into organized sports or looking to break through to elite performance, our sports performance coaching approaches are designed to help you reach the next level—and enjoy the journey along the way.
The Four Pillars of Peak Performance

When I talk with athletes about what makes the difference between good and great performance, I always come back to the same foundation. Effective sports performance coaching isn't about a single magic workout or technique—it's about building a complete system that addresses every aspect of athletic development.
Think of it as a four-legged chair—remove any leg, and the whole thing becomes unstable. These four pillars work together to create something much more powerful than any one element alone could provide.

Pillar 1 – Strength, Speed & Conditioning
The physical foundation of athletic performance isn't just about getting stronger or faster—it's about building the right qualities for your specific sport in the right sequence.
Before we design any training program at Evolve, we start with a thorough movement assessment. This helps us understand how you move, where imbalances might exist, and what limitations might be holding you back. It's like getting a detailed map before starting a journey—you need to know your starting point before plotting the best route forward.
We then create periodized programming that strategically builds your capabilities over time. Unlike cookie-cutter workout plans, true sports performance coaching recognizes that timing is everything. We'll design preparatory phases to build your base, strength blocks to increase your force production, and power phases timed perfectly to peak for your most important competitions.
For most athletes, plyometric training becomes a crucial component of their development. These explosive exercises bridge the gap between raw strength and sport-specific power. We carefully progress from basic jumps to complex reactive drills, always with an eye toward proper landing mechanics to keep you injury-free.
Modern technology has revolutionized how we train athletes. Through velocity-based training, we can measure exactly how fast you're moving weights or performing movements, allowing us to fine-tune the perfect resistance for your goals that day. Some days you'll be fresh and can push harder; other days we'll adjust to keep quality high while managing fatigue.
Sport isn't just about straight-line speed—it's about change of direction, reaction time, and sport-specific movement patterns. Our agility development protocols train not just your body but the crucial connection between your brain and muscles, helping you make faster decisions under pressure.
Pillar 2 – Mindset & Sports Psychology
I've worked with countless athletes who had all the physical tools but couldn't perform when it mattered most. That's why mental training isn't optional in comprehensive sports performance coaching—it's essential.
We help athletes build confidence through evidence-based strategies that create genuine self-belief—not just empty pep talks. This includes tracking performance accomplishments, developing pre-competition routines that trigger confident states, and learning to reframe setbacks as valuable learning opportunities.
The ability to maintain focus under pressure separates champions from contenders. We teach specific attention control techniques that help you stay present when distractions mount, whether it's a hostile crowd, high stakes, or your own thoughts trying to pull you off task.
Visualization and mental rehearsal have been used by Olympic athletes for decades, and for good reason—they work. We'll guide you through multi-sensory imagery practices that prepare your brain and body for successful performance, helping you see and feel success before you step onto the field or court.
The conversation you have with yourself during training and competition can either lift or undermine your performance. We'll help you reshape negative self-talk patterns into constructive internal dialogue that supports your goals rather than sabotages them.
These mental skills aren't just for struggling athletes—they're essential tools for anyone looking to perform at their best consistently. Resources like mental training audio programs from Peak Sports can help reinforce these skills between our coaching sessions.
Pillar 3 – Smart Fueling & Hydration
You wouldn't put regular gas in a Formula 1 car and expect peak performance. Similarly, your body needs the right fuel at the right time to perform at its best.
Macronutrient periodization is a fancy way of saying we adjust your food intake based on your training demands. Heavy training days might require more carbohydrates, while recovery days might shift toward more protein and healthy fats. We help you understand not just what to eat, but when to eat it for optimal results.
Performance timing is critical—what you eat before, during, and after training dramatically affects how you feel and recover. We'll create practical strategies that fit your schedule and preferences, from pre-workout meals that provide steady energy to post-workout nutrition that jumpstarts recovery.
Different sports have vastly different nutritional needs. A marathon runner needs different fueling strategies than a football lineman or gymnast. We tailor recommendations to your specific sport's demands, competition schedule, and body composition goals.
The supplement industry is full of bold claims and questionable products. Our approach to supplement safety and efficacy cuts through the marketing hype to focus on evidence-based options that have been third-party tested for purity and effectiveness. We'll help you prioritize what might actually benefit you and avoid wasting money on unnecessary products.
Proper hydration is about more than just drinking water—it's about maintaining the right fluid and electrolyte balance for your body size, sweat rate, and environment. We'll help you develop personalized hydration strategies that prevent both dehydration and the equally problematic overhydration.
Pillar 4 – Recovery & Resilience
The fourth pillar might be the most overlooked aspect of athletic development, yet it's often where the biggest performance gains hide. Recovery isn't just rest—it's an active process that requires as much attention as your workouts.
Sleep optimization forms the foundation of all recovery. We help athletes understand how to improve both sleep quantity and quality through better sleep hygiene, timing strategies, and environment optimization. For athletes who travel frequently, we develop specific protocols to minimize jet lag and sleep disruption.
Balancing training stress with recovery is a delicate art. Our training load management approach monitors your volume, intensity, and readiness markers to ensure you're pushing hard enough to improve but not so hard that you risk overtraining. Strategic deload weeks become planned parts of your program, not just responses to fatigue.
Your body's tissues need direct attention to recover optimally. We teach soft-tissue therapy techniques including self-myofascial release (foam rolling), compression therapy, and when appropriate, connect you with our Physical Therapy for Athletes services to address specific needs.
Prevention is always better than rehabilitation. Our regular injury prevention screening helps catch small movement compensations before they become injuries. This proactive approach includes Prehabilitation for Sports-Related Injuries to strengthen vulnerable areas before problems develop.
The mental aspect of recovery is just as important as the physical. Mental recovery techniques help athletes decompress from competitive pressure, manage stress, and maintain a healthy balance between sport and life. Simple mindfulness practices can make a profound difference in both performance and enjoyment of your sport.
At Evolve Physical Therapy + Sports Rehabilitation, our background in physical therapy gives us a unique perspective on recovery. We've seen how proper recovery not only prevents career-derailing injuries but also extends athletic careers and improves performance quality. It's not just about bouncing back—it's about bouncing forward stronger than before.
Pathways & Credentials for Sports Performance Coaches

Becoming a qualified sports performance coach isn't something that happens overnight. It's a journey that combines education, hands-on experience, and a genuine passion for helping athletes reach their potential. Think of it as training for a marathon rather than a sprint!
Must-Have Qualifications & Knowledge
The foundation of any great sports performance coach starts with education. Most successful coaches have at least a bachelor's degree in exercise science, kinesiology, or a related field. This gives them the scientific understanding of how the body works and responds to training.
But book smarts are just the beginning. A truly effective coach needs to understand the mechanics of movement—how the body should move and what it looks like when something's off. They need to know how different training methods affect the body, both immediately and over time.
Communication skills are absolutely crucial too. The most knowledgeable coach in the world won't get results if they can't connect with their athletes. At Evolve, we've seen how the ability to explain complex concepts in simple terms makes all the difference in helping athletes understand and buy into their training programs.
Good coaches also need a basic understanding of sports nutrition and psychology. They don't need to be experts in these fields (that's what specialists are for!), but they should understand how these elements affect performance.
The job outlook for this field is promising too. The U.S. Bureau of Labor Statistics projects 10% growth for coaching positions through 2031—faster than the average for all careers. This reflects the growing recognition of how specialized coaching can transform athletic performance.
Top Certifications Recognized Worldwide
In sports performance coaching, certain certifications have emerged as gold standards that signal a coach's expertise and commitment.
The NSCA Certified Strength and Conditioning Specialist (CSCS) certification is widely considered the industry benchmark. It's comprehensive, covering everything from program design to exercise technique, and requires a bachelor's degree just to sit for the exam. When you see a coach with CSCS after their name, you know they've demonstrated a serious level of knowledge.
For coaches focused on practical application, the NSPA Certified Sports Performance Coach (CSPC) certification provides excellent training in real-world coaching scenarios. It covers injury recognition, programming, nutrition, and conditioning with an emphasis on how these elements work together in actual training environments.
The NASM Performance Improvement Specialist (PES) is particularly strong in its approach to movement quality and corrective exercise. Many coaches who start as personal trainers use this certification as a bridge into performance coaching.
The mental side of performance shouldn't be overlooked, which is why certifications like the Mental Game Coaching Professional (MGCP) are valuable. This specialization helps coaches address the psychological aspects of performance—building confidence, improving focus, and developing a competitive mindset.
For coaches looking to improve their ability to motivate and break through psychological barriers, the iPEC Energy Leadership Coaching certification provides unique tools and approaches. This is particularly valuable when working with elite athletes who may be dealing with high-pressure situations.
Many serious sports performance coaches collect multiple certifications over time, building a diverse toolkit they can draw from to help different types of athletes. The best coaches never stop learning!
Career Opportunities & Earning Potential
One of the exciting things about pursuing sports performance coaching is the variety of career paths available. You're not locked into a single track.
In the private sector, coaches can work in dedicated performance training facilities, corporate wellness programs, or even launch their own training businesses. Online coaching has exploded in recent years too, allowing coaches to work with athletes around the world.
Educational settings offer stable opportunities—from high school strength programs to collegiate strength and conditioning departments. Some coaches even move into research positions at universities or develop coach education programs to train the next generation.
For those drawn to elite sports, professional teams hire performance coaches at various levels. You might start as an assistant strength coach and work your way up to head performance coach or specialize in areas like sports science coordination or recovery.
There's also growing demand in what's called "tactical strength and conditioning"—preparing military personnel, law enforcement officers, firefighters, and other tactical professionals for the physical demands of their jobs.
The financial rewards can be substantial. According to Lumia's coaching survey, coaching salaries range from $62,500 to $245,000 annually. The International Coaching Federation reports an average hourly rate of $244 for coaching sessions, though rates vary widely based on experience, location, and clientele.
At Evolve Physical Therapy + Sports Rehabilitation, we believe in continuous learning. We invest in our team's professional development to ensure we're always bringing the latest advances in sports performance coaching to our Brooklyn community. After all, when our knowledge grows, so do our athletes' possibilities!
From Assessment to MVP: Designing & Monitoring Athlete Programs
The journey from average athlete to MVP status doesn't happen by accident. At the heart of effective sports performance coaching lies a methodical process that transforms initial assessments into customized training programs with continuous monitoring and refinement.
Baseline Testing & Goal Mapping
Every great athletic journey begins with knowing your starting point. When you first step into our Brooklyn facility, we conduct a comprehensive assessment that paints a complete picture of where you stand today.
We begin with a thorough movement screening that examines how your body functions during fundamental patterns. This isn't just about identifying problems—it's about understanding your unique movement signature. We observe your mobility, stability, and movement quality, looking for those subtle compensation patterns that might limit performance or increase injury risk.
Performance testing adds objective data to this picture. Whether it's measuring your vertical jump on our force plates, timing your sprint acceleration, or establishing your strength benchmarks, these numbers provide concrete starting points against which we'll measure your progress.
But physical metrics tell only part of the story. Your mental approach to performance matters tremendously, which is why we assess your competitive mindset, how you respond under pressure, and your ability to maintain focus when it counts.
With this comprehensive baseline in hand, we collaborate with you to establish meaningful goals using the SMART framework—making sure they're Specific, Measurable, Achievable, Relevant, and Time-bound. We'll help you balance performance goals (like increasing your vertical jump) with outcome goals (like making the starting lineup), while emphasizing the process-focused targets that will get you there.
As Lou often tells our athletes, "Your baseline assessment isn't a judgment—it's your launchpad."
Program Design & Progression
With your assessment complete, the real artistry of sports performance coaching begins. We design your program by first analyzing the specific demands of your sport—understanding the energy systems you need, the movement patterns you perform, and the common injury mechanisms you face.
Your training calendar isn't random; it's periodized with purpose. We structure your year into macrocycles that align with your competitive season, break these down into 4-6 week mesocycles focused on specific adaptations, and then plan each week (microcycle) to balance intensity and recovery. Even individual sessions are sequenced to maximize performance and safety.
Progressive overload—the principle that you must continually challenge your body to improve—is carefully implemented through strategic adjustments to volume, intensity, exercise complexity, and technical demands. We don't just make things harder; we make them smarter.
Perhaps most importantly, we build strategic deload periods into your program. These reduced-load weeks aren't breaks from training—they're essential components that allow adaptations to take hold. As one college athlete working with us remarked, "I never understood why I kept hitting plateaus until Evolve taught me that sometimes doing less is actually doing more."
We also incorporate cross-training elements that complement your primary sport, prevent overuse injuries, and maintain mental freshness. This might include activities that develop transferable skills or simply provide a refreshing change of pace during the off-season.
At Evolve, we view program design as both science and art—blending research-backed principles with our deep understanding of you as an individual athlete.
Tracking, Feedback & Adjustments
The difference between good programs and great ones often comes down to monitoring and adjustment. Modern sports performance coaching leverages both sophisticated technology and good old-fashioned observation to ensure you're always on the optimal path.
After each session, we gather data on your Rate of Perceived Exertion (RPE), volume-load, movement quality, and subjective feedback. This immediate information helps us make micro-adjustments to keep you in the sweet spot between being challenged and being overwhelmed.
Technology amplifies our observational powers. Depending on your needs, we might employ GPS tracking to monitor distance and speed, heart rate monitoring for intensity, force plate assessment for power output, or velocity measurement for strength quality. Our video analysis helps refine your technique with frame-by-frame precision.
But performance isn't just about what happens in training. We track wellness factors like sleep quality, fatigue levels, stress, muscle soreness, and overall mood. These indicators often provide early warning signs of overtraining or readiness for increased challenges.
Regular reassessment is built into your program. These scheduled check-ins measure your progress toward established goals and evaluate the effectiveness of your current program. Sometimes they reveal the need for Prehabilitation for Sports-Related Injuries to address emerging issues before they become problems.
The true power of this monitoring system is that it creates a continuous feedback loop. Your program isn't static—it evolves as you do. We make data-driven adjustments based on your individual responses, constantly targeting weaknesses while building on strengths.
One high school athlete working with us put it perfectly: "What I love about training at Evolve is that nothing is random. Every exercise, every set, every rep has a purpose—and that purpose keeps evolving as I improve."
This systematic approach—from thorough assessment through thoughtful design and continuous monitoring—is what transforms potential into performance, and athletes into MVPs.
Finding the Right Sports Performance Coach or Program

Let's face it – choosing the right sports performance coach can feel a bit like dating. You're looking for that perfect match who understands your goals, challenges you appropriately, and ultimately helps you become the best athlete you can be. With so many options out there (and not all created equal), how do you find your athletic soulmate?
Questions Athletes & Parents Should Ask
Think of your first meeting with a potential coach as an interview – because it absolutely is! You're potentially investing significant time, money, and trust in this relationship, so don't be shy about asking the tough questions.
When my athletes and their families come to Evolve for the first time, I actually encourage them to interview me. Credentials and experience matter tremendously in this field. Ask about specific certifications related to sports performance, their educational background, and how long they've been working specifically with athletes in your sport. A coach who gets defensive about these questions might not be the right fit.
The coach's programming philosophy reveals a lot about how they'll approach your development. A good coach should eagerly explain their assessment process, periodization approach, and how they balance sport-specific training with overall athletic development. At Evolve, we love these questions because they let us showcase our thoughtful, evidence-based approach to sports performance coaching.
Don't overlook the practical logistics and structure of the program. What's the coach-to-athlete ratio? (Hint: lower is usually better!) How will your program be individualized, even in group settings? What technologies do they use for monitoring progress? These details can make or break your experience.
Finally, any coach worth their salt should be able to provide examples of results and references. Ask about specific athletes who've improved under their guidance and how they measure success. A great coach tracks progress systematically and can show you the evidence.
Common Challenges a Coach Can Solve
One of the most rewarding aspects of being a sports performance coach is helping athletes overcome obstacles they couldn't tackle alone.
Performance plateaus happen to every athlete – even the pros. A skilled coach identifies what's holding you back, whether it's a movement inefficiency, insufficient recovery, or simply that your body has adapted to your current training stimulus. We've helped countless Brooklyn athletes break through these plateaus by implementing novel training approaches custom to their unique needs.
Injury prevention and return-to-play represent another crucial area where coaching makes all the difference. Through proper movement screening, balanced strength development, and progressive loading strategies, we help athletes stay healthy and performing at their best. And if an injury does occur, our Sports Rehab Physical Therapy Brooklyn services provide a seamless transition back to peak performance.
The mental side of performance often goes underappreciated until it becomes a problem. Mental performance barriers like competition anxiety, focus issues, or confidence problems can derail even the most physically gifted athletes. A comprehensive coaching approach addresses these psychological aspects alongside physical training, helping you develop the complete mental toolkit needed for clutch performances.
Training consistency challenges plague athletes at all levels. Life gets busy, motivation fluctuates, and suddenly you've missed several workouts. A good coach creates accountability systems and helps you develop the habits that lead to long-term success. We've found that tracking progress in concrete ways provides powerful motivation when the initial excitement wanes.
Finding sport-life balance might be the most universal challenge athletes face. Between school, work, family, and social commitments, training can sometimes take a backseat. Your coach should help you steer these competing priorities with time management strategies and energy allocation guidance that keeps you progressing without burning out.
At Evolve Physical Therapy + Sports Rehabilitation, we see these challenges as opportunities to demonstrate the value of our holistic approach. By addressing the whole athlete – not just their physical performance – we help create sustainable success both in sport and in life. Our Brooklyn location has become a hub where athletes find not just improved performance, but a supportive community that helps them steer their entire athletic journey.
Conclusion
The journey from aspiring athlete to MVP isn't just about natural talent—it's about strategic development and comprehensive support. Sports performance coaching has revolutionized how athletes at every level approach their development, offering a roadmap that addresses all aspects of athletic excellence.
Throughout this guide, we've explored how the integration of physical conditioning, mental resilience, nutritional strategies, and recovery protocols creates a foundation for breakthrough performances. This holistic approach doesn't just produce temporary gains; it builds sustainable excellence that can withstand the pressures of competition and the test of time.
What makes sports performance coaching so powerful is its adaptability. Whether you're a high school athlete hoping to earn a college scholarship, a weekend warrior looking to improve your recreational league performance, or a professional seeking that championship-winning edge, the principles remain the same—only the application changes to match your specific needs and goals.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen how this approach transforms athletes throughout Brooklyn's diverse neighborhoods. From the dedicated young gymnast in Park Slope to the veteran marathon runner in Marine Park, the basketball player in Gravesend to the tennis competitor in Midwood—each has finded new potential through structured, science-backed coaching.
Our unique perspective as physical therapists allows us to bridge the gap between rehabilitation and performance improvement. We don't just help athletes recover from injuries; we help them rebuild stronger and more resilient than before. This preventative mindset is at the heart of effective sports performance coaching—addressing weaknesses before they become limitations and building strengths that translate directly to competitive advantages.
If you're feeling stuck on the bench when you know you have more to offer, or if you're already performing well but sense there's another level you could reach, the right coaching approach might be the missing piece. Every championship performance is built on a foundation of deliberate practice, expert guidance, and personalized programming.
We invite you to learn more about our Physical Therapy for Athletes and explore how our team at Sports Rehab Physical Therapy Brooklyn can support your athletic journey. Our hands-on approach combines evidence-based methods with genuine care for your long-term success.
Every MVP was once a beginner, and every athletic breakthrough begins with a decision to seek excellence. With the right sports performance coaching, your potential isn't just waiting to be finded—it's waiting to be releaseed.
Finding Strength Together – Top Online Parkinson's Support Groups
Finding Connection Through Shared Experience

Online support groups for Parkinson's disease are virtual communities where people affected by PD can connect, share experiences, and find emotional support. Here are the top options available today:
| Support Group | Members | Focus | Platform |
|---|---|---|---|
| Parkinson's Buddy Network | 9,000+ | Peer mentoring | Web forum |
| Cure Parkinson's Community | 21,000+ | Research updates | HealthOpen uped |
| PatientsLikeMe | 20,000+ | Symptom tracking | Web forum |
| PD Conversations | Varies | Moderated discussions | Foundation website |
| YOPD Connections | Varies | Young onset | Video meetings |
When you or someone you love receives a Parkinson's diagnosis, the journey ahead can feel overwhelming. The progressive nature of the disease brings unique challenges that change over time, affecting not just physical movement but emotional wellbeing and daily routines. While medical care is essential, there's another powerful resource that many find invaluable: connecting with others who truly understand.
Online support groups for Parkinson's disease offer something that even the best healthcare providers sometimes can't—firsthand experience and emotional understanding from peers facing similar challenges. These virtual communities break down geographic barriers, providing 24/7 access to support, information sharing, and a sense of belonging that can significantly improve quality of life.
"Many people find support groups help them deal with the challenges of having Parkinson's disease or being a care partner," notes the Parkinson's Foundation, highlighting how these connections can make a profound difference in navigating the PD journey.
Whether you're newly diagnosed, a long-time patient, or a care partner, online communities offer specialized spaces where you can ask questions, share victories, vent frustrations, and learn practical coping strategies—all from the comfort and convenience of your home.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've witnessed how online support groups for Parkinson's disease complement physical rehabilitation by providing the emotional support and practical wisdom that comes only from shared experience.

Why Online Support Groups for Parkinson's Disease Are Game-Changers
Living with Parkinson's disease comes with a unique set of challenges that evolve over time. While medical treatment forms the cornerstone of care, there's something incredibly powerful about connecting with others who truly understand what you're going through. This is where online support groups for Parkinson's disease have become absolute game-changers in the PD community.

These virtual communities offer a lifeline of support that works in ways traditional care sometimes can't. Always-available access means you can reach out at 3 AM when worry keeps you awake, or in the middle of a particularly challenging day when symptoms flare up. No need to wait until next Tuesday's meeting – help is there when you need it most.
The beauty of geographic freedom cannot be overstated. I've seen patients who live in remote areas light up when finding these online communities. Suddenly, the isolation that came with their diagnosis melts away as they connect with others from across the globe. Physical limitations or transportation problems no longer stand in the way of meaningful support.
Many members value the option for privacy that online groups provide. "I wasn't ready to share my diagnosis with my community," one participant told me, "but I desperately needed to talk to someone who understood. Being able to join anonymously gave me space to process my feelings at my own pace."
The global perspective these groups offer brings unexpected benefits too. Members frequently share approaches to managing symptoms that might not be common knowledge in your local area. From innovative gadgets available in other countries to cultural perspectives on living well with PD, the worldwide community becomes a treasure trove of ideas.
For care partners who can't easily leave their loved ones, online support provides crucial connections without the logistical nightmare of arranging alternative care. As one caregiver shared, "These late-night forum conversations have been my sanity-saver when I can't possibly attend an in-person meeting."
The collective wisdom of thousands of members creates a remarkable knowledge base that even the best medical professionals can't match. While doctors provide essential medical guidance, fellow travelers on the PD journey offer practical, lived experience that proves invaluable.
Research published in the Journal of Parkinson's Disease confirms what we see in practice – people who engage with peer support report better quality of life, improved coping skills, and significantly less isolation. As scientific research on peer support benefits shows, these connections can make a meaningful difference in disease management.
"Before finding this group," one Parkinson's Buddy Network member confided, "I felt like I was the only one experiencing these symptoms. Now I have friends around the world who truly understand what I'm going through and offer practical advice that even my doctors hadn't thought of."
Online vs. In-Person Support – Key Differences
While both formats offer valuable benefits, understanding their differences helps you choose what works best for your situation:
| Feature | Online Support Groups | In-Person Support Groups |
|---|---|---|
| Accessibility | Available 24/7 from anywhere with internet | Limited to specific locations, dates, and times |
| Geographic Reach | Global community with diverse experiences | Limited to local participants |
| Communication Style | Text-based forums allow time to compose thoughts; video options available | Real-time verbal communication; nonverbal cues more apparent |
| Anonymity | Can participate with varying levels of identity disclosure | Face-to-face interaction with local community members |
| Technical Requirements | Requires internet access and basic computer skills | Requires transportation and physical mobility |
| Response Time | May wait hours or days for responses | Immediate feedback during scheduled meetings |
| Record of Discussions | Searchable archives of past conversations | Must rely on memory or personal notes |
| Group Size | Can accommodate thousands of members | Typically limited to 5-20 participants |
Many of our patients at Evolve find tremendous value in a hybrid approach – attending local in-person meetings when possible while maintaining connections in online communities for continuous support. The warmth of a face-to-face hug combined with the constant availability of digital friends creates a comprehensive support system that improves quality of life in meaningful ways.
Choosing the Right "Fit": Types of Online Support Groups for Parkinson's Disease
Finding your place in online support groups for Parkinson's disease is a bit like finding the perfect pair of shoes – comfort matters, and what works for someone else might not work for you. The beautiful thing is that today's digital landscape offers communities custom to virtually every need, stage, and life circumstance.

When I speak with patients about finding their ideal support community, I always suggest thinking about what matters most to you right now. Are you newly wrestling with a diagnosis? Perhaps you're navigating the unique challenges of young-onset PD while raising children. Maybe you're a veteran seeking others who understand both service-related issues and Parkinson's.
The right group feels like coming home – a place where people "get it" without lengthy explanations. As one support group member beautifully put it, "If a support group meets your specific needs, it's the right group for you." Don't be discouraged if the first community you try doesn't click – many people visit several before finding their perfect match.
When searching for your ideal community, consider what speaks to your situation: disease stage (newly diagnosed vs. advanced), age group (young onset or traditional), your role (patient or care partner), special demographics (veterans, women, solo-livers), language preferences, treatment focus (like DBS experience), and even format preference (text forums or video calls). Some people prefer professionally moderated groups, while others thrive in peer-led environments.
Finding Groups by Need or Niche
The Parkinson's journey looks different for everyone, which is why specialized communities have emerged to address unique challenges:
Those newly diagnosed often seek spaces focused on adjustment, early symptom management, and processing the emotional impact. Meanwhile, young onset (YOPD) communities tackle career concerns, parenting with PD, and long-term planning with decades ahead.
Veterans benefit from groups that steer the complexities of VA benefits and service-connected PD issues, while care partners share invaluable caregiving strategies and much-needed self-care techniques.
Many women find comfort in women-only spaces where they can freely discuss gender-specific symptoms and concerns. Those living solo with Parkinson's connect to exchange independence strategies and build support networks. And the growing DBS community shares experiences before and after Deep Brain Stimulation surgery.
Finding these specialized havens is easier than you might think. Start with the PMD Alliance's state-by-state directory, contact the Parkinson's Foundation Helpline (1-800-4PD-INFO) for personalized recommendations, ask your neurologist about groups they trust, or explore Facebook's numerous PD-focused communities with specific themes.
"Online Support Groups for Parkinson's Disease" by Stage
As Parkinson's progresses, your support needs naturally evolve, and different communities rise to meet these changing challenges:
In newly diagnosed groups, the focus often centers on education, processing emotional reactions, understanding medication options, and learning about lifestyle modifications that can make a difference. These communities balance future planning with maintaining hope and optimism.
Mid-stage groups typically address adapting to changing symptoms, managing increasingly complex medication schedules, maintaining independence in relationships, and balancing work with health needs. Many discussions explore advanced treatment options as symptoms evolve.
Those in advanced stage groups find support navigating increased care needs, addressing complex medication regimens, managing challenging non-motor symptoms, and supporting care partners with growing responsibilities. These communities emphasize maintaining quality of life and dignity through difficult transitions.
Living solo groups create space for discussing safety plans for independent living, building reliable support networks, adapting homes for accessibility, managing medications independently, and thoughtfully planning for future care needs.
These categories aren't rigid boundaries – many people benefit tremendously from participating in multiple communities as their needs change and evolve. The digital nature of online support groups for Parkinson's disease makes it possible to find your people, no matter where you are in your journey.
Top 10 Online Support Groups for Parkinson's Disease (2024 Edition)
Based on member feedback, active participation levels, and quality of information shared, here are the top online support groups for Parkinson's disease currently available:
1. Parkinson's Buddy Network
When it comes to finding your tribe online, the Parkinson's Buddy Network stands out as a true global community. With over 9,000 members spanning 84+ countries as of late 2023, this vibrant network has created a digital home where distance disappears and understanding flourishes.
What makes this community special isn't just its size—it's the thoughtful design behind the connections. Their innovative peer mentoring program pairs newcomers with experienced members who've "been there," offering that invaluable combination of empathy and practical wisdom that only comes from lived experience.
"Finding my buddy through the network was like finally having someone who could finish my sentences," shares one member. "They understood exactly what I meant when describing symptoms I couldn't even name yet."
Key Features:
- A sophisticated matching algorithm that connects you with members facing similar symptoms or challenges—whether that's tremor management, sleep issues, or navigating work with PD
- Carefully moderated forums ensuring information accuracy and maintaining a supportive atmosphere where all questions are welcomed
- Round-the-clock availability for those middle-of-the-night worries or breakthrough moments you want to share
- Thoughtfully organized topic threads making it easy to find discussions relevant to your specific concerns
The platform's global reach means you'll gain perspectives on treatments and approaches that might not be common knowledge in your local area. Members regularly share insights about everything from international research developments to cultural approaches to living well with Parkinson's.
Best For: Anyone seeking a large, active community with diverse global perspectives and structured mentorship opportunities. This is particularly valuable for those who appreciate having conversations organized by specific topics and want to connect with others who share their particular symptoms or challenges.
Whether you're newly diagnosed or years into your journey with Parkinson's, the Buddy Network offers that perfect blend of wisdom, warmth, and worldwide connection that makes online support groups for Parkinson's disease such powerful tools for living well.
2. PD Conversations (Parkinson's Foundation)
When you're looking for reliable information backed by true experts, PD Conversations stands out as a guide of trustworthy support. This vibrant community is carefully overseen by trained staff from the Parkinson's Foundation Helpline, ensuring conversations remain both supportive and factually sound.
Key Features:
- Professional moderation that gently keeps discussions on track while allowing for genuine connection
- Fully bilingual platform available in both English and Español, making support accessible to more families
- Thoughtfully organized discussion threads that help you quickly find conversations about specific symptoms or concerns
- Regular participation from medical professionals who can weigh in on complex questions
- Strong commitment to evidence-based information that you can trust when making decisions
What makes PD Conversations special is the balance they strike between professional oversight and genuine peer support. You'll find a welcoming community where questions receive thoughtful, accurate responses, often within hours.
"The moderators make all the difference," shares Maria, a long-time member. "They know when to step in with corrections and when to let the community support each other. Plus, being able to participate in Spanish has been a game-changer for my mother who doesn't speak English."
The symptom-specific threads are particularly helpful when you're dealing with a new challenge. Whether it's tremor management, sleep issues, or medication adjustments, you can quickly connect with others who've walked the same path.
Best For: People who value carefully vetted information and prefer a structured, professionally guided conversation space. If you're newly diagnosed or feeling overwhelmed by conflicting information online, the trustworthy environment of PD Conversations provides a solid foundation for learning and connection.
3. Cure Parkinson's / HealthOpen uped
Imagine stepping into a virtual room where more than 21,000 people from around the world share your journey with Parkinson's disease. That's exactly what you'll find in the Cure Parkinson's community on the HealthOpen uped platform – a vibrant blend of emotional support and cutting-edge research information.
Key Features:
- The community regularly receives fresh research updates directly from the Cure Parkinson's organization, keeping members informed about promising developments in the field
- Members actively participate in community polls that gather valuable real-world experiences – your voice matters here
- Important resources and upcoming webinars are highlighted through pinned posts, so you never miss critical information
- There's a palpable sense of hope throughout discussions, with many conversations centered around research breakthroughs
- Finding what you need is simple thanks to well-organized topic categories that make navigation intuitive
What makes this community special is its dual focus on emotional support and scientific advancement. One member shared, "When I'm feeling discouraged, I come here not just for comfort but to remind myself that brilliant minds are working on solutions every day. It gives me hope."
The moderators do an excellent job balancing scientific accuracy with emotional sensitivity. They understand that behind every question about a new treatment is a person seeking not just information, but hope.
Best For: This community is particularly valuable for those who find comfort in staying informed about research progress. If you're someone who feels empowered by understanding the science behind treatments and potential breakthroughs, you'll feel right at home in this online support group for Parkinson's disease.
4. PatientsLikeMe – Parkinson's Community
There's something incredibly powerful about seeing your journey reflected in data and shared experiences. With over 20,000 members living with Parkinson's, the PatientsLikeMe community offers exactly that – a blend of heartfelt support with practical, data-driven insights that can help make sense of your PD experience.
Key Features:
- Innovative symptom tracking tools that help you spot patterns in your own health journey
- Treatment comparison features that let you see how others respond to medications you're considering
- Anonymous data sharing that contributes to research while protecting your privacy
- Detailed profile options that connect you with others facing similar challenges
- Quick-response Q&A format where questions rarely go unanswered for long
What makes this community special is how it transforms individual experiences into collective wisdom. As one member shared, "Being able to track my symptoms over time helped me have more productive conversations with my neurologist. Plus, seeing that others had similar side effects made me feel less alone."
The platform's clean, intuitive design makes it accessible even for those who aren't particularly tech-savvy. You can dive as deep into the data as you want, or simply connect with others for emotional support.
Best For: People who appreciate seeing patterns in their health data and want to make informed decisions based on real-world experiences. If you're the type who brings charts to your doctor appointments or likes comparing notes with others, you'll feel right at home in this online support group for Parkinson's disease.
5. Smart Patients PD Community
When you're looking for thoughtful, evidence-based discussions about Parkinson's, the Smart Patients PD Community offers a refreshing approach. This community, run in partnership with the American Parkinson Disease Association (APDA), creates a space where scientific accuracy matters just as much as emotional support.
What makes this group special is its commitment to quality over quantity. Unlike some of the larger forums where conversations can sometimes get lost in the shuffle, Smart Patients maintains a more intimate atmosphere where your questions won't disappear into a sea of posts.
Key Features:
- A private, application-required membership process that helps maintain a safe, focused environment
- Regular contributions from APDA experts who bring professional insights to discussions
- A comprehensive, searchable knowledge base built from years of valuable conversations
- A culture that values both emotional support and scientific accuracy
- A community that welcomes complex questions without judgment
I've heard from many patients that they appreciate how this group strikes a balance between being welcoming to newcomers while still offering depth for those who've been living with Parkinson's for years. As one member shared, "When I need to understand a new research paper or medication option, this is where I turn first. People here take the time to really think before responding."
The smaller size of this community can be a real advantage if you're looking for more meaningful connections rather than just quick answers. Many members develop ongoing relationships that provide consistent support through the ups and downs of the PD journey.
Best For: People who value quality information in a more intimate online setting, especially those who feel overwhelmed by larger forums or want to dive deeper into evidence-based discussions about their condition.
6. Parkinson's UK Forum
The Parkinson's UK Forum stands out as a vibrant online community that has become a digital home for thousands of people affected by Parkinson's throughout the United Kingdom and beyond. With its welcoming atmosphere and thoughtfully organized sections, it offers something for everyone on the PD journey.
Key Features:
- A dedicated "Just diagnosed" section creates a safe space for newcomers still processing their diagnosis and figuring out their next steps
- The unique "Creative corner" showcases artistic expressions from community members—from poetry to painting—highlighting how creativity thrives despite Parkinson's challenges
- Medication discussions are particularly valuable, with members sharing real-world experiences about effectiveness, side effects, and practical tips for managing complex medication regimens
- Regional UK support information connects members with local resources, while international visitors gain insights from the UK's robust healthcare approach to Parkinson's
- A notably supportive culture where both questions and answers are treated with respect and empathy
"Finding this forum was like finding a second family who truly understood what I was going through," shares one long-time member. "The medication discussions alone saved me months of trial and error."
While focused on UK healthcare systems and resources, the forum warmly welcomes international members who appreciate the British perspective on Parkinson's care and research. The conversations blend practical advice with emotional support, creating connections that many members describe as life-changing.
Best For: UK residents navigating the NHS system, anyone interested in UK-based research and support approaches, and those who appreciate a well-moderated, compassionate online community with clear guidelines and helpful organization.
The forum particularly shines in its balance between emotional support and practical information—making it an excellent complement to physical therapy and other medical interventions in a comprehensive online support groups for Parkinson's disease approach.
7. YOPD Connections (PMD Alliance)
If you're among the 10% of people diagnosed with Parkinson's before age 50, you face a unique set of challenges that differ from those of older-onset patients. YOPD Connections creates a space specifically for this community, where the conversations naturally center around juggling career demands, raising children, and navigating decades of life with PD ahead.
YOPD Connections hosts welcoming twice-monthly Zoom gatherings that feel more like catching up with friends than formal support meetings. The format balances structured discussions with casual conversation, often breaking into smaller virtual rooms where deeper connections can form. Many members describe these breakout sessions as the highlight of their meetings—a chance to laugh, vent, and problem-solve with others who truly understand.
"When I was diagnosed at 42, I felt completely alone until I found this group," shares one regular participant. "Now I have friends across the country who get exactly what it's like to manage a team meeting when your medications are wearing off, or how to explain your diagnosis to young children."
The discussions frequently address workplace accommodation strategies, parenting with Parkinson's, and long-term financial planning—topics that might receive less attention in general PD groups. Members exchange practical advice about disclosure decisions at work, managing energy through demanding careers, and maintaining an active role in children's activities despite symptoms.
For those who can't attend live sessions, recordings are available afterward, though many members note that the real-time interaction provides the greatest benefit. The group maintains an active private message board between meetings where members continue conversations and share resources.
Best For: People diagnosed with Parkinson's before age 50 who want age-appropriate support and practical strategies for managing PD during their working and family-raising years.
8. Flying Solo
For those navigating Parkinson's while living independently, the Flying Solo group offers a uniquely supportive community that understands the additional challenges of managing PD without a live-in care partner.
Key Features:
- Practical tips for independent living
- Emergency planning strategies
- Home modification ideas
- Building community support networks
- Regular resilience-building sessions
Living alone with Parkinson's brings distinct challenges that many general support groups don't fully address. The Flying Solo community fills this gap beautifully, creating a space where members share innovative solutions for everything from medication management to home safety.
"When my tremors made it hard to prepare meals, someone in the group suggested meal prep techniques I'd never considered," shares one member. "Now I cook once a week and have nutritious options ready when my symptoms flare."
The group regularly discusses practical matters like creating emergency response plans, installing smart home technology for safety, and building relationships with neighbors who can help during difficult times. Their monthly resilience sessions focus on emotional wellbeing and maintaining independence despite progressive symptoms.
What makes Flying Solo particularly valuable is how members transform isolation into connection. Many participants report that the strategies shared in this online support group for Parkinson's disease have allowed them to maintain their independence much longer than they initially thought possible.
Best For: People managing Parkinson's while living alone
9. Care Partner Monthly Meet-Up (Davis Phinney Foundation)
When you're caring for someone with Parkinson's, sometimes you need your own circle of support. The Care Partner Monthly Meet-Up hosted by the Davis Phinney Foundation creates exactly that safe space where caregivers can breathe, connect, and recharge.
Key Features:
- Stress relief workshops that offer practical techniques you can use during challenging moments
- Self-care strategies designed specifically for the unique demands of Parkinson's caregiving
- Expert guest speakers who understand the caregiver journey and provide valuable insights
- Flexible drop-in format that respects your busy and often unpredictable schedule
- Practical caregiving tips shared among peers who truly "get it"
- Emotional support in a judgment-free environment
"The first time I joined, I cried for ten minutes straight just feeling understood," shares Maria, a regular attendee who cares for her husband with Parkinson's. "Now I never miss a meeting—it's my monthly lifeline."
What makes this group special is its exclusive focus on the caregiver experience. While many online support groups for Parkinson's disease include caregivers, this dedicated space acknowledges that care partners have their own unique journey running parallel to their loved one's PD experience.
The monthly format strikes a perfect balance—frequent enough to build meaningful connections, but not so demanding that it becomes another obligation in an already full schedule. Many members report that these sessions help prevent burnout and provide practical solutions to everyday challenges.
Best For: Spouses, adult children, friends, and anyone else in a caregiving role for someone with Parkinson's disease.
10. Sunday Mornings with Twitchy Women
There's something special about the warmth and understanding that flows through this women-only community. Sunday Mornings with Twitchy Women creates a unique sanctuary where women with Parkinson's can share their experiences in an environment that truly gets the gender-specific journey of PD.
Key Features:
- Women-only safe space where participants can openly discuss intimate concerns without hesitation
- Monthly webinars with expert guests who address everything from hormonal impacts on symptoms to female-specific medication responses
- Focus on symptoms that affect women differently, acknowledging the research showing women often experience PD differently than men
- Wellness strategies with female perspectives that balance self-care with family responsibilities many women juggle
- Humor and positivity emphasized throughout every interaction, because sometimes laughter truly is the best medicine
"What I love about Twitchy Women is that I don't have to explain myself," shares Maria, a long-time member. "We all understand the unique challenges of being a woman with Parkinson's—from managing symptoms during hormonal changes to navigating relationships as our bodies change."
The group's founder, Sharon Krischer (known affectionately as "Twitchy Woman"), created this space after recognizing that women's voices were often underrepresented in online support groups for Parkinson's disease. Her warmth and authentic approach have cultivated a community where genuine friendships form alongside practical support.
Beyond the scheduled webinars, members exchange wellness hacks that work specifically for women's bodies and lifestyles. The conversations flow naturally from managing tremors while applying makeup to navigating intimacy with partners—topics that might feel uncomfortable in mixed-gender settings.
Best For: Women with Parkinson's seeking gender-specific support in a judgment-free environment where both tears and laughter are welcomed equally.
Getting the Most Out of Your Online Parkinson's Group
Joining an online support group for Parkinson's disease is just the first step on a journey of connection and growth. To truly benefit from these virtual communities, you'll want to engage in ways that feel meaningful and supportive for both yourself and others.

When I first joined a Parkinson's support group, I felt a bit like a wallflower at a dance – unsure of when to step in and how to move with the rhythm of the community. What I learned was that listening first gives you a feel for the group's culture before diving in. Spend a week or two simply observing conversations, noting the tone and topics that resonate most.
Setting personal goals for what you hope to gain makes a world of difference. Are you looking for emotional support during tough days? Practical tips for managing symptoms? The latest research updates? Or simply the comfort of knowing you're not alone? Being clear about your needs helps you engage in ways that serve you best.
I've noticed that members who participate regularly tend to build the strongest connections. Even a simple "I relate to that" comment can begin meaningful friendships that extend beyond the virtual walls of the group. When you're ready, sharing your journey – both the challenges and victories – creates a ripple effect of support that often comes back to you tenfold.
"The first time I shared about my freezing episodes, I was flooded with understanding responses and practical suggestions I'd never heard from my doctors," shares Maria, a long-time member of the Parkinson's Buddy Network. "Now I make sure to pass along what works for me to newcomers facing similar challenges."
When seeking advice, ask specific questions rather than general ones. "How do others manage morning stiffness?" will likely get more helpful responses than "Any advice for Parkinson's symptoms?" And always remember to respect boundaries – what works beautifully for one person may not work at all for another due to the uniquely personal nature of Parkinson's.
While peer wisdom is invaluable, it's crucial to verify medical information with your healthcare team before making changes to your treatment approach. Online support complements but doesn't replace professional care – a healthy balance keeps you both connected and safe.
Don't forget to express gratitude when others share insights that help you. A simple "thank you for sharing that" encourages continued openness within the community. And when discussions become overwhelming (which happens to all of us), it's perfectly fine to take breaks – step away, breathe, and return when you're ready.
For those in Brooklyn seeking to complement their online support with in-person connection, our Parkinson's Boxing Classes offer physical benefits while building face-to-face relationships with others who understand your journey.
Coping With Specific Challenges Together
The beauty of online support groups for Parkinson's disease lies in their ability to address specific challenges at every stage of the journey.
The shock of a new diagnosis often leaves people feeling adrift. In newly diagnosed groups, you'll find others who remember exactly how that feels and can share how they moved from initial fear to finding a path forward. They offer practical advice on explaining the diagnosis to loved ones and maintaining hope while adjusting to this new reality.
Medication management becomes less daunting when you can learn from others' experiences. Fellow group members often share brilliant timing strategies to maximize effectiveness, creative solutions for tracking complex regimens, and honest discussions about managing side effects. One group member created a simple medication diary template that's now been downloaded by thousands of others seeking better symptom control.
For those providing support to loved ones, discussions about caregiver burnout create a safe space to express difficult emotions without judgment. Experienced care partners share self-care strategies that actually work with limited time, resources for finding respite care, and validation that it's okay – necessary, even – to prioritize your own wellbeing.
When mobility challenges arise, the collective wisdom of the group shines. Members exchange home modification suggestions that preserve both safety and dignity, recommend adaptive equipment that's actually worth purchasing, and share exercise routines that help maintain independence longer. These practical solutions often come from years of trial and error – wisdom you won't find in medical textbooks.
Becoming a Super-Member or Moderator
As you become more comfortable in your online community, you might find yourself drawn to taking on a more active role. Many groups welcome volunteers who can help with welcoming newcomers, answering common questions, or starting thoughtful discussion threads. This deeper involvement often enriches your own experience while supporting others.
Effective moderation practices create spaces where everyone feels heard. Setting clear ground rules for respectful communication, using open-ended questions to encourage participation, and ensuring quieter voices have space to contribute all help build a thriving community. Good moderators find gentle ways to redirect conversations when they veer into unproductive territory.
Handling misinformation requires both tact and accuracy. Rather than shutting down conversations, skilled moderators guide discussions toward evidence-based resources while honoring personal experiences. Something as simple as "That's interesting – here's what recent research suggests about that approach" can keep conversations both supportive and accurate.
To avoid volunteer burnout, remember to set clear boundaries around your time and emotional energy. You're not responsible for solving everyone's problems or being available 24/7. Taking regular breaks helps maintain your enthusiasm and effectiveness in supporting others.
Even small contributions make a meaningful difference. Something as simple as sharing an article that helped you or posting an encouraging comment on someone's tough day creates ripples of support throughout the community.
Staying Safe & Informed Online
While online support groups for Parkinson's disease offer tremendous benefits, navigating them wisely helps ensure you're getting reliable information while protecting your privacy.

When I first started recommending online communities to my patients, I noticed how quickly they acceptd the support—but sometimes without the same caution they'd use in other online spaces. Even in these caring communities, it's important to protect yourself.
Before sharing personal details, take a moment to review the privacy settings on whatever platform you're using. Many people feel comfortable using their real names, while others prefer using a nickname or first name only—both approaches are perfectly fine. Just remember that most online forums aren't HIPAA-protected environments, so sharing should always be a conscious choice rather than an assumption of complete privacy.
The wealth of information in these groups is invaluable, but it requires a thoughtful approach. When someone shares advice about treatments or symptom management, consider the source. Is it backed by research? Has their neurologist recommended it? Parkinson's affects everyone differently—what provides miraculous relief for one person might do nothing for another.
"I've learned to appreciate the wisdom in these groups while keeping my doctor in the loop," shared Maria, a regular in several online support groups for Parkinson's disease. "The emotional support is immediate, but I always verify medical suggestions with my healthcare team."
Be particularly cautious when you notice:
Red flags that should raise your awareness include solicitations for money, aggressive product promotions, miracle cure claims, or pressure to abandon prescribed treatments. According to research on health misinformation, people with chronic conditions are frequently targeted with questionable treatment claims, making critical thinking an essential skill in these spaces.
Handling Misinformation in Online Support Groups for Parkinson's Disease
Even in the most well-intentioned communities, misinformation can spread. When someone shares questionable medical information, a gentle "May I ask what research that's based on?" can open a productive conversation without creating confrontation.
Most platforms have simple ways to report concerning content to moderators—don't hesitate to use these features if something seems potentially harmful. You can also help maintain the integrity of the group by sharing reliable resources from trusted organizations like the Parkinson's Foundation or Michael J. Fox Foundation when relevant.
Perhaps most importantly, always consult your healthcare team before trying any new treatment or supplement discussed online. Your neurologist or movement disorder specialist understands your specific situation and can help you evaluate whether a suggestion is appropriate for you.
When sharing your own experiences, using phrases like "In my experience..." or "This worked for me..." helps clarify that you're sharing a personal story rather than giving universal medical advice. This simple language choice acknowledges the beautiful diversity of the Parkinson's journey.
The best online support groups for Parkinson's disease have thoughtful moderation policies, but every community member plays a role in maintaining a space that's both supportive and trustworthy. With some basic awareness, you can enjoy all the benefits these groups offer while avoiding potential pitfalls.
Frequently Asked Questions about Online Support Groups for Parkinson's Disease
What should I expect the first time I log in?
Taking that first step into an online support group for Parkinson's disease can feel a bit like walking into a party where everyone already knows each other. It's completely normal to feel a mix of curiosity and nervousness!
Most newcomers find it helpful to simply observe for a little while before jumping into conversations. Think of it as getting the lay of the land. You'll notice that many groups have special "Welcome" or "New Member Introduction" sections specifically designed to help you ease in gently.
"When I first joined, I spent about a week just reading posts and getting a feel for the community vibe," shares Maria, a support group member from Arizona. "That made me much more comfortable when I finally introduced myself."
There's absolutely no rush to share your personal story right away. Many long-time members started as "lurkers" (people who read but don't post), and that's perfectly fine! The community will be there when you're ready to engage.
Are video meet-ups better than message boards?
This is a bit like asking whether texting is better than phone calls—they each have their own special strengths!
Video meet-ups create that face-to-face connection many of us crave. Seeing smiles, hearing laughter, and catching those subtle expressions can make conversations feel more personal and immediate. They're wonderful for building deeper connections and combating isolation.
Message boards, on the other hand, offer remarkable flexibility. You can participate at 3 AM in your pajamas if that's when your thoughts are clearest! They also give you time to carefully compose your questions or responses, which many people appreciate when discussing complex health matters.
Online support groups for Parkinson's disease often offer both formats because they complement each other beautifully. Many members tell us they check message boards throughout the week for specific information and attend monthly video calls for that more personal connection. Your preference might also change depending on your energy levels, symptoms, or schedule.
How do I keep my personal data private?
In our connected world, it's wise to think about privacy when joining any online community. Here's how to participate meaningfully while maintaining your comfort level:
Be thoughtful about your username—something that feels personal to you without revealing your full identity often works well. Many members use a first name or nickname combined with a meaningful number or word.
Consider what personal details really need sharing. Specifics about your Parkinson's journey are relevant, but your home address or financial information aren't necessary for meaningful connections.
Take a few minutes to review and adjust the privacy settings on whatever platform you're using. Most online support groups for Parkinson's disease have options to control who sees your profile information.
Even in closed groups, information isn't necessarily confidential. A good rule of thumb: if you wouldn't be comfortable seeing it on a community bulletin board, consider keeping it private.
Many seasoned members create a separate email address specifically for their support group activities, which helps keep their support life and personal life nicely organized.
The beauty of these communities is finding your own balance—sharing enough to form genuine connections while maintaining the privacy boundaries that feel right for you.
Conclusion & Next Steps
The journey with Parkinson's disease presents unique challenges, but you don't have to face them alone. Online support groups for Parkinson's disease offer powerful connections that complement medical care with peer wisdom, emotional support, and practical strategies for daily living.
As we've explored, these virtual communities come in many forms—from large international forums to specialized groups for specific demographics or needs. The key is finding the right fit for your situation and engaging in a way that serves your wellbeing.

Think of support groups as vital pieces in your Parkinson's management puzzle. They don't replace medical care but rather improve it by providing something healthcare appointments often can't: unlimited time to connect with others who truly understand your daily reality.
When you combine professional medical care with peer support, you create a holistic approach that addresses both the physical symptoms and emotional challenges of living with Parkinson's. This comprehensive strategy helps many people maintain a better quality of life despite the progressive nature of the condition.
Here in Brooklyn, we at Evolve Physical Therapy + Sports Rehabilitation understand the power of community support alongside specialized physical therapy. Our Rock Steady Boxing program, which was featured on NBC News, gives local patients the opportunity to build physical strength while simultaneously creating meaningful connections with others traveling the same path.
Whether you're newly diagnosed and feeling overwhelmed, a long-time patient looking for fresh perspectives, or a devoted care partner seeking your own support network, we encourage you to explore the online communities we've highlighted. And when possible, complement these virtual connections with in-person support opportunities in your local area.
For Brooklyn residents looking to improve their Parkinson's management strategy, our Parkinson's Physical Therapy programs are specifically designed to improve mobility, balance, and overall quality of life. These specialized sessions work wonderfully alongside the emotional support and practical wisdom you'll gain from online communities.
As one of our long-time support group members beautifully expressed: "Alone, we face tremendous challenges. Together, we find strength we never knew we had." This sentiment captures the essence of why connecting with others matters so deeply—our collective wisdom and shared experiences create a foundation of resilience that helps everyone stand stronger.
Take that first step today. Whether it's joining an online forum, signing up for a video meet-up, or reaching out to learn more about physical therapy options, you're not just finding support—you're becoming part of a community that understands, cares, and empowers.
Mobilize Those Ankles! A Fun Guide to Ankle Mobilization with Movement
Open up Better Movement With Ankle Mobilization Techniques

Ankle mobilization with movement is a hands-on technique that combines joint mobilization with active movement to improve ankle range of motion and function. Here's what you need to know:
- Definition: A manual therapy technique that applies a gliding force to the ankle joint while the patient actively moves the joint
- Main Benefits: Increases dorsiflexion by ~4°, improves walking speed by 0.08 m/s, and improves balance
- Basic Technique: Stabilize the talus bone while applying posterior glide as the ankle moves into dorsiflexion
- When to Use: For limited ankle mobility, post-ankle sprain, chronic stiffness, or as part of stroke rehabilitation
- Safety: Should be pain-free during application; stop if pain increases
When your ankles can't move properly, everything above them suffers. Limited ankle mobility—particularly dorsiflexion (the motion of bringing your toes toward your shin)—can create a chain reaction of problems throughout your body. From altered walking patterns to compromised squat form and even increased knee pain, stiff ankles often contribute to issues you might not immediately connect to your feet.
Research shows that mobilization with movement (MWM) techniques can significantly improve ankle function, especially in people recovering from injuries or those with chronic stiffness. What makes MWM different from regular stretching is the combination of joint gliding with active movement, which helps restore normal mechanics while reducing pain.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've spent nearly two decades helping patients overcome mobility limitations using specialized ankle mobilization with movement techniques to restore function and prevent recurring injuries. At Evolve, we've refined these methods to ensure you get lasting relief, not just temporary flexibility gains.

Why Ankle Mobility Matters for Everyday Movement & Sport
Your ankles might seem small compared to other joints, but they're mighty in importance. Think of your ankle as the foundation of a house—when that foundation can't move properly, everything built on top becomes a little wobbly.
Ankle dorsiflexion (that upward motion bringing your foot toward your shin) isn't just a fancy term physical therapists throw around. It's the movement that allows you to walk normally, climb stairs without stumbling, and squat down to pick up your grandchild—or that heavy Amazon package.
For our athletes in Brooklyn, we see how limited ankle mobility creates a ripple effect throughout the body. Ankle mobilization with movement techniques often become game-changers for them because proper ankle function affects everything from how you squat in the gym to how efficiently you run in Prospect Park.
"I had no idea my knee pain was actually coming from my ankles until my therapist at Evolve showed me the connection," is something we hear regularly from surprised patients. Your body truly is a connected chain—restriction in one link affects all the others.
Hidden Costs of Stiff Ankles
The consequences of poor ankle mobility go far beyond not being able to touch your toes to the wall. Here's what we commonly see in our Brooklyn practice:
Increased injury risk becomes almost inevitable when ankles can't move properly. Your body is smart but sometimes too accommodating—it will find ways to move even if that means overloading your knees, hips, or lower back.
Chronic pain patterns often develop as a result. That nagging plantar fasciitis? The Achilles tendon that always feels tight? Your ankle mobility might be the hidden culprit behind these persistent problems.
For our older patients, restricted ankle mobility significantly contributes to balance problems and fall risk. When your ankles can't adjust quickly to uneven surfaces, you're more likely to stumble.
And for our stroke recovery patients, the challenge is often compounded by spasticity (muscle tightness). This is where ankle mobilization with movement techniques become particularly valuable, as they address both joint restrictions and neurological factors affecting movement.
Research Snapshot: How Much Motion Do You Really Need?
Science gives us clear targets for healthy ankle mobility:
Walking down Smith Street requires about 10° of dorsiflexion. Seems small, but without it, your gait becomes inefficient and potentially painful.
For our runners hitting the Brooklyn Bridge Park paths, you'll need nearly 20° during the stance phase of running. Without this range, other joints compensate, often leading to injury.
And if you're working on those deep squats at the gym? Your ankles need almost 35° of dorsiflexion to maintain proper form without your heels lifting.
These aren't arbitrary numbers. Research published in Physical Medicine and Rehabilitation confirms these requirements for normal function.
What's particularly exciting is how effective proper treatment can be. Studies show that adding ankle mobilization with movement techniques to conventional exercises for stroke patients improved:
- Gait speed by 0.08 m/s
- Cadence by 9 steps/minute
- Step length by 5 cm
While these might seem like small numbers, they represent meaningful improvements in daily function and independence.
Common Culprits Behind Tight Ankles

Understanding what's causing your ankle stiffness helps us target treatment more effectively. Here at Evolve Physical Therapy, we commonly find several factors at play:
Previous ankle sprains often leave a lasting impact, even years later. That "rolled ankle" from your basketball days might still be affecting your movement patterns through joint restrictions.
Periods of immobilization from wearing a boot or cast can create both joint stiffness and positional faults that don't automatically resolve when the boot comes off.
Your footwear choices matter more than you might think. Those stylish high heels or even overly supportive athletic shoes can limit natural ankle movement over time.
ATFL scarring (that's the anterior talofibular ligament—the most commonly injured ankle ligament) often heals with adhesions after sprains, limiting how well your ankle moves.
Muscle guarding is your body's protective response after injury. While initially helpful, this persistent muscle tension can restrict movement long after healing.
For our older patients, arthritis changes in the joint surfaces can mechanically block normal motion, requiring specialized treatment approaches.
If you're experiencing ankle pain or stiffness, our specialized team can help with comprehensive treatment options. Learn more about our physical therapy for ankle pain at our Brooklyn clinic.
At Evolve Physical Therapy, we carefully assess each patient to identify the specific causes of their ankle mobility restrictions. This allows us to target treatment precisely, rather than using a one-size-fits-all approach that might miss the true source of your limitations.
Ankle Mobilization with Movement: Science & Step-by-Step
Ankle mobilization with movement (MWM) was developed by Brian Mulligan, a New Zealand physiotherapist who recognized that joint "positional faults" could be corrected through specific mobilization techniques performed during active movement.
The basic principle is simple yet profound: When a joint isn't moving correctly due to a positional fault (like the talus bone being slightly out of optimal position), applying a corrective glide while actively moving the joint can restore normal mechanics and reduce pain immediately.
How Mobilization with Movement Works
MWM works through several mechanisms:
- Correcting positional faults: The manual glide helps restore proper joint alignment
- Joint distraction: Creating space in the joint reduces impingement and pain
- Neurophysiological effects: Stimulation of mechanoreceptors can decrease pain signals
- Improved proprioception: Improved joint position sense leads to better movement control
Research suggests that in many ankle conditions, particularly following lateral ankle sprains, the talus bone may be positioned slightly anteriorly. By applying a posterior glide to the talus while the patient actively dorsiflexes the ankle, normal joint mechanics can be restored.
This is different from traditional passive joint mobilization because the active movement component improves the neurophysiological effects and makes the technique more functional.
Core Technique Walk-Through — Posterior Talar Glide MWM
Here's how we perform the basic posterior talar glide MWM at Evolve Physical Therapy:
Therapist-Applied Technique:
- Patient position: Standing with the affected foot on a stable surface, hands supported for balance
- Therapist position: Kneeling or sitting at the level of the patient's ankle
- Hand placement:
- One hand stabilizes the distal tibia and fibula
- The other hand contacts the talus just below the malleoli (ankle bones)
- The mobilization:
- Apply a gentle but firm posterior glide to the talus
- Maintain this glide while instructing the patient to actively bend the knee forward over the foot (dorsiflexion)
- Hold end range for 2-3 seconds, then return to starting position
- Maintain the glide throughout the movement
- Dosage: 6-10 repetitions, 2-3 sets
The technique should be pain-free. If pain occurs, adjust the direction or force of the glide, or try a different technique.
Self-Ankle Mobilization with Movement on an Incline Board
We often teach our patients self-mobilization techniques to continue their progress between visits:
Incline Board Self-MWM:
- Setup: Position a slant board or wedge (approximately 10° incline) with the high end away from you
- Foot placement: Stand with the affected foot on the board, heel down
- Stabilization: Use a non-elastic strap or belt wrapped around the lower leg just above the ankle
- The mobilization:
- Pull the strap backward to create a posterior glide of the talus
- While maintaining this glide, slowly bend your knee forward over your foot
- Focus on keeping your heel down and feeling a stretch in your calf
- Dosage: Hold each repetition for 2-3 seconds, perform 10 repetitions, 3 sets daily

This self-mobilization technique can be particularly effective for patients to practice at home between therapy sessions at our Brooklyn clinics.
Immediate Benefits Backed by Evidence
The research supporting ankle mobilization with movement is compelling:
- Range of motion improvements: Studies show an average increase of 4° in dorsiflexion range of motion after MWM techniques
- Walking improvements: Walking speed increases by an average of 0.08 m/s, cadence by 9 steps/min, and step length by 5 cm
- Balance improvements: Berg Balance Scale scores improve significantly with MWM compared to static stretching
One study of chronic stroke patients showed that the MWM group experienced a 53.5% increase in dorsiflexion range of motion compared to just 7.5% in the control group. These improvements translated directly to functional gains in walking and balance.
What's particularly impressive about MWM techniques is the immediacy of results. Many patients experience noticeable improvements in their first session, unlike traditional stretching which often requires weeks to show significant changes.
DIY vs. Clinician-Applied Techniques
When it comes to ankle mobilization with movement, you have options – do it yourself at home or work with a trained physical therapist. Both approaches can be effective, but they come with different advantages.
I've seen many patients try self-mobilization techniques after watching online videos, and while some make progress, others struggle with the precision these techniques require. Let me break down the key differences:
| Aspect | Self-MWM | Clinician-Applied MWM |
|---|---|---|
| Precision | Limited by self-visibility and reach | Precise targeting of specific joints |
| Force control | May be inconsistent | Carefully graded and adjusted |
| Feedback | Limited self-assessment | Immediate professional feedback |
| Technique variety | Limited options | Multiple techniques based on assessment |
| ROM gains | Moderate | Often greater due to precision |
| Equipment needs | Straps, wedges, etc. | Minimal - therapist's hands |
At Evolve Physical Therapy in Brooklyn, we typically start with hands-on techniques during your session. This gives us the chance to feel exactly how your ankle responds and make real-time adjustments. Once we see how your body reacts, we'll teach you effective self-mobilization methods to practice between visits.
Some of our more advanced clinical techniques include talus taping to maintain the corrected position after mobilization, banded MWM using resistance bands during functional movements, and combining MWM with specific Maitland grade mobilizations for optimal results.
When to See a Physical Therapist
While I'm all for taking charge of your own health, certain situations definitely call for professional help. Your ankles are too important to risk making things worse!
You should book an appointment if you're dealing with:
- Recent ankle sprains, especially if walking is painful
- Any post-surgical ankle condition
- Severe mobility limitations affecting your daily activities
- Pain that appears during your mobilization attempts (these should never hurt!)
- Complex health conditions like diabetes or neuropathy
- Self-care techniques that haven't improved things after 1-2 weeks
At our Brooklyn clinic, we specialize in thorough ankle assessments that pinpoint exactly what's causing your mobility restrictions. This allows us to develop a targeted plan that addresses your specific needs, not just generic exercises. Learn more about our physical therapy for ankle injury.
Integrating MWM into a Full Program
Ankle mobilization with movement works best when it's part of a comprehensive approach. It's like trying to fix a car – changing just one part rarely solves the whole problem!
When working with patients at Evolve, we combine MWM techniques with strengthening exercises for key muscles like the peroneals, tibialis anterior, and calves. We'll also incorporate eccentric calf training (slow, controlled lengthening exercises) that research shows is particularly effective for tendon health.
Balance training is another crucial component – we'll progressively challenge your proprioception (your body's position sense) on various surfaces. This helps "rewire" your brain's connection to your ankle.
We also focus on correcting movement patterns in everyday activities like walking and squatting. Sometimes we'll even include neurodynamic techniques when nerve tension contributes to your symptoms.
This well-rounded approach ensures that your newfound mobility actually translates into better function in real life – whether that's simply walking without pain or returning to high-level sports. After all, improved range on a measurement tool means nothing if it doesn't help you move better in your daily life!
Programming, Safety & Progress Tracking
Getting the most from ankle mobilization with movement isn't just about doing the technique correctly—it's also about smart programming. At Evolve, we've found that consistency is key to seeing lasting improvements in ankle mobility.
For most of our Brooklyn patients, we recommend practicing these techniques 3-5 times weekly. A typical 4-5 week program usually produces significant gains in mobility and function. Don't worry about spending hours on these exercises—quality matters more than quantity.
When structuring your sessions, aim for 3 sets of 10 repetitions for each MWM technique with a short 30-second breather between sets. We usually suggest performing these mobilizations before any strengthening work in the same session—this helps "open up" the joint before asking it to work harder.
"Think of mobility work as opening the door before you walk through it," I often tell my patients. "It makes everything that follows more effective."
Your progression journey should follow a logical path. If weight-bearing is painful initially, start with techniques lying down or seated. As comfort improves, progress to partial weight-bearing, then full weight-bearing, and finally incorporate the movements into functional activities like walking, squatting, or sport-specific drills.
Must-Know Contraindications
While ankle mobilization with movement techniques are generally safe and effective, they aren't right for every situation. Safety always comes first at Evolve Physical Therapy.
These techniques should be avoided or modified if you have acute fractures (let proper healing occur first), severe osteoporosis (which may require gentler approaches), or significant ligament instability. If you're experiencing an inflammatory arthritis flare-up, it's best to wait until the inflammation subsides before starting mobilization.
Some people actually have too much mobility (hypermobility) and need stabilization rather than mobilization. Others may have vascular compromise or circulation issues that require medical clearance before beginning these techniques.
It goes without saying, but we'll say it anyway—don't perform these techniques over open wounds or skin infections in the treatment area. This is both for comfort and to prevent potential complications.
At our Brooklyn clinic, we always perform thorough evaluations before recommending any mobilization program to ensure it's appropriate and safe for your specific situation.
Measuring Success
How do you know if your ankle mobility is actually improving? We believe in tracking objective measures rather than just going by feel (though that matters too!).
One of our favorite assessment tools is the half-kneeling wall test. We measure the distance from your toe to the wall when your knee can touch the wall while keeping your heel firmly planted. As mobility improves, this distance increases.
For more precise measurement, we use a goniometer to measure dorsiflexion range in degrees. The weight-bearing lunge test is another reliable option, where we measure the angle of the tibia during a forward lunge with the heel down.
Beyond these specific mobility measurements, we track functional improvements that matter in daily life:
- Walking speed using the 10-meter walk test
- Overall mobility with the timed up-and-go test
- Balance capabilities through single-leg balance time
- Comprehensive function via the Berg Balance Scale (especially helpful for our neurological patients)
We document these measurements during your initial evaluation and regularly throughout treatment. This gives us—and you—clear evidence of progress and helps us adjust your program as needed.
Beyond the Basics: Advanced Variations
Once you've mastered the fundamental techniques and are seeing improvements, we can introduce more advanced ankle mobilization with movement variations to further improve your results.
Talus-Stabilizing Taping offers a way to maintain the corrected talus position between sessions. We apply non-elastic tape from front to back, creating a gentle posterior glide force. This allows you to perform active movements throughout the day with the joint in optimal alignment, essentially extending your therapy beyond the treatment room.
For patients with fibular positional faults (common after rolling your ankle), we often use a Modified Fibular MWM. This involves applying an anterior glide to the distal fibula while you actively move your ankle in and out. It's remarkable how often this technique dramatically improves lateral ankle pain and mobility in a single session.
Athletic patients returning to jumping activities benefit from our Hopping MWM approach. We apply the appropriate glide (usually to the talus) while you perform mini-hops, gradually increasing height as symptoms allow. This bridges the gap between basic mobility work and the dynamic demands of sports.

These advanced techniques aren't for everyone—they're tools we select based on your specific needs and goals. At Evolve, we're committed to personalizing your care rather than applying a one-size-fits-all approach to ankle mobility.
Frequently Asked Questions about Ankle Mobilization with Movement
What's the difference between MWM and regular joint mobilization?
When patients ask me this question at our Brooklyn clinic, I explain it simply: think of regular joint mobilization as a passive experience—like being a passenger in a car. The therapist does all the work while you relax.
Ankle mobilization with movement is completely different—you're an active participant in the process. While I apply a specific glide to your joint, you're actively moving your ankle at the same time. This teamwork approach is what makes MWM so special.
This isn't just a technical difference—it creates real results. The active movement engages your nervous system in a unique way that often produces immediate pain relief and better movement. Many of our patients are surprised when they can walk with noticeably less pain right after their first session. Research consistently shows that this combined approach works better for improving ankle dorsiflexion than passive techniques alone.
How long before I feel improvements in my dorsiflexion?
The good news? You might feel better after just one session! Research shows a single ankle mobilization with movement treatment can increase dorsiflexion by 2-3 degrees immediately. Many of our patients at Evolve are pleasantly surprised when they stand up and can bend their ankle more freely right away.
For lasting changes, though, consistency matters. Most research points to a 4-5 week program (usually 3 sessions per week) for significant, sustainable improvements. During this time, you'll likely notice gradual improvements in walking speed, balance, and ability to climb stairs.
In our Brooklyn practice, we typically see meaningful functional improvements within 2-3 weeks when patients combine their in-clinic treatments with their home exercise program. Every person heals differently, but this timeline gives you a realistic expectation of progress.
Can I perform ankle MWM if I've had a recent sprain?
I get this question often, and the answer is: it depends on where you are in the healing process. If you've just sprained your ankle in the last few days, your priority should be protecting the joint and managing inflammation.
However, gentle ankle mobilization with movement can often be introduced earlier than many people expect—sometimes within the first week after injury. The golden rule we follow at Evolve is that MWM should never increase your pain. If a technique hurts, either the timing isn't right or we need to try a different approach.
For those chronic ankle issues—maybe you sprained your ankle months ago but it still doesn't feel right—MWM is often exactly what you need. Research shows that after ankle sprains, the talus bone often shifts slightly out of its optimal position. These techniques are specifically designed to address those positional faults.
I always recommend consulting with a physical therapist before trying self-mobilization on a recently injured ankle. At our Brooklyn clinic, we can assess your specific condition and create a personalized approach that respects your body's healing timeline while maximizing recovery.
Conclusion & Next Steps
Ankle mobilization with movement isn't just another stretching technique—it's a transformative approach that can change how you move through the world. By combining specific joint glides with active movement, these techniques often produce immediate improvements that you can actually feel from your very first session.
Whether you're dealing with lingering stiffness from an old ankle sprain, working through post-surgical recovery, or managing chronic ankle tightness that's affecting your daily life, MWM techniques can be the missing piece in your mobility puzzle.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe in the power of hands-on care. Our approach blends the science of rehabilitation with the art of manual therapy—we're not just treating your ankle, we're treating you as a whole person with unique needs and goals.
"The foundation affects everything above it," we often tell our patients. When your ankles move better, your knees, hips, and even your back often feel better too. That's why we take ankle mobility so seriously.
Our team proudly serves the Brooklyn communities of Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin with specialized programs custom to diverse needs. Our Rock Steady Boxing program for Parkinson's patients (featured on NBC News) demonstrates our commitment to innovative, effective care for complex conditions.
The journey to better mobility doesn't have to be complicated, but it does require expert guidance and a personalized approach. We're here to provide both, integrating ankle mobilization with movement into a comprehensive plan that addresses your specific challenges.
Ready to feel the difference that proper ankle mobility can make? We'd love to help you take that first step. Contact us today to schedule an evaluation at one of our Brooklyn locations, and experience how our approach to ankle mobilization with movement can transform not just your ankles, but your entire movement experience.
Don't let ankle stiffness keep you from the activities you love. Your body deserves to move with freedom and confidence—and we're here to help make that happen!
Exercise Your Right: Designing Therapeutic Programs
Understanding Therapeutic Exercise Programs: A Comprehensive Guide

Therapeutic exercise programs are structured, individualized physical activities prescribed by healthcare professionals to correct impairments, restore function, and promote overall wellness. Unlike general fitness routines, these programs are specifically designed to address medical conditions, injuries, or functional limitations.
Key Elements of Therapeutic Exercise Programs:
- Assessment-based - Custom to individual needs and capabilities
- Goal-oriented - Targets specific functional outcomes and pain reduction
- Progressive - Gradually increases in difficulty as function improves
- Evidence-based - Follows established clinical guidelines and research
- Supervised - Initially guided by physical therapists or healthcare professionals
Therapeutic exercise programs typically include combinations of:
- Strengthening exercises (isometric, isotonic, isokinetic)
- Flexibility and range of motion activities
- Balance and coordination training
- Endurance/aerobic conditioning
- Neuromuscular re-education
Research shows these programs are highly effective - with studies reporting 93% of patients experiencing reduced pain after participation and a 69% improvement in patient retention among those who complete their full course of care.
Whether you're recovering from surgery, managing a chronic condition like osteoarthritis, or rehabilitating a sports injury, a properly designed therapeutic exercise program can be your pathway back to optimal function and an active lifestyle.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've spent nearly two decades designing therapeutic exercise programs that help patients overcome pain, regain function, and return to their active lives with confidence and strength.

Therapeutic Exercise Programs: Definition, Goals & Who Benefits
When you hear "exercise program," you might think of treadmills and dumbbells at your local gym. But therapeutic exercise programs are something quite different – they're healing tools designed with precision and care.
At Evolve Physical Therapy in Brooklyn, we see therapeutic exercise programs as medicine in motion – structured physical activities carefully selected to address your specific needs, whether you're recovering from surgery, managing chronic pain, or working to regain lost function.
These aren't random workouts pulled from a fitness magazine. They're evidence-based interventions built on thorough clinical assessments that target the root cause of your physical limitations. According to scientific research, these specialized programs effectively reduce pain and improve function across a wide range of conditions.
Main Goals of therapeutic exercise programs
The beauty of therapeutic exercise programs lies in their multifaceted approach to healing. They're designed to rebuild your body's capabilities from the ground up:
Your mobility comes first – we work to restore range of motion and flexibility that may have been compromised by injury or disuse. This creates the foundation for everything else.
With improved movement comes strength development – not just building muscle, but teaching those muscles to fire correctly and support your joints properly.
We focus on endurance building too, because life isn't just about lifting something once – it's about having the stamina to make it through your day without fatigue.
Perhaps most important is neuromotor control – retraining your brain and body to communicate effectively, improving balance, coordination, and body awareness.
All these elements work together toward our ultimate goals: reducing your pain, preventing future injuries, and restoring your ability to participate fully in life's activities.
Why therapeutic exercise programs differ from general fitness
While both have value, therapeutic exercise programs and general fitness routines serve different purposes. Think of it this way: general fitness is like taking a group cooking class, while therapeutic exercise is like having a personal nutritionist design meals specifically for your health condition.
| Aspect | Therapeutic Exercise Programs | General Fitness Programs |
|---|---|---|
| Assessment | Comprehensive clinical evaluation | Basic fitness assessment |
| Design | Based on specific impairments and functional limitations | Based on general fitness goals |
| Supervision | Initially guided by healthcare professionals | Often self-directed or led by fitness instructors |
| Progression | Carefully structured based on healing timelines and functional milestones | Usually based on performance improvements |
| Monitoring | Regular reassessment of symptoms and function | Typically tracks weight, strength, or endurance metrics |
| Focus | Correcting impairments and restoring function | Improving general fitness components |
| Individualization | Highly customized to specific conditions | May use standardized protocols with minor modifications |
| Safety Parameters | Includes specific precautions based on medical condition | General safety guidelines |
This distinction matters because jumping into general fitness when you need therapeutic intervention can sometimes set back your recovery or even cause new problems.
Therapeutic exercise programs benefit a remarkably diverse group of people. Our Brooklyn clinics in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin welcome:
Older adults working to maintain independence and reduce fall risk through improved balance and strength.
Athletes eager to return to their sport after injury, using targeted exercises that rebuild sport-specific movements.
Post-surgical patients following precise protocols to ensure proper healing while regaining function.
Individuals managing chronic diseases like diabetes or COPD, using exercise as an effective management tool.
People with neurological conditions like stroke or Parkinson's, for whom the right exercises can dramatically improve quality of life.
Those with balance and vestibular disorders, who find relief through specialized movement patterns that retrain the body's balance systems.
Whether you're dealing with knee osteoarthritis, recovering from back surgery, or working to improve your functional capacity, a properly designed therapeutic exercise program can be transformative. Learn more about our approach to Therapeutic Exercise in Brooklyn and how we can help you move better, feel better, and live better.
Core Components & Exercise Types
Let's take a closer look at what actually goes into therapeutic exercise programs. Think of these components as the building blocks your physical therapist will use to construct your personalized road back to health and function.

Strengthening & Endurance
When it comes to rebuilding your body after injury or managing a chronic condition, strengthening exercises are often the cornerstone of recovery. At Evolve, we tailor these exercises to match exactly where you are in your healing journey.
Isometric exercises are often where we begin, especially when movement is painful or limited. These involve contracting muscles without actually moving the joint – like when you tighten your thigh muscle while keeping your leg straight. They're gentle yet effective for maintaining muscle during those early healing stages.
As you progress, we'll introduce isotonic exercises, which involve movement while your muscles work. These come in two flavors: concentric contractions (when muscles shorten as you lift something) and eccentric contractions (when muscles lengthen under tension as you lower something). Both are crucial for real-world function – after all, life involves both picking things up and putting them down!
For some conditions, we might use isokinetic exercises, which maintain consistent speed regardless of how hard you push. These are particularly valuable for rehabilitation because they provide appropriate resistance throughout your entire range of motion.
The science behind our approach comes from the American College of Sports Medicine guidelines, which recommend specific parameters for rehabilitation:
- Starting with moderate intensity (about 60-70% of your maximum capacity)
- Typically performing 1-3 sets of 8-12 repetitions
- Exercising each muscle group 2-3 times weekly with recovery days in between
- Gradually increasing difficulty as your strength improves
For rebuilding endurance, we follow similar evidence-based protocols, typically aiming for moderate-intensity activities 3-5 days weekly for 20-60 minutes. The goal is to progressively rebuild your stamina without overloading your healing tissues.
Flexibility & Range of Motion
Tight, restricted movement can be both a cause and consequence of injury. That's why flexibility training is essential to most therapeutic exercise programs.
We use several approaches to restore your normal movement patterns:
Static stretching is probably what you think of when someone mentions stretching – holding a position for 30-45 seconds to gradually lengthen tight muscles. It's simple but effective, especially for overall flexibility improvements.
Dynamic stretching involves moving through your available range of motion, gradually increasing reach or speed. Think of arm circles that get progressively larger. These are particularly helpful before functional activities since they mimic real-life movements.
For more challenging restrictions, we might use Proprioceptive Neuromuscular Facilitation (PNF) techniques. Despite the tongue-twister name, the concept is straightforward – we alternate between stretching and contracting specific muscle groups to "trick" your body into allowing greater range. It sounds complex, but the results speak for themselves!
Sometimes, our therapists will perform joint mobilization techniques – gentle, passive movements that help restore normal joint play and reduce pain. These hands-on techniques are one way we distinguish therapeutic stretching from general fitness approaches.
For most people, we recommend holding stretches for 30-45 seconds and doing 2-4 repetitions per muscle group, at least 2-3 times weekly. Daily stretching, though, typically yields the best results – something many of our Brooklyn patients build into their morning or evening routines.
Balance, Coordination & Neuromotor
The ability to control your body in space – whether you're standing on one leg or reaching for something on a high shelf – depends on complex systems working together. After injury or during aging, these systems often need retraining.

Balance training is about challenging your body's ability to maintain stability. We start with static exercises (like standing on one foot) and progress to dynamic challenges (like walking on uneven surfaces). To make these exercises more effective, we might narrow your base of support, use unstable surfaces like foam pads, have you close your eyes, or ask you to perform a mental task while balancing. Each variation retrains different aspects of your balance system.
Coordination training focuses on the timing and sequencing of movements. This might include agility exercises, reciprocal patterns (like opposite arm and leg movements), and activities that improve eye-hand coordination. For our athletes returning to sports, we incorporate sport-specific movement patterns to ensure you're ready for the playing field.
Many of our older Brooklyn residents benefit tremendously from programs like the Otago Exercise Program, which research shows can reduce falls by up to 35%. This structured approach combines strength and balance exercises specifically designed for fall prevention.
One interesting finding from recent research is that "error-based progression" – advancing exercises when movement quality improves rather than after a set time period – often yields better results. That's why our therapists are constantly assessing your performance and making adjustments, rather than following a rigid timeline.
At Evolve Physical Therapy + Sports Rehabilitation, we've found that the most effective therapeutic exercise programs combine multiple components – strengthening, flexibility, balance, and endurance – custom to your specific needs. Whether you're recovering from surgery in Park Slope, managing arthritis in Marine Park, or improving athletic performance in Midwood, these fundamental exercise types form the foundation of your recovery journey.
Customizing, Progressing & Ensuring Safety
The effectiveness of therapeutic exercise programs largely depends on proper customization and progression. At Evolve Physical Therapy + Sports Rehabilitation, we believe that no two patients are alike, and therefore, no two exercise programs should be identical.
Role of Physical Therapists in Designing & Supervising therapeutic exercise programs
Physical therapists play a crucial role in creating and implementing effective therapeutic exercise programs. Our expertise includes:
Comprehensive Evaluation: Before designing a program, we conduct a thorough assessment that includes:
- Medical history review
- Pain assessment
- Range of motion measurements
- Strength testing
- Functional movement analysis
- Balance and coordination assessment
- Specific tests related to the patient's condition
Individualized Program Design: Based on the evaluation findings, we create customized programs using the FITT principle:
- Frequency: How often exercises should be performed
- Intensity: How challenging the exercises should be
- Time: Duration of each exercise session
- Type: Specific exercises included in the program
Expert Supervision and Guidance: We provide:
- Hands-on assistance and manual cues to ensure proper form
- Visual demonstrations of exercises
- Verbal cues to improve movement quality
- Modifications as needed during the session
Progressive Adjustment: As patients improve, we:
- Increase exercise difficulty at the appropriate pace
- Add functional components that mimic daily activities
- Adjust resistance, repetitions, or duration
- Incorporate more challenging variations
Patient Education: We empower patients by:
- Explaining the purpose of each exercise
- Teaching proper body mechanics
- Providing home exercise instructions
- Educating about pain management and activity pacing
Outcome Tracking: We regularly:
- Reassess functional abilities
- Document progress
- Adjust goals as needed
- Celebrate achievements
The Karvonen formula is one tool we use to calculate target heart rate zones for aerobic exercise: Target HR = ((HRmax - HRrest) × % intensity) + HRrest
Where:
- HRmax = maximum heart rate (often estimated as 220 - age)
- HRrest = resting heart rate
- % intensity = desired training intensity (e.g., 60-80% for moderate to vigorous exercise)
This formula helps us prescribe aerobic exercise at the appropriate intensity for each individual's cardiovascular fitness level and goals.
Safety Considerations & Red Flags
Safety is paramount when implementing therapeutic exercise programs. At Evolve Physical Therapy, we emphasize the following safety considerations:
Pre-Exercise Screening:
- Medical clearance when necessary, especially for patients with cardiovascular, pulmonary, or metabolic conditions
- Identification of contraindications or precautions specific to the patient's condition
- Assessment of vital signs before, during, and after exercise as needed
Exercise Execution:
- Proper warm-up before and cool-down after each session
- Correct body positioning and alignment during exercises
- Appropriate breathing techniques (avoiding breath-holding)
- Gradual progression of intensity and complexity
Pain Monitoring:
- Distinguishing between therapeutic discomfort and harmful pain
- Using pain scales (0-10) to guide exercise intensity
- Following the "24-hour rule" (pain should not increase for more than 24 hours after exercise)
Red Flags that warrant immediate attention include:
- Sudden or severe pain during exercise
- Joint swelling or instability
- Dizziness, lightheadedness, or unusual shortness of breath
- Chest pain or pressure
- Excessive fatigue that doesn't resolve with rest
- Headache during exertion
- Unusual muscle weakness
Environmental Considerations:
- Appropriate exercise surface and footwear
- Adequate space for movement
- Proper equipment maintenance and use
- Temperature and humidity control when possible
Special Populations:
- Modified protocols for patients with osteoporosis (avoiding spinal flexion)
- Careful monitoring for diabetic patients (blood glucose checks)
- Adapted approaches for patients with balance deficits (ensuring proper support)
By addressing these safety considerations, we create an environment where patients can challenge themselves appropriately while minimizing the risk of injury or setbacks.
Evidence-Based Benefits & Digital Support Tools
When it comes to therapeutic exercise programs, the science speaks volumes. At Evolve Physical Therapy + Sports Rehabilitation, we don't just believe these programs work—we have the research to prove it.

Let's talk about real results. For those struggling with knee osteoarthritis, the evidence is clear—exercise therapy significantly reduces pain and improves physical function. What's even better? These benefits continue long after your formal therapy ends. The research doesn't lie: properly designed exercise programs are both safe and effective for managing this common condition. Learn more about the science behind therapeutic exercise here.
For our Brooklyn neighbors recovering from stroke, therapeutic exercise programs offer a pathway back to independence. Early, progressive exercise significantly improves walking ability, balance, and overall function. I've seen how these structured programs transform lives, one step at a time.
Living with chronic low back pain? You're not alone. That's why clinical guidelines consistently recommend exercise as a first-line treatment. At our Brooklyn clinics, we focus on core stability, flexibility, and conditioning exercises that have shown remarkable results in reducing pain and getting people back to doing what they love.
Tennis players from Park Slope to Marine Park know the frustration of epicondylitis (tennis elbow). Our progressive resistance programs, combined with targeted stretching and strengthening for those forearm muscles, help players get back on the court faster and stronger.
I'm particularly proud of our work with Parkinson's disease patients. Our specialized programs, including Rock Steady Boxing (which even caught NBC News' attention!), harness high-intensity exercise to slow disease progression and improve motor symptoms. The change we see in these patients is nothing short of inspiring.
For our older adult community members, fall prevention is crucial. Programs like Otago have demonstrated up to a 35% reduction in falls. That's not just a statistic—it's peace of mind for families throughout Brooklyn.
The numbers tell a powerful story:
- 93% of patients report less pain after participating in therapeutic exercise programs
- Patient retention improves by 69% when people complete their full care plan
- FOTO (Focus On Therapeutic Outcomes) effectiveness scores jump by 12% when digital home exercise programs are used
- No-shows and cancellations decrease by 15% with digital support tools
Home Exercise Program Adherence Strategies
Let's be honest—even the best therapeutic exercise program won't help if you're not doing the exercises regularly. That's why we've developed strategies to help you stay on track.

Education is everything. When you understand why you're doing each exercise and how it helps your recovery, you're more likely to stick with it. We take time to demonstrate each movement, provide clear instructions, and answer all your questions. The "why" behind each exercise is just as important as the "how."
Digital tools make a difference. Using platforms like HEP2go and MedBridge, we create personalized exercise programs you can access right from your smartphone or tablet. These aren't just static instructions—they include video demonstrations, tracking features, and reminders to keep you accountable. It's like having a PT in your pocket!
Making exercise fun might sound impossible when you're recovering, but we've found that adding gamification elements like achievement badges and progress visualization can transform your mindset. Some patients even enjoy friendly competition with themselves or others in similar recovery journeys.
We also focus on practical implementation. Rather than overwhelming you with a lengthy routine, we might start with just 10-15 minutes of targeted exercises that fit into your daily life. Exercise calendars, integration with your existing routines, and simplified programs all boost your chances of success.
Regular check-ins between in-person sessions help us catch and correct any form issues early. Our telehealth options allow us to review your exercise technique without requiring an extra trip to our Brooklyn clinics. We're always ready to adjust your program based on your feedback and progress.
Many patients benefit from wearable technology like activity trackers and heart rate monitors. These devices provide objective data about your movement and exercise intensity, helping us fine-tune your program for optimal results.
Research confirms what we see every day: patients who receive clear instructions, regular feedback, and digital support stick with their home exercises more consistently. And those who complete at least 80% of their prescribed exercises achieve twice the functional improvement compared to those who don't.
At Evolve Physical Therapy + Sports Rehabilitation, we've found that combining hands-on guidance during your visits with user-friendly digital tools for home use creates the perfect environment for successful rehabilitation. Learn more about our strengthening programs in Brooklyn or explore how we approach core stabilization.
Frequently Asked Questions about Designing Therapeutic Programs
What makes a therapeutic exercise program effective?
When patients ask me what makes their therapeutic exercise program truly effective, I tell them it's a bit like cooking a great meal—you need the right ingredients in the right proportions!
First and foremost, an effective program must be evidence-based. At Evolve Physical Therapy + Sports Rehabilitation, we're constantly reviewing the latest research to ensure our Brooklyn patients receive care that reflects current best practices. There's simply no substitute for approaches backed by solid science.
But science alone isn't enough—your program needs to be uniquely yours. I've seen how personalization transforms outcomes. A program designed specifically for your body, your limitations, and your goals will always outperform generic exercises. Your knee pain isn't the same as someone else's, so why would your exercises be identical?
Progressive overload is another essential ingredient. Your body adapts to challenges, so your program must evolve as you do. When those 2-pound weights start feeling light, it's time to level up! This gradual increase in difficulty is what builds strength and function over time.
The most successful programs I've designed over my years in Brooklyn also maintain a strong connection to real life. If you're a teacher who needs to bend down to help students, or a grandmother who wants to lift your grandchildren, your exercises should prepare you specifically for those movements. This functional relevance ensures your improvements translate to everyday life.
A well-rounded program typically balances strengthening, flexibility, endurance, and coordination components—though we'll emphasize whatever areas you need most. Think of it as addressing all sides of the rehabilitation pyramid, not just the most obvious one.
Patient engagement makes a world of difference too. When you understand why you're doing each exercise and how it contributes to your recovery, you're much more likely to stick with it. That's why we take time to educate, not just instruct.
How often should a program be updated?
This is one of the most common questions I hear in our Brooklyn clinics! The simple answer is: it depends on you, not the calendar.
Rather than rigidly updating programs every X days, we prefer milestone-based progression. When you can complete your exercises with good form and minimal effort, or when you achieve specific functional goals we've set together, that's our signal to advance your program.
That said, we typically reassess and update programs every 2-4 weeks for most patients. Acute injuries might need more frequent adjustments as healing progresses rapidly, while chronic condition management might involve less frequent changes as we find what works best for your body.
You might need a program update when:
- Exercises start feeling too easy (you're breezing through them without much effort)
- Your progress plateaus (measurements of strength or motion aren't improving)
- Your pain patterns change (either improving or worsening)
- You have new goals or activities you want to return to
I remember working with a runner recovering from an ankle sprain who was progressing beautifully with basic balance exercises. When those became too easy, we didn't wait for her scheduled reassessment—we immediately added dynamic movements to match her improving function. Listening to your body and communicating with your therapist is key to timing these updates perfectly.
Can I design my own program without a therapist?
I get it—we all love a good DIY project! But designing your own therapeutic exercise program is a bit like being your own mechanic when your car makes a strange noise. You might identify some issues, but without specialized training, you might miss the underlying cause.
The biggest challenge with self-designed programs is accurate assessment. What feels like simple knee pain might actually stem from hip weakness or foot mechanics. Our physical therapists are trained to connect these dots through specialized assessment techniques that aren't easily replicated at home.
Safety is another significant concern. Some exercises that look harmless on YouTube could actually worsen certain conditions. For instance, specific spinal conditions have clear movement contraindications that aren't obvious without clinical training.
Many self-designed programs I've seen overemphasize certain aspects (usually strengthening) while completely neglecting others (like proprioception or neuromuscular control). It's like only changing your car's oil but never checking the brakes or tires—you're missing crucial components.
That said, there are situations where you can safely implement basic exercises:
- Following a previously prescribed program for a familiar, recurring condition
- Maintaining function after completing formal therapy
- General conditioning when you're free from acute injuries or significant medical issues
At Evolve Physical Therapy, we aim to make you as independent as possible. Many of our Brooklyn patients eventually transition to more self-directed programs, but with the solid foundation and education we provide through professional therapy. Think of us as your guides, helping you build the knowledge and skills to eventually manage more of your physical health on your own.
The ideal approach? Start with professional guidance, learn proper techniques, understand your body's unique needs, and gradually take on more self-management as appropriate for your condition. Your body deserves that level of care!
Conclusion
Therapeutic exercise programs are so much more than just a workout routine – they're a scientifically-backed pathway to recovery that addresses the root causes of pain and dysfunction while building lasting strength and mobility. When designed with care and implemented consistently, these programs truly transform lives.
Here at Evolve Physical Therapy + Sports Rehabilitation, we've seen how properly designed therapeutic exercise programs help our Brooklyn neighbors recover faster, move with greater confidence, and return to the activities they love. Our dedicated team brings together clinical expertise and genuine compassion at each of our locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin.
The numbers speak for themselves – 93% of patients experience meaningful pain reduction through therapeutic exercise, and the improvements in functional outcomes can be truly life-changing. Whether you're bouncing back from surgery, managing arthritis, rehabilitating after a sports injury, or working to prevent future problems, a personalized approach makes all the difference.
What makes our approach special is that we don't just hand you a sheet of exercises and send you on your way. We take the time to understand your unique needs, design a program specifically for you, and guide you through each step with expertise and encouragement. We believe the best therapeutic exercise program is one that fits seamlessly into your life and actually feels doable – because consistency is where the magic happens.
Beyond the exercises themselves, we focus on making the entire process engaging and understandable. We want you to not just do the movements but understand why they matter for your recovery. This deeper understanding often becomes the motivation that carries patients through challenging moments in their rehabilitation journey.
The evidence is clear and compelling: properly designed and consistently performed therapeutic exercises lead to significant improvements across a wide range of conditions. From reducing pain to restoring function and enhancing quality of life, these specialized programs deliver results that matter.
We invite you to experience the Evolve difference – where evidence-based, expertly guided therapeutic exercise becomes your pathway to better movement and improved wellbeing. Your journey to feeling better and moving with confidence begins with that first step of reaching out to our team.
Exercise your right to move well, feel better, and enjoy the active Brooklyn lifestyle you deserve with a therapeutic exercise program created just for you. Let's evolve together.
The Ultimate Guide to Drugs in Parkinsonism
Understanding the Complex World of Drugs in Parkinsonism

Drugs in parkinsonism fall into two main categories: those that cause parkinsonian symptoms and those that treat them. Here's a quick overview:
Drugs that can cause parkinsonism:
- Typical antipsychotics (haloperidol, chlorpromazine)
- Some atypical antipsychotics
- GI motility drugs (metoclopramide)
- Calcium channel blockers (flunarizine, cinnarizine)
- Antiepileptics (valproate)
- Lithium
Drugs that treat parkinsonism:
- Levodopa (often with carbidopa)
- Dopamine agonists (pramipexole, ropinirole)
- MAO-B inhibitors (selegiline, rasagiline)
- COMT inhibitors (entacapone, opicapone)
- Anticholinergics (trihexyphenidyl)
- Amantadine
Parkinsonism describes a group of neurological conditions characterized by movement problems similar to those seen in Parkinson's disease: tremor, rigidity, bradykinesia (slowness of movement), and postural instability. While Parkinson's disease is the most common cause, drug-induced parkinsonism (DIP) ranks as the second most prevalent form, especially in older adults.
The relationship between drugs and parkinsonism is complex. Some medications disrupt the delicate balance of dopamine in the brain, either by blocking dopamine receptors or interfering with dopamine production and storage. When this happens, the symptoms can mimic those of Parkinson's disease so closely that even experienced clinicians may struggle to tell them apart.
What makes this topic particularly important is that drug-induced parkinsonism is often reversible if caught early and the offending medication is stopped. However, studies show that in 10-50% of patients, symptoms may persist even after discontinuation, suggesting that some drugs might unmask an underlying predisposition to Parkinson's disease.
I'm Lou Ezrick, and throughout my career as a physical therapist, I've worked with numerous patients experiencing the physical limitations caused by drugs in parkinsonism, developing specialized protocols that complement medication management with targeted movement therapies.
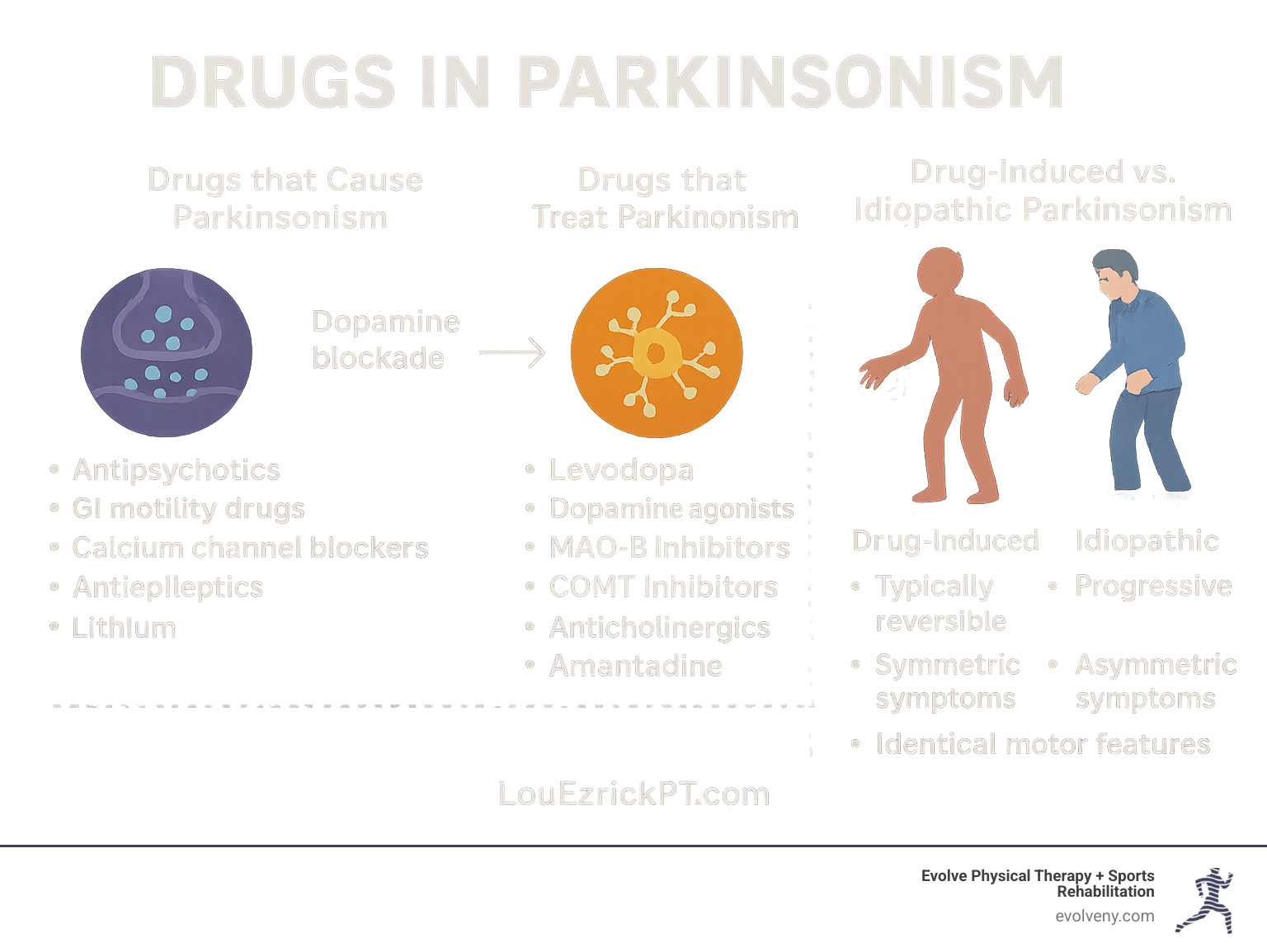
Understanding Parkinsonism: Definitions, Types & Causes
Parkinsonism is an umbrella term for a group of neurological conditions that cause movement problems similar to those seen in Parkinson's disease. These include tremor (especially at rest), rigidity, bradykinesia (slowness of movement), and postural instability. While these symptoms might look the same on the surface, their underlying causes can vary significantly.

Idiopathic vs Secondary Syndromes
Idiopathic Parkinson's Disease (PD) is the most common form, affecting approximately 1% of individuals over the age of 65. It results from the progressive degeneration of dopamine-producing neurons in the substantia nigra, a region of the brain involved in movement control. This degeneration is associated with the accumulation of a protein called alpha-synuclein, which forms clumps known as Lewy bodies within neurons.
The progression of Parkinson's disease follows what scientists call Braak staging, where pathological changes begin in specific brain regions and spread in a predictable pattern. Interestingly, symptoms only become apparent after about 60-80% of dopaminergic neurons have been lost—highlighting the brain's remarkable compensatory abilities.
Secondary parkinsonism includes several subtypes:
Drug-Induced Parkinsonism (DIP): The second most common cause of parkinsonism, particularly in older adults. Several large, population-based studies in Europe estimated a prevalence of DIP ranging from 0.09% to 1.7%, which is only slightly lower than idiopathic PD (0.37% to 1.9%).
Vascular Parkinsonism: Caused by small strokes in brain regions controlling movement.
Post-traumatic Parkinsonism: Following severe head injury.
Toxin-induced Parkinsonism: From exposure to certain environmental toxins.
Genetic forms: Including those linked to specific gene mutations.
Key Risk Factors for Drug-Induced Cases
Understanding who's at risk for developing drug-induced parkinsonism is crucial for prevention and early intervention. Key risk factors include:
Age: The percentage of patients with drug-induced parkinsonism increases with age, with the highest incidence in those between 60 and 80 years. This is partly because dopamine cell count and transport naturally decline with age, lowering the threshold for developing parkinsonism.
Sex: Women appear more susceptible than men, with some studies showing a female-to-male ratio of 2:5.
Medication dose and duration: Higher doses and longer treatment durations increase risk.
Renal or hepatic impairment: These conditions can lead to higher blood levels of medications due to reduced clearance.
Polypharmacy: Taking multiple medications that affect dopamine pathways can have additive effects.
Genetic factors: Some genetic variants may predispose individuals to developing DIP.
It's worth noting that about 50% of patients with DIP are treated with dopamine receptor blocking agents for conditions unrelated to psychosis, including depression, gastrointestinal disturbances, anxiety, and insomnia—highlighting the importance of medication review across all specialties.
The Ultimate Breakdown of Drugs in Parkinsonism: Offending & Therapeutic Agents
When it comes to drugs in parkinsonism, there's a fascinating paradox at work. Some medications can trigger parkinsonian symptoms, while others are specifically designed to relieve them. Understanding this dual relationship is essential for anyone navigating this complex neurological territory.
Which Drugs in Parkinsonism Are Most Likely to Cause Symptoms?
The medications most likely to trigger parkinsonian symptoms typically work by interfering with dopamine—either by blocking its receptors or disrupting its storage and release in the brain.
The most common culprits are antipsychotics, especially the older "typical" ones like haloperidol and chlorpromazine. These medications pack a powerful dopamine-blocking punch, with studies showing that about 40% of patients taking chlorpromazine develop parkinsonian side effects. In fact, about 80% of people taking typical antipsychotics will experience at least one type of movement-related side effect.
Surprisingly, medications prescribed for completely unrelated conditions can also trigger parkinsonism. Metoclopramide, commonly used for nausea and digestive issues, crosses into the brain and blocks dopamine receptors. Similarly, certain calcium channel blockers like flunarizine, prescribed for migraines and dizziness, can cause parkinsonism through mechanisms that researchers are still working to fully understand.
Other medications to watch out for include the antiepileptic drug valproate (causing parkinsonism in about 5% of long-term users), mood stabilizers like lithium, and various antidepressants and cardiac medications. The prevalence of drug-induced parkinsonism ranges from 0.09% to 1.7% in the general population—nearly as common as Parkinson's disease itself.
Therapeutic Drugs for Managing Parkinsonism
On the flip side, several medication classes help manage parkinsonian symptoms by boosting dopamine function in the brain.
Levodopa/carbidopa remains the gold standard treatment. Levodopa converts to dopamine in the brain, while carbidopa prevents its breakdown outside the brain, reducing side effects. It comes in various formulations, from immediate-release tablets to extended-release capsules and even an intestinal gel for advanced cases. With a short half-life of about 90 minutes, long-term users often develop "wearing off" symptoms as the medication's effects fluctuate.
Dopamine agonists like pramipexole and ropinirole work differently—they directly stimulate dopamine receptors, bypassing the need for dopamine production entirely. These medications last longer in the body (4-6 hours) and may cause fewer motor fluctuations, but they tend to bring more psychiatric side effects like hallucinations and compulsive behaviors.
For many patients, the supporting cast of medications is just as important. MAO-B inhibitors like selegiline and rasagiline prevent dopamine breakdown in the brain, while COMT inhibitors like entacapone extend levodopa's effects. Amantadine, originally developed as an antiviral medication, helps release dopamine from nerve terminals and can reduce the involuntary movements (dyskinesias) that often develop with long-term levodopa use.
Anticholinergics such as trihexyphenidyl may help with tremor but come with significant cognitive side effects, especially for older adults. The newest addition to the arsenal, istradefylline, works through a completely different mechanism (adenosine A2A antagonism) to help with "off" episodes.
Pathophysiology & Course after Drug Exposure
Drug-induced parkinsonism differs from Parkinson's disease at the cellular level. While Parkinson's involves the death of dopamine-producing neurons, drug-induced parkinsonism temporarily blocks dopamine receptors without killing cells—like putting a lock on a door rather than demolishing the building.
After starting an offending medication, symptoms typically appear within days to months. The good news is that after stopping the medication, most people improve within weeks to months. However, in 10-50% of patients, symptoms persist or progress, suggesting that the medication may have unmasked an underlying predisposition to Parkinson's disease. Even more intriguingly, in about 7% of patients who fully recover, symptoms mysteriously return months later.
| Feature | Drug-Induced Parkinsonism | Idiopathic Parkinson's Disease |
|---|---|---|
| Onset | Subacute (days to months) | Gradual (months to years) |
| Symmetry | Usually symmetric | Typically asymmetric |
| Tremor | Less common, symmetric | Common, asymmetric rest tremor |
| DAT imaging | Normal DAT uptake | Reduced asymmetric DAT uptake |
| Response to levodopa | Limited or poor | Good |
| Progression after drug cessation | Usually resolves (50-90%) | Progressive |
| Risk factors | Age, female sex, high medication dose | Age, family history, environmental exposures |
Understanding these patterns helps clinicians distinguish between drug-induced and idiopathic parkinsonism—a critical distinction that determines treatment approach and long-term prognosis. At Evolve Physical Therapy, we work alongside your medical team to provide comprehensive care that addresses both the neurological and physical aspects of parkinsonism, regardless of its cause.
Diagnosing & Differentiating Drug-Induced Parkinsonism
Telling the difference between drug-induced parkinsonism (DIP) and idiopathic Parkinson's disease (PD) can feel like detective work. As someone who's worked with many patients facing this exact challenge, I can tell you that the distinction is crucial – yet the symptoms can look nearly identical to even trained eyes.

When a patient comes to us with parkinsonian symptoms, we start with a comprehensive approach:
First, we dive into their medication history – did symptoms appear after starting a new medication? We're particularly interested in recent additions of any dopamine-blocking agents. I once had a patient whose tremor began just weeks after starting an anti-nausea medication she didn't even realize could affect her movement.
Next comes a thorough medication review, including those over-the-counter supplements many patients forget to mention. You'd be surprised how often the culprit is hiding in plain sight!
During the neurological examination, we use tools like the Unified Parkinson's Disease Rating Scale (UPDRS) to objectively measure symptoms. We're looking for patterns – is the tremor symmetrical? How severe is the rigidity? Does the patient have that characteristic "masked face" expression?
Role of Imaging in Confirming or Ruling Out PD
Brain imaging has truly transformed how we distinguish between these conditions. When clinical evaluation leaves us uncertain, these tests can provide clarity:
DAT-SPECT imaging has become our gold standard. This specialized brain scan uses radioactive tracers that bind to dopamine transporters in the brain. What we're looking for is quite straightforward: in drugs in parkinsonism cases, these scans typically show normal dopamine transporter binding. In contrast, Parkinson's disease patients show reduced binding, usually in an asymmetric pattern.
Other options include PET scans (offering higher resolution) and Beta-CIT SPECT (with impressive 87.7% diagnostic accuracy in distinguishing between the two conditions).
These imaging tests become particularly valuable when symptoms stick around after stopping the suspected medication, or when something about the clinical picture just doesn't add up. Research published in the Journal of Neurology, Neurosurgery & Psychiatry has shown that DAT-SPECT can significantly improve diagnostic accuracy, with one study finding that nearly 7% of patients initially diagnosed with PD were actually suffering from drug-induced symptoms.
Red Flags Suggesting Underlying Degeneration
Sometimes what looks like simple medication side effects might actually be an underlying Parkinson's disease that was "unmasked" by the medication. Here are the warning signs we watch for:
Asymmetric symptoms often point to PD – when tremor or stiffness affects one side of the body more than the other, it's less likely to be medication-related. Classic rest tremor that has that "pill-rolling" quality between thumb and forefinger is another red flag.
Other concerning signs include reduced sense of smell (which often precedes motor symptoms in PD by years), REM sleep behavior disorder (acting out dreams during sleep), and continued progression despite stopping the medication.
I remember working with a gentleman who initially improved after stopping his antipsychotic medication, but then noticed his symptoms returning months later. His neurologist ordered a DAT scan, which revealed early Parkinson's disease – the medication had simply revealed what was already beginning.
Response to levodopa can also be telling – significant improvement with this medication typically suggests true Parkinson's rather than drug-induced symptoms.
At Evolve Physical Therapy + Sports Rehabilitation, we partner closely with neurologists to ensure our patients receive an accurate diagnosis. This collaboration forms the foundation for our specialized physical therapy interventions, allowing us to tailor our approach to each individual's unique needs and underlying condition.
Treating, Managing & Preventing Drug-Induced Parkinsonism
The management of drug-induced parkinsonism (DIP) differs significantly from that of idiopathic Parkinson's disease, primarily because DIP is often reversible when the offending medication is discontinued.

Do Standard Drugs in Parkinsonism Help Drug-Induced Cases?
When it comes to drugs in parkinsonism that's triggered by medications, the treatment approach is quite different from what works for Parkinson's disease itself.
Levodopa, the gold standard treatment for Parkinson's disease, typically doesn't work as well for drug-induced cases. This makes perfect sense when you think about it - in DIP, those dopamine receptors are being blocked rather than depleted. Adding more dopamine through levodopa is a bit like trying to enter a locked door by pushing harder - the key issue is the lock, not the force!
That said, we sometimes do try a careful course of levodopa if we can't stop the offending medication, or if symptoms stick around after withdrawal. Interestingly, contrary to what many doctors learned in medical school, giving levodopa to DIP patients doesn't necessarily make their psychotic symptoms worse.
Anticholinergic medications like trihexyphenidyl and benztropine can actually help in DIP cases by rebalancing the dopamine-acetylcholine relationship in the brain. The downside? They can make you feel like you've got a mouth full of cotton, blur your vision, and confuse your thinking - especially troublesome for older adults who are already the most vulnerable to DIP.
Amantadine often proves to be a better option, especially for our older patients. It works through several mechanisms and typically causes fewer cognitive side effects than anticholinergics.

The most effective approach to managing DIP is straightforward but requires careful coordination with your prescribing doctor. First and foremost, discontinuing or reducing the offending medication is the most effective strategy when possible. About 70% of patients show improvement within weeks to months after stopping the troublemaker drug.
If you can't completely stop a psychiatric medication, switching to alternatives with lower risk makes sense. Quetiapine or clozapine typically cause fewer movement problems than older antipsychotics. For digestive issues, domperidone (which doesn't cross into the brain) is preferable to metoclopramide.
When stopping medications, a gradual approach is usually best. Quitting certain drugs cold turkey (especially antipsychotics) can trigger withdrawal symptoms or a flare-up of the condition being treated.
For persistent symptoms, we might recommend anticholinergics or amantadine, but we'll keep a close eye on side effects, especially in our older patients. We typically limit how long someone stays on anticholinergics when possible.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen remarkable results when combining medication management with specialized physical therapy. Our programs include gait training to improve walking, balance exercises to prevent falls, and strength training to maintain muscle function. Many of our patients with parkinsonism symptoms have benefited tremendously from our Rock Steady Boxing program, which specifically targets Parkinson's symptoms through an engaging, fun format that doesn't feel like traditional therapy.
Prevention Strategies for High-Risk Populations
An ounce of prevention is worth a pound of cure - especially true for drugs in parkinsonism. For those at higher risk (older adults, women, and people with existing neurological issues), we recommend several protective strategies.
First, careful drug selection is crucial. When possible, avoid medications that block dopamine, especially in high-risk individuals. When these medications are necessary, use the lowest effective dose possible.
Regular monitoring makes a huge difference - checking for subtle signs of parkinsonism every 3-6 months can catch problems early. We also emphasize patient and caregiver education so everyone knows what early warning signs look like.
For conditions like nausea or vertigo, exploring alternative treatments without dopamine-blocking properties can prevent problems before they start. And regular medication reconciliation helps identify potential drug interactions that might increase DIP risk.
At Evolve Physical Therapy + Sports Rehabilitation, we work as part of your healthcare team, collaborating with neurologists and primary care physicians to provide comprehensive care. We combine our specialized physical therapy interventions with medication management guidance to help you recover faster and prevent recurrence. Our hands-on approach means we're with you every step of the way, celebrating each improvement and adjusting strategies as needed to optimize your recovery.
Frequently Asked Questions about Drugs in Parkinsonism
What is the difference between drug-induced and idiopathic Parkinson's disease?
If you've ever wondered about the key differences between these two conditions, you're not alone. While they may look similar on the surface, they're actually quite distinct under the hood.
Drug-induced parkinsonism (DIP) happens when certain medications disrupt your brain's dopamine system. Think of it as temporarily jamming the signals that control movement. In contrast, idiopathic Parkinson's disease involves the actual death of dopamine-producing cells in your brain – a much more permanent situation.
You can often spot the difference in how symptoms appear. DIP typically affects both sides of your body equally, while Parkinson's disease usually starts on one side before spreading. When doctors perform specialized brain scans (dopamine transporter imaging), DIP patients show normal dopamine activity, while those with Parkinson's show reduced activity.
Perhaps most importantly, DIP has a good chance of reversing once you stop taking the problematic medication, while Parkinson's disease continues to progress over time. This reversibility is why proper diagnosis is so crucial – it could mean the difference between a temporary and a lifelong condition.
How long does parkinsonism last after stopping the culprit drug?
"When will I feel normal again?" This is often the first question patients ask after learning their symptoms are medication-related. The good news is that improvement typically begins within days to weeks after stopping the offending medication.
Most people experience complete resolution within 2-6 months. Research shows the average recovery time is about 13 weeks, though this varies from person to person. Your age, how long you took the medication, and your overall health all influence your recovery timeline.
It's important to know that for some patients—about 10-50% according to studies—symptoms may persist even after stopping the medication. This doesn't necessarily mean the drug caused permanent damage; rather, it might have unmasked an underlying predisposition to Parkinson's disease that would have eventually emerged anyway.
In a small percentage of cases (around 7%), symptoms may completely resolve but then return months later. This is why we at Evolve Physical Therapy + Sports Rehabilitation recommend ongoing monitoring even after symptoms improve.
Can physical therapy replace medications for drug-induced parkinsonism?
While physical therapy can't replace the critical step of discontinuing the problematic medication, it plays an invaluable supporting role in recovery. I've seen how the right physical therapy approach can dramatically improve quality of life while patients wait for medication effects to wear off.
At Evolve Physical Therapy + Sports Rehabilitation, we focus on addressing the specific movement challenges caused by drugs in parkinsonism. Our specialized programs target rigidity, improve balance, and help restore normal movement patterns through neuroplasticity – your brain's remarkable ability to rewire itself with proper stimulation.
One of our most successful programs is Rock Steady Boxing, which was even featured on NBC News for its effectiveness in combating parkinsonian symptoms. The program's combination of high-intensity exercise, cognitive challenges, and social interaction creates the perfect environment for neurological recovery.
Even when medications cannot be discontinued (which happens in some psychiatric conditions), our physical therapy approaches can significantly improve function and prevent complications like muscle contractures and falls. We've seen patients regain independence in daily activities even while continuing necessary psychiatric medications.
The research strongly supports this combined approach – patients who receive both appropriate medication management and specialized physical therapy consistently show better outcomes than those receiving either intervention alone. This is why we work closely with neurologists and primary care physicians to coordinate care for optimal results.
Your body has an amazing capacity to heal when given the right support. Our team is here to guide that process every step of the way.
Conclusion
Navigating the complex world of drugs in parkinsonism is like finding your way through a maze—it requires understanding both the medications that trigger symptoms and those that provide relief. Throughout this guide, we've seen how drug-induced parkinsonism represents a significant portion of cases, especially among older adults, yet it often flies under the diagnostic radar.
The silver lining is that with proper identification and timely intervention, many people suffering from drug-induced parkinsonism can experience a reversal of their symptoms. Recovery begins with early recognition—noticing when tremors or stiffness appear shortly after starting a new medication. A proper diagnostic workup, sometimes including specialized brain imaging, helps distinguish drug-induced symptoms from Parkinson's disease.
When possible, the most effective approach is simply stopping the problematic medication. This often requires working with your doctor to find alternative treatments for your underlying condition—whether it's a mental health issue, digestive problem, or another medical concern. In some cases, medications specifically designed for Parkinson's disease may help manage symptoms while waiting for the effects of the offending drug to wear off.
Here at Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe that managing parkinsonism goes beyond medication adjustments. Our hands-on programs provide the human touch that complements medical care. Many of our patients find remarkable benefits from our Rock Steady Boxing program (the same one featured on NBC News), which specifically targets the motor symptoms that make daily activities challenging.
We take pride in our holistic approach, recognizing that each person's experience with parkinsonism is unique. Whether you're dealing with medication-induced symptoms or idiopathic Parkinson's disease, our team works in harmony with your neurologists and primary care physicians to create a coordinated care plan that addresses all aspects of your condition.
Drug-induced parkinsonism, while certainly challenging, stands out as one of the few potentially reversible forms of parkinsonism. With quick recognition, appropriate medical management, and specialized physical therapy, many patients can reclaim their mobility and quality of life.
If you're experiencing shakiness, stiffness, or slowness of movement and take any of the medications we've discussed, we encourage you to have a conversation with your healthcare provider. Consider how our specialized physical therapy services might complement your medical care and accelerate your recovery.
For our neighbors in Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin areas—our team at Evolve Physical Therapy + Sports Rehabilitation is ready to support your journey back to fluid, confident movement and improved quality of life. Your recovery doesn't have to be a solo journey—we're here to walk alongside you every step of the way.
Knock Out Parkinson's Symptoms with Boxing Classes
Fighting Back: The Power of Parkinson's Boxing Classes
Parkinson's boxing classes are specialized exercise programs that use non-contact boxing techniques to help manage and reduce symptoms of Parkinson's disease. These classes combine boxing fundamentals with exercises specifically designed to address Parkinson's symptoms.
What Are Parkinson's Boxing Classes? Key Benefits - Non-contact boxing exercises - Improved balance and coordination - Taught by specially trained instructors - Increased strength and mobility - Adapted for all stages of Parkinson's - Improved cognitive function - Available in-person and online - Reduced tremors and rigidity - Often offered through Rock Steady Boxing - Social support and community
When it comes to managing Parkinson's symptoms, traditional medications only address part of the challenge. Parkinson's boxing classes provide a complementary approach that targets multiple symptoms simultaneously through intense, "forced" exercise that may actually slow disease progression.
The concept is simple but powerful: by engaging in exercises that challenge balance, coordination, agility, and strength, people with Parkinson's can improve the very functions that the disease impairs. The boxing format creates an engaging, motivational environment where participants don't just exercise—they fight back against their condition.
"My first thought was this would be strictly an exercise class, but it turned out to be much more. The other people in the class became friends. Those friendships became as important to me as the exercise itself." - Dr. Sam T., Program Participant
What makes Parkinson's boxing classes particularly effective is their comprehensive approach. A typical class includes:
Stretching and warm-up exercises
Footwork and balance drills
Punching techniques on heavy bags
Voice exercises to address soft speech
Cognitive challenges through boxing combinations
Group activities for social engagement
Most importantly, these classes create a supportive community where participants—often called "fighters" or "boxers"—can share experiences, celebrate victories, and motivate each other.
I'm Lou Ezrick, a physical therapist with extensive experience helping patients with neurological conditions through specialized exercise programs including Parkinson's boxing classes that I've seen transform lives by combining targeted movement therapy with the powerful motivational elements of boxing training.
Parkinson's Boxing Classes: How They Work
At the heart of Parkinson's boxing classes is a thoughtfully structured approach that blends boxing basics with principles from neurological rehabilitation. These aren't your typical boxing classes—there's no competition or sparring. Instead, they use boxing movements to strengthen the vital connection between brain and body.
What Are Parkinson's Boxing Classes?
Parkinson's boxing classes are specialized group exercise programs designed with Parkinson's symptoms in mind. They use non-contact boxing techniques—meaning nobody gets hit. Participants work with punching bags, focus mitts, and other equipment in a supportive environment.
A typical class runs 60-90 minutes and flows through several key components. You'll start with gentle warm-ups to prepare your body, including stretching and joint mobility work. Voice activation is often incorporated, with participants counting punches aloud or shouting boxing commands—a clever way to address the soft voice many people with Parkinson's experience.
The heart of the class focuses on boxing fundamentals—proper stance, footwork, and basic punches like jabs, crosses, hooks, and uppercuts. You'll practice combinations on heavy bags to build strength, work with speed bags to improve coordination, and move through footwork patterns that improve balance and mobility.
What makes these classes special is the cognitive challenge built in. You might need to remember complex punch combinations while moving, engaging your brain and body simultaneously. Classes wrap up with a gentle cool-down to safely transition out of the workout.
Trained coaches lead these sessions with knowledge of both boxing techniques and Parkinson's management, making adjustments for different symptom levels and mobility challenges.
Parkinson's Boxing Classes vs. Traditional Fitness
What sets Parkinson's boxing classes apart from regular gym workouts? The difference is in the details and the design.
Feature Parkinson's Boxing Classes Traditional Fitness Classes Focus Symptom-specific exercises targeting balance, coordination, and neurological function General fitness, weight management, and cardiovascular health Intensity Higher intensity "forced exercise" shown to benefit neurological symptoms Variable intensity based on general fitness goals Instruction Coaches trained in Parkinson's management with understanding of symptom fluctuations General fitness instructors without specialized neurological training Adaptability Modified for all stages of Parkinson's with level-appropriate challenges Limited modifications for neurological conditions Community Shared experience with others facing similar challenges General fitness community without disease-specific support Cognitive Element Dual-task training combining movement with cognitive challenges Limited cognitive training components Voice Work Incorporates vocal exercises to address speech symptoms No vocal training component
The higher intensity of these classes is particularly important. Research suggests that "forced" exercise—pushing harder than you might naturally choose—may be especially beneficial for people with Parkinson's, potentially triggering protective mechanisms in the brain.
Parkinson's Boxing Classes & Rock Steady Boxing
When talking about Parkinson's boxing classes, Rock Steady Boxing (RSB) stands out as the pioneer that developed and popularized this approach. Founded in 2006 by Scott Newman after his early-onset Parkinson's diagnosis, RSB has grown into a global movement with over 900 affiliate locations worldwide.
Rock Steady Boxing thoughtfully organizes participants into four levels based on symptoms and fitness:
Level 1 serves those with minimal movement challenges who function independently, while Level 2 works for those with mild to moderate symptoms who remain mostly independent. Level 3 is designed for those with moderate symptoms who may use assistive devices, and Level 4 provides appropriate support for those with more advanced symptoms needing greater assistance.
This smart leveling system ensures everyone gets the right challenge with appropriate modifications. The core boxing elements remain consistent across levels, but coaches adjust intensity, complexity, and support as needed.
What makes Rock Steady Boxing particularly effective is its holistic approach to neuro-conditioning. Rather than focusing on just one aspect of fitness, it addresses multiple dimensions: cardiovascular conditioning through sustained boxing movements, strength training via resistance exercises, balance challenges through footwork, cognitive stimulation by learning combinations, and perhaps most importantly, social engagement through group activities and peer support.
At Evolve Physical Therapy + Sports Rehabilitation, we've witnessed remarkable changes through our Rock Steady Boxing program in Brooklyn. The combination of physical challenge, cognitive engagement, and community support creates a powerful formula for fighting back against Parkinson's symptoms. Learn more about the scientific research behind boxing for PD and why it's becoming such a popular approach.
Proven Benefits & Scientific Evidence
The rising popularity of Parkinson's boxing classes isn't just another fitness trend—it's backed by solid scientific research showing real results. The evidence keeps growing, and the improvements we see in our clients at Evolve Physical Therapy reflect what researchers are finding in clinical studies.
Key Studies on Boxing & Parkinson's
The science behind Parkinson's boxing classes is compelling. In one eye-opening study, researchers worked with 31 people with Parkinson's, dividing them between boxing training and traditional exercise groups. Both groups participated in 24-36 sessions over 12 weeks, with each session lasting 90 minutes. The results? Both approaches showed significant improvements across multiple measures, with boxing proving to be at least as effective as other evidence-based exercises. In fact, the only slight difference was in balance confidence, which marginally favored traditional exercise.
What's particularly encouraging is the staying power of these benefits. A follow-up trial tracked six participants through 12 weeks of boxing training (24-36 sessions). Every single person improved in at least five of the 12 outcome measures by the end of the program. Even better, when researchers checked back at 24 and 36 weeks, these improvements hadn't faded away—suggesting that boxing training offers lasting benefits.
The University of Texas Southwestern Medical Center has seen similar success with their Parkinson's Boxing Program. Their 12-week community boxing class participants showed noticeable improvements in functional strength, walking while doing other tasks, walking speed, backward walking, and dynamic balance.
These findings support what experts call the "forced-exercise theory"—the idea that pushing yourself harder than you naturally would (with the motivation of coaches and classmates) may actually trigger greater neurological benefits than exercising at your own pace. It's like having someone else turn up the dial on your workout's effectiveness!
Symptoms Most Improved
Not all Parkinson's symptoms respond equally to boxing training, but many show remarkable improvement. On the physical side, balance and stability often show dramatic gains—not surprising when you consider all that footwork and constant weight shifting. Tremors frequently decrease during the activity itself, as focused muscle engagement seems to temporarily override the tremor pattern.
Rigidity—that stiffness that makes movement difficult—tends to decrease as boxing movements encourage full range of motion. Many participants also report improved walking with less freezing and more confidence. And of course, all that work on the heavy bag translates to increased strength that helps with everyday activities.
Beyond the physical benefits, Parkinson's boxing classes address many non-motor symptoms too. Cognitive function gets a workout as participants learn combinations and respond to coaching cues. Mood improvement is nearly universal—partly from endorphins released during exercise and partly from the social connections formed in class.
For many, improvements in voice volume are a welcome surprise, as shouting numbers or boxing commands helps counteract the soft speech (hypophonia) common in Parkinson's. Participants often report better energy levels over time, and many find their sleep quality improves as well.
Real-Life Success Stories
The statistics are impressive, but the real magic of Parkinson's boxing classes shines through in personal stories.
Take Marc from the MAR-JCC Rock Steady Boxing program in North Miami Beach. At 79, this retired dentist started in a wheelchair, progressed to a walker, then to a cane. During one unforgettable session, he walked across the court unassisted for the first time. The entire class stopped what they were doing to cheer him on—a moment of triumph that energized everyone present.
Then there's Rosh, a 48-year-old former hospitalist diagnosed with Parkinson's who found such benefit in the classes that he became a certified coach. He now volunteers twice weekly, leading workouts while maintaining his own exercise regimen. As both participant and coach, he's a powerful inspiration to everyone in the program.
Ellen's story highlights how these classes address the emotional aspects of Parkinson's: "Rock Steady Boxing is the best gift I could ever have given myself," she shares. "It has taken me from a very dark, depressed place and lifted me to the final stage of grief – 'acceptance'." Her experience reminds us that healing happens on multiple levels.
Dr. Sam from the University of Texas Southwestern program finded an unexpected benefit: "My first thought was this would be strictly an exercise class, but it turned out to be much more. The other people in the class became friends. Those friendships became as important to me as the exercise itself."
The growth of the MAR-JCC program from about 40 to more than 150 boxers since August 2016 speaks volumes about both the effectiveness of the program and the power of word-of-mouth from satisfied participants. When something works this well, people talk about it!
At Evolve Physical Therapy, we've seen these same changes in our Brooklyn Rock Steady Boxing program—physical improvements paired with newfound confidence and community connections that make living with Parkinson's more manageable and more joyful.
Safety, Adaptations & Instructor Qualifications
While the benefits of Parkinson's boxing classes are substantial, safety remains paramount. These programs incorporate numerous safeguards and adaptations to ensure participants can exercise effectively without undue risk.
Are Parkinson's Boxing Classes Safe?
When people first hear about Parkinson's boxing classes, they often wonder about safety. Rest assured, these programs are designed with safety as their foundation.
First and foremost, these are completely non-contact classes. Nobody is getting punched or punching another person! All boxing activities happen with equipment like heavy bags, speed bags, and focus mitts. Before joining, most programs require participants to get a thumbs-up from their doctor, ensuring the program matches their health needs.
In quality programs, you'll notice a low ratio of participants to coaches. This isn't by accident—it ensures everyone gets proper attention and supervision. Many programs, like the one at UT Southwestern, even bring in trained volunteers (often enthusiastic physical therapy students) who stand ready to prevent falls and offer support when needed.
"Safety first" isn't just a slogan in Parkinson's boxing classes—it's built into everything from the equipment to the environment. Training spaces feature clear pathways, supportive rails where needed, and non-slip flooring. Coaches are trained to spot signs of fatigue or medication wearing off, making adjustments on the fly to keep everyone safe.
While these classes do involve energetic exercise, the structured environment and specialized training create a space where participants can safely push their limits and see real improvement.
Adapting for Every Stage of PD
One of the beautiful things about Parkinson's boxing classes is how they meet each person exactly where they are in their journey. Programs like Rock Steady Boxing group participants into levels based on symptoms and function, ensuring everyone gets the right balance of challenge and support.
For those in early stages (Levels 1-2), classes might include standard boxing stance and footwork, full punching bag workouts, and complex combinations that challenge both body and mind. The focus is on prevention and maintaining function through challenging exercise.
As symptoms progress to moderate stages (Level 3), coaches might modify the stance for better stability, keep a chair nearby for quick rest breaks, or simplify punch combinations. The core boxing elements remain, but with thoughtful adjustments that keep the workout effective and safe.
For those with more advanced symptoms (Level 4), options expand to include chair boxing for seated participants, care partner assistance during sessions, and a greater focus on range of motion and strength. Sometimes resistance bands replace heavy bags, offering gentler resistance while maintaining the boxing framework.
Across all levels, coaches use sensory cues like visual targets, rhythmic counting, and beat-driven music to help overcome movement initiation difficulties—a common Parkinson's challenge. Classes are often scheduled to align with participants' medication timing, ensuring everyone can participate during their "on" periods when symptoms are better controlled.
At Evolve Physical Therapy + Sports Rehabilitation, we pay close attention to each boxer's unique needs, making real-time adjustments to keep the workout challenging but manageable for everyone in the room.
Who Can Teach Parkinson's Boxing Classes?
Behind every effective Parkinson's boxing class stands a well-trained instructor. Programs like Rock Steady Boxing have developed comprehensive certification systems that ensure quality and safety across their global network.
The instructor hierarchy starts with Head Coaches who complete extensive training—10 hours online plus a two-day in-person training camp. These individuals typically come from fitness, physical therapy, or exercise science backgrounds and hold nationally-recognized fitness certifications. They're the primary instructors who lead classes and oversee program safety.
Supporting the Head Coach are Coaches (10 hours of online training) and Assistant Coaches (3 hours of training), who provide additional eyes, hands, and encouragement during classes. Many Assistant Coaches are volunteers or family members who want to contribute to the program's success.
For healthcare professionals, there's a Clinician track—physical therapists, occupational therapists, and other medical professionals complete 8 hours of online training plus a two-day clinical application course. These specialists often weave boxing techniques into one-on-one therapy sessions or serve as medical advisors to boxing programs.
What really makes a great Parkinson's boxing instructor goes beyond certifications. The best instructors combine deep knowledge of Parkinson's symptoms with genuine compassion and sharp observation skills. They communicate clearly and loudly (essential for participants with hearing challenges), modify exercises on the fly, and know exactly when to push and when to pull back.
All certified instructors must recertify every two years, staying current with evolving research and best practices. This commitment to ongoing education ensures Parkinson's boxing classes continue to improve based on the latest evidence.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, our Rock Steady Boxing program is led by instructors who bring both professional expertise and personal warmth to every class. Their specialized training in Parkinson's management creates a safe, effective environment where participants can truly "fight back" against their symptoms. Learn more about our Rock Steady Boxing Brooklyn NYC program and how it might benefit you or your loved one.
Finding & Choosing a Parkinson's Boxing Program
With Parkinson's boxing classes becoming increasingly popular, you'll find more options available both locally and online. Finding the right program isn't just about location—it's about finding a good match for your specific needs, symptoms, and goals.
Using "Find a Class" Tools
Looking for Parkinson's boxing classes near you? You're in luck—several easy-to-use resources can help you locate programs in your area.
The official Rock Steady Boxing website offers a comprehensive "Find a Class" tool that connects you with their nearest affiliate program. With over 900 locations worldwide, chances are good you'll find one nearby. Their global network ensures consistent quality and approach, regardless of location.
The Parkinson's Foundation also maintains an excellent resource directory that includes specialized exercise programs. This directory often includes both RSB affiliates and other boxing-inspired programs developed specifically for the Parkinson's community.
Don't forget to check with local hospitals and rehabilitation centers. Many medical facilities now recognize the benefits of Parkinson's boxing classes and have developed their own programs or partnerships with existing ones. A quick call to your local neurology department might reveal options you didn't know existed.
Local Parkinson's support groups are another goldmine of information. Members often share first-hand experiences with different programs and can provide honest feedback about what worked for them. These personal recommendations can be invaluable in making your decision.
Many YMCAs and community centers have also partnered with Parkinson's-specific programs, offering classes in convenient, accessible locations throughout the community.
Here in Brooklyn and surrounding areas, we at Evolve Physical Therapy + Sports Rehabilitation offer Rock Steady Boxing classes serving the communities of Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin.
What to Ask Before Enrolling
Before committing to a Parkinson's boxing class, it's worth doing a bit of homework. The right questions can help you determine if a program is the right fit for your needs.
Start by asking about the program itself: Is it an official Rock Steady Boxing affiliate or another type of program? How long has it been operating? A well-established program with a track record of success can provide added confidence. Ask about typical class sizes too—smaller groups generally mean more individual attention.
The instructors' qualifications are crucial. What specific training do they have in Parkinson's disease? Beyond boxing skills, do they understand the unique challenges of Parkinson's? A good instructor-to-participant ratio is essential for safety and personalized guidance, so don't hesitate to ask about this.
Practical matters matter too. What are the costs involved, and are there scholarship options available? Some programs offer financial assistance for those who need it. Ask what equipment is provided and what you'll need to bring yourself. Is the facility fully accessible for those with mobility challenges? And importantly, when are classes scheduled? Timing classes to align with your medication cycle can make a big difference in your ability to participate fully.
Safety should be a top priority. Ask how progress is tracked and measured, what safety protocols are in place for falls or emergencies, and whether care partners can attend if needed. A good program will have thoughtful answers to all these questions.
Many programs offer trial classes or observation options, which can be extremely helpful in determining if the environment and approach are right for you. Don't be shy about asking to try before you commit.
For more information about specialized Parkinson's physical therapy options in Brooklyn, visit Evolve's Parkinson's Physical Therapy page.
Parkinson's Boxing Classes Online
Can't make it to an in-person class? Online Parkinson's boxing classes have become a game-changer for many people, especially those in rural areas or with transportation challenges.
These virtual options come in several formats. Live-streamed classes offer real-time interaction where instructors can see you and provide feedback, creating an experience similar to being in the gym. Pre-recorded workouts offer flexibility, allowing you to exercise whenever works best with your medication schedule and energy levels.
Some programs take a hybrid approach, combining periodic in-person assessments with regular online sessions. This gives you the benefits of professional in-person evaluation while maintaining the convenience of home-based exercise. For those wanting more personalized attention, tele-coaching provides one-on-one virtual sessions with a certified instructor who can tailor the workout to your specific needs.
The benefits of online classes extend beyond convenience. They allow you to exercise in a familiar environment with whatever supports you need already in place. There's no exhausting travel before or after your workout. You can progress at your own pace without feeling self-conscious, and you can participate regardless of where you live.
If you're considering an online option, make sure you have adequate space—about 6' x 6' minimum—for safe movement. Set up in an area free of fall hazards, with sturdy support nearby if needed. Many participants find it helpful to have a care partner present, especially if balance is a concern. Use a device with a screen large enough to clearly see demonstrations, and test your technology before the first session to avoid frustration.
Many programs, including several Rock Steady Boxing affiliates, now offer virtual options alongside their in-person classes. This expanded accessibility has been a silver lining of recent years, bringing Parkinson's boxing classes to people who previously couldn't access them.
DIY Checklist for First Class
Your first Parkinson's boxing class can feel a bit intimidating, but being prepared will help you feel more confident and get the most from your experience.
What to bring: Pack comfortable, breathable clothing (layers work best as you'll warm up during exercise) and supportive athletic shoes with good traction. Don't forget a water bottle—hydration is essential during this type of workout. It's wise to bring your regular medications in case class runs through a dosing time, and always wear or carry medical identification.
Some programs provide boxing gloves, while others recommend purchasing your own. The same goes for hand wraps, which go under gloves for wrist support and hygiene. Check with your program about their specific equipment policies before your first class.
Preparation extends beyond packing your bag. Try to eat lightly 1-2 hours before class—you'll want some fuel but not a heavy meal. If possible, schedule class during your medication "on" time when symptoms are better controlled. Make sure you're well-rested the night before, as fatigue can exacerbate symptoms.
Consider keeping a simple symptom journal noting how you feel before and after class. This can help you track benefits over time and provide valuable information to both you and your healthcare team.
Mental preparation is just as important as physical preparation. Set realistic expectations—understand that skills develop over time, and your first class is just the beginning of your journey. Try to adopt what many programs call a "fighter's mindset"—approaching class as an opportunity to actively fight back against Parkinson's rather than passively experiencing symptoms.
Be open to the social aspects of the program too. The community that forms in Parkinson's boxing classes often becomes an essential source of support, understanding, and motivation. And don't hesitate to communicate your needs or limitations to instructors—they're there to help you succeed.
Everyone starts somewhere. These classes are designed to welcome newcomers regardless of prior boxing or fitness experience. Your fellow classmates have all been where you are now, taking that brave first step toward fighting back against Parkinson's.
For more information about Rock Steady Boxing classes in Brooklyn, visit Rock Steady Boxing Brooklyn NYC.
Frequently Asked Questions about Parkinson's Boxing Classes
What if I've never boxed before?
Don't worry! The vast majority of people who join Parkinson's boxing classes have never stepped into a boxing ring before. These programs are specifically designed with beginners in mind.
When you first arrive, you'll find instructors who understand you're starting from scratch. They'll patiently break down each movement into manageable steps, demonstrate proper form, and provide plenty of repetition so you can build confidence gradually.
These classes aren't about becoming the next heavyweight champion. The focus is on using boxing-inspired movements to address your specific Parkinson's symptoms. Everyone learns at their own pace in an environment where others are facing similar challenges. Many participants find that the learning process itself—figuring out new movements and combinations—provides valuable cognitive stimulation alongside the physical benefits.
As one participant shared, "I was intimidated at first because I'd never thrown a punch in my life, but by the end of my first class, I was jabbing and crossing like I'd been doing it for weeks!"
Can boxing slow Parkinson's progression?
This is perhaps the most hopeful question people ask about Parkinson's boxing classes. While we can't claim that any exercise can stop Parkinson's disease completely, there's growing scientific evidence suggesting that intense exercise like boxing may actually slow symptom progression.
The concept of "neuroprotection" through vigorous exercise is gaining substantial support in the research community. Several mechanisms might explain why boxing seems particularly effective:
First, the intense cardiovascular workout increases blood flow to the brain, potentially supporting neuronal health and function. Second, this type of exercise stimulates production of brain-derived neurotrophic factor (BDNF)—think of it as fertilizer for your brain cells that helps them survive and thrive. Third, the complex movements in boxing promote neuroplasticity, helping your brain form new neural connections that may compensate for those damaged by Parkinson's. Finally, regular exercise has anti-inflammatory effects that might help slow disease processes.
Many neurologists now actively prescribe intensive exercise like Parkinson's boxing classes as a core component of managing the disease and potentially slowing its progression. As one doctor put it, "Medicine helps manage symptoms, but exercise might actually change the disease course."
How often should I attend Parkinson's boxing classes?
Finding your ideal schedule for Parkinson's boxing classes depends on your individual situation, but research consistently shows that more frequent participation yields better results. Most programs recommend attending 2-3 classes per week for maximum benefit.
Consistency truly is the key to success here. Many of our participants report that their symptoms become noticeably more manageable when they maintain a regular exercise schedule. The benefits seem to build upon themselves—what researchers call "cumulative effects"—in ways that occasional participation simply cannot match.
If attending multiple weekly classes isn't feasible for you, don't worry. Supplementing with home exercises or other forms of Parkinson's-specific activity on non-boxing days can help maintain your progress. Your instructor can recommend complementary exercises that reinforce the skills you're developing in class.
As with any exercise program, it's important to listen to your body and avoid pushing too hard too fast. Some people find success starting with just one class per week and gradually increasing as their stamina improves. One of our participants at Evolve Physical Therapy + Sports Rehabilitation started with a single weekly class and now attends three times weekly, noting, "I schedule my entire week around my boxing classes because they make such a difference in how I feel and move."
Consistency trumps intensity—showing up regularly, even on days when symptoms are challenging, often yields the greatest long-term benefits for managing your Parkinson's symptoms.
Conclusion
The journey through Parkinson's boxing classes reveals much more than just an exercise program—it represents a powerful way to reclaim control in the face of a challenging condition. These classes stand out as one of the most innovative approaches to managing Parkinson's symptoms, offering a comprehensive strategy that works on multiple levels simultaneously.
When you step into a boxing class designed for Parkinson's, you're not just working your muscles—you're challenging your brain, strengthening your voice, and connecting with others who truly understand your experience. The research backs what participants have been saying for years: these programs lead to real improvements in balance, mobility, strength, and cognitive function.
But perhaps the most profound benefit goes beyond what can be measured in a clinical study. There's something deeply empowering about putting on boxing gloves and literally fighting back against your condition. As one boxer shared, "For the first time since my diagnosis, I felt like I was doing something to Parkinson's instead of Parkinson's doing something to me."
The community that forms in these classes creates a support system unlike any other. People who arrive as strangers quickly become teammates and friends, celebrating each other's victories and providing encouragement through challenges. The emotional benefit of this connection can be just as important as the physical exercise itself.
At Evolve Physical Therapy + Sports Rehabilitation, we've witnessed these changes through our Rock Steady Boxing program in Park Slope. Our team combines physical therapy expertise with specialized boxing training to create an environment where people with Parkinson's can safely push their limits and experience breakthroughs.
Whether you're newly diagnosed or have been living with Parkinson's for years, Parkinson's boxing classes offer a path forward that focuses on what you can do rather than what you can't. The program meets you where you are today while helping you build strength for tomorrow.
Are you ready to lace up your gloves and start fighting back? Contact us to learn more about our Rock Steady Boxing program in Brooklyn and take that first powerful step toward knocking out Parkinson's symptoms.
How to Find TMJ Massage Therapy Relief in 5 Easy Steps
Why TMJ Massage Therapy is Your Gateway to Pain-Free Living
TMJ massage therapy can provide significant relief for jaw pain, headaches, and muscle tension through targeted techniques that address the root causes of temporomandibular joint dysfunction. Here's what you need to know:
Quick TMJ Massage Therapy Relief Options:
• Self-massage techniques - Masseter kneading, friction massage, and gentle stretching (30-60 seconds per area)
• Professional therapy - Intraoral work, trigger point release, myofascial techniques
• Complementary approaches - Heat/cold therapy, breathing exercises, posture correction
• Frequency - Daily self-massage + weekly professional sessions for optimal results
TMJ disorders affect over 10 million Americans, with research showing that 20-40% of adults experience some form of jaw dysfunction. The good news? Multiple studies have proven that massage therapy ranks as one of the most effective self-care strategies for TMJ pain relief.
"In a 2003 survey of 192 TMJ patients, massage was rated as the most common and one of the most helpful complementary and alternative therapies."
Whether you're dealing with jaw clicking, morning headaches, or that familiar jaw tension from stress and teeth grinding, the right massage approach can break the pain cycle and restore normal function.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience treating complex musculoskeletal conditions, including chronic TMJ massage therapy cases at Evolve Physical Therapy in Brooklyn. My hands-on approach combines manual therapy techniques with patient education to address both symptoms and underlying causes of jaw dysfunction.
Step 1: Know Your TMJ Disorder Inside Out
Think of your temporomandibular joint as the hardest-working hinge in your body. This small but mighty joint connects your jawbone to your skull and gets a workout every time you talk, chew, yawn, or even smile. When something goes wrong with this intricate system, the effects can ripple throughout your entire head and neck.
Understanding your specific TMJ symptoms is crucial before starting any TMJ massage therapy routine. You wouldn't try to fix a car without knowing what's under the hood, right? The same principle applies to your jaw.
The telltale signs of TMJ dysfunction often start subtly. You might notice jaw pain or tenderness when you're chewing your morning toast or talking on a long phone call. Many people experience clicking, popping, or grating sounds when they open their mouth—it's like your jaw is trying to tell you something important.
One simple test you can do right now: try to fit three fingers vertically between your upper and lower teeth when your mouth is open. If you can't, you may have limited mouth opening, which is a common TMJ symptom.
Morning headaches are another red flag, especially if you wake up feeling like you've been hit by a truck. Your jaw muscles have been working overtime while you sleep, and that tension travels upward. Ear pain, fullness, or ringing might make you think you have an ear infection, but often it's your TMJ acting up.
The domino effect continues with neck and shoulder tension, facial aching, and even difficulty chewing or a sudden change in how your bite feels. It's amazing how one small joint can cause such widespread chaos.
Bruxism—teeth grinding or clenching—is the biggest troublemaker when it comes to TMJ problems. Many people grind their teeth during sleep or when stressed, often without realizing it. Your poor jaw muscles are essentially doing an all-night workout they never signed up for.
Other culprits include arthritis affecting the joint, jaw injury or trauma (even something that happened years ago), and genetic factors that affect how your jaw is structured. Chronic stress and poor posture from hunching over computers all day don't help either—your neck and jaw are more connected than you might think.
Here's something that might surprise you: research shows that 20-40% of adults experience some degree of TMJ dysfunction. You're definitely not alone in this struggle. Women tend to be affected more frequently than men, particularly during reproductive years when hormonal changes can influence joint and muscle function.
Red-Flag Symptoms That Need a Pro
While TMJ massage therapy is generally safe and wonderfully effective, some symptoms wave a big red flag that says "get professional help now." Think of these as your jaw's emergency signals.
Jaw locking is the most serious warning sign. If you suddenly can't open or close your mouth properly, this isn't the time for DIY solutions. Severe swelling around your jaw joint or fever accompanying jaw pain could indicate infection or other serious conditions that need immediate medical attention.
If you've had recent trauma to your head, neck, or jaw—maybe from a car accident, sports injury, or even a dental procedure—professional evaluation should come before massage. Sudden onset of severe symptoms or numbness in your face or jaw area are also situations where it's better to be safe than sorry.
The good news? Most TMJ cases don't involve these red-flag symptoms and respond beautifully to the right massage techniques. But when in doubt, getting a professional opinion first is always the smartest move.
Step 2: Prepare Safely for TMJ Massage
Think of preparing for TMJ massage therapy like setting up for a cooking project—having everything ready makes the whole process smoother and safer. At Evolve Physical Therapy, we've learned that a few minutes of prep work can make the difference between a helpful session and one that leaves you feeling worse.
Let's start with the non-negotiables. If you have an active infection in your jaw or facial area, recent jaw dislocation, or acute inflammation with significant swelling, hold off on massage until these issues resolve. The same goes if you've had recent oral surgery or dental work—give your tissues time to heal first.
For those with a latex allergy, skip the gloves during any intraoral work, or find latex-free alternatives. And if you have blood clotting disorders, check with your healthcare provider before starting any massage routine.
Now for the fun part—getting ready for your session. Hygiene comes first: wash your hands thoroughly and trim those nails. Nobody wants a scratchy massage, especially around sensitive jaw muscles. Grab a clean towel, some disposable gloves if you're planning intraoral work, and set a timer so you don't overdo it.
Create a calm environment where you can focus. Dim the lights, find a comfortable chair, and put your phone on silent. This isn't just about relaxation—it's about tuning into your body so you can feel what's happening during the massage.
Before you start, rate your pain on a scale of 1 to 10. This simple step helps you track whether the massage is actually helping. Then spend a minute on relaxation breathing: breathe in for 4 counts, out for 6 counts, and repeat this 5 times. This activates your body's relaxation response and helps tight muscles release more easily.
Self-Assessment Checklist Before TMJ Massage Therapy
Every TMJ massage therapy session should start with a quick check-in with your jaw. Think of it as taking your jaw's temperature—you want to know what you're working with before you dive in.
Start with a range of motion test. Open your mouth as wide as feels comfortable and notice how far it goes. Normal opening is about 35-50mm—roughly the width of three fingers stacked vertically. Does your jaw deviate to one side as you open? Any pain or restriction? Mental note taken.
Next, do a gentle muscle tension check. Lightly clench your jaw and feel for tight spots in the masseter muscles—those thick muscles you can feel when you bite down. Press gently along your jawline to identify tender areas. Notice if one side feels different from the other.
Finally, take a moment for a posture scan. Is your head sitting forward of your shoulders? Are your shoulders hiked up toward your ears? Is your tongue resting comfortably on the roof of your mouth? These details matter because jaw tension rarely exists in isolation.
This baseline assessment becomes your roadmap for the massage session ahead. It tells you which areas need attention and helps you track improvement over time. Plus, it only takes about two minutes—time well spent for better results.
Step 3: Master 3 Core TMJ Massage Therapy Techniques
Here's where the magic happens. After years of helping patients at Evolve Physical Therapy, I've found that mastering just three core techniques can dramatically reduce TMJ pain and restore normal jaw function. These aren't complicated moves—think of them as your new best friends for jaw relief.
The beauty of TMJ massage therapy lies in its simplicity. You don't need fancy equipment or years of training. What you do need is the right technique, proper pressure, and a little patience with yourself as you learn.
Masseter kneading is your go-to starting technique. This thick muscle on the side of your jaw does most of the heavy lifting when you chew, which means it often holds the most tension. Place two or three fingertips on your cheek, right above your jawline where you can feel the muscle bulk up when you clench. Now make small, slow circles with gentle but firm pressure—imagine you're kneading tiny pieces of dough. Work your way from the back corner of your jaw toward your cheekbone, spending a full 30 to 60 seconds on each side.
Friction massage targets those stubborn knots that feel like tiny marbles under your skin. These trigger points are like reset buttons for your jaw muscles. When you find a tender spot during your gentle exploration along the jawline, place your index finger there and apply steady pressure. Hold it for 15 to 30 seconds—you might feel the muscle gradually soften under your finger. It's normal to feel some discomfort, but it should be the "good hurt" kind, not sharp or stabbing pain.
The third technique, stretching massage, combines the best of both worlds. Place both thumbs under your jawline and apply gentle upward pressure while slowly opening your mouth. This lengthens tight muscles while improving your range of motion. Hold for 5 to 10 seconds, then slowly close your mouth and repeat the process 5 to 10 times.
Here's a game-changer that many people overlook: diaphragmatic breathing during massage. Before starting each technique, place one hand on your chest and one on your belly. Breathe slowly and deeply so that only your bottom hand moves. This simple addition activates your body's relaxation response and makes the massage much more effective.
How to Perform TMJ Massage Therapy at Home
More info about TMJ Self Massage
Creating a routine takes the guesswork out of TMJ massage therapy and ensures you're getting consistent results. Think of this as your personal spa time—you deserve these few minutes of self-care.
Start with 2 to 3 minutes of preparation. Find a comfortable chair with good back support, then take five deep diaphragmatic breaths to center yourself. A warm compress on your jaw for a couple of minutes helps relax the muscles before you begin—like warming up before exercise.
Your main massage sequence should take 8 to 10 minutes. Begin with masseter kneading for a full minute on each side. Then move to your temples for temporalis massage—place your fingertips there and use the same gentle circular motions for 30 seconds per side. Follow this with trigger point work on any tender spots you finded during your assessment, holding each point for 15 to 30 seconds. Finish with 10 repetitions of the stretching massage technique.
The cool-down phase is just as important as the massage itself. Spend 2 minutes doing gentle jaw movements—open and close your mouth, then move it slowly from side to side. End with some relaxation breathing and take a moment to rate your pain level. You'll be surprised how satisfying it is to notice the improvement.
For frequency, think of daily self-massage as brushing your teeth—it's basic maintenance for your jaw health. During flare-ups, you can safely increase to 2 or 3 times daily. The golden rule is simple: always stop if your pain increases rather than decreases.
TMJ Massage Therapy Troubleshooting Tips
Even with perfect technique, you might hit some bumps along the way. Let's address the most common concerns I hear from patients.
Mild soreness for 24 to 48 hours after massage is completely normal, especially when you're just starting out. Think of it like the day after a good workout—your muscles are adjusting to the new attention. However, if you experience increased pain or swelling, you're probably applying too much pressure. Dial it back and try applying ice for 10 to 15 minutes to calm things down.
If you're not feeling relief, don't give up just yet. Check your pressure first—many people start too gently and don't get deep enough into the muscle, while others go too hard too fast. The sweet spot feels like the pressure you'd use to check if a peach is ripe. Also make sure you're hitting the right muscles—the masseter and temporalis are your main targets.
Sometimes warming the muscles with a heat pack before massage makes all the difference. And remember, some TMJ cases are more complex and truly benefit from professional intervention. There's no shame in getting help when you need it.
Hydration plays a bigger role than most people realize. Dehydrated muscles are harder to massage and don't respond as well to treatment. Drink plenty of water before and after your massage sessions—your jaw muscles will thank you.
Step 4: Blend Professional Care with Home Practice
Here's the truth about TMJ massage therapy: while your home routine is incredibly valuable, the magic really happens when you combine it with professional care. Think of it like learning to play piano—you can practice scales at home, but you need a skilled teacher to help you master the complex pieces.
A 2007 survey of 126 TMJ patients ranked massage as one of the most effective self-care strategies, but here's what that study also revealed: patients who combined professional treatment with home practice saw dramatically better results than those who went solo.
Why professional TMJ massage therapy makes such a difference comes down to access and expertise. There are muscles deep inside your mouth—like the pterygoid muscles—that you simply can't reach safely on your own. These muscles are often major players in TMJ dysfunction, but they require specialized training to treat effectively.
Professional therapists also bring a trained eye to spot things you might miss. That shoulder tension you've gotten used to? It could be contributing to your jaw pain. The way you breathe when you're stressed? That's affecting your jaw muscles too. We look at the whole picture, not just the obvious spots that hurt.
Recent research from 2021 backs this up, showing that conservative manual techniques of physical therapy, including massage, provide significant improvements in both pain relief and jaw mobility. The scientific research on manual therapy outcomes demonstrates measurable improvements that patients can feel in their daily lives.
Most patients find success with this frequency approach: starting with 2-3 sessions per week for the first month, then scaling back to weekly or bi-weekly maintenance sessions. Meanwhile, you keep up your daily self-massage routine between visits. It's like having a personal trainer—they push you further than you'd go alone, then you maintain the gains with homework.
The insurance piece is worth mentioning too. Many insurance plans cover physical therapy for TMJ dysfunction, making professional care more accessible than you might expect.
Choosing a TMJ Massage Therapy Specialist
More info about TMJ Pain Providers
Not all massage therapists know how to work with TMJ disorders—and honestly, that's okay. TMJ work requires specific training in jaw anatomy and specialized techniques. You want someone who treats TMJ patients regularly, not someone who's willing to give it a try.
The key qualifications to look for include licensing as either a massage therapist or physical therapist, plus specific training in TMJ and cranial techniques. If you need intraoral work (massage inside the mouth), make sure they're trained and certified for that—it's a specialized skill that requires additional education.
When you're interviewing potential providers, ask direct questions. How many TMJ patients do they see each week? What's their specific approach to treatment? Do they work with other healthcare providers like dentists when needed? A good TMJ specialist should have clear, confident answers to these questions.
Trust your gut during that first consultation. You should feel heard and understood. TMJ dysfunction affects so many aspects of daily life—eating, talking, sleeping—and your provider should appreciate that reality. If someone promises to "cure" your TMJ in one session or seems to minimize your symptoms, keep looking.
At Evolve Physical Therapy, we've found that spending quality time with each patient makes all the difference. Our hands-on approach means we're actually working with you, not just giving you a list of exercises and sending you on your way. That personal attention helps us catch the subtle patterns that contribute to TMJ dysfunction.
TMJ Massage Therapy vs. Other Options
Treatment Option Effectiveness Side Effects Cost Invasiveness TMJ Massage Therapy High for muscle-related TMJ Minimal (mild soreness) Moderate Non-invasive Dental Splints Moderate to High Tooth movement, jaw soreness High Minimally invasive Anti-inflammatory Meds Moderate (temporary) GI issues, liver concerns Low to Moderate Non-invasive Botox Injections Moderate Weakness, difficulty chewing High Minimally invasive Surgery Variable Significant risks Very High Highly invasive
TMJ massage therapy has a unique advantage over other treatment options: it actually improves how your muscles and joints function, rather than just masking the problem. Anti-inflammatory medications can provide temporary relief, but they don't address the underlying muscle tension and movement patterns causing your pain.
Dental splints work well for many people, especially if teeth grinding is a major factor. But they're expensive, and some patients find them uncomfortable or worry about long-term effects on tooth position. TMJ massage therapy complements splint therapy beautifully—the massage addresses the muscle tension while the splint protects your teeth.
The really invasive options like surgery should be last resorts. The beauty of massage therapy is that it's completely reversible. If it doesn't help (which is rare), you haven't lost anything. If it does help—which research suggests it will—you've gained a skill you can use for life.
Most patients find that TMJ massage therapy gives them a sense of control over their condition. Instead of feeling helpless when symptoms flare up, you have tools you can use immediately. That psychological benefit is just as important as the physical relief.
Step 5: Add Exercises & Lifestyle Hacks for Lasting Relief
Here's the truth about TMJ massage therapy—it's incredibly effective, but it works best when you think bigger picture. Massage addresses the immediate muscle tension and pain, but lasting relief comes from combining it with targeted exercises and smart lifestyle changes that prevent the problem from coming back.
Think of it like this: massage is your rescue tool when things flare up, while exercises and lifestyle modifications are your insurance policy against future problems.
Building Strength and Mobility
Your jaw muscles need both flexibility and strength to function properly. Chin tucks are one of the most powerful exercises we teach at Evolve Physical Therapy because they directly address the forward head posture that contributes to TMJ dysfunction. Stand against a wall with your head touching, then draw your chin back like you're making a double chin. Hold for 3-5 seconds and repeat 10 times. It might feel silly, but this simple movement can dramatically reduce jaw strain.
Jaw mobility drills keep your joint moving smoothly. Start with relaxed jaw opening—touch your tongue to the roof of your mouth, then slowly open and close your jaw 10 times. Follow this with gentle side-to-side movements and forward-backward motions. These aren't dramatic movements; we're talking small, controlled motions that maintain healthy joint function.
Resisted opening exercises strengthen the muscles that oppose your powerful closing muscles (which tend to be overactive in TMJ patients). Place your thumb under your chin and open your mouth against gentle resistance. Hold for 3-5 seconds and repeat 10 times. This helps restore balance to your jaw system.
Heat and Cold: Your New Best Friends
Temperature therapy perfectly complements your TMJ massage therapy routine. Apply heat for 10-15 minutes before massage to relax tight muscles and improve blood flow. If you experience soreness after massage, cold therapy for 10 minutes can reduce inflammation. For chronic tension, try contrast therapy—alternate 3 minutes of heat with 1 minute of cold, repeating this cycle 3 times.
Expanding Your Toolkit
More info about TMJ Trigger Points
Myofascial release tools can extend your treatment beyond what your hands can reach. Small, firm trigger point balls help you address neck and shoulder trigger points that often contribute to jaw problems. A Theracane allows you to reach those stubborn upper back knots that your fingers can't quite access. Don't forget about foam rolling for your shoulders and upper back—remember, TMJ dysfunction rarely exists in isolation.
Stress reduction deserves special attention because emotional stress directly translates to physical tension in your jaw. Regular meditation, yoga, or even simple diaphragm breathing exercises can significantly reduce the unconscious clenching that happens throughout the day.
Whole-Body Habits that Protect Your TMJ
Your jaw doesn't exist in a vacuum—it's connected to your entire body through a complex web of muscles, nerves, and fascia. That's why we take a whole-body approach at Evolve Physical Therapy.
Sleep position matters more than you might think. Sleeping on your back maintains proper neck alignment and reduces strain on your jaw. If you're a side sleeper, make sure your pillow properly supports your neck without tilting your head up or down. Stomach sleeping is the worst position for TMJ—it forces your neck into rotation and can strain your jaw all night long.
Screen ergonomics have become crucial in our digital world. Position your computer monitor at eye level so you're not constantly looking down or craning your neck forward. Take movement breaks every 30 minutes, and never cradle your phone between your ear and shoulder—this creates massive tension in the exact muscles that contribute to TMJ dysfunction.
Anti-inflammatory nutrition supports healing from the inside out. Focus on omega-3 rich foods like fish, walnuts, and flax seeds, while emphasizing colorful fruits and vegetables for their antioxidant properties. Limit processed foods and excess sugar, which can increase inflammation throughout your body. And here's something simple but important—stay well-hydrated. Dehydration can increase muscle tension and make your massage therapy less effective.
The beauty of this comprehensive approach is that each element supports the others. Your TMJ massage therapy works better when your posture is improved, your stress is managed, and your muscles are properly conditioned. It's not about perfection—it's about creating a sustainable routine that keeps you pain-free and functional for the long haul.
Frequently Asked Questions about TMJ Massage Therapy
Can TMJ massage therapy help with headaches and neck pain?
This is one of the most common questions we hear at our Brooklyn clinic, and the answer is a resounding yes! Here's the thing about TMJ massage therapy—your jaw muscles don't exist in isolation. They're part of an interconnected web that includes your neck, shoulders, and even the muscles around your ears.
When your jaw muscles are tight or develop trigger points, they can create what we call referred pain. This means the pain shows up in places you might not expect. Those morning headaches that feel like a tight band around your temples? Often, they're actually coming from overworked jaw muscles.
Research from 2009 showed that massaging the lateral pterygoid muscle (one of the deeper jaw muscles) helped reduce both jaw clicking and headache symptoms. At Evolve Physical Therapy, we see this connection play out daily. Patients come in complaining about neck stiffness that won't budge, only to find their jaw tension is the real culprit.
The muscles of mastication—your chewing muscles—have extensive connections throughout your head and neck. When we address jaw tension through TMJ massage therapy, patients often experience relief from tension headaches, shoulder tightness, and even that annoying ear pain that seems to come from nowhere.
How often should I book sessions or self-massage?
The frequency question really depends on where you are in your healing journey. Think of it like learning a new skill—you need more practice at the beginning, then you can maintain your progress with less frequent sessions.
For professional TMJ massage therapy sessions, we typically recommend starting with 2-3 visits per week during the acute phase when symptoms are most bothersome. This usually lasts about 2-4 weeks. Once you start feeling better, we space sessions to once weekly for 4-6 weeks. After that, most patients do well with maintenance sessions every 2-4 weeks.
Self-massage is a different story—this should become part of your daily routine. We recommend 5-10 minutes of gentle techniques every day for maintenance. During flare-ups, you can increase this to 2-3 shorter sessions throughout the day. The key word here is gentle—your jaw muscles respond much better to consistent, light pressure than occasional intense sessions.
I always tell my patients that consistency beats intensity every time. It's better to do a little bit every day than to skip several days and then try to make up for it with one long session.
When should I see a healthcare professional instead of DIY?
While we're big believers in self-care and patient empowerment, there are definitely times when professional help isn't just recommended—it's necessary.
Seek immediate care if you experience jaw locking (you literally can't open or close your mouth), severe pain that doesn't respond to gentle measures, or any signs of infection like fever, significant swelling, or warmth around the joint. If you've had recent trauma to your head or jaw, or if symptoms come on suddenly and severely, don't wait—get evaluated right away.
There are also situations where professional guidance can save you weeks of frustration. If you've been consistent with TMJ massage therapy self-care for 2-3 weeks without any improvement, it's time to bring in reinforcements. Sometimes symptoms actually get worse despite your best efforts, which usually means there's something else going on that needs professional assessment.
At Evolve Physical Therapy, we often see patients who've been struggling with DIY approaches for months. Our comprehensive evaluation can identify contributing factors you might not think to look for—things like breathing pattern dysfunction, postural imbalances, or even how your sleeping position might be affecting your jaw.
If you have a history of jaw dislocation or simply feel uncertain about proper technique, professional guidance can give you the confidence and skills to manage your condition effectively. There's no shame in asking for help—sometimes a fresh pair of trained eyes can spot exactly what's been missing from your self-care routine.
Conclusion
You now have everything you need to start your journey toward TMJ massage therapy relief. These five steps—understanding your condition, preparing safely, mastering core techniques, integrating professional care, and adding supportive exercises—aren't just random suggestions. They're a proven roadmap that's helped thousands of people reclaim their lives from jaw pain.
The beauty of TMJ massage therapy lies in its simplicity and effectiveness. You don't need expensive equipment or complicated procedures. Your hands, some basic knowledge, and a commitment to consistency can provide remarkable relief. The research backs this up completely—multiple studies show massage as one of the most effective self-care strategies for TMJ dysfunction.
Here's the truth we've learned after treating countless TMJ patients: consistency beats intensity every single time. Five minutes of gentle daily massage will outperform sporadic aggressive sessions. Your jaw muscles respond to regular, caring attention, not forceful manipulation.
Start small and build your routine gradually. Begin with the self-assessment to understand where you're starting from. Then introduce the three core massage techniques we've covered. You might feel a bit awkward at first—that's completely normal. Like any new skill, it takes practice to find the right pressure and rhythm that works for your body.
Don't try to change everything at once. Pick one or two lifestyle modifications that feel manageable right now. Maybe it's improving your sleep position or taking breaks from screen time. Small changes compound into significant improvements over time.
Professional guidance makes a real difference when you're dealing with persistent symptoms. If you're not seeing improvement within 2-3 weeks of consistent self-care, that's your signal to seek help. There's no shame in needing support—some TMJ cases involve complex patterns that require trained eyes and hands to solve.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we've built our practice around this holistic approach to TMJ care. Our hands-on methodology combines the massage techniques you've learned here with specialized programs custom to your unique needs. We've seen people go from chronic daily pain to complete freedom of movement, and it never gets old.
More info about TMJ therapy services
Your jaw pain doesn't define you, and it doesn't have to control your life. Whether you're dealing with morning stiffness, stress-related grinding, or years of chronic discomfort, relief is absolutely possible. The tools in this guide can start working immediately, and we're here when you need additional support.
Take that first step today. Your future self—the one who can eat, speak, and smile without pain—is waiting for you to begin.
Midwood Magic – How Physical Therapy in Brooklyn Can Transform Your Health
Why Midwood Residents Choose Physical Therapy for Better Health
Midwood physical therapy brooklyn offers residents a proven path to better health, faster recovery, and lasting pain relief. Whether you're dealing with chronic back pain, recovering from surgery, or want to prevent future injuries, physical therapy provides non-invasive solutions that get to the root of your problems.
Top Midwood Physical Therapy Services:
• Orthopedic rehabilitation - Back pain, joint injuries, post-surgical recovery
• Sports rehabilitation - Athletic injuries, performance optimization
• Specialized programs - Vestibular therapy, pelvic health, Schroth Method for scoliosis
• Advanced treatments - Manual therapy, TMJ treatment, Parkinson's boxing programs
• Convenient options - Same-day appointments, telehealth consultations, home care
The Midwood neighborhood has become a hub for innovative physical therapy care. Clinics here offer everything from traditional orthopedic treatment to cutting-edge programs like balance training for seniors and specialized scoliosis correction.
Most clinics accept major insurance plans and offer direct access - meaning you can start treatment without a doctor's referral in New York State.
As Lou Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades helping Brooklyn residents overcome chronic pain and movement dysfunction through hands-on, personalized care. My experience treating complex cases in midwood physical therapy brooklyn has shown me that the right approach can transform lives - whether you're an athlete returning to competition or someone just wanting to walk without pain.
Why Physical Therapy Matters in Midwood
The heart of Brooklyn's midwood physical therapy brooklyn scene beats strong because of one simple truth: this neighborhood gets it. From the teenager nursing a basketball injury to the grandmother determined to keep gardening, Midwood residents understand that taking care of your body isn't just about fixing problems—it's about preventing them.
Walk through Midwood on any given day and you'll see what I mean. There's the jogger stretching against a tree, the construction worker rolling his shoulders after a long shift, the mom chasing toddlers at the playground. This community stays active, which means they also understand when something doesn't feel right.
Pain relief through physical therapy isn't just about making hurt go away. It's about understanding why your lower back screams every morning or why your shoulder aches when you reach for something on a high shelf. We dig deeper than the symptoms to find the real culprits—maybe it's how you sit at your desk, or perhaps an old ankle injury that never quite healed right.
Mobility means freedom. When you can't bend down to tie your shoes or turn your head to check your blind spot while driving, life gets smaller. Physical therapy opens those doors back up, restoring the movements you thought you'd lost forever.
The beauty of injury prevention lies in its simplicity. Teaching a weekend warrior proper warm-up techniques or showing a senior how to strengthen their core can prevent months of pain and frustration down the road.
Midwood's wellness culture accepts this forward-thinking approach. Our seniors come in not just when they're hurt, but when they want to stay strong enough to play with grandchildren. Local athletes use us to fine-tune their performance, not just patch up injuries. Even kids benefit from movement education that sets them up for a lifetime of healthy habits.
Post-surgical patients find their way back to normal life through carefully planned rehabilitation that respects healing timelines while pushing toward full recovery. Our community resources and evidence-based care work hand-in-hand to create a support system that extends far beyond the clinic walls.
Key Benefits for Midwood Residents
Fall-risk reduction transforms how our older neighbors steer their daily lives. Balance training and targeted strengthening exercises can cut fall risk by up to 30%. When Mrs. Rodriguez walks confidently to the corner store instead of worrying about every step, that's the real victory.
Faster return-to-work programs get people back to their livelihoods safely and efficiently. Whether you're a teacher dealing with neck pain from looking down at papers or a plumber recovering from a back injury, we focus on the specific movements your job demands.
Sports performance improvement helps local athletes push past their previous limits. We analyze how you move, identify weak links in the chain, and build strength training protocols that don't just fix problems—they make you better than before.
Chronic-pain management offers hope to those who've been told to "just live with it." Through our comprehensive approach combining hands-on treatment, targeted exercises, and education about your condition, many residents have broken free from pain cycles they thought were permanent.
Midwood Physical Therapy Brooklyn: Core Services & Specialties
At Evolve Physical Therapy, we offer a comprehensive range of services designed to meet the diverse needs of Midwood residents. Our approach combines traditional physical therapy techniques with innovative treatment methods to deliver exceptional outcomes.
Orthopedic Rehabilitation forms the foundation of our practice. We treat everything from acute injuries like ankle sprains to complex post-surgical cases. Our orthopedic rehab programs focus on restoring normal joint mechanics, reducing pain, and preventing future injuries through targeted strengthening and movement re-education.
Sports Rehabilitation addresses the unique needs of athletes at all levels. Our sports rehab specialists understand the demands of different sports and develop return-to-play protocols that ensure safe, effective recovery while optimizing performance.
Specialized Programs set us apart in the midwood physical therapy brooklyn landscape:
Vestibular Therapy: Addresses dizziness, vertigo, and balance disorders through specialized exercises that retrain the vestibular system
Pelvic Health: Provides discreet, effective treatment for pelvic pain, incontinence, and postpartum recovery
Schroth Method: Offers non-surgical scoliosis treatment using specialized exercises and postural training
TMJ Treatment: Relieves jaw pain and dysfunction through manual therapy and targeted exercises
Pediatric Physical Therapy serves our younger community members with age-appropriate interventions for developmental delays, sports injuries, and neurological conditions.
Our signature Rock Steady Boxing for Parkinson's program has gained national attention, even being featured on NBC News. This innovative approach uses boxing-inspired exercises to improve balance, coordination, and quality of life for individuals with Parkinson's disease.
Home Care Options bring our expertise directly to patients who cannot easily travel to our clinic, ensuring that everyone in the Midwood community has access to quality physical therapy care.
Traditional Physical Therapy vs Physiotherapy in Midwood Physical Therapy Brooklyn
Understanding the difference between traditional physical therapy and physiotherapy approaches helps patients make informed decisions about their care. While both aim to restore function and reduce pain, their methodologies differ significantly.
Traditional Physical Therapy typically emphasizes:
Passive modalities like heat, ice, and electrical stimulation
Structured exercise protocols
Focus on structural issues (bones, muscles, joints)
Gradual progression through standardized phases
Physiotherapy takes a more active, neuro-focused approach:
Hands-on manual therapy techniques
Neuro-corrective training that addresses nervous system dysfunction
Active patient participation in movement re-education
Emphasis on neural drive and movement quality
Aspect Traditional PT Physiotherapy Primary Focus Structural healing Neurological function Patient Role Passive recipient Active participant Techniques Modalities + exercise Manual therapy + movement training Session Style Protocol-driven Individualized assessment Goals Pain reduction Movement optimization
At Evolve Physical Therapy, we integrate the best of both approaches, using evidence-based techniques that address both structural and neurological components of dysfunction.
Special Programs Elevating Midwood Physical Therapy Brooklyn Care
Our specialized programs represent the cutting edge of midwood physical therapy brooklyn care, addressing conditions that traditional approaches often struggle to treat effectively.
Vestibular Rehabilitation helps patients with dizziness, vertigo, and balance disorders regain stability and confidence. Using specialized exercises, we retrain the vestibular system to process sensory information correctly, dramatically reducing symptoms and fall risk.
Pelvic Floor Therapy addresses a range of conditions including incontinence, pelvic pain, and postpartum dysfunction. Our trained specialists provide compassionate, evidence-based care in a comfortable, private setting.
Schroth Method for Scoliosis offers a non-surgical alternative for managing spinal curvatures. This specialized technique uses three-dimensional exercises and breathing patterns to improve posture and reduce curve progression.
LSVT BIG for Parkinson's Disease is a certified protocol that helps patients with Parkinson's improve amplitude of movement and functional mobility. This intensive program has shown remarkable results in maintaining independence and quality of life.
TMJ Mobilization combines manual therapy techniques with patient education to address temporomandibular joint dysfunction. We focus on restoring normal jaw mechanics and reducing associated headaches and facial pain.
Research supports many of these interventions. For example, studies on trigger-point injections show the effectiveness of targeted manual techniques in treating myofascial pain syndromes.
The Patient Journey: From First Call to Full Recovery
Starting physical therapy can feel overwhelming, especially when you're already dealing with pain or mobility issues. At Evolve Physical Therapy, we've designed our patient journey to feel as comfortable and straightforward as possible - think of it as your roadmap to getting back to the activities you love.
Your initial evaluation is where the magic begins. We spend a full 60-90 minutes getting to know you, your condition, and what matters most in your daily life. This isn't a rushed appointment where you feel like just another number. We dive deep into your medical history, discuss your pain patterns, and really listen to your concerns about how your condition affects your work, family time, or weekend trips.
Functional testing helps us become detectives, uncovering the real reasons behind your symptoms. We might watch how you walk, test your balance, or have you demonstrate movements that typically cause problems. If you're an athlete, we'll look at sport-specific movements. If you're dealing with everyday activities like getting out of bed or carrying groceries, we'll assess those too. It's all about understanding your unique movement patterns and identifying what's not working quite right.
The goal setting conversation is one of my favorite parts of the process. This is where we talk about your dreams - whether that's getting back on the tennis court, playing with your grandkids on the floor, or simply sleeping through the night without back pain. We make sure your goals become our goals, creating a shared vision for your recovery.
Your individualized treatment plan emerges from everything we've learned about you. We'll explain exactly why we're recommending specific techniques or exercises, and how each piece fits into your bigger recovery picture. No cookie-cutter approaches here - your plan is as unique as you are.
During your one-on-one sessions, you'll receive hands-on manual therapy and guided exercise instruction. We believe in the power of human touch and personalized attention. You'll never be handed a sheet of exercises and left to figure things out on your own. We're right there with you, making sure you understand each movement and feel confident in your progress.
Progress tracking happens naturally throughout your care. We use objective measures whenever possible - not just "how do you feel?" but actual functional improvements we can measure and celebrate together. We regularly reassess your condition and adjust your treatment plan as you improve, always keeping your original goals in mind.
Discharge planning might seem premature to discuss early on, but we start thinking about your long-term success from day one. We focus on giving you the tools and knowledge to maintain your improvements long after you've graduated from formal therapy. This includes home exercise programs you can actually stick with and lifestyle modifications that make sense for your real life.
Our prevention tips aren't just generic advice - they're specific strategies based on what we've learned about your body and your lifestyle during our time together. We want to help you avoid future problems, not just fix current ones.
How Treatment Plans Are Personalized
Every person who comes through our doors gets a completely customized approach to care. We've learned over the years that even when two people have the same diagnosis, their treatment needs can be completely different.
Your lifestyle assessment considers everything that makes you, well, you. A construction worker dealing with lower back pain needs different strategies than someone who sits at a desk all day with the same condition. We factor in your work demands, how you spend your free time, your family responsibilities, and even your personal preferences about exercise and activity.
Movement analysis goes way beyond just identifying what hurts. We examine how your whole body works together, what compensations you've developed over time, and which movement patterns might be contributing to your symptoms. Sometimes the real problem isn't where you feel the pain - and that's exactly what we're trained to find.
We use outcome measures to track your progress objectively. These are validated assessment tools that measure things like pain levels, functional capacity, and how much your condition affects your quality of life. It's incredibly motivating to see concrete proof of your improvements over time.
Shared decision-making means you're never just a passive recipient of treatment. We explain your options, discuss potential benefits and any risks, and make sure your preferences are incorporated into your final treatment plan. After all, you're the one who has to live with the results.
Patient education is woven throughout everything we do. We want you to understand your condition, learn proper body mechanics, and develop strategies for managing symptoms on your own. The goal is to make you the expert on your own body, so you feel confident and empowered long after your formal treatment ends.
This personalized approach is what makes midwood physical therapy brooklyn care at Evolve so effective. We're not just treating your symptoms - we're treating you as a whole person with unique needs, goals, and circumstances.
Advanced Techniques & Technology Driving Results
Modern physical therapy extends far beyond basic exercises and hot packs. At Evolve Physical Therapy, we employ cutting-edge techniques and technology to deliver superior outcomes for our Midwood patients.
Manual Therapy remains the cornerstone of our hands-on approach. Our therapists are trained in various manual techniques including joint mobilization, soft tissue mobilization, and myofascial release. These hands-on interventions can immediately improve mobility, reduce pain, and restore normal movement patterns.
Soft Tissue Release techniques address muscle tension, trigger points, and fascial restrictions that contribute to pain and dysfunction. We use instruments and hands-on techniques to break up scar tissue and improve tissue quality.
Neuromuscular Re-education helps retrain movement patterns and improve motor control. This is particularly important for patients recovering from neurological conditions or those who have developed compensatory movement strategies due to pain or injury.
Dry Needling Alternatives provide similar benefits to traditional dry needling without the use of needles. We employ techniques like instrument-assisted soft tissue mobilization and targeted compression to achieve trigger point release.
Laser Therapy uses specific wavelengths of light to promote tissue healing, reduce inflammation, and decrease pain. This non-invasive treatment can accelerate recovery and improve the effects of other interventions.
Balance Platforms and stability training equipment help improve proprioception and postural control. These tools are particularly valuable for fall prevention programs and sports performance improvement.
Motion Capture Technology allows us to analyze movement patterns with precision, identifying subtle dysfunctions that might be missed during visual observation alone.
EMG-Guided Exercise uses electromyography to provide real-time feedback about muscle activation patterns, helping patients learn to recruit muscles more effectively during therapeutic exercises.
Research supports many of these approaches. Studies on ACDF rehabilitation demonstrate the importance of specialized post-surgical protocols in optimizing outcomes after spinal fusion procedures.
Insurance, Scheduling & Preparing for Your First Visit
Getting started with midwood physical therapy brooklyn care shouldn't feel overwhelming. At Evolve Physical Therapy, we've designed our process to remove barriers and get you the help you need quickly.
Insurance coverage is rarely a problem for physical therapy services. Most major insurance plans recognize the value of PT and cover our treatments. Our friendly billing team takes the guesswork out of the equation - they'll verify your benefits before your first visit and explain exactly what you can expect to pay.
Here's something many people don't know: New York State's direct access laws mean you can start physical therapy immediately without waiting for a doctor's referral. You get up to 30 days or 10 visits to begin treatment, which often makes the difference between a quick recovery and a lingering problem.
Same-day appointments are available because we understand that pain doesn't wait for convenient scheduling. Whether you tweaked your back moving furniture or woke up with a stiff neck, we can usually see you within 24 hours.
What should you wear? Think comfortable and accessible. If your shoulder hurts, a tank top works better than a turtleneck. Knee problems? Shorts are your friend. Basically, dress like you're going to the gym, not a business meeting.
Preparing for your visit is simple. We'll send you intake forms to complete online beforehand - this saves time and lets us focus on your treatment rather than paperwork. Bring your insurance card, a list of any medications you're taking, and any X-rays or MRI reports you have.
Telehealth options have become increasingly popular, especially for follow-up visits and certain types of treatment. Sometimes the best therapy session happens in your own living room where you can practice exercises in your actual environment.
Parking is available right at our clinic, and we're easily accessible by public transportation if you prefer not to drive.
For questions about scheduling or to book your first appointment, check out our contact page. Our team is always happy to help you get started on your path to better health.
Frequently Asked Questions about Midwood Physical Therapy
Do I need a doctor's referral to start?
Thanks to New York State's direct access laws, you can start your healing journey without waiting for a doctor's referral. Licensed physical therapists with at least three years of experience can evaluate and treat you for up to 30 days or 10 visits - whichever comes first.
This means when you wake up with that nagging back pain or twist your ankle during weekend basketball, you can call us directly and start treatment right away. No sitting in waiting rooms, no scheduling multiple appointments just to get permission to feel better.
If your condition needs additional medical attention beyond our scope, we'll connect you with the right physician. It's a system that gets you faster relief while keeping your safety as the top priority.
How long does each session last and how many will I need?
Each midwood physical therapy brooklyn session runs 60-90 minutes, giving us real time to work on your specific needs. We're not rushing you in and out - there's time for hands-on treatment, guided exercises, and answering all your questions.
How many sessions you'll need depends on what brought you in. That fresh ankle sprain might feel dramatically better in 4-6 visits, while recovering from knee surgery could take 12-20 sessions or more. We follow a phase-based approach that makes sense:
Phase 1 focuses on calming down pain and protecting injured tissues during those first few weeks. Phase 2 gets you moving again as we restore mobility and introduce gentle movement. Phase 3 builds your strength and endurance back up over several weeks. Phase 4 gets you ready to return to all your normal activities, whether that's playing tennis or lifting your grandchildren. Phase 5 keeps you healthy long-term with prevention strategies.
We track your progress every step of the way, so you'll always know where you stand and what comes next.
What conditions are most commonly treated in Midwood clinics?
Lower back pain is hands down our most frequent visitor - and honestly, it makes sense given how much sitting and stress we all deal with. Whether you threw out your back moving furniture or it's been bothering you for months, targeted physical therapy can make a world of difference.
Sports injuries keep us busy too, especially with all the active families in Midwood. Twisted ankles from basketball, shoulder problems from tennis, knee issues from running - we see it all. Our sports rehab experience means we understand not just how to get you pain-free, but how to get you back to performing your best.
Post-surgical rehabilitation is another big part of what we do. After joint replacements, arthroscopic procedures, or spinal surgeries, the right rehabilitation makes the difference between just okay results and truly great outcomes.
We also frequently treat neck pain (often from too much computer time), headaches, arthritis that's slowing you down, balance problems that worry you or your family, and those annoying repetitive strain injuries from work. Whatever brought you in, we've probably seen it before and know how to help.
Conclusion
The midwood physical therapy brooklyn community is witnessing something remarkable - a fundamental shift toward proactive health management that's changing lives throughout our neighborhood. Instead of accepting pain as "just part of getting older" or relying solely on medications, residents are finding the power of hands-on, evidence-based physical therapy care.
This change represents more than just a healthcare trend. It's about reclaiming control over your body and choosing treatments that address the root causes of dysfunction rather than masking symptoms. Whether you're a weekend warrior dealing with a nagging shoulder injury, a senior wanting to prevent falls, or someone recovering from surgery, physical therapy offers a path forward that emphasizes healing, strength, and long-term wellness.
At Evolve Physical Therapy + Sports Rehabilitation, we've had the privilege of being part of thousands of recovery stories. From our Rock Steady Boxing program for Parkinson's patients (which even caught the attention of NBC News) to our specialized manual therapy techniques, we've seen how the right approach can transform someone's relationship with their body.
What sets our approach apart isn't just our advanced techniques or specialized programs - it's our belief that every person deserves individualized, hands-on care. We don't believe in one-size-fits-all protocols or cookie-cutter treatment plans. Your journey is unique, and your care should be too.
The beauty of living in a community like Midwood is having access to world-class healthcare right in your neighborhood. You don't need to travel to Manhattan or deal with complicated referral processes. Quality physical therapy care is available here, with providers who understand the specific needs of our diverse community.
Whether you're dealing with chronic pain that's been holding you back, recovering from an injury, or simply want to move better and feel stronger, we invite you to take that first step. Sometimes the hardest part of any healing journey is simply making the decision to begin.
Consider starting with our prehabilitation services for rotator cuff surgery if you're facing upcoming surgery, or reach out to discuss how our comprehensive approach might help with your specific situation. Your future self - the one moving without pain, sleeping through the night, and living life to the fullest - is waiting.
Your healing journey starts with a single phone call. Let's take that step together.
From Stroke to Strength: Mastering Neurological Rehabilitation
Why Rehabilitation for Neurological Disorders Changes Everything
Rehabilitation for neurological disorders is a specialized medical approach that helps people with brain, spinal cord, or nervous system injuries regain function and independence. Whether you're dealing with stroke, Parkinson's disease, multiple sclerosis, or traumatic brain injury, the right rehabilitation program can dramatically improve your quality of life.
Quick Overview: What Neurological Rehabilitation Offers
Physical recovery: Restore movement, balance, and strength
Cognitive support: Improve memory, attention, and problem-solving
Speech therapy: Regain communication and swallowing abilities
Daily living skills: Relearn essential activities like dressing and cooking
Emotional support: Address depression, anxiety, and adjustment challenges
Family education: Train caregivers to support your recovery journey
Neurological rehabilitation stands as what researchers call "a shining source of hope for countless individuals seeking to regain control of their lives after being impacted by neurological issues." The field has evolved dramatically since 2000, with new evidence showing that intensive, task-specific practice can literally rewire your brain through neuroplasticity.
Studies show that over 80% of stroke survivors benefit from rehabilitation, with some patients regaining significant function even years after their initial injury. The key is starting early and using the right combination of therapies custom to your specific needs and goals.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've spent nearly two decades specializing in complex neurological cases, including my early work in Tel Aviv treating trauma victims and wounded soldiers. My experience with rehabilitation for neurological disorders has shown me that with the right approach, patients can achieve recovery milestones that seemed impossible at the start of their journey.
Rehabilitation for Neurological Disorders: What It Is & Who It Helps
When life throws you a curveball like a stroke, brain injury, or neurological condition, it can feel like your world has been turned upside down. Rehabilitation for neurological disorders is your roadmap back to independence—a carefully designed, doctor-supervised program that helps your brain and body learn to work together again.
Think of your nervous system as your body's electrical grid, controlling everything from lifting a coffee cup to remembering your grandchild's name. When neurological conditions disrupt these pathways, the effects can ripple through every aspect of daily life. That's exactly why effective rehabilitation takes a team approach, addressing not just physical challenges but cognitive, emotional, and social needs too.
Here's what makes rehabilitation for neurological disorders so powerful: it's built on the science of neuroplasticity. Your brain has an amazing ability to rewire itself and form new connections throughout your entire life. This means that even after significant injury or disease, your brain can find fresh pathways to accomplish tasks and reclaim lost abilities.
Disorders That Benefit
Stroke affects nearly 800,000 Americans every year, making it the leading cause of adult disability. When blood flow to your brain gets suddenly blocked or a vessel bursts, it can impact movement, speech, thinking, and emotions all at once. The encouraging news? Many of our patients notice improvements after just their first therapy session.
Traumatic brain injury touches the lives of over 5.3 million Americans. Whether from car accidents, falls, sports injuries, or military service, these injuries can affect everything from coordination and memory to personality changes. Each person's journey looks different, which is why individualized care matters so much.
Spinal cord injuries can dramatically change how you move through the world, potentially affecting sensation, movement, and bodily functions. Our focus shifts to maximizing what's working well while teaching new strategies for staying independent.
Multiple sclerosis presents unique challenges because symptoms can change from day to day. This autoimmune condition affects the protective covering around nerve fibers, leading to fatigue, weakness, balance issues, and cognitive changes that come and go unpredictably.
Parkinson's disease affects over one million Americans with tremors, stiffness, slow movements, and balance problems. We've seen incredible results with specialized programs—our Rock Steady Boxing program has even caught the attention of NBC News for its effectiveness.
ALS (Lou Gehrig's disease) progressively affects the nerve cells controlling voluntary muscles. While we can't cure it, rehabilitation for neurological disorders can help maintain function and quality of life for as long as possible, making every day count.
Cerebral palsy typically appears in early childhood, affecting movement and posture in ways that last a lifetime. Our approach focuses on maximizing independence while preventing complications that could develop over time.
Vestibular dysfunction might sound technical, but it simply means problems with your inner ear that cause dizziness, balance issues, and falls. Interestingly, up to 50% of stroke survivors also deal with spatial neglect, where they have trouble noticing one side of their environment—but targeted rehabilitation can make remarkable improvements.
Core Goals & Objectives
Every person's recovery journey is unique, but rehabilitation for neurological disorders typically focuses on six key areas that can transform your daily life.
Mobility and movement often take center stage because they affect everything else. Whether you're relearning to walk, figuring out safer ways to transfer from your bed to a chair, or adapting to new mobility equipment, we break down complex movements into manageable steps.
Activities of daily living cover those essential tasks that help you feel like yourself again—bathing, dressing, cooking, managing medications. We tackle these one piece at a time, building your confidence along the way so you can reclaim your independence.
Cognitive function encompasses the thinking skills that make you who you are: memory, attention, problem-solving, and planning abilities. Through targeted exercises and practical strategies, we help your mind get back to its sharpest.
Speech and communication challenges can feel isolating, whether you're struggling with finding words, speaking clearly, or swallowing safely. Our speech therapy approaches help you reconnect with family and friends while ensuring proper nutrition.
Emotional well-being deserves just as much attention as physical recovery. Depression, anxiety, and adjustment difficulties commonly accompany neurological conditions, and addressing these feelings is crucial for overall healing.
Community reintegration represents the ultimate goal—returning to work, social activities, and meaningful roles in your family and community. This might include vocational counseling, driver training, or simply building the confidence to engage with the world again.
Personalized Recovery Path: Assessment, Neuroplasticity & Care Settings
When you walk into our Brooklyn clinic, we know that your story is completely unique. Your rehabilitation for neurological disorders journey won't look like anyone else's—and that's exactly how it should be.
We start every relationship with a thorough evaluation that goes way beyond just reading your medical chart. We need to know your diagnosis, but what we really want to understand is you. What did your typical day look like before your injury? What activities bring you joy? What goals are keeping you motivated to push through the hard days?
Our comprehensive assessment covers all the basics—movement patterns, strength, balance, cognitive abilities, and how well you can handle daily tasks. We use proven tools like the Barthel Index to measure exactly where you're starting from, giving us clear data to track your progress. But we also spend time understanding your living situation, your support system, and what "success" means to you personally.
Timing matters enormously in neurological recovery. Research consistently shows that early and intensive rehabilitation leads to better outcomes and greater independence. Ideally, we want to start working with you within 72 hours of your injury or when you're medically stable. Your brain is most ready to learn and adapt in those early stages.
The setting where you receive care depends on your specific needs and current function level. Inpatient rehabilitation offers the most intensive approach—typically 3+ hours of therapy daily, five days a week for 2-6 weeks. This works best for people with acute injuries or multiple impairments who need that level of support.
Outpatient rehabilitation provides 45-60 minute sessions, usually 2-3 times per week for several months. This option works well for people who are medically stable and have specific goals they want to achieve. Many of our Brooklyn patients prefer this approach because they can sleep in their own beds and maintain some of their normal routines.
Home-based services offer the most flexibility, with therapy intensity custom to your needs and delivered in your familiar environment. This can be especially helpful for people with mobility limitations or those transitioning from more intensive care.
Crafting an Individualized Plan for Rehabilitation for Neurological Disorders
Creating your personalized plan starts with comprehensive functional testing that reveals your strengths, not just your challenges. We want to know what you can do so we can build from there.
We use something called the International Classification of Functioning, Disability and Health (ICF) framework. Don't worry—it's not as complicated as it sounds. It's simply a way of looking at how your condition affects your body functions, your daily activities, and your ability to participate in the life roles that matter to you. This approach ensures we're treating the whole person, not just symptoms.
Your values and preferences drive everything we do. Maybe your biggest goal is cooking Sunday dinner for your family again. Perhaps you're determined to get back to work or play with your grandchildren on the floor. We listen carefully to what matters most to you, then design interventions that move you toward those specific goals.
Family involvement makes a huge difference in recovery outcomes. We educate your loved ones about your condition and teach them safe ways to help with exercises and daily activities. Often, family members become our most important partners in your recovery journey.
For more detailed information about our comprehensive approach, you can learn more about neurological therapy and how we customize treatment plans.
The Science of Neuroplasticity
Here's the amazing news: your brain never stops learning and adapting. Neuroplasticity—your brain's ability to form new connections and reorganize itself—is the foundation of all rehabilitation for neurological disorders. Even after significant injury, healthy parts of your brain can learn to take over functions that were previously handled by damaged areas.
Think of it like this: if your usual route to work is blocked by construction, you find a new way to get there. Your brain does the same thing. When neural pathways are damaged, it creates new routes to accomplish the same goals.
The secret to open uping neuroplasticity lies in intensive, repetitive, task-specific practice. Every time you practice a movement or skill, you're strengthening the neural pathways that control that function. It's like building a new highway in your brain—the more traffic it gets, the stronger and more efficient it becomes.
Several factors boost your brain's ability to rewire itself: High repetition creates stronger neural connections. Task-specific practice (doing real-world activities rather than abstract exercises) proves more effective. Your motivation and active engagement accelerate the process—your brain changes more readily when you're invested in the outcome. Progressive challenges keep your brain adapting and learning new skills.
One of the most dramatic examples comes from constraint-induced movement therapy research. Stroke survivors who had their unaffected arm restrained while intensively training their affected arm for 3-6 hours daily over two weeks regained significant function—even years after their stroke. The improvements lasted for months, proving that the brain had truly rewired itself.
You can explore more scientific research on brain recovery to understand how these principles apply to different neurological conditions.
The key takeaway? Your brain wants to heal and adapt. Our job is creating the right conditions and providing the right challenges to help that natural process along.
Evidence-Based Therapies & Innovations in Rehabilitation for Neurological Disorders
The world of rehabilitation for neurological disorders has transformed dramatically over the past two decades. What once seemed impossible—helping someone walk again after a stroke or reducing tremors in Parkinson's disease—is now happening in clinics every day. The secret lies in combining time-tested therapeutic approaches with cutting-edge innovations that harness your brain's natural ability to heal and adapt.
Think of modern neurological rehabilitation as having two powerful toolkits. The first contains the proven, foundational therapies that have helped millions of people regain function. The second holds exciting new technologies that can accelerate recovery in ways we never imagined possible.
Conventional Cornerstones
Physical Therapy remains the foundation of neurological recovery, but it's evolved far beyond simple exercises. Today's rehabilitation for neurological disorders uses sophisticated movement analysis and targeted interventions that literally retrain your nervous system.
Gait re-education helps you relearn the complex choreography of walking. We break down each component—weight shifting, stepping, balance—and rebuild these skills systematically. Many patients are amazed when they take their first independent steps after thinking they'd never walk again.
Balance training goes beyond preventing falls. We challenge your stability systems through specific exercises that force your brain to develop new strategies for staying upright. This might involve standing on unstable surfaces, practicing reaching movements, or navigating obstacle courses.
Strength training isn't just about building muscle. Research shows that moderate aerobic and strengthening programs can significantly improve function across multiple neurological conditions. The key is progressive challenge—gradually increasing difficulty so your nervous system continues adapting.
Neuromuscular re-education focuses on improving communication between your brain and muscles. Through repetitive, purposeful movements, we help damaged neural pathways find new routes to control your body.
Our comprehensive approach to Physical Therapy for Neurological Disorders combines all these elements into personalized treatment plans.
Occupational Therapy transforms the seemingly impossible back into the possible. Occupational therapists are problem-solvers who help you regain independence in daily activities. They might teach you new ways to button a shirt with limited hand function or reorganize your kitchen for easier meal preparation. The goal isn't just to complete tasks—it's to restore your confidence and sense of self-reliance.
Speech-Language Therapy addresses both communication disorders and swallowing problems that can profoundly impact quality of life. Modern speech therapy uses constraint-induced language therapy, applying the same intensive practice principles that work for motor recovery to language rehabilitation. Patients with aphasia often see remarkable improvements when they practice communication skills for several hours daily over concentrated periods.
Neuropsychology recognizes that neurological conditions affect your mind as much as your body. Neuropsychologists provide strategies for memory problems, attention deficits, and mood disorders that commonly accompany neurological conditions. They help you understand how your brain has changed and develop new ways to think, learn, and cope.
Cutting-Edge Techniques
Robotics and Exoskeletons are bringing science fiction into rehabilitation reality. Over 400 centers worldwide now use medical exoskeletons for gait training. These remarkable devices allow patients to practice walking movements even when they don't have the strength to support their own body weight.
The magic happens through high-dose repetition training. Where a human therapist might help you practice 50 steps in a session, an exoskeleton can support thousands of steps. This massive increase in practice time can accelerate motor learning while reducing the physical demands on therapists.
Virtual Reality is revolutionizing rehabilitation for neurological disorders by creating immersive, engaging environments for practice. Imagine practicing crossing a busy street or navigating a grocery store—all from the safety of a clinic. VR can bypass cognitive deficits that might interfere with traditional therapy and dramatically improve patient motivation.
Patients often don't realize they're working hard because they're having fun. One stroke survivor told me that playing VR games to improve her arm function felt more like entertainment than therapy. The results speak for themselves—recent studies show promising outcomes for VR in stroke rehabilitation. You can explore this research in this latest study on virtual reality for stroke.
Brain-Computer Interfaces represent the frontier of neurological rehabilitation. These systems translate brain signals into commands that can control external devices. While still experimental, BCIs show promise for people with severe paralysis, potentially allowing them to control prosthetic limbs or computer cursors with their thoughts alone.
Prism Adaptation Therapy offers hope for patients with spatial neglect, a common challenge after stroke where people lose awareness of one side of their body or environment. Using special 20-diopter wedge prism lenses, patients perform simple pointing tasks. This surprisingly simple intervention can lead to significant improvements in daily activities like self-dressing and wheelchair navigation.
Transcranial Stimulation techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) can improve the effects of traditional therapy. These non-invasive brain stimulation methods make the brain more receptive to learning during rehabilitation sessions, potentially accelerating recovery.
Functional Electrical Stimulation uses precisely timed electrical impulses to stimulate paralyzed muscles. Beyond maintaining muscle mass, FES can potentially improve motor control by providing sensory feedback that helps retrain neural pathways.
Wearable Sensors bring rehabilitation into your daily life. Modern technology allows us to monitor your activity and progress outside the clinic. These devices track walking patterns, sleep quality, and daily activity levels, providing valuable data to fine-tune your treatment plan.
Specialized Programs & Community Resources
Rock Steady Boxing represents our commitment to innovative, evidence-based programs. At Evolve Physical Therapy, we're proud to offer this specialized program for people with Parkinson's disease. This non-contact boxing program, featured on NBC News, shows remarkable results in improving balance, coordination, and confidence.
The program combines high-intensity exercise with the neuroplasticity-enhancing effects of learning complex movement patterns. Participants often describe feeling more like athletes than patients, which transforms their relationship with their condition. Learn more about our Physical Therapy for Parkinson's Disease in Brooklyn.
Aquatic Therapy harnesses the unique properties of water for rehabilitation. Buoyancy reduces joint stress while water resistance provides strengthening benefits. The hydrostatic pressure can improve circulation and reduce swelling. Many patients find they can move more freely in water than on land, giving them hope and motivation to continue their recovery journey.
Vocational Counseling addresses the practical reality that many people want to return to work after neurological injury. Vocational counselors assess work capabilities, recommend workplace modifications, and facilitate communication with employers. The goal is helping you maintain your professional identity and financial independence.
Support Groups provide something that no technology can replace—human connection. Meeting others who understand your challenges offers emotional support, practical tips, and motivation to continue with rehabilitation efforts. Many patients tell us that their support group became like a second family during their recovery journey.
Measuring Progress, Overcoming Barriers & Thriving Beyond Rehab
Recovery from neurological conditions isn't like following a recipe where you add ingredients and get predictable results. It's more like learning to dance again—some days you'll feel graceful and confident, other days you might step on your own toes. That's completely normal, and it's why having the right team and measurement tools makes all the difference in your journey with rehabilitation for neurological disorders.
Think of your rehabilitation team as your personal recovery squad. Each member brings unique skills to help you reach your goals, and they work together like a well-orchestrated symphony. Your physiatrist serves as the conductor, overseeing your entire care plan and making medical decisions. Your physical therapist focuses on getting you moving stronger and safer, while your occupational therapist helps you master daily activities like cooking and dressing.
If you're dealing with speech or swallowing challenges, your speech-language pathologist becomes your communication coach. Rehabilitation nurses provide round-the-clock care and education in hospital settings, and case managers act like your personal navigators, helping coordinate services and plan your next steps.
Don't overlook the crucial roles of neuropsychologists, who address the emotional and cognitive aspects of recovery, and social workers, who connect you with community resources and family support. This team meets regularly to discuss your progress—they're literally talking about you behind your back, but in the best possible way!
Tracking Outcomes & Adjusting the Plan
Measuring progress in rehabilitation for neurological disorders requires more than just asking "How do you feel today?" We use specific, scientifically-validated tools that give us objective data about your recovery.
The Functional Independence Measure (FIM) tracks how much help you need with everyday activities. It measures everything from eating and dressing to walking and thinking tasks. Think of it as a detailed report card for independence—and unlike school report cards, everyone wants to see your scores improve!
The 6-Minute Walk Test sounds simple, but it's incredibly revealing. How far you can walk in six minutes tells us volumes about your endurance, balance, and overall functional capacity. It's also motivating because you can see concrete improvement as the weeks go by.
For balance concerns, we use the Berg Balance Scale, which evaluates how steady you are during various activities. This assessment is particularly important because it helps predict fall risk—and preventing falls is crucial for maintaining the progress you've worked so hard to achieve.
We believe in setting SMART goals together. Instead of vague hopes like "get better," we create specific, measurable targets. For example, "walk 100 feet independently with a walker within 4 weeks" gives everyone a clear target to work toward.
Here's something important to understand: recovery rarely follows a straight line upward. Research shows that neurological recovery follows complex, non-linear patterns. You might make rapid progress for weeks, then hit a plateau that feels frustrating. These plateaus don't mean you've stopped healing—sometimes your brain needs time to consolidate new learning before the next breakthrough happens.
Data-driven metrics help us track these patterns and adjust your treatment accordingly. We also value patient-reported outcomes—your own assessment of how you're feeling and functioning matters enormously. Technology now allows us to monitor your activity and progress outside the clinic through wearable sensors and mobile apps, giving us a complete picture of your recovery.
Family & Caregiver Support
Family members often become unsung heroes in rehabilitation for neurological disorders. They provide motivation when you want to give up, celebrate small victories that others might not notice, and offer the kind of support that no medical professional can replicate. But caregiving can also feel overwhelming, which is why we make sure families get the education and support they need.
We teach family members practical skills like how to assist with exercises safely, recognize signs of fatigue or distress, and encourage independence while providing appropriate support. It's a delicate balance—you want to help without taking over tasks that your loved one can do independently.
Home safety becomes a top priority as you transition from clinical settings back to daily life. We assess your living environment and recommend modifications that prevent falls and injuries. Simple changes like adding grab bars, improving lighting, removing trip hazards, and installing ramps can make the difference between independence and setbacks.
Our team helps families understand medication management and medical equipment use. We also connect caregivers with respite care services because taking breaks isn't selfish—it's necessary. Caregivers who take care of themselves are better able to support their loved ones' recovery.
For comprehensive strategies about staying safe at home, check out our detailed guide on Physical Therapy for Fall Prevention.
Frequently Asked Questions about Rehabilitation for Neurological Disorders
How long does neurological rehabilitation take? This is like asking "How long is a piece of string?"—it depends on many factors. Your condition, severity of symptoms, personal goals, and commitment to the process all influence timing. Some patients see significant improvements in weeks, while others continue making gains over months or years. The encouraging news is that neuroplasticity allows for continued improvement with consistent practice, even years after injury.
What can I realistically expect from rehabilitation? While we can't promise specific outcomes, research consistently shows that 60-80% of patients with neurological disorders experience meaningful functional improvements with intensive rehabilitation. Many patients regain independence in daily activities, return to work, and report significantly improved quality of life. The key is starting with realistic expectations while remaining open to possibilities.
Will insurance cover my rehabilitation? Most insurance plans cover medically necessary rehabilitation services, but coverage varies significantly. Some plans limit the number of visits or require prior authorization. Our team works directly with insurance companies to maximize your benefits and helps you understand your specific coverage. We believe financial concerns shouldn't prevent you from getting the care you need.
What if I'm not seeing progress? Plateaus happen to everyone in neurological recovery, and they're incredibly frustrating. When progress stalls, we reassess your entire program and often try different approaches. Sometimes changing the type of therapy, adjusting intensity, or adding new techniques can restart progress. Your brain retains the capacity for change throughout your entire life.
Can I do rehabilitation exercises at home? Absolutely! Home exercise programs form a crucial part of rehabilitation for neurological disorders. We teach you and your family safe, effective exercises to practice between therapy sessions. The magic happens in consistent daily practice—this is where neuroplasticity really kicks in. We provide detailed instructions and follow up to ensure you're doing exercises correctly.
How do I know if I need inpatient versus outpatient rehabilitation? This decision depends on your medical stability, severity of impairments, and support system at home. Inpatient rehabilitation provides intensive therapy (3+ hours daily) with 24-hour medical supervision, making it ideal for people with complex needs or multiple impairments. Outpatient therapy offers more flexibility and allows you to practice skills in your actual home environment, which can be incredibly valuable for real-world application.
Conclusion
Rehabilitation for neurological disorders represents hope in action—where cutting-edge science meets genuine human compassion. At Evolve Physical Therapy + Sports Rehabilitation, we've witnessed countless moments when patients surprise themselves with what they can achieve. That first independent step after a stroke. The steady hands of a Parkinson's patient throwing a boxing combination. The clear words from someone who thought they'd never speak again.
Our hands-on approach in Brooklyn starts with a simple belief: every person's recovery journey is unique and deserves personalized attention. Whether you're navigating the early days after a stroke, learning to live with Parkinson's disease, or working through the challenges of a traumatic brain injury, we craft treatment plans that honor your specific goals and circumstances.
From our Rock Steady Boxing program that's been featured on NBC News to our comprehensive neurological services across Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, we combine proven techniques with innovative approaches. Our team understands that recovery isn't just about regaining physical function—it's about reclaiming your independence, confidence, and quality of life.
The future of neurological rehabilitation continues to unfold with exciting possibilities. Virtual reality systems, robotic assistants, and brain stimulation techniques are opening new doors for recovery. Yet what never changes is the fundamental truth that your brain's capacity for healing—neuroplasticity—remains active throughout your lifetime.
Starting early makes a difference, but it's never too late to begin. We've seen patients make meaningful improvements months and even years after their initial diagnosis. The key ingredients remain the same: intensive practice, consistent effort, and a support team that believes in your potential.
Your recovery story is still being written. Every therapy session, every home exercise, every small victory builds toward the larger goal of living life on your terms again. We're honored to be part of that journey, celebrating your progress and providing encouragement when the path feels challenging.
Ready to take the next step? Rehabilitation for neurological disorders works best when you have the right team supporting you. Contact us today to find how our holistic approach can help you move forward with confidence and strength.
For more information about our comprehensive services and personalized care philosophy, visit our sports rehabilitation and personalized care page.
Your journey toward recovery and renewed independence starts with reaching out. We're here to help you take that important first step.
Brooklyn's Finest Physical Therapy Spots in Park Slope
Why Park Slope Residents Choose Local Physical Therapy Over Big Chains
Park Slope physical therapy offers something unique - neighborhood clinics that combine world-class expertise with the personal touch of local care. Whether you're dealing with runner's knee from jogging around Prospect Park or chronic pain that's keeping you from your active lifestyle, this Brooklyn neighborhood has become a hub for innovative rehabilitation services.
Top Park Slope Physical Therapy Services:
• Community-focused practices - Serving multiple generations since 2006
• Specialized locations - Multiple clinics with convenient parking partnerships
• Holistic manual therapy - Comprehensive approach with wide insurance acceptance
• Sports medicine programs - Advanced sports injury and concussion rehabilitation
• Manual-focused practices - Hands-on treatment with telehealth options
• Specialized women's health - Pelvic floor therapy with integrated Pilates
Services Available:
One-on-one manual therapy sessions
Sports injury rehabilitation and return-to-play programs
Pelvic floor therapy and women's health
Telehealth appointments for convenience
Specialized programs (Parkinson's boxing, running analysis, TMJ treatment)
Most clinics accept major insurance plans including Medicare, offer direct access (no prescription needed), and can schedule appointments within 24 hours.
The neighborhood's active culture - from Prospect Park runners to families biking to school - has created demand for physical therapists who understand how movement fits into daily life. These aren't cookie-cutter clinics but practices that have grown roots in the community.
As Lou Ezrick, founder of Evolve Physical Therapy with nearly two decades of experience in chronic pain management and holistic rehabilitation, I've seen how Park Slope physical therapy providers prioritize individualized care over high-volume treatment models. This guide will help you find the right clinic for your specific needs and recovery goals.
Why Physical Therapy Matters in Park Slope
Living in Park Slope means embracing an active lifestyle that revolves around Prospect Park runs, family bike rides, and playground trips. But what happens when pain threatens to sideline you from the neighborhood activities you love? That's where Park Slope physical therapy becomes essential – not just for treating injuries, but for preserving the vibrant way of life that defines this Brooklyn community.
Physical therapy offers proven benefits that go far beyond temporary pain relief. Scientific research on the benefits of physical therapy demonstrates that PT can reduce the need for surgery by up to 60%, decrease reliance on pain medications, and dramatically improve long-term functional outcomes. For Park Slope families, this means getting back to weekend farmers-market walks and keeping up with energetic kids at the playground.
The preventive medicine approach of physical therapy particularly resonates with health-conscious Park Slope residents. Rather than waiting for that nagging back pain to become a chronic problem, many locals use PT for movement screens and ergonomic assessments. This proactive mindset is especially valuable for the neighborhood's many remote workers who've found that their home-office setup is wreaking havoc on their posture.
Aging in place comfortably is another priority for long-time Park Slope residents. Physical therapy helps maintain the mobility and strength needed to steer those beautiful brownstone stairs, carry groceries from the co-op, and continue enjoying neighborhood festivals well into retirement.
From a practical standpoint, choosing local Park Slope physical therapy offers significant cost-effective care advantages. Most neighborhood clinics accept major insurance plans including Medicare, and their transparent pricing makes quality rehabilitation accessible to families at every income level. You're investing in your long-term well-being while supporting the local healthcare ecosystem that keeps this community thriving.
Park Slope Physical Therapy Roundup: Where Recovery Meets Community
The beauty of seeking Park Slope physical therapy lies in the neighborhood's incredible diversity of healing approaches. Walk down any tree-lined street, and you'll find everything from cozy practices that have treated three generations of the same family to sleek modern facilities with the latest recovery technology.
What makes this neighborhood special isn't just the variety - it's how each practice has developed its own personality while staying true to Park Slope's community-focused values. Some clinics have become neighborhood institutions, where therapists know your kids' names and remember your marathon training goals. Others offer boutique experiences with cutting-edge treatments that draw patients from across Brooklyn.
The practical side matters too. Many practices have figured out creative solutions to urban challenges, like partnering with local parking garages or offering weekend hours for busy families. The rise of telehealth options has added another layer of convenience, though the hands-on nature of physical therapy means most of your healing will still happen in person.
Feature In-Person Care Telehealth Options Hands-on manual therapy ✓ Limited Exercise prescription ✓ ✓ Movement assessment ✓ Modified Equipment access ✓ Home alternatives Convenience Scheduled visits Flexible timing Insurance coverage Most plans Growing acceptance
Best All-Around "Neighborhood" Experience for Park Slope Physical Therapy
Some practices just feel like they've grown up with the neighborhood. These are the clinics where three generations of the same family might get treatment, where the front desk staff knows your coffee order, and where therapists understand that your "simple" back pain is actually about keeping up with your toddler at the playground.
Community-rooted practices excel at the human side of healing. They've mastered rapid scheduling because they know that when you're in pain, waiting two weeks isn't an option. Their private treatment rooms provide comfort for sensitive conditions, and their therapists have seen every possible injury that comes from Park Slope's active lifestyle.
The real advantage of these established practices is their deep insurance knowledge and referral networks. They've figured out how to work with every major plan, including Medicare, and they know exactly which local specialists to recommend when you need additional care. It's healthcare that feels personal because it actually is.
Best Boutique & Manual-Therapy Choice for Park Slope Physical Therapy
For those who prefer a more intimate healing experience, Park Slope's boutique practices offer something special. These smaller clinics focus on hands-on manual therapy in private office settings, where your therapist can dedicate their full attention to understanding exactly how your body moves and heals.
The manual therapy approach treats your body like the complex, interconnected system it is. Instead of just addressing symptoms, these practitioners work on the underlying movement patterns and tissue restrictions that create problems in the first place. It's particularly effective for chronic pain conditions that haven't responded well to other treatments.
These boutique practices often blend in-office sessions with video visits for exercise coaching and check-ins. While they might have more limited hours than larger facilities, the trade-off is deeply personalized care that adapts to your specific needs and goals.
Best Sports & Performance Hub for Park Slope Physical Therapy
Park Slope's athletic culture has created demand for specialized sports medicine services that go far beyond basic injury treatment. These performance-focused practices understand that getting back to your weekend warrior activities isn't just about pain relief - it's about returning stronger and smarter than before.
Return-to-play programs here include comprehensive testing to ensure you're truly ready for action. Running analysis helps Prospect Park joggers optimize their form and prevent future injuries. Concussion rehabilitation provides crucial support for athletes of all ages dealing with head injuries.
The equipment at these sports-focused facilities often includes advanced tools like anti-gravity treadmills and blood flow restriction therapy. But what really sets them apart is their understanding of Park Slope's specific athletic culture - they know the difference between training for a local 5K and preparing for your first marathon.
Athlete screening services help prevent injuries before they happen, while performance evaluation programs can help you break through training plateaus. It's the kind of comprehensive approach that turns weekend warriors into lifelong athletes.
Best Pelvic-Health Sanctuary for Park Slope Physical Therapy
The neighborhood's focus on family life has created exceptional pelvic floor therapy options that address everything from prenatal preparation to postpartum recovery. These specialized practices understand that pelvic health affects far more than you might expect - from core strength to overall confidence.
Prenatal and postpartum care at these practices goes beyond traditional physical therapy. Many integrate Pilates and other movement approaches to create comprehensive programs that support you through pregnancy, delivery, and beyond. The private treatment rooms and specially trained therapists create a comfortable environment for addressing sensitive health concerns.
The holistic approach these practices take recognizes that pelvic health is connected to your entire body and overall well-being. They address both the physical and emotional aspects of recovery, which particularly resonates with Park Slope residents who value comprehensive, patient-centered care.
More info about pelvic-floor services can help you understand the full scope of these specialized services and how they might fit into your health journey.
Specialized Therapies Elevating Your Recovery
When you step into a Park Slope physical therapy clinic today, you're entering a world far beyond traditional exercises and ice packs. The neighborhood's therapists have acceptd cutting-edge treatments that address everything from chronic pain to neurological conditions, creating programs that truly transform how people move through their daily lives.
Pelvic floor therapy has become one of the most sophisticated specialties in the area. Whether you're recovering from childbirth, dealing with chronic pelvic pain, or experiencing issues that many people feel too embarrassed to discuss, these specialized programs offer real solutions. The approach goes far beyond basic exercises - it's about restoring confidence and comfort in your own body.
Myofascial release techniques work like magic for many Park Slope residents, especially those spending long hours hunched over laptops. This hands-on therapy breaks up the tight, knotted tissue that develops from poor posture and repetitive stress. Patients often describe feeling like they can finally breathe again after these sessions.
One of the most inspiring programs making waves in the community is Rock Steady Boxing for Parkinson's patients. This isn't your typical physical therapy - it's boxing-based exercises specifically designed to help people with Parkinson's rebuild strength, balance, and coordination. The program has gained so much attention that it was even featured on NBC News, showing how innovative approaches can make a real difference in people's lives.
Vestibular rehabilitation addresses those dizzy spells and balance issues that can make simple activities feel overwhelming. This specialized therapy retrains your inner ear and brain to work together properly, helping you feel steady on your feet again.
Blood flow restriction therapy might sound intimidating, but it's actually a gentle way to build strength using lighter weights. This FDA-approved technique is perfect for people recovering from surgery or dealing with joint pain who can't handle traditional strength training yet.
For Park Slope families, pediatric physical therapy offers hope for children facing developmental challenges. These programs use creative, play-based activities that make therapy feel like fun rather than work. Kids develop strength and coordination while playing games and exploring movement in ways that feel natural to them.
Prehab and post-surgical care keeps active Park Slope residents moving before and after procedures. Manual therapy and active release techniques help restore normal movement patterns that might have been disrupted by injury or surgery.
How Therapists Personalize Care in Park Slope
The best Park Slope physical therapy experiences start with therapists who really listen. Instead of rushing into generic exercises, quality practices begin with detailed conversations about your goals, your daily routine, and what activities matter most to you.
Goal-setting becomes a collaborative process. Maybe you want to run the Brooklyn Half Marathon, keep up with your toddler at the playground, or simply sleep through the night without back pain. Your therapist designs a program around what success looks like for your life specifically.
Movement screens reveal how your body actually moves, not just where it hurts. These assessments often uncover surprising connections - like how tight ankles might be contributing to knee pain, or how desk posture affects shoulder mobility.
Evidence-based treatment forms the foundation, but the magic happens when therapists adapt proven techniques to your unique situation. They understand that your pain has its own personality - its specific triggers, timing, and quirks that make your experience different from everyone else's.
Many practices now use home exercise apps that sync with your treatment plan. These digital tools help busy Park Slope residents stay consistent with their exercises between appointments, turning your smartphone into a personal rehab coach.
Typical Conditions Treated by Park Slope Physical Therapy Experts
The conditions that bring people through the doors of Park Slope clinics tell the story of a neighborhood that refuses to slow down. Back pain tops the list, affecting everyone from weekend cyclists to work-from-home parents who've turned their kitchen table into a permanent office.
Runner's knee and other overuse injuries are practically neighborhood badges of honor, earned through countless loops around Prospect Park. These conditions require therapists who understand not just the injury but the passion that drives people to keep moving despite discomfort.
TMJ disorders have become increasingly common, often linked to stress and the jaw clenching that comes with navigating city life. Treatment involves both hands-on techniques and lifestyle modifications that address the root causes.
Vertigo and balance issues can be particularly frightening in an urban environment where navigating stairs and crowded sidewalks requires confidence in your footing. Specialized vestibular therapy helps people regain that sense of stability.
Chronic pain conditions require a different approach entirely - one that looks beyond symptoms to address the complex factors that keep pain cycles active. Sports injuries range from acute weekend warrior mishaps to more complex conditions requiring careful return-to-play protocols.
Insurance, Payment & Your First Visit
Navigating the financial side of Park Slope physical therapy doesn't have to be complicated. Thanks to New York's direct access laws, you can walk into most clinics without a doctor's prescription - though it's worth checking if your insurance plan requires a referral for coverage.
The good news is that most Park Slope practices work with major insurance plans including Medicare. Workers' compensation cases are also commonly accepted, which is helpful if your injury happened on the job. The expansion of telehealth coverage has been a game-changer, especially for follow-up visits when you just need to review exercises or check in on progress.
Copays vary depending on your specific insurance plan, but most practices have streamlined their billing with online payment systems. Nobody likes financial surprises, so many clinics now provide upfront cost estimates and will work with you on payment plans if needed. It's always worth asking about your options during that first phone call.
Preparing for your first visit is pretty straightforward. You'll need your insurance cards, a valid ID, and any relevant medical records - think MRI results or notes from your doctor if you have them. Most practices suggest arriving 10-15 minutes early to handle paperwork, though many now offer online forms you can fill out from home (much easier when you're dealing with pain).
What to wear is simple: comfortable clothing that lets you move easily. Think athletic wear or loose-fitting clothes - you want your therapist to see how you move naturally. Non-skid shoes are essential for safety during movement assessments and exercises. Nobody wants to slip during their first evaluation!
The atmosphere at most Park Slope practices is welcoming and relaxed. Your therapist will likely spend time understanding not just your injury, but how it affects your daily life - whether that's chasing kids around Prospect Park or sitting at a desk all day.
More info about coverage provides additional details about insurance and payment options to help you plan ahead.
Frequently Asked Questions about Park Slope Physical Therapy
Do I need a doctor's prescription?
Here's some good news: New York's direct access laws mean you can walk into any Park Slope physical therapy clinic without a doctor's prescription. It's that simple. You can literally wake up with back pain and be in treatment the same day.
But here's the catch - while you don't need a prescription, your insurance company might have other ideas. Some plans still require a referral before they'll cover your visits. The smart move? Call your insurance provider or ask the clinic to check your coverage before your first appointment. Most Park Slope physical therapy practices are pros at navigating insurance requirements and can save you from any surprise bills.
How soon can I get an appointment?
If you're used to waiting weeks for medical appointments, you're in for a pleasant surprise. Many Park Slope practices can get you in within 24 hours, especially for urgent issues. That nagging shoulder pain from sleeping wrong? You could be getting treatment tomorrow.
The timeline really depends on your schedule flexibility and which clinic you choose. Some practices reserve slots for urgent cases, while others offer telehealth consultations that can happen even faster than in-person visits. During busy periods (hello, post-New Year's resolution season), you might wait a few days, but it's rarely the weeks-long wait you'd expect elsewhere.
Pro tip: if you're flexible with timing, mentioning you can take a last-minute cancellation often gets you in sooner.
What should I wear and bring?
Think "comfortable gym clothes" and you're 90% there. Loose-fitting athletic wear or anything that lets you move freely works perfectly. Skip the jeans and button-down shirts - your therapist needs to see how your body moves, and tight clothes just get in the way.
Non-skid shoes are essential for safety during movement tests and exercises. Those fancy leather loafers might look great, but they'll have you slipping around during balance assessments.
For paperwork, bring your insurance card, a valid ID, and a list of current medications. If you have any MRI results, X-rays, or medical records related to your condition, toss those in your bag too. Many practices now let you fill out forms online ahead of time, which saves you from arriving early just to tackle paperwork.
Some clinics provide gowns or shorts if needed for specific evaluations, but it's always better to come prepared. When in doubt, call ahead - the front desk staff are usually happy to walk you through exactly what to expect for your specific appointment.
Conclusion & Next Steps Toward Pain-Free Living
Your journey to better movement and less pain doesn't have to be complicated. Park Slope physical therapy offers something special - a chance to work with practitioners who truly understand how you live, move, and thrive in Brooklyn.
Think about it: your physical therapist should know what it's like to steer the 7th Avenue subway entrance with a sore back, or understand why missing your morning Prospect Park run affects your entire day. That's the difference local care makes.
The neighborhood's therapy practices have grown alongside the community, developing programs that fit real life. Whether you're dealing with runner's knee from those weekend long runs or chronic desk pain from working at home, these aren't cookie-cutter treatments. They're solutions designed around how Park Slope residents actually live.
Many practices go beyond individual appointments to offer community workshops and injury prevention seminars. Some host wellness events that bring neighbors together around shared health goals. It's healthcare that builds connections, not just fixes problems.
At Evolve Physical Therapy + Sports Rehabilitation, we've spent nearly two decades learning how holistic care can change everything - not just your pain levels, but how you move through your daily life. Our hands-on manual therapy approach combined with specialized programs like Rock Steady Boxing for Parkinson's patients (which even caught NBC News' attention) shows how innovative care can address both immediate concerns and long-term wellness.
The best part? Getting started is easier than you might think. Most Park Slope practices can schedule you within 24 hours, and thanks to New York's direct access laws, you don't need to wait for a doctor's referral. Your insurance likely covers care, and many clinics accept everything from major plans to Medicare.
Ready to take that first step? Start by thinking about what you really want - maybe it's getting back to those Saturday morning bike rides with your family, or simply being able to carry groceries without wincing. Then reach out to a practice that feels right for your style and needs.
Your path to pain-free living is waiting, and in Park Slope, you have access to some of Brooklyn's most thoughtful, skilled practitioners to guide you there. More info about getting started in Park Slope can help you begin today.
Is There Treatment for Parkinson Disease? Your Essential Guide
Understanding Your Treatment Options for Parkinson's Disease
Is there treatment for Parkinson disease? Yes, there are multiple effective treatments available that can significantly improve symptoms and quality of life, though there is currently no cure for the disease.
Quick Answer:
• Medications - Levodopa, dopamine agonists, and other drugs can control motor symptoms
• Surgery - Deep brain stimulation helps when medications become less effective • Therapy - Physical, occupational, and speech therapy maintain function and mobility
• Exercise - Regular activity may slow progression and improve symptoms
• Lifestyle changes - Diet, sleep, and stress management support overall health
Parkinson's disease affects nearly 1 million Americans, with symptoms appearing only after about 60-80% of dopamine-producing brain cells are already lost. While this progressive neurological condition causes tremors, stiffness, and movement difficulties, early intervention with the right treatment combination can help people maintain their independence and active lifestyles for years.
The key is understanding that Parkinson's treatment isn't one-size-fits-all. As research shows, people who start exercising at least 2.5 hours per week early in their disease experience slower decline in quality of life. Similarly, deep brain stimulation provides meaningful improvement in 90% of severe cases, often eliminating tremors completely.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience helping people with neurological conditions, including those asking is there treatment for Parkinson disease regain function and improve their quality of life. Through my work at Evolve Physical Therapy, I've seen how the right combination of treatments can transform outcomes for people with Parkinson's.
Understanding Parkinson's Disease and Why Treatment Matters
When people ask "is there treatment for Parkinson disease?" it helps to know what we are treating. Parkinson’s begins when dopamine-producing cells in the substantia nigra die off; by the time the first tremor appears, about 60-80 % of those cells are already gone. Roughly 1 % of adults over 60 live with the disease, and 5-10 % develop symptoms before age 50.
Parkinson’s shows up as both motor and non-motor problems: • Tremor, stiffness, slowed movement (bradykinesia) and balance changes
• Loss of smell, constipation, mood changes or sleep trouble that can precede motor signs
Typical day-to-day effects include handwriting that shrinks (micrographia), reduced arm swing, softer voice, depression or acting out dreams during sleep.
Why Early, Multidisciplinary Care Helps
Data from the Parkinson's Outcomes Project show that people who connect with a complete care team early stay independent longer. A movement-disorder neurologist handles medication; physical, occupational and speech therapists keep you moving, functioning and communicating; mental-health and nutrition specialists address mood, sleep and digestion. Shared decision-making keeps treatment aligned with personal goals—whether that means gardening, working or playing with grandchildren.
Is There Treatment for Parkinson Disease?
Absolutely. Modern care blends medication, therapy, lifestyle change and, when needed, surgery so people can stay active for decades.
Medications: First-Line Answers
Drug class Purpose Examples Key points Levodopa + carbidopa Replaces dopamine Sinemet, Rytary Most effective; motor fluctuations over time Dopamine agonists Mimic dopamine pramipexole, ropinirole, rotigotine patch Useful early or with levodopa; watch impulse control MAO-B inhibitors Slow dopamine breakdown rasagiline, selegiline, safinamide Mild benefit; once daily COMT inhibitors Extend levodopa effect entacapone, tolcapone Added when doses wear off too fast Other agents Target specific issues amantadine, trihexyphenidyl, pimavanserin Help with dyskinesia, tremor or hallucinations
Fine-tuning dose size and timing often smooths “wearing-off” periods without new drugs.
Surgical Interventions
• Deep Brain Stimulation (DBS) – adjustable electrical pulses delivered through electrodes in the subthalamic nucleus or globus pallidus can cut tremor, rigidity and dyskinesias and let many patients lower medication. See NICE guidance on DBS.
• Focused ultrasound or lesion surgery – non-invasive options for people who cannot have DBS.
• Intestinal levodopa infusion (Duopa pump) – steady medication flow to reduce peaks and valleys.
Supportive & Rehabilitative Therapies
Medications treat chemistry; therapy treats function. At Evolve we combine large-amplitude gait training, balance work and voice programs like LSVT LOUD to help clients:
Walk farther with fewer falls
Handle daily tasks such as dressing or writing
Speak clearly and swallow safely
Creating Your Personalized Parkinson's Treatment Plan
When you're facing a Parkinson's diagnosis, one of the first questions that comes to mind is "is there treatment for Parkinson disease that will work for me?" The answer depends on creating a treatment plan that's as unique as you are.
Your age makes a big difference in how we approach treatment. If you're in your 40s or 50s, you might be worried about staying productive at work or keeping up with your kids' activities. We'll focus on treatments that help you maintain those important roles. If you're in your 70s or 80s, your priorities might center more on staying safe at home and maintaining your independence.
The stage of your disease also shapes your treatment options. Early on, you might do well with a single medication and some targeted physical therapy. As symptoms progress, we typically need to get more creative with combination approaches - maybe adding a second medication or introducing specialized exercise programs.
Your other health conditions matter too. If you have heart problems or diabetes, some Parkinson's medications might not be the best fit. That's why your neurologist needs to see the whole picture of your health, not just your Parkinson's symptoms.
Here's something I've learned after nearly 20 years of working with people who have Parkinson's: your lifestyle goals should drive your treatment decisions. If you love gardening, we'll focus on treatments that help preserve your fine motor skills and balance. If walking your dog around the neighborhood is what matters most, we'll prioritize medications and therapies that keep you mobile and steady on your feet.
The beauty of modern Parkinson's care is that we can adjust your treatment as your needs change. Regular check-ins with your care team ensure that your medications and therapies continue to match your evolving symptoms and goals.
Technology is becoming a helpful partner in this process. Telehealth appointments make it easier to stay connected with your neurologist between visits. Wearable devices can track your movement patterns throughout the day, giving us objective data about how well your treatments are working.
Working With Your Healthcare Team
Think of your Parkinson's care team as your personal support squad. Each member brings something different to the table, and together, they help you tackle this disease from every angle.
Your neurologist or movement disorder specialist is like the conductor of an orchestra - they coordinate everything and make sure all the different treatments work together harmoniously. These doctors have spent extra years learning specifically about Parkinson's disease, so they know the latest medications and treatment strategies.
As a physical therapist who specializes in neurological conditions, I see my role as helping you move better and feel more confident in your body. We work on big, exaggerated movements that can help overcome the small, shuffling steps that Parkinson's often causes. Balance training becomes crucial because we want to keep you on your feet and prevent falls. More info about Physical Therapy for Neurological Therapy explains how our specialized approach can make a real difference in your daily life.
Your dietitian helps steer the tricky relationship between food and medications. Some Parkinson's drugs work better on an empty stomach, while protein can interfere with levodopa absorption. They also help with common issues like constipation and unintended weight loss or gain.
Don't underestimate the importance of a mental health provider on your team. Living with Parkinson's brings emotional challenges that are completely normal but often overlooked. Depression and anxiety are common, and addressing them can actually improve your physical symptoms too.
The magic happens when everyone on your team talks to each other. That's why many of us use shared electronic medical records and coordinate our recommendations. It prevents you from getting conflicting advice and ensures everyone is working toward the same goals.
Tracking Symptoms and Adjusting Over Time
Here's something that might surprise you: managing Parkinson's is as much about good detective work as it is about medical treatment. The more information you can gather about your symptoms, the better your doctors can fine-tune your care.
The MDS-UPDRS scale sounds complicated, but it's really just a systematic way for your medical team to measure how Parkinson's is affecting different aspects of your life. It looks at everything from how well you can button your shirt to how your mood has been lately.
Keeping a medication diary might feel tedious at first, but it becomes incredibly valuable. Write down when you take each dose, when you feel your best, and when symptoms return. Note any side effects too. This information helps your neurologist adjust timing and dosages to give you more "good" hours each day.
Wearable sensors and smartphone apps are getting pretty sophisticated these days. Some can detect tremor patterns or changes in your walking speed that you might not notice yourself. While they're not perfect, they can provide helpful objective data for your doctor visits.
Your care partner - whether that's a spouse, adult child, or close friend - often sees things you might miss. They might notice that your voice has gotten softer or that you're having more trouble with certain tasks. Their observations are incredibly valuable, so don't hesitate to bring them to appointments when possible.
Adjusting your treatment isn't a sign that something's wrong - it's a sign that your team is staying on top of the disease and adapting to keep you feeling your best.
Lifestyle, Exercise, and Complementary Approaches
Drugs change brain chemistry; lifestyle changes strengthen the whole system.
Exercise: The Game-Changer
People who move at least 150 minutes a week keep abilities longer. Choose what you enjoy: • Brisk walking, cycling or swimming
• Rock Steady Boxing for power, balance and voice
• Tai chi, yoga or dance for flexibility, rhythm and social connection
Nutrition & Daily Habits
• Mediterranean-style diet supplies antioxidants and healthy fats
• Take levodopa 30–60 minutes before high-protein meals for better absorption
• 25–35 g fiber + plenty of water fight constipation
• Consistent sleep schedule and a cool, dark room improve rest
• Mindfulness, massage or breathing exercises reduce stress-related symptom flare-ups
Omega-3s and vitamin D may help, but always clear supplements with your healthcare team.
Emerging Research and Clinical Trials
Parkinson’s science is accelerating:
• Gene-therapy trials deliver enzymes that boost dopamine production
• Stem-cell studies aim to replace lost neurons
• Adaptive DBS devices adjust stimulation in real time
• Alpha-synuclein assays may allow diagnosis before symptoms
• New levodopa formulations (ABBV-951, IPX203) await FDA review
Interested in participating? Search ClinicalTrials.gov or contact the Parkinson’s Foundation or Michael J. Fox Foundation for local studies. Enrollment is voluntary and involves detailed informed consent.
More info about Parkinson's Disease Can Be Conquered
Frequently Asked Questions about Treating Parkinson's Disease
Is there a cure for Parkinson's disease?
No, there isn't a cure for Parkinson's disease yet - but that doesn't mean you should lose hope. While we can't reverse or completely stop the disease, the treatments available today can make a tremendous difference in how you feel and function day-to-day.
I've worked with hundreds of people with Parkinson's over the years, and I've seen patients who were diagnosed decades ago still living independently and enjoying activities they love. The key is understanding that "Is there treatment for Parkinson disease?" has a resounding yes answer, even without a cure.
What we have now are highly effective symptom management strategies. Medications can dramatically reduce tremors and stiffness. Deep brain stimulation can eliminate tremors completely in many cases. Physical therapy and exercise programs like our Rock Steady Boxing can help you maintain strength, balance, and confidence.
The research pipeline is also incredibly promising. Gene therapy trials are showing early success, and scientists are getting closer to treatments that might actually slow down disease progression. Some researchers believe we're within reach of turning Parkinson's into a manageable chronic condition rather than a progressive one.
When should medication treatment begin?
This is one of the most common questions I hear from newly diagnosed patients, and honestly, there's no universal answer. The decision to start medications depends entirely on how symptoms are affecting your daily life and what matters most to you.
Some people start medications as soon as they're diagnosed because they want to maintain their current level of function at work or in activities they enjoy. Others prefer to wait until symptoms become more bothersome, especially if they're concerned about potential side effects or want to delay the eventual complications that can come with long-term medication use.
Your movement disorder specialist will help you weigh these factors. They'll consider things like your age, how fast your symptoms are progressing, what your work and family responsibilities look like, and your personal preferences about medication.
The good news is that starting medications doesn't have to be permanent or set in stone. You can always adjust the approach as your needs change. I've seen patients successfully manage early symptoms with exercise and therapy alone, then add medications when they feel ready.
Can lifestyle changes slow disease progression?
This is where the science gets really exciting, and it's honestly one of my favorite topics to discuss with patients. Yes, lifestyle changes - especially exercise - appear to actually slow down Parkinson's progression, not just make you feel better in the moment.
The research on exercise is particularly compelling. Studies show that people who exercise at least 2.5 hours per week early in their disease experience slower decline in quality of life compared to those who start exercising later. That's not just about feeling stronger - that's about the disease itself progressing more slowly.
We see this in our Rock Steady Boxing program here in Brooklyn. Participants often tell us they feel like they're fighting back against the disease, and in many ways, they really are. The high-intensity, large-amplitude movements seem to help maintain neural connections and even promote the growth of new ones.
Nutrition also plays a role, though it's less dramatic than exercise. The Mediterranean diet with its emphasis on antioxidants and healthy fats supports brain health. Good sleep hygiene helps with the fatigue and mood issues that often accompany Parkinson's.
The important thing to understand is that lifestyle changes work best alongside medical treatment, not instead of it. Think of it as giving your brain every possible advantage in this fight. When patients ask "Is there treatment for Parkinson disease?" I always emphasize that the most effective approach combines the best of medical science with the power of an active, healthy lifestyle.
Conclusion & Next Steps
Is there treatment for Parkinson disease? Absolutely. While we don't yet have a cure, the combination of medications, surgical interventions, rehabilitative therapies, and lifestyle modifications can dramatically improve symptoms and maintain quality of life for years after diagnosis.
At Evolve Physical Therapy + Sports Rehabilitation, we take a holistic approach to Parkinson's care that goes beyond traditional physical therapy. Our specialized programs, including Rock Steady Boxing, address the unique challenges of Parkinson's disease while building strength, confidence, and community among our patients.
The key to successful Parkinson's treatment lies in early intervention, comprehensive care, and ongoing adaptation as the disease evolves. No single treatment works for everyone, but the right combination of interventions can help you maintain independence and continue enjoying the activities that matter most to you.
Our team in Brooklyn - serving Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin - understands that living with Parkinson's affects not just patients but entire families. We work closely with each person to develop personalized treatment plans that address individual symptoms, goals, and lifestyle needs.
If you or a loved one is facing a Parkinson's diagnosis, you're not alone in this journey. With the right treatment team and comprehensive approach, it's possible to live well with Parkinson's disease. More info about Parkinson's physical therapy programs can help you take the next step toward better symptom management and improved quality of life.
The future of Parkinson's treatment continues to evolve, with new medications, technologies, and approaches constantly in development. By staying informed, working with specialized healthcare providers, and maintaining an active lifestyle, people with Parkinson's can look forward to continued improvements in treatment options and outcomes.
How to Treat Labral Tears with Physical Therapy: 5 Effective Methods
Understanding Labral Tears: When Cartilage Causes Pain
Physical therapy for labral tears is an effective first-line treatment that can reduce pain, improve function, and potentially help patients avoid surgery. Here's what you need to know:
Physical Therapy for Labral Tears: Quick Facts • Can occur in both hip and shoulder joints • Conservative PT management helps 50% of patients avoid surgery • Typical PT program lasts 10-12 weeks • Includes manual therapy, stretching, strengthening, and education • Post-surgical PT rehabilitation takes 9-12 months for complete healing
A labral tear is damage to the ring of cartilage (labrum) that surrounds either your hip socket (acetabulum) or shoulder socket (glenoid). This specialized cartilage deepens the socket, provides stability, and helps distribute pressure evenly across the joint.
Studies show that labral tears are present in up to 22% to 55% of patients with mechanical hip pain, while shoulder labral tears are common in athletes and individuals who perform repetitive overhead activities.
The good news? Physical therapy for labral tears offers hope. A well-designed PT program can significantly improve symptoms, with research showing that up to 50% of patients can avoid surgery through conservative management.
"When your labrum tears, it can lead to pain and disability—exercises that stretch and strengthen the joint can effectively decrease both."
I'm Lou Ezrick, founder of Evolve Physical Therapy, with nearly two decades of experience treating complex orthopedic conditions including labral tears; my approach to physical therapy for labral tears combines manual therapy techniques with targeted exercise progressions to restore function and reduce pain.
Method 1: Accurate Evaluation & Diagnosis
Getting to the root of your pain starts with an accurate diagnosis. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we begin with a thorough evaluation to determine if you're dealing with a labral tear and understand its severity.
Clinical Tests That Matter
For hip labral issues, we perform specialized tests like the FADIR test, which often reproduces pain if a tear is present. The FABER test helps distinguish between labral problems and other issues like sacroiliac joint dysfunction. A simple resisted straight leg raise can reveal labral tears, particularly those involving the acetabular rim.
For shoulder labral tears, O'Brien's Active Compression Test is effective for detecting SLAP tears. The Crank Test involves compressing your shoulder joint while rotating it to check for labral damage. For suspected anterior labral tears (Bankart lesions), apprehension and relocation tests help confirm our suspicions.
Diagnostic Method Sensitivity Specificity Best For Physical Exam Tests 70-85% 65-80% Initial screening MRI 66-79% 80-90% Soft tissue assessment MR Arthrography 90-95% 85-95% Gold standard for labral tears Diagnostic Injection 85-90% 85-90% Confirming pain source
Why Early Imaging Matters
MR arthrography—an MRI with contrast injected directly into your joint—provides the highest diagnostic accuracy for labral tears. This detailed imaging helps us confirm the tear's location and extent, and spot accompanying issues like femoroacetabular impingement (FAI) in hip cases or rotator cuff damage in shoulders.
Screening for Surgical Red Flags
While many labral tears respond to conservative care, certain situations may indicate a need for surgical consultation: joint locking or catching, significant instability (particularly in the shoulder), large displaced tears, or severe bony abnormalities that will continue damaging your labrum. If you've given physical therapy for labral tears a solid 8-12 weeks without improvement, it might be time to explore other options.
Method 2: Pain Relief & Joint Protection in the Acute Phase
Once diagnosed, the initial phase of physical therapy for labral tears focuses on controlling pain and protecting the joint from further damage.
Activity Modification Strategies
The first step is giving your body a chance to calm down. For hip labral tears, avoid deep squatting, prolonged sitting, and quick pivoting movements. With shoulder labral tears, reaching overhead or lifting heavy objects can worsen the condition.
Depending on severity, we might recommend crutches for 1-2 weeks for hip tears, or a brief period with a sling for shoulder tears.
Physical Therapy for Labral Tears: Early Goals
During the first couple of weeks, we focus on:
Reducing inflammation: Ice therapy (15 minutes, 3-4 times daily) can significantly decrease pain levels
Protecting injured tissue: Learning movement patterns that don't stress your labrum
Maintaining mobility in surrounding joints
Gentle isometric exercises to maintain strength without stressing the tear
Scientific research on non-operative management confirms these early interventions can dramatically reduce pain and create the foundation for successful healing.
Movements to Avoid with a Fresh Tear
For hip labral tears, avoid deep hip flexion beyond 90 degrees, combinations of flexion, adduction, and internal rotation, and high-impact activities like running or jumping.
For shoulder labral tears, avoid reaching overhead, heavy lifting, and quick rotational movements like throwing or tennis serves.
"Finding the sweet spot between rest and movement is the art of early labral tear management," explains our team. "Too much stillness leads to stiffness, but pushing too hard can set you back weeks."
Method 3: Physical Therapy for Labral Tears – Mobility Restoration with Manual Therapy
As pain and inflammation subside, we focus on restoring normal movement through hands-on care and targeted exercises.
Hands-On Techniques That Work
For hip labral tears, we use grade I-IV joint glides and hip distraction techniques to create space in the joint. Many patients describe this as feeling like "finally being able to take a deep breath" in their hip.
With shoulder labral tears, we focus on posterior-to-anterior glides (especially helpful for anterior tears) while working on your shoulder blade (scapula) to ensure proper movement of the entire shoulder complex.
"The magic often happens when we combine these techniques with gentle contract-relax stretching," explains Lou, our founder. "It's like we're having a conversation with your nervous system, asking it to let go of unnecessary tension."
Stretching & Range-of-Motion Drills
For hip labral tears, child's pose rock backs create space in your hip joint without aggravating the tear, while dynamic pigeon pose variations gradually expand your range.
For shoulder labral tears, wall stretches and the cross-body stretch are remarkably effective when performed correctly.
"Stretching should never cause sharp pain," we remind our patients. "You're looking for a gentle pull, not a painful tug."
Our approach also addresses thoracic and lumbar mobility, which directly impacts how your hip or shoulder functions. Research shows this progressive, gentle mobility work improves range of motion and helps manage pain by improving joint nutrition and reducing stiffness.
Want to learn more about post-surgical rehab? Check out our detailed information about post-surgical rehab for labral tears.
Method 4: Progressive Strengthening & Motor Control
As mobility improves, strengthening becomes the focus of physical therapy for labral tears. This phase is critical for providing stability to the injured joint and preventing recurrence.
Core Foundation First
Before targeting the specific joint, we build a strong foundation with fundamental exercises like dead bug, bird dog, and carefully progressed planks. We also focus on pelvic and scapular control, as these connecting areas significantly influence shoulder and hip function.
Physical Therapy for Labral Tears: Key Exercises
For hip labral tears, we focus on:
Clam shells (3 sets of 15-20 repetitions) to target the gluteus medius
Single-leg bridges to strengthen glutes while teaching proper hip control
Monster walks with resistance bands
Side-lying leg lifts to build strength in multiple planes of movement
For shoulder labral tears, we emphasize:
External rotation exercises using light resistance bands
Prone row to external rotation to reinforce proper shoulder mechanics
"Many patients are surprised by how much better they feel once we establish proper strength around the joint," says Lou Ezrick. "It's about teaching the right muscles to fire at the right time."
Progression Principles
Your strengthening program will follow these key principles:
Start in supported positions before standing exercises
Progress from isometric to dynamic movements
Advance from closed-chain to open-chain exercises
Gradually increase load starting with bodyweight before introducing bands and weights
Focus on eccentric control for tendon strength and joint control
"Proper form is more important than the amount of weight or number of repetitions," our team reminds patients.
Return-to-Function Milestones
We track specific milestones including range of motion (at least 75% of normal early in treatment), pain levels (2/10 or less during daily activities), functional tests like pain-free single-leg squats, and strength symmetry (90% compared to your unaffected side).
Research published in the Journal of Orthopaedic & Sports Physical Therapy confirms that patients who achieve these milestones have significantly better long-term results and lower recurrence rates.
Method 5: Sport-Specific Conditioning & Prevention Strategies
The final phase of physical therapy for labral tears prepares you to return to the activities you love while ensuring you stay injury-free.
Advanced Exercise Progression
Once you've built a solid foundation, we help you progress with:
Plyometric training: Starting with gentle double-leg jumps before advancing to single-leg hops
Agility drills: Side-to-side movements and controlled directional changes
Sport-specific movement patterns customized to your activities
For overhead athletes with shoulder labral tears, we implement a structured throwing program that gradually increases distance, speed, and volume.
Movement Retraining
We use video analysis to identify problematic movement patterns and implement neuromuscular training to improve body awareness and joint position sense. Our fatigue-resistant training teaches your body to maintain proper form even when tired, which is when most injuries occur.
Ergonomic and Equipment Modifications
We'll help you adjust your workspace setup to reduce joint strain, optimize your sleep positioning, and evaluate your sports equipment to ensure it's not contributing to your problem.
Criteria for Return to Play
We measure readiness to return to sports through:
Functional test scores like the iHOT-33 for hip or ASES for shoulder (90% or higher)
Strength at least 90% compared to your unaffected side
Movement quality during sport-specific activities
Psychological readiness and confidence in your body's ability
Long-Term Injury Prevention
We'll design a maintenance exercise program (15-20 minutes, 2-3 times weekly), recommend periodic "tune-up" visits during competitive seasons, teach activity modification strategies, and offer preseason screening to identify risk factors before they lead to injury.
Want to learn more about recovery over time? Check out our detailed labral tear recovery timeline.
Frequently Asked Questions about Physical Therapy for Labral Tears
How long does recovery take with conservative care?
A comprehensive physical therapy for labral tears program typically spans about 10-12 weeks, though individual timelines vary based on the tear's location and severity, additional issues like FAI or rotator cuff damage, your age, activity level, and exercise compliance.
Many patients notice real improvements within 4-6 weeks. Research shows that nonoperative management of femoroacetabular impingement (a common cause of labral tears) leads to significant improvements for 70% of patients.
When is surgery the better option?
Surgery might be the right choice if you're dealing with:
Large, displaced tears causing catching or locking sensations
Tears alongside substantial bony abnormalities
Persistent symptoms despite 3-4 months of dedicated therapy
High-level athletic demands requiring quicker return to sport
Significant joint instability, particularly in the shoulder
Even when surgery becomes necessary, physical therapy remains crucial both before and after the procedure.
Can a labral tear heal without physical therapy?
The labrum has limited blood supply, affecting its healing capacity. While small tears might become less painful over time with rest alone, without proper rehabilitation:
Your body develops compensation patterns that can create new problems
Muscle weakness and imbalances often persist, increasing re-injury risk
Underlying factors that contributed to your tear remain unaddressed
Research consistently shows that a structured physical therapy for labral tears program significantly improves outcomes compared to rest alone.
Conclusion: The Evolve Approach to Labral Tear Recovery
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe in treating you as a whole person, not just your symptoms. Our approach to physical therapy for labral tears is customized to your unique needs.
We start with a thorough evaluation using specialized clinical tests and appropriate imaging when necessary. From there, we craft an individualized treatment plan whether you're dealing with a hip labral tear from weekend activities or a shoulder tear from swimming.
Our hands-on manual therapy techniques improve joint mobility, calm irritated tissues, and address compensatory patterns. As you progress, your exercises will advance from basic activation to sport-specific training, each step building on the last.
We empower you with knowledge about your condition, helpful movements, and strategies to manage flare-ups, putting you in control of your recovery.
Our Brooklyn neighbors—from Marine Park to Park Slope, Gravesend to Midwood, and Mill Basin—have found their way back to pain-free living through our program. Some have avoided surgery entirely, while others have achieved optimal outcomes after surgical intervention.
Whether you're a competitive athlete eager to return to your sport, a professional who wants to sit through meetings without pain, or a grandparent who misses lifting your grandchildren, we're committed to helping you achieve your goals.
Time matters with labral tears—the sooner you begin appropriate treatment, the better your outcomes typically are. Contact Evolve Physical Therapy + Sports Rehabilitation today to schedule your comprehensive evaluation and take that important first step toward reclaiming your active, pain-free life.
More info about our physical therapy for labral tears services
The Definitive Guide to Understanding Anterior Hip Pain Causes
Understanding the Pain at the Front of Your Hip
Anterior hip pain is discomfort experienced at the front of the hip joint, where your thigh meets your pelvis. If you're experiencing this type of pain, here's what you need to know:
Common Causes of Anterior Hip Pain:
Hip osteoarthritis (most common in adults over 50)
Femoroacetabular impingement (FAI)
Labral tears
Hip flexor strain or tendinopathy
Iliopsoas bursitis
Stress fractures
Acetabular dysplasia
Nerve entrapment
Anterior hip pain affects people of all ages and activity levels, from young athletes to older adults. The lifetime risk for developing hip osteoarthritis—a leading cause of anterior hip pain—is 18.5% for men and 28.6% for women. For active individuals, hip and groin injuries represent between 28-55% of injuries in sports like soccer.
The pain may present as a deep ache in the groin, sharp pain with certain movements, or discomfort that worsens with activities like running, squatting, or prolonged sitting. Many patients describe pointing to the pain using what clinicians call the "C-sign"—cupping their hand around the front of the hip.
Understanding the true source of your anterior hip pain is crucial because treatment varies significantly depending on the underlying cause. While soft tissue problems like muscle strains may respond well to stretching and strengthening, joint-related issues often require different approaches.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've helped thousands of patients overcome anterior hip pain through a comprehensive, hands-on approach that addresses not just symptoms but the root causes of hip dysfunction.
Why This Guide Matters
Hip pain can be confusing and frustrating. With so many potential causes and structures in a relatively small area, getting the right diagnosis and treatment plan is essential for recovery. This comprehensive guide will help you:
Understand the complex anatomy of the hip and what might be causing your pain
Recognize symptoms that suggest specific conditions
Learn about evidence-based assessment and treatment approaches
Find strategies to prevent recurrence and maintain hip health
Whether you're an athlete dealing with a sudden injury, someone experiencing gradual onset of pain, or simply looking to understand hip pain better, this guide provides the information you need to take control of your hip health.
Understanding Anterior Hip Pain: Definition & Key Anatomy
Anterior hip pain refers to discomfort felt at the front of your hip. If you're pointing to the area where your thigh meets your pelvis, or that crease at the front of your hip, you're identifying the anterior hip region. This area stretches from your pubic bone in the middle to the prominent hip bone (anterior superior iliac spine) on the side, and from your lower abdomen down to about 2-4 inches into your thigh.
Your hip is an engineering marvel – a perfect ball-and-socket joint where the round head of your thigh bone (femur) fits snugly into the cup-shaped socket (acetabulum) in your pelvis. This design gives you incredible freedom of movement while keeping everything stable. It's like having a golf ball sitting in a tee, but with muscles, ligaments, and cartilage holding everything together perfectly.
When we look at the anatomy around the front of the hip, several key structures can contribute to anterior hip pain:
The acetabulum (your hip socket) and femoral head (the ball) form the main joint
A ring of tough cartilage called the labrum surrounds your socket, deepening it and creating suction for added stability
The joint capsule, a strong fibrous envelope, wraps around the entire joint
Your iliopsoas muscle (a major hip flexor) runs across the front of your hip and helps you lift your leg
The rectus femoris (part of your quadriceps) crosses the front of your hip and helps with both hip flexion and knee extension
Several bursae (fluid-filled cushions) reduce friction between moving tissues
The front of your hip is also home to important blood vessels and nerves, including the femoral nerve, artery, and vein – your body's superhighway to and from your leg.
Common Symptoms of Anterior Hip Pain
When people visit us at Evolve Physical Therapy with anterior hip pain, they typically describe some familiar patterns:
Many report a deep ache in the groin that can be hard to pinpoint. We often see what we call the "C-sign" – where patients cup their hand in a C-shape around the front of their hip to show where it hurts. This gesture is so common it's become a clinical clue!
Morning stiffness or stiffness after sitting is another telltale sign. You might notice this when getting up from your desk or out of your car after a long drive.
Clicking, catching, or a feeling that something is "out of place" can signal problems with the labrum or joint surfaces. Some patients even experience a sensation of the hip "giving way" during activities.
Certain movements typically make anterior hip pain worse. These include bringing your knee toward your chest, turning your leg inward, squatting deeply, or climbing stairs. Many runners find their pain increases with distance, while office workers might struggle most after long periods of sitting.
Differentiating Anterior Hip Pain from Lateral & Posterior Presentations
Hip pain isn't one-size-fits-all – where it hurts gives us important diagnostic clues. Here's how anterior hip pain differs from pain in other parts of the hip:
Location Typical Pain Area Common Causes Key Features Anterior (Front) Groin, front of thigh Osteoarthritis, FAI, labral tears, hip flexor strain C-sign, pain with hip flexion and internal rotation Lateral (Side) Outer hip, greater trochanter Greater trochanteric pain syndrome, gluteus medius tendinopathy, IT band syndrome Pain lying on affected side, pain with side-stepping Posterior (Back) Buttock, back of hip Piriformis syndrome, ischiofemoral impingement, hamstring tendinopathy, referred lumbar pain Pain with sitting, deep squat, or stretching hamstrings
What makes diagnosis tricky is that pain can be referred from one area to another. Your brain sometimes gets confused about where pain is coming from! Hip joint problems can send pain down to your knee. Back issues can make your hip hurt. And hip problems can disguise themselves as groin pain.
At Evolve Physical Therapy in Brooklyn, our detailed assessment helps untangle these complex relationships. We look at the whole picture – not just where it hurts, but how it hurts, when it started, and what makes it better or worse – to get to the true source of your anterior hip pain.
Top Causes of Anterior Hip Pain (Joint, Soft Tissue, Bone, Nerve)
That nagging pain at the front of your hip can come from many different sources. Understanding what's causing your anterior hip pain is the first step toward effective treatment. Let's explore the most common culprits:
Joint-Related Drivers
When we talk about joint-related causes of anterior hip pain, we're looking at problems with the ball-and-socket connection and its surrounding structures.
Hip Osteoarthritis (OA) is the most common joint-related cause, especially if you're over 50. This progressive wearing down of cartilage affects nearly 1 in 10 adults over age 45, with a lifetime risk of 25% by age 85. You might notice morning stiffness, pain that gets worse with activity but then improves, and gradually decreasing range of motion. X-rays typically show narrowing joint spaces, bone spurs, and increased bone density beneath the cartilage.
Ever heard of Femoroacetabular Impingement (FAI)? This condition occurs when the hip bones don't fit together perfectly. There are three types: cam (extra bone on the femoral head/neck), pincer (overcoverage of the socket), and mixed (both problems together). FAI is particularly common in young active adults—especially athletes. Research shows cam deformities appear in 41% of male soccer players compared to just 17% of non-athletes. According to scientific research on cam morphology, unfortunately, FAI often leads to early arthritis, with 6-25% developing OA within 5-19 years.
Labral tears affect the fibrocartilage ring around your hip socket. They're found in about 64% of people with hip pain, though interestingly, they're also present in 54% of people without symptoms! These tears often occur alongside FAI and typically cause catching, locking, and pain with pivoting movements. If you're experiencing these symptoms, your labrum might be compromised.
The ligamentum teres is a small but important ligament connecting your femoral head to the acetabulum. Tears here are present in nearly half of painful hips but only 2% of pain-free hips. These tears create a deep groin pain and feelings of instability, and when combined with labral tears, they increase the risk of needing surgery by 16 times.
Rounding out our joint-related causes are synovitis and capsular issues—inflammation of the joint lining or capsule that can result from trauma, overuse, or underlying conditions. These typically cause diffuse pain and restricted movement due to discomfort.
Soft-Tissue & Muscle-Tendon Sources
The front of your hip contains several muscles and tendons that can become irritated or injured.
Iliopsoas tendinopathy or strain affects your primary hip flexor muscle. If you're involved in activities with lots of hip flexion—like running, dancing, or soccer—you're at higher risk. You'll typically feel pain when lifting your leg or resisting hip flexion. Sometimes this condition causes a snapping feeling known as snapping hip syndrome.
Are you a sprinter or involved in kicking sports? Watch out for rectus femoris strains. This muscle is part of your quadriceps but also crosses the hip joint. Strains often happen during explosive movements and cause pain with both hip flexion and knee straightening.
That clicking sound when you move your hip might be snapping hip syndrome (coxa saltans). There are two main types: external (IT band snapping over the greater trochanter) and internal (iliopsoas tendon snapping over bony prominences). While often more annoying than painful, repeated snapping can eventually cause inflammation and discomfort.
Athletes who make quick direction changes often develop adductor strains or tendinopathy in the inner thigh muscles. This presents as groin pain that worsens when bringing your legs together and may contribute to sports hernias.
Finally, iliopsoas bursitis—inflammation of the fluid-filled sac between the iliopsoas tendon and hip joint—often occurs alongside snapping hip syndrome. It typically causes pain that worsens with activity and improves with rest.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we regularly see patients with these soft tissue injuries, often related to overtraining or improper movement patterns. For more information about anterior hip pain causes, visit our dedicated resource page. The good news? These conditions generally respond well to targeted physical therapy.
Bone & Morphology Contributors
Sometimes anterior hip pain stems from the bones themselves or their structural arrangement.
Femoral neck stress fractures are overuse injuries causing tiny cracks in the neck of your femur. Distance runners, military recruits, and people with low bone density face higher risk, particularly female athletes with menstrual irregularities. The pain typically develops gradually in the groin, sometimes hurting at night. These fractures require prompt diagnosis as displacement can lead to serious complications.
Born with shallow hip sockets? That's called acetabular dysplasia—an underdevelopment of the acetabulum that leaves the femoral head insufficiently covered. It's more common in women and firstborn children, with risk factors including family history and breech positioning before birth. The condition causes pain as your labrum and cartilage bear extra load, potentially leading to early arthritis if untreated.
Your femur's natural rotation can also cause problems. Femoral version abnormalities (excessive inward or outward rotation) alter your hip biomechanics and can lead to impingement or instability. Normal femoral anteversion is 10°–20°, with anything over 20° considered excessive.
Growing teens face unique risks like apophyseal injuries—damage to growth plates where tendons attach to bone. These are common during growth spurts and present with acute pain, swelling, and sometimes a palpable gap. Similarly, slipped capital femoral epiphysis (SCFE) involves displacement of the femoral head from the femoral neck at the growth plate. This typically affects overweight adolescents and requires urgent orthopedic evaluation.
Nerve & Referred Pain Considerations
Sometimes what feels like hip pain isn't actually coming from your hip at all.
Lumbar spine referral happens when compressed or irritated nerve roots (especially L1-L3) send pain signals to your anterior hip region. This may come with sensory changes, weakness, or back pain, and often follows a predictable pattern based on which nerve is affected. Many patients have both spine and hip issues simultaneously, making diagnosis tricky.
Nerve entrapment syndromes involve compression of nerves supplying the anterior hip region—including the ilioinguinal, iliohypogastric, lateral femoral cutaneous, or femoral nerves. These typically cause burning, tingling, or shooting pain and may be triggered by surgery, pregnancy, or even tight clothing.
Athletes in twisting, cutting sports should be aware of sports hernia/athletic pubalgia—injury to the muscular or tendinous attachments in the lower abdomen and pubic area. This causes exercise-induced groin pain that may radiate to the inner thigh. Diagnosis can be challenging, as symptoms overlap with other conditions.
Don't overlook visceral referral—pain that originates from abdominal or pelvic organs but is felt in the hip region. Conditions like appendicitis, inguinal hernia, gynecological issues, or urinary tract infections can all mimic hip pain. These usually come with other systemic symptoms and require different treatment approaches.
Finally, osteitis pubis—inflammation of the pubic symphysis and surrounding structures—is common in soccer and rugby players. Recovery typically takes months (about 7 months for women and 10 months for men).
Understanding these varied causes explains why diagnosing anterior hip pain requires a comprehensive approach. At Evolve Physical Therapy + Sports Rehabilitation, we consider all potential contributors to ensure you receive the most accurate and effective treatment plan for your specific condition.
Diagnosing & Measuring Anterior Hip Pain
Getting to the root cause of anterior hip pain is like solving a puzzle - one that requires careful assessment and the right diagnostic tools. At Evolve Physical Therapy, we believe an accurate diagnosis forms the foundation of successful treatment.
Clinical Examination Flow for Anterior Hip Pain
When you visit us with anterior hip pain, we'll take you through a comprehensive evaluation that leaves no stone unturned.
We start with a conversation about your story - when your pain began, what makes it better or worse, and how it's affecting your daily life. Understanding whether your pain started suddenly during a tennis match or gradually developed over months gives us important clues about what might be happening.
Next, we observe how you move. The way you walk, stand, and shift your weight can reveal valuable information about what's happening at your hip. We might notice subtle compensation patterns you've developed without even realizing it.
Range of motion testing helps us understand what movements provoke your pain and whether you have restrictions in certain directions. Healthy hips should move freely through flexion (bringing your knee toward your chest), extension (moving your leg behind you), rotation, and other movements. Limitations or pain with specific movements often point to particular problems.
Muscle strength assessment is equally important. We'll check the strength of muscles around your hip, looking for weaknesses or pain during resistance. Sometimes what feels like joint pain actually stems from overworked or weak muscles trying to stabilize your hip.
Special tests are where our clinical expertise really shines. Tests like the FADDIR (where we flex, adduct, and internally rotate your hip) can reproduce symptoms of impingement, while the FABER test helps differentiate between hip, SI joint, and back issues. These maneuvers help us narrow down potential diagnoses with surprising accuracy.
We'll gently palpate (touch) key areas around your hip to identify tender spots, and we'll screen for nerve involvement too. Hip pain sometimes originates from pinched nerves in your back or around your pelvis, so we need to rule this out.
At Evolve, we pride ourselves on thorough evaluations that consider the whole picture - not just isolated symptoms. Our comprehensive physical therapy evaluation is designed to get to the heart of what's causing your discomfort.
Imaging & Special Tests for Confirming Anterior Hip Pathology
While our hands-on examination provides tremendous insight, sometimes we need to look beneath the surface to confirm a diagnosis.
X-rays are typically the first imaging study we recommend. A standing AP (anteroposterior) pelvis view shows both hips for comparison and can reveal arthritis, bone spurs, or structural abnormalities. Special views like the Dunn view are particularly good at showing cam-type impingement deformities at the femoral head-neck junction.
For soft tissue problems like labral tears or muscle injuries, MRI is the gold standard. The good news is that modern 3-Tesla MRIs offer excellent visualization without always needing contrast injection. That said, MR arthrography (MRI with contrast injected into the joint) still provides the most detailed view of labral tears, with about 90% sensitivity.
Ultrasound has a special place in our diagnostic toolkit because it allows for dynamic assessment - we can actually see structures move in real-time. This is particularly useful for conditions like snapping hip syndrome, where the problem only occurs during specific movements.
Sometimes, diagnostic injections can be both informative and therapeutic. If an anesthetic injection into your hip joint significantly relieves your pain, it confirms the joint itself is the source of the problem. This can help differentiate hip pain from referred pain originating in your back.
Outcome Measures & Tracking Progress
How do we know if you're getting better? We measure it!
We use validated questionnaires like the Hip Disability and Osteoarthritis Outcome Score (HOOS) or the International Hip Outcome Tool (iHOT-33) to quantify your symptoms and function. These tools ask about your pain levels, stiffness, daily activities, and more, giving us a numerical score we can track over time.
Beyond questionnaires, we assess real-world function through performance tests. Can you stand up from a chair repeatedly for 30 seconds? How far can you walk in 6 minutes? Can you balance on your affected leg? These objective measures help us document your progress and identify areas that still need work.
For our athletes, we go a step further with sport-specific assessments. Before getting you back on the field or court, we want to see not just pain-free movement but also restored power, agility, and movement quality. Typically, we look for at least 90% symmetry between your sides before clearing you for full return to sport.
At Evolve Physical Therapy + Sports Rehabilitation, we don't just treat symptoms - we measure outcomes to ensure you're truly getting better. This data-driven approach, combined with our hands-on expertise, means you're getting the most effective care possible for your anterior hip pain.
Evidence-Based Management & Prevention Strategies
Managing anterior hip pain effectively requires a custom approach based on the specific diagnosis, severity, and individual factors. Research supports a progressive, multimodal approach for most conditions.
Conservative Care for Anterior Hip Pain
For most cases of anterior hip pain, conservative management is the first-line approach. Here at Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe in treating the whole person, not just the symptoms. Our evidence-based strategies include a thoughtful blend of several approaches.
We often start with activity modification – not complete rest, but smart adjustments to your daily routine. This might mean temporarily scaling back on those deep squats at the gym or modifying your running schedule. Think of it as pressing the pause button, not stopping altogether. We'll help you find that sweet spot where you're still active but not aggravating your hip.
Our hands-on manual therapy techniques can work wonders for many patients. Whether it's gentle joint mobilizations to improve how your hip moves or targeted soft tissue work to release tight muscles, these techniques help restore normal mobility and decrease pain. Many patients find immediate relief after these sessions, which we typically recommend 1-3 times weekly over a 6-12 week period.
The cornerstone of our approach is therapeutic exercise – but not just any exercises. We prescribe specific movements custom to your condition. For tight hip flexors, we might start with gentle stretching and isometric holds, being careful not to overstretch already irritated tissues. Those deep hip stabilizers that often get neglected? We'll teach you how to activate them properly, which research shows can actually shift joint loads away from damaged areas.
Gluteal strengthening is particularly important – I often tell my patients that "your butt is your hip's best friend." Strong glutes help position your femur properly in the socket, reducing stress on sensitive structures. We'll make sure you're engaging those glutes correctly, not compensating with your hamstrings or back.
As you improve, we'll incorporate functional movement retraining to address those patterns that might have contributed to your pain in the first place. Whether it's correcting how you walk, squat, or perform sport-specific movements, this step is crucial for long-term success.
We may complement your treatment with therapeutic modalities like ultrasound or electrical stimulation when appropriate. These tools can help manage pain and facilitate healing, though they're always secondary to active treatments.
Perhaps most importantly, we emphasize education and self-management. Understanding your condition and learning how to manage it independently gives you control over your recovery. We'll teach you about pain mechanisms, proper ergonomics, and home exercises you can perform between sessions.
Throughout this process, we follow progressive loading principles – starting gently and gradually increasing challenges as your hip responds positively. We're always monitoring your symptoms to guide our next steps.
For more information about hip impingement, one of the common causes of anterior hip pain, check out our article on What is Hip Impingement?
When to Refer or Consider Surgical Options
While most people with anterior hip pain improve with conservative care, sometimes surgery becomes necessary. Knowing when to consider this option is important.
If you've been diligently following an appropriate therapy program for 3-6 months without significant improvement, it might be time to discuss other options. Similarly, if your symptoms are progressively worsening despite therapy or you're experiencing mechanical symptoms like locking or catching that severely limit function, an orthopedic consultation makes sense.
Common surgical interventions include hip arthroscopy for labral tears and impingement, with about 90% of patients returning to their activities for certain conditions. Younger patients without significant arthritis tend to have the best outcomes with this approach.
For those with acetabular dysplasia, a periacetabular osteotomy (PAO) might be recommended, especially for patients under 40 without advanced arthritis. This procedure improves the socket's coverage of the femoral head and can prevent early osteoarthritis.
In cases of advanced osteoarthritis, a total hip arthroplasty (replacement) may be the best option. While typically reserved for older adults or those with end-stage disease, modern techniques have made this procedure incredibly successful for pain relief and function restoration.
For stress fractures or acute fractures, fracture fixation may be necessary – particularly important for femoral neck stress fractures to prevent displacement.
At Evolve, we also provide comprehensive post-surgical rehabilitation for patients who undergo these procedures. Our protocols are customized to the specific surgical approach and your individual needs, ensuring optimal recovery.
Lifestyle, Exercise & Load-Optimization for Long-Term Prevention
Preventing recurrence of anterior hip pain is just as important as treating the initial problem. Long-term success requires addressing several modifiable factors.
Weight management plays a significant role in hip health. According to scientific research on hip OA management, every 1% weight loss reduces hip replacement risk by 3% – not just by reducing joint loading but also by decreasing systemic inflammation. When appropriate, we can help connect you with nutritional resources.
Smart exercise dosage is crucial. I often tell my patients that it's not just about what exercises you do, but how you do them and how you progress. We'll help you find the right balance of training loads, ensure adequate recovery between sessions, and incorporate cross-training to distribute stress across different structures. For competitive athletes, we'll discuss periodization strategies to optimize performance while minimizing injury risk.
Movement quality trumps quantity every time. We focus on proper technique rather than just piling on more reps or heavier weights. Finding the right balance between mobility and stability while addressing any compensatory patterns helps protect your hip long-term.
Don't underestimate the importance of proper footwear and equipment. The right athletic shoes for your specific activity, proper bike fitting for cyclists, and appropriate workout equipment adjustments can make a tremendous difference in how stress is distributed through your hip.
For many of us who sit at desks all day, workplace ergonomics matter enormously. We'll discuss proper sitting posture, desk setup, the importance of regular movement breaks, and whether options like standing desks might benefit your specific situation.
Finally, we believe in the value of an ongoing maintenance program – periodic "tune-up" sessions, progressive self-management strategies, and monitoring for early signs of recurrence before they become major problems.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we see successful management of anterior hip pain as a journey that extends well beyond symptom resolution. Our goal is to empower you with the knowledge, skills, and strategies that support long-term hip health and get you back to doing what you love – whether that's running marathons or simply playing with your grandchildren without pain.
Frequently Asked Questions about Anterior Hip Pain
What activities commonly aggravate anterior hip pain?
If you're dealing with anterior hip pain, you've probably noticed certain movements or activities make it worse. This isn't random—specific movements tend to stress the front of the hip in predictable ways.
Activities involving deep hip flexion are often the biggest culprits. Think about sitting in a low chair, performing deep squats, or bringing your knee close to your chest during stretches. Many yoga poses, especially deep lunges, can also trigger discomfort.
High-impact activities are another common aggravator. Running (especially downhill), jumping, and sports that involve quick cutting movements can all flare up front hip pain. The repetitive impact sends forces through the hip joint that can irritate already sensitive structures.
Don't overlook how static positions affect your hip too. Many patients tell us their pain worsens after prolonged sitting, particularly in car seats. Standing with your weight shifted to one side for extended periods can also stress the anterior hip structures.
The way your hip moves during activities matters as well. Movements combining internal rotation with flexion often reproduce pain in people with impingement issues. Repetitive kicking motions in sports like soccer or martial arts, and quick acceleration or deceleration can also trigger symptoms.
At Evolve Physical Therapy in Brooklyn, we find that identifying your specific pain triggers provides valuable clues about what's happening in your hip. This information helps us create a more targeted treatment approach.
How long does it take to recover from a hip flexor strain?
Recovery from a hip flexor strain isn't one-size-fits-all—it depends on several factors including severity, your overall health, and how well you follow your treatment plan.
For mild (Grade 1) strains with minimal tissue damage, you might feel significantly better within 1-2 weeks. Many people can return to their normal activities, including sports, within 2-3 weeks if they're diligent about their rehabilitation.
Moderate (Grade 2) strains involve partial tearing of muscle fibers and typically take 3-6 weeks to heal properly. Most people can return to sports within 4-8 weeks, but rushing this process often leads to reinjury.
Severe (Grade 3) strains or complete tears are much more serious. Recovery typically takes 8-12 weeks at minimum, with return to high-level activities often delayed for 3-6 months. Some cases may require surgical intervention.
Your rehabilitation will progress through several phases, each with specific goals:
During the acute phase (first week), we focus on controlling pain and inflammation while protecting the injured tissues. We'll have you perform gentle movement and isometric exercises that don't increase your pain.
In the subacute phase (weeks 1-3), we'll gradually increase your range of motion and begin light strengthening. This is when manual therapy techniques can be particularly helpful in restoring normal tissue mobility.
The strengthening phase (weeks 2-6) involves progressive resistance training and reintroducing functional movement patterns. We'll address any biomechanical issues that might have contributed to your injury.
Finally, the return to activity phase (4+ weeks) focuses on sport-specific training and ensuring you can perform all necessary movements without pain or compensation.
Several factors can delay recovery, including continuing painful activities too soon, skipping the crucial early rest period, or failing to address underlying movement problems. That's why working with our physical therapists at Evolve gives you the best chance for a complete recovery—we'll help you steer each stage appropriately.
Can anterior hip pain be prevented in young athletes?
Yes! Many cases of anterior hip pain in young athletes are preventable with the right approach. At Evolve Physical Therapy, we work closely with young athletes to reduce their risk of developing these painful conditions.
Regular movement screenings are invaluable for catching potential problems early. We look for restricted hip mobility, muscle imbalances, and dysfunctional movement patterns that might increase injury risk. When we spot these issues, we can address them before they lead to pain.
Neuromuscular training forms the foundation of prevention. We teach athletes how to properly activate their core and hip stabilizers, improve their balance, and refine sport-specific techniques. This training helps distribute forces more evenly through the hip joint during athletic movements.
Smart training load management is especially crucial for growing athletes. During growth spurts, young athletes are particularly vulnerable to overuse injuries. We educate coaches and parents about appropriate training progression, the importance of adequate recovery time, and the benefits of cross-training to distribute stress across different tissues.
Different sports create unique demands on the hip. Dancers and gymnasts need proper turnout technique that comes from the hips rather than compensating at the knees and feet. Soccer and hockey players benefit from hip strengthening to control forces during kicking and skating. Runners need gradual mileage progression and technique refinement to reduce impact forces.
We also emphasize the importance of awareness during periods of rapid growth. Many parents don't realize that growth spurts increase injury risk, so we provide guidance on modifying training during these vulnerable times. Proper nutrition and adequate sleep are also essential components of injury prevention that we discuss with our young athletes.
Equipment choices matter too. We help athletes select appropriate footwear for their specific activities and consider how playing surfaces might affect hip loading.
By implementing these preventive strategies, we've helped many young athletes at Evolve Physical Therapy stay healthy and perform at their best while avoiding the frustration of anterior hip pain.
Conclusion & Next Steps
The journey to understanding and resolving anterior hip pain begins with knowledge. Throughout this guide, we've explored how hip pain can originate from many sources – from joint mechanics and soft tissue problems to bone structure issues and movement patterns that put stress on your hip.
Here's what we hope you'll take away from this comprehensive look at hip pain:
Anterior hip pain isn't just one condition – it represents a spectrum of possibilities from common arthritis and impingement to muscle strains and even pain referred from other body regions. Getting the right diagnosis matters enormously for your recovery.
Most people experiencing hip pain find significant relief through non-surgical approaches. Physical therapy, smart activity modifications, and properly progressed exercise often resolve even stubborn cases when properly custom to your specific condition.
Sometimes, despite our best conservative efforts, certain conditions may require surgical intervention. The good news is that modern surgical techniques have dramatically improved outcomes for many hip conditions.
Prevention really is the best medicine. By focusing on quality movement, appropriate exercise loading, and lifestyle factors that support hip health, you can often avoid recurrence and maintain an active lifestyle.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we see hip pain cases every day. Our approach combines careful assessment with hands-on treatment and personalized exercise programs. We work with everyone from seniors managing arthritis to high-level athletes returning to competition after injury.
If you're dealing with anterior hip pain, don't wait until it becomes debilitating. Early intervention typically leads to better outcomes and helps prevent the domino effect where one painful area creates problems elsewhere in your body.
We've made accessing quality hip care convenient with locations throughout Brooklyn – in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin. At each location, you'll find therapists experienced in comprehensive hip rehabilitation who will create an individualized plan to get you back to living without limitations.
Don't let hip pain keep you from the activities and lifestyle you love. Reach out to Evolve Physical Therapy + Sports Rehabilitation today to schedule your evaluation and take that first important step toward resolving your anterior hip pain.
Recovery isn't just about following a cookie-cutter protocol – it's a partnership between you and your physical therapist. With expert guidance and your commitment, most people with anterior hip pain can achieve remarkable improvements and return to their favorite activities with confidence, armed with strategies to maintain their hip health for years to come.
Surgical Solutions for Scoliosis: What You Need to Know1Deep Research2Outline3Content
Understanding Surgical Options for Scoliosis
Scoliosis surgery is typically recommended when spinal curvature exceeds 45-50 degrees or continues to worsen despite non-surgical treatments. Here's what you need to know:
When it's considered: For curves >45° in mature patients or >40° in growing children
Main goals: Stop curve progression, reduce deformity, maintain trunk balance
Types: Spinal fusion (most common), growing rods (for young children), vertebral body tethering
Success rate: 60-100% curve correction depending on flexibility
Recovery time: Hospital stay of 3-4 days, return to school in 4-6 weeks, full activities in 2-6 months
Scoliosis surgery represents a significant decision for patients and families facing progressive spinal curvature. While many cases of scoliosis can be managed with observation or bracing, surgical intervention becomes necessary when curves reach a severity that threatens long-term health and quality of life.
The decision to pursue surgery isn't made lightly. Doctors typically recommend surgical treatment when curves exceed 45-50 degrees or continue to worsen despite other treatments. For growing children with curves above 40 degrees, the decision becomes even more important as these curves almost always continue to progress.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've helped numerous patients through both pre-surgical preparation and post-operative rehabilitation following scoliosis surgery, developing specialized protocols that address the unique challenges these patients face during recovery.
Understanding Scoliosis & When Surgery Is Considered
When you hear the word "scoliosis," think of a spine that curves sideways instead of running straight down the back. This S-shaped or C-shaped curve must measure at least 10 degrees on an X-ray to be officially diagnosed as scoliosis. Though it sounds rare, scoliosis affects about 2% of teenagers, with girls being eight times more likely to develop significant curves than boys.
Scoliosis comes in several different forms, each with its own story:
Idiopathic scoliosis (about 80% of cases) appears without any known cause, typically during growth spurts
Congenital scoliosis happens before birth when the spine doesn't form properly
Neuromuscular scoliosis develops in people with conditions affecting muscle control, like cerebral palsy
Degenerative scoliosis shows up later in life as the spine naturally wears down with age
Doctors measure scoliosis severity using something called the Cobb method – essentially calculating the angle of the curve from X-rays. This number becomes incredibly important when deciding whether surgery might be necessary.
The science is clear on what happens with larger curves. Research shows that curves over 50 degrees in someone who's finished growing will still progress about 1 degree each year. Even more concerning, curves exceeding 60 degrees can reduce lung capacity to just 68% of normal, potentially causing breathing problems down the road.
A groundbreaking study in the Journal of Bone and Joint Surgery followed patients for over 40 years and found thoracic curves between 50-75 degrees progressed an average of 29.4 degrees over that time. This confirms what many surgeons already suspected – significant curves don't simply stop progressing once you're done growing.
Is scoliosis surgery always necessary?
Good news – the vast majority of scoliosis cases never require surgery! In fact, only about 5% of young people with scoliosis eventually need bracing or surgical intervention. Most mild curves (under 25 degrees) simply need regular check-ups to watch for changes.
For growing children with moderate curves between 25-40 degrees, bracing often works wonderfully. When worn consistently (16-23 hours daily), braces can stop curve progression in about 75% of adolescents with idiopathic scoliosis. It's not always easy wearing a brace as a teenager, but the results speak for themselves.
Here at Evolve Physical Therapy + Sports Rehabilitation, we offer specialized Schroth therapy – a three-dimensional exercise approach specifically designed for scoliosis patients. This therapy can be incredibly helpful for patients with mild to moderate curves, those preparing for or recovering from surgery, and anyone looking to improve posture and reduce scoliosis-related pain. More info about scoliosis treatment
The decision to try non-surgical approaches depends heavily on skeletal maturity. Once growth is complete (typically around 14 for girls and 16 for boys), curves under 45 degrees are much less likely to worsen rapidly.
Surgical indication checklist
How do doctors determine if scoliosis surgery is truly necessary? They consider several important factors:
Curve magnitude typically triggers surgical discussions when it exceeds 45-50 degrees in someone who's finished growing, or 40 degrees in someone still growing. Curve flexibility matters too – surgeons assess this through special bending or traction X-rays to predict potential correction. More flexible curves generally have better surgical outcomes.
While pain is rarely a major issue in adolescent idiopathic scoliosis, persistent discomfort that doesn't respond to conservative treatment might influence the surgical decision. Cosmetic concerns like visible deformity, rib humps, or uneven shoulders causing significant psychological distress are also valid considerations.
In rare cases, neurological symptoms like numbness or weakness might appear, requiring prompt surgical attention. Pulmonary function becomes important for severe thoracic curves that might compromise breathing. And of course, curves that continue progressing despite bracing often indicate surgery is needed.
As one orthopedic surgeon we collaborate with puts it: "The decision to operate isn't based solely on numbers. We consider the whole person—their age, curve pattern, symptoms, and how scoliosis affects their daily life and self-image."
At Evolve Physical Therapy, we work closely with surgical teams to support patients through their entire journey, whether that involves preparing for surgery or helping them avoid it altogether through targeted therapy approaches.
Scoliosis Surgery: Goals, Techniques, Bone Grafts
When it comes to scoliosis surgery, there are three main goals that guide the entire process:
Stop curve progression to prevent future deformity and related health issues
Reduce existing deformity by safely straightening the spine as much as possible
Maintain trunk balance while preserving the natural curves that should be there
Today's surgical techniques can typically improve scoliosis curves by 50-70%, with some more flexible curves seeing even better results. It's worth noting that surgeons aren't always aiming for a perfectly straight spine—instead, they're focused on creating balance, improving appearance, and enhancing overall function.
Main types of scoliosis surgery
If you or your child is facing scoliosis surgery, understanding the different approaches can help you feel more prepared for discussions with your surgical team.
Posterior Spinal Fusion is by far the most common approach, used in about 80-90% of cases. The surgeon makes an incision along the back of the spine, then uses rods, screws, and hooks to straighten the curve. Bone graft material is added to help the vertebrae fuse together over time. Most patients stay in the hospital for 3-4 days, and correction rates range from 60-100% depending on how flexible the curve is.
Anterior Spinal Fusion approaches the spine from the front or side of the body. This technique can sometimes preserve more motion segments in certain curve patterns, making it particularly useful for thoracolumbar or lumbar curves. Hospital stays are slightly longer (4-7 days), but the benefit is that fewer vertebrae may need to be fused.
For young children under 10 with progressive scoliosis, Growing Rod Techniques offer a way to control curves while allowing continued growth. The rods attach to the spine above and below the curve and are lengthened every 6-12 months as the child grows. This approach delays final fusion until the child is closer to skeletal maturity, allowing for an average spine length increase of 4.7 cm through these periodic adjustments.
Vertebral Body Tethering (VBT) represents a newer, fusionless option for growing children and adolescents. Rather than fusing the spine, VBT uses a flexible cord on the outside of the curve to guide growth, preserving motion and flexibility. The FDA approved this technique in 2019 specifically for idiopathic scoliosis.
Children with thoracic insufficiency syndrome may benefit from Vertical Expandable Prosthetic Titanium Rib (VEPTR), a specialized technique that increases thoracic volume while correcting scoliosis, improving breathing and lung development.
How does minimally invasive scoliosis surgery differ?
Minimally invasive scoliosis surgery (MISS) marks a significant evolution in how we approach spine correction. While traditional scoliosis surgery involves a long incision and substantial muscle dissection, MISS takes a gentler approach.
Instead of one long incision, surgeons make multiple smaller ones (typically 1-2 inches each). They use specialized tubular retractors that spread muscle fibers apart rather than cutting through them. Real-time X-ray imaging guides precise placement of implants. The benefits are substantial: less blood loss (824 ml versus 1,791 ml in traditional surgery), shorter hospital stays (typically 1-2 days less), and potentially faster recovery.
One specific minimally invasive approach is Video-Assisted Thoracoscopic Surgery (VATS), which uses small chest incisions, specialized cameras, and instruments to access the front of the spine.
Research published in the Journal of Spinal Disorders & Techniques found that patients who underwent minimally invasive procedures experienced less pain, needed fewer pain medications, and returned to school or work about two weeks earlier than those who had traditional open procedures.
That said, minimally invasive techniques aren't right for everyone. They typically work best for curves under 70 degrees, require surgeons with specialized training and equipment, and may not be suitable for all curve patterns. As one spine surgeon I work with puts it: "We need to balance the recovery advantages against the need for adequate correction. Not every patient is a candidate, but for those who are, the benefits can be significant."
You can learn more about these advanced techniques in this research on minimally invasive techniques.
Bone graft options & risks
Bone grafting plays a crucial role in spinal fusion, providing the biological material needed to create a solid bridge between vertebrae. There are several options to consider:
Autograft uses the patient's own bone, traditionally harvested from the pelvis (iliac crest). Surgeons often consider this the "gold standard" for fusion success because it contains living bone cells and growth factors. The downside? It requires an additional incision, can cause donor site pain, and offers limited quantity.
Allograft comes from bone banks and eliminates the need for that additional incision and donor site pain. The bone is carefully processed to reduce disease transmission risk, with infection risk being remarkably low—about 1 in 1 million for hepatitis and 1 in 10 million for AIDS.
For some patients, synthetic or biological alternatives may be appropriate. These include bone morphogenetic proteins (BMPs) that stimulate bone formation and synthetic calcium-based substitutes. These are often used in combination with autograft or allograft but are less commonly used in pediatric cases.
It's worth noting that pseudarthrosis—failure of the bones to fuse properly—occurs in up to 1% of children but is more common in adults, especially those who smoke. While initial stability happens relatively quickly, complete solid fusion typically takes 6-12 months.
At Evolve Physical Therapy + Sports Rehabilitation, we work closely with patients before and after scoliosis surgery to optimize outcomes and support the healing process. Our hands-on approach helps patients steer the challenges of recovery while building the strength needed for long-term success.
Getting Ready for Your Operation
Preparing for scoliosis surgery isn't just about the medical checklist—it's about setting yourself up for the best possible outcome. When my patients are getting ready for surgery, I walk them through a comprehensive preparation process that helps calm their nerves and optimize their recovery.
Your surgical team will conduct a thorough preoperative evaluation that typically includes several key components. You'll undergo a comprehensive physical examination to assess your overall health. The imaging portion is particularly important—standing full-spine X-rays give surgeons your baseline, while special side-bending or traction X-rays help determine how flexible your spine is (which affects how much correction can be achieved). Many surgeons also order an MRI to ensure there are no spinal cord abnormalities that could complicate surgery.
Blood work is another essential step—your surgical team will need a complete blood count, coagulation studies, and a metabolic panel to ensure you're healthy enough for surgery. You'll also meet with an anesthesiologist who will review your medical history and discuss the anesthesia plan. For patients with severe curves, pulmonary function tests may be ordered to check how the scoliosis affects breathing.
At Evolve Physical Therapy + Sports Rehabilitation, we've developed specialized programs to help our patients physically prepare for scoliosis surgery. We focus on strengthening your core muscles to support your spine during recovery and teach important breathing exercises that will help prevent post-surgical complications like pneumonia. One of the most practical skills we cover is proper log-rolling technique—trust me, you'll be grateful you learned this before surgery when you need to get in and out of bed without bending your spine!
"The physical therapy team at Evolve taught me exactly what to expect after surgery," shared Maya, one of our 16-year-old patients. "Learning how to log-roll and practice deep breathing beforehand made a huge difference in my recovery."
If you smoke, your surgeon will ask you to quit at least two weeks before surgery, as smoking significantly impairs bone healing. You'll also need to stop taking blood thinners, anti-inflammatories, and certain supplements that could increase bleeding risk. Good nutrition in the weeks before surgery can help support your body's healing process afterward.
Day-before checklist
The day before your scoliosis surgery is all about final preparations. You'll need to stop eating and drinking after midnight (or follow your surgical team's specific instructions). Take only medications that your surgeon has explicitly approved—this is really important, as some common medications can interfere with anesthesia or increase bleeding risk.
Some surgeons prescribe a bowel preparation protocol to follow, and you may be given an antimicrobial soap for showering. When packing for the hospital, think comfort: loose clothing that's easy to put on and take off, slip-on shoes (bending to tie laces won't be possible right after surgery), and personal hygiene items. Don't forget entertainment like books or a tablet—recovery involves a lot of downtime. A small pillow can make the ride home much more comfortable, and always bring all your regular medications in their original bottles.
Intra-op safety measures
Modern scoliosis surgery has become remarkably safe thanks to advanced monitoring techniques and protocols. One of the most important safety measures is neuromonitoring—continuous electrical monitoring of your spinal cord and nerve function throughout the procedure. This technology has reduced the risk of neurological injury to less than 1%, as surgeons receive immediate feedback if there's any change in nerve function.
You'll receive prophylactic antibiotics before the first incision and for about 24 hours afterward to prevent infection. Many hospitals use cell-saver technology, which collects, filters, and returns your own blood during surgery, reducing the need for transfusions. Your anesthesiologist will carefully manage your blood pressure using controlled hypotensive anesthesia to minimize blood loss, while also maintaining your body temperature at the optimal level for clotting and infection prevention.
Perhaps the most important safety factor is having an experienced surgical team. As one spinal surgeon I work with explains: "The advancements in neuromonitoring have dramatically improved safety. We receive immediate feedback if there's any change in nerve function, allowing us to adjust our approach before any permanent damage occurs."
At Evolve Physical Therapy, we coordinate closely with surgical teams to ensure our patients understand each step of this preparation process. This comprehensive approach not only improves surgical outcomes but also helps reduce the anxiety that naturally comes with preparing for such a significant procedure.
Recovery, Risks & Life After Surgery
Coming home after scoliosis surgery marks the beginning of an important healing journey. While every patient's experience is unique, most follow a similar path to recovery that unfolds over several months.
The first few days in the hospital are focused on pain management and getting you back on your feet. Most patients stay about 3-4 days, starting with a PCA (patient-controlled analgesia) pump on day one that lets you manage your own pain medication. You'll likely surprise yourself by sitting in a chair that very first day! By day two, you'll be taking your first steps with assistance and transitioning to oral pain medications. As days three and four approach, you'll be walking more independently, your digestive system will wake up, and the discharge planning begins.
Those first six weeks at home require some patience. You'll need to limit bending, twisting, and lifting anything heavier than a half-gallon of milk (about 5 pounds). Daily walking becomes your main activity, gradually increasing distance as you build strength. Most teens return to school part-time around the 4-6 week mark, often with some accommodations like elevator access or a second set of textbooks to avoid heavy backpacks.
As you move into the 6-week to 6-month phase, life starts feeling more normal. Physical therapy becomes a key part of your recovery, focusing on rebuilding strength and function. Most surgeons clear patients to drive around the 6-week mark (once you're off pain medications), and non-contact sports typically get the green light between 4-6 months.
The final stage of recovery happens between 6-12 months when your bone fusion fully matures. This is when most patients receive clearance to return to all activities, including contact sports if desired. Your surgeon will take final X-rays to confirm that your fusion is solid and complete.
One of the unexpected bonuses? Most patients gain about 1 to 1.5 inches in height after their curve is corrected!
While scoliosis surgery has an excellent track record, it's important to understand potential risks. Infection affects about 1-3% of patients. Some experience more blood loss than anticipated and may need a transfusion. Serious nerve injuries are quite rare (less than 1%) thanks to advanced monitoring techniques. Failed fusion (pseudarthrosis) can occur, though it's more common in adults than teens. Sometimes implants can cause issues like rod breakage or screw loosening. And over many years, the vertebrae above or below the fusion may experience accelerated wear and tear.
Managing pain & physical therapy
"The first two weeks were tough, but then each day got noticeably better," shares Emma, a former patient who had fusion surgery at age 14. This mirrors what most patients experience with post-surgical pain.
Pain management after scoliosis surgery follows a thoughtful progression. Initially, you'll have a PCA pump that lets you administer small, controlled doses of pain medication when needed. Around day 2-4, you'll transition to oral medications, typically including both opioids and muscle relaxants. By the time you're home, you'll be on a schedule of gradually decreasing pain medication, with most teens able to discontinue opioids within two weeks and transition to over-the-counter options.
At Evolve Physical Therapy + Sports Rehabilitation, we've developed specialized protocols for scoliosis recovery. Our approach begins with gentle, early mobilization—simply getting you moving safely as soon as possible. We then progress to rebuilding core strength, which provides crucial support for your healing spine. We pay special attention to your walking pattern and posture, helping you adapt to your new spinal alignment.
Our therapists incorporate elements of Schroth therapy, addressing the three-dimensional nature of scoliosis even after surgical correction. This specialized approach optimizes breathing, posture, and functional movement during your recovery.
"The physical therapists at Evolve truly understood what I was going through," says Sarah, who had spinal fusion at 15. "They knew exactly when to push me and when to let me rest. Six months after surgery, I was back to dancing, which I never thought would be possible."
Long-term outlook
The good news is that the long-term outlook after scoliosis surgery is overwhelmingly positive. Modern techniques achieve impressive correction—anywhere from 60-100% improvement depending on how flexible your curve was before surgery. More importantly, research consistently shows significant improvements in quality of life, self-image, and physical function.
Your corrected spine alignment typically remains stable over time, with minimal loss of correction (usually less than 5 degrees). While the fused segments no longer move, you'll retain sufficient motion in the unfused portions of your spine for nearly all activities. As one surgeon explains, "We aim to fuse the fewest segments possible while still achieving adequate correction."
Most patients return to their pre-surgical activity levels, including sports. While certain high-impact activities might need modification, few are permanently off-limits. For young women concerned about future pregnancy, it's reassuring to know that those who have undergone scoliosis surgery can have normal pregnancies and deliveries—the fusion doesn't typically interfere with childbearing.
Perhaps most importantly, surgical correction dramatically reduces the risk of future curve progression and its associated complications. A study published in Spine followed patients for 20 years after scoliosis surgery and found that 90% were satisfied with their results and would choose to have the surgery again if faced with the same decision.
At Evolve Physical Therapy, we're committed to supporting you through every phase of this journey, from pre-operative preparation through long-term recovery and return to the activities you love. Our specialized Schroth therapy program offers ongoing support even years after surgery to maintain optimal function and prevent secondary issues.
Alternatives, Innovation & FAQs
When it comes to addressing scoliosis, surgery isn't the only option on the table. While scoliosis surgery remains the most effective treatment for severe curves, medical science has developed several alternatives worth exploring.
At Evolve Physical Therapy + Sports Rehabilitation, we're passionate about offering comprehensive care options. Our certified Schroth therapists provide specialized physical therapy custom to each patient's unique curve pattern. This non-surgical approach can be remarkably effective for managing smaller curves or complementing surgical treatment for optimal outcomes.
Bracing technology has come a long way, too! Modern braces are more comfortable and effective than ever before. When worn consistently (16-23 hours daily), they can halt progression in up to 75% of adolescents with moderate curves. Many of our patients are pleasantly surprised by how today's braces can fit discreetly under clothing.
"The brace my daughter received was nothing like what I remembered from my childhood," shared one parent. "It was lightweight, custom-molded, and she could still participate in most activities."
The field of scoliosis treatment is constantly evolving with exciting innovations. Magnetically controlled growing rods represent a breakthrough for young children, allowing lengthening through external magnets rather than repeated surgeries. Meanwhile, robotic-assisted surgery is enhancing the precision of screw placement while reducing operative time and radiation exposure.
Speaking of radiation, the new EOS imaging systems reduce exposure by an impressive 50-85% compared to conventional X-rays, while providing superior 3D visualization of the spine. This technology is especially valuable for patients requiring frequent monitoring.
The financial aspect of scoliosis surgery deserves careful consideration. While costs vary depending on location, hospital, implants, and length of stay, most insurance plans cover the procedure when medically necessary. I always recommend working closely with your surgeon's office to understand insurance coverage and potential out-of-pocket expenses.
You're not alone on this journey. Both in-person and online support groups offer invaluable emotional support and practical advice. Organizations like the Scoliosis Research Society and the National Scoliosis Foundation can connect you with others who truly understand what you're going through.
Frequently Asked Questions about scoliosis surgery
What are the biggest risks of scoliosis surgery?
While scoliosis surgery has an excellent safety profile, it's important to understand the potential risks. Bleeding occurs in most surgeries, but advances like cell-saver technology have significantly reduced the need for transfusions (now required in less than 30% of cases).
Infection remains a concern with any surgery, with rates of approximately 1-3% for scoliosis procedures. Your surgical team will take multiple precautions, including prophylactic antibiotics and strict sterile technique, to minimize this risk.
Nerve injury is perhaps the most feared complication, but modern neuromonitoring has reduced the risk of major neurological injury to well under 1%. Minor numbness or tingling sensations are more common but typically resolve within weeks to months.
Pseudarthrosis (failure of the fusion to heal properly) occurs in up to 1% of children but is more common in adults (5-10%), particularly smokers. If detected, revision surgery may be necessary to ensure proper healing.
"The most serious complications are extremely rare," explains one spine surgeon I work with. "The vast majority of patients experience a smooth recovery with excellent outcomes."
Will my back be stiff after fusion?
This is one of the most common questions I hear from patients considering scoliosis surgery. Yes, the fused segments will no longer move, but several factors determine how this affects your daily life.
The extent of fusion matters tremendously. Surgeons aim to fuse the minimum number of vertebrae necessary, preserving as much natural motion as possible. The location of fusion also plays a role – lumbar fusions tend to affect forward bending more than thoracic fusions.
What many patients don't realize is how well the unfused portions of the spine adapt, often developing increased mobility to compensate for the fused segments. The human body is remarkably adaptable!
One of my patients, now 10 years post-fusion, puts it perfectly: "I honestly forget I have rods in my back most days. I can do everything I want to do—yoga, hiking, playing with my kids. The only thing I notice is that I bend differently to pick things up, but it's second nature now."
After fusion, we typically recommend avoiding extreme sports with high fall risk, using proper body mechanics for lifting, and maintaining core strength through regular exercise – all things we can help with at Evolve.
How soon can my child return to normal activities?
Recovery follows a predictable timeline, though individual experiences vary. Most patients return to school part-time at 4-6 weeks after scoliosis surgery. Driving is typically permitted at 6 weeks, once pain medications are no longer needed.
Swimming often becomes the first approved exercise at 6-8 weeks, offering gentle resistance without jarring impacts. Non-contact sports usually get the green light at 4-6 months, while contact sports and full activities are generally cleared at 6-12 months, once fusion is solid.
At Evolve Physical Therapy + Sports Rehabilitation, we collaborate closely with surgeons to create customized return-to-activity protocols based on each patient's recovery, fusion levels, and activity goals. We understand how important it is for young people to return to their passions.
The mother of one teenage dancer shared: "We were worried about her missing her entire dance season, but with the rehabilitation program at Evolve, she was back to modified dance at 4 months and performing fully by 7 months. The timeline they gave us was spot-on."
With proper planning, patience, and expert guidance, most patients can return to the activities they love – often with better posture and less pain than before surgery.
Conclusion & Next Steps
Scoliosis surgery marks a significant milestone in the journey of someone with severe spinal curvature. I've seen how today's advanced surgical techniques, paired with thoughtful rehabilitation, can transform lives and futures.
If you're standing at this crossroads with your child—or perhaps for yourself—I want you to know that while the decision feels enormous, you don't have to steer it alone.
Here at Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we walk alongside our scoliosis patients through every step of their surgical journey. We believe preparation is just as important as the recovery phase, which is why we focus on both pre-surgical conditioning and comprehensive post-operative rehabilitation.
What makes our approach different? We see beyond the spine. We understand that scoliosis surgery impacts not just your physical body, but your emotional wellbeing, your daily routines, and your return to the activities that bring you joy. Our specialized Schroth therapy protocols address the three-dimensional nature of scoliosis correction, while our hands-on techniques target the specific challenges that arise during recovery.
Before taking your next steps, consider:
Connecting with a surgeon who specializes specifically in scoliosis (not just general spine surgery). Their expertise makes a tremendous difference in surgical outcomes.
Getting that second opinion—especially for complex curves or unusual presentations. Different surgeons may offer different approaches.
Exploring all available options thoroughly. Sometimes surgery is clearly necessary, but understanding the full spectrum of treatments helps you make peace with your decision.
Building physical and emotional readiness before surgery. The stronger your body and mindset going in, the smoother your recovery tends to be.
Planning your rehabilitation pathway in advance. Knowing what to expect after surgery removes much of the anxiety from the recovery process.
Our team serves patients throughout Brooklyn—from Marine Park to Gravesend, Midwood to Park Slope, and Mill Basin—making specialized scoliosis care accessible across our community. We've guided countless patients from pre-surgical jitters to post-operative success stories, and we'd be honored to be part of your journey too.
While facing scoliosis surgery might feel overwhelming today, I want to leave you with this thought: the patients I work with consistently tell me that looking back, they wish they'd worried less. With proper preparation, skilled surgical care, and dedicated rehabilitation, the road ahead leads toward improved alignment, better function, and a quality of life that may have seemed out of reach before.
To learn more about how our Schroth scoliosis therapy program can support your surgical journey, visit our Schroth scoliosis physical therapy page or reach out to our office directly. We're here to help turn this significant medical intervention into a positive turning point in your life.
TMJ Trigger Points Unlocked: Your Essential Guide
Understanding TMJ Trigger Points: The Hidden Source of Jaw Pain
TMJ trigger points are hyperirritable knots in the muscles around your jaw that can cause pain, stiffness, and limited movement. These sensitive spots can refer pain to other areas, creating symptoms that might seem unrelated to jaw problems.
What Are TMJ Trigger Points?
Tight, sensitive knots in jaw and facial muscles
Can cause local pain and referred pain to teeth, ears, and head
Often activated by stress, teeth grinding, or jaw overuse
May lead to clicking, popping, and limited jaw movement
Can be treated with massage, physical therapy, and self-care techniques
If you've ever experienced unexplained jaw pain, headaches, or even ear discomfort that your dentist couldn't solve, TMJ trigger points might be the culprit. These tense muscle knots develop in the muscles of mastication—primarily the masseter, temporalis, and pterygoid muscles—and can refer pain to surprising areas like your teeth, sinuses, or even deep into your ear canal.
What makes these trigger points particularly troublesome is their ability to mimic other conditions. That tooth pain might not be a cavity at all, but referred pain from a masseter trigger point. The ringing in your ear? Possibly linked to tension in your jaw muscles rather than an ear infection.
TMJ trigger points commonly develop due to everyday habits many of us don't even notice: teeth clenching during stressful meetings, nighttime grinding (bruxism), poor posture while working at a computer, or even chewing gum excessively. The repetitive strain creates micro-trauma in the muscle fibers, leading to those painful knots that can persist for months or even years if left untreated.
I'm Lou Ezrick, and as a physical therapist specializing in chronic pain management, I've helped thousands of patients find relief from TMJ trigger points through targeted manual therapy techniques and individualized treatment plans that address both symptoms and underlying causes.
TMJ Trigger Points 101
Have you ever felt that tight, tender spot in your jaw that just won't go away? That's likely a TMJ trigger point – a small knot in your muscle tissue that can cause big problems. These trigger points are essentially taut bands within your muscles that have become hypersensitive and irritable.
Think of these trigger points as tiny muscle cramps that got stuck in the "on" position. When muscle fibers remain contracted for too long, they create a self-sustaining cycle of pain and tension. As the pioneering work of Dr. Janet Travell showed, these spots become painful when pressed and can send pain signals to completely different areas of your head and face.
TMJ trigger points come in two main varieties:
Active trigger points are the troublemakers – they hurt even when you're not touching them, refer pain to other areas in predictable patterns, and limit how wide you can open your mouth. These are the ones that might wake you up at night or distract you during the day.
Latent trigger points are the sneaky ones – they don't cause spontaneous pain but still create muscle tightness and restriction. They're like sleeping dragons that can awaken when you're stressed, overuse your jaw, or come down with an illness.
Why do these pesky trigger points develop in the first place? Many of my Brooklyn patients are surprised to learn that everyday habits are often the culprit. Constant gum chewing, nail biting, or even that chocolate-covered almond addiction can overwork your jaw muscles. Stress is another major factor – that jaw clenching during your morning commute or while focusing on work adds up over time.
Nighttime teeth grinding (bruxism) is perhaps the most damaging trigger point creator, as your jaw muscles can generate tremendous force while you sleep – completely unconsciously! Poor posture, especially that forward-head position many of us adopt while looking at our phones, places extra strain on the entire jaw-neck system. Even a minor car accident or a long dental procedure can set the stage for trigger point development.
As one of our patients at Evolve Physical Therapy recently shared: "For years, I thought I needed root canals because of the tooth pain. Turns out, it was my jaw muscles the whole time! Understanding these trigger points has been life-changing."
How TMJ Trigger Points Cause TMD
Temporomandibular disorder (TMD) isn't just about the jaw joint itself – it's a complex relationship between your joints, muscles, and nervous system. TMJ trigger points are often key players in this painful drama.
These trigger points contribute to TMD through several important mechanisms. First, they create micro-trauma in your muscles. Each time you clench or grind, you're causing tiny injuries to muscle fibers, especially in the powerful masseter and temporalis muscles. These micro-tears lead to inflammation, pain, and – you guessed it – more trigger points.
TMJ trigger points also throw off the balance between muscle groups. When certain muscles become shortened and overactive due to trigger points, their opposing muscles become lengthened and weakened. This neuromuscular imbalance is why many patients notice their jaw deviating to one side when they open their mouth.
Perhaps most concerning is how trigger points alter joint loading. When your jaw muscles don't contract normally, they create abnormal movement patterns that place excessive stress on your temporomandibular joint. Over time, this can lead to disc displacement (that clicking or popping sound), joint inflammation, and even arthritic changes.
Research confirms how central these muscle issues are – a study in the Journal of Oral & Facial Pain and Headache found that myofascial trigger points are the primary source of pain in up to 55% of TMD patients. That's why addressing these muscle knots is often the key to resolving jaw pain.
Typical TMJ Trigger Points Referral Map
One of the most fascinating (and frustrating) aspects of TMJ trigger points is how they can cause pain far away from the actual problem spot. This "referred pain" follows predictable patterns that we've mapped extensively at Evolve Physical Therapy.
Your masseter muscle – the powerful chewing muscle you can feel bulging when you clench your teeth – commonly refers pain to your upper and lower molars. This is why so many patients undergo unnecessary dental work! These trigger points can also send pain deep into your ear canal, creating sensations that mimic ear infections or even tinnitus.
Trigger points in your temporalis muscle (the fan-shaped muscle at your temple) typically refer pain to your temple, eyebrow, and upper teeth. Many patients come to us thinking they have chronic migraines, only to find their headaches are actually stemming from jaw muscle tension.
The pterygoid muscles are hidden heroes (or villains) in the TMJ story. Lateral pterygoid trigger points often cause pain in front of your ear, around the TMJ itself, and even into your sinus region. These are often responsible for that annoying jaw clicking. Medial pterygoid trigger points create deep pain inside your mouth and throat area.
Even your neck muscles can join the party – particularly the sternocleidomastoid (SCM). Though not technically a jaw muscle, SCM trigger points commonly refer pain to your cheek, eye area, and ear, perfectly mimicking TMJ problems.
Understanding these referral patterns helps both our therapists and patients identify the true source of pain. As we often say at Evolve, "Treat the cause, not just the symptom." By targeting these specific trigger points, we can provide relief where other approaches have failed.
Key Muscles That Develop TMJ Trigger Points
The jaw is a marvel of muscular teamwork, with several key players working together to help you talk, chew, and express yourself. When these muscles develop TMJ trigger points, they can create a surprising array of painful symptoms. Let's get to know the muscles behind your jaw troubles:
Masseter: The Power Chewer
Think of your masseter as the heavyweight champion of your jaw muscles. This powerful muscle connects your cheekbone to your lower jaw and generates incredible force when you bite down. It's actually one of the strongest muscles in your body relative to its size!
Your masseter has two layers working together – a larger superficial layer that provides raw power for jaw closure, and a deeper layer that helps with more precise movements and grinding. When TMJ trigger points develop here, they're notorious troublemakers.
These masseter trigger points are incredibly common, affecting more than half of people with jaw pain. They're masters of disguise too – often creating pain that perfectly mimics a toothache in your molars. Many patients tell us they've had unnecessary dental work because everyone (including their dentist) thought the problem was with their teeth!
Beyond tooth pain, tight masseter muscles can limit how wide you can open your mouth, cause jaw tenderness, refer pain up to your eyebrow, and even create deep ear pain or ringing. As one of our Brooklyn patients recently told us, "I spent two years thinking I had an ear infection until my physical therapist found these knots in my jaw muscle!"
Common culprits behind masseter trigger points include teeth grinding at night, daytime stress clenching (often unconscious during work or driving), excessive gum chewing, and even that forward-head posture many of us adopt while using our phones. For deeper insights into masseter pain, check out this scientific research on masseter pain.
Lateral & Medial Pterygoids: Hidden Culprits
If the masseter is the star of the show, the pterygoid muscles are the behind-the-scenes crew that rarely get enough credit. These muscles hide deep inside your jaw, making them difficult to reach but incredibly important to address.
The lateral pterygoid is your jaw-opening specialist. It helps you open wide, move your jaw side to side, and push your jaw forward. When trigger points develop here, you might notice clicking or popping when you open your mouth, pain right in front of your ear, or your jaw might even shift to one side when opening.
These trigger points love to develop in musicians (especially violin players who hold their instrument with their jaw), people who've had long dental procedures, and chronic teeth grinders. One professional violinist we treated at Evolve Physical Therapy was amazed when we addressed her pterygoid trigger points: "Twenty years of jaw pain, and it was coming from a muscle I'd never even heard of!"
The medial pterygoid works as a teammate to your masseter, helping close the jaw and create grinding movements. When this muscle develops trigger points, it creates some truly odd symptoms – pain deep inside your mouth and throat, difficulty swallowing, and sensations of ear fullness that no ear doctor can explain.
Treating these hidden muscles requires specialized skills. Sometimes we use external approaches, but for stubborn cases, gentle intra-oral techniques (working inside the mouth with gloved hands) can provide remarkable relief when nothing else has worked.
Neck & Shoulder Contributors
Your jaw doesn't exist in isolation – it's part of a connected system that includes your neck and shoulders. This explains why TMJ trigger points often appear alongside trigger points in these neighboring areas.
The sternocleidomastoid (SCM) is that rope-like muscle running from behind your ear down to your collarbone. When it develops trigger points, it can create pain in your cheek, around your ear, near your eye, and even in your sinuses. Many patients are shocked to find their "sinus headaches" are actually coming from this neck muscle!
Your upper trapezius – that large muscle spanning your shoulders and upper back – can refer pain upward to your jaw and temple when it harbors trigger points. It's a major contributor to tension headaches and can increase overall tightness throughout your head and neck.
Don't forget the suboccipital muscles – those small but mighty muscles at the base of your skull. When tight, they can send pain to the top of your head and behind your eyes, contributing to headaches and increasing tension throughout your jaw.
We often see a domino effect with these muscles. Trigger points in one area can activate "satellite" trigger points in related muscles. For example, that tight upper trapezius from hunching over your computer might create secondary trigger points in your jaw muscles, creating a complex pattern that needs comprehensive treatment.
"Tech neck" from looking down at phones and computers is one of the biggest contributors we see in our Brooklyn practice. As we often tell our patients at Evolve Physical Therapy, treating just the jaw without addressing these connected areas rarely solves the whole problem.
For more information about specialists who can help with this interconnected approach, visit our guide to TMJ Pain Providers.
Symptoms & Self-Assessment
Have you ever woken up with a jaw that feels like it went ten rounds in a boxing match? Or maybe you've noticed a clicking sound when you yawn that wasn't there before? These could be telltale signs of TMJ trigger points at work.
The tricky part about these symptoms is they often masquerade as other conditions, sending many people down expensive treatment rabbit holes before finding the true cause.
Most people with TMJ trigger points experience jaw pain that feels like a deep, persistent ache. This discomfort typically intensifies when you're chewing that crusty Brooklyn bagel or chatting with friends over coffee. You might also notice your jaw making clicking or popping sounds that can be alarming (and sometimes loud enough for others to hear!).
Opening wide becomes a challenge too. Maybe you've noticed you can't yawn fully anymore, or perhaps your jaw seems to open unevenly, shifting to one side. These are classic signs of muscle imbalance caused by those pesky trigger points.
What surprises many of our Brooklyn patients are the symptoms that seem unrelated to the jaw. Ear fullness, ringing, or even occasional dizziness can all stem from TMJ trigger points. Headaches, particularly around the temples or behind the eyes, are incredibly common companions to jaw issues as well.
"I spent thousands on dental work thinking I had tooth problems, only to find my pain was coming from trigger points in my jaw muscles," shared one of our Park Slope patients. "The relief I felt after just two physical therapy sessions was incredible."
Locating Your Own TMJ Trigger Points
Good news—you can do some detective work at home to find your own TMJ trigger points. Think of it as a treasure hunt, except instead of gold, you're finding the source of your discomfort (still valuable!).
Start with your masseter, the workhorse of your chewing muscles. After washing your hands, place your fingers on your cheeks just in front of your ears. Give a gentle clench of your teeth and feel that muscle bulge—that's your masseter saying hello. Now relax and begin pressing into the muscle with moderate pressure. Work your way from top to bottom, feeling for tender spots, nodules, or tight bands that feel like guitar strings under the skin.
When you find a spot that makes you wince, you've likely found a trigger point. Rate the pain on a scale from 0-10—a 7/10 is actually the sweet spot for treatment intensity. Too gentle won't create change, while too painful can cause your muscles to guard.
Next, explore your temporalis muscle by placing your fingers on your temples. This fan-shaped muscle can harbor trigger points that cause headaches and tooth pain in the upper jaw. Use small circular motions and pay special attention to the area near your eyebrows.
The pterygoid muscles are trickier to access but worth investigating. Place your finger just below your cheekbone in front of your ear and press inward and upward while slightly opening and closing your mouth. Tenderness here often signals pterygoid involvement, which commonly causes clicking jaws and ear pain.
True trigger points typically feel like a taut band or small nodule, are quite tender when pressed, and often reproduce your familiar pain pattern or cause pain to radiate elsewhere—like that mysterious earache that appears when you press a certain spot in your jaw.
Want more guidance on self-massage techniques? We've put together detailed instructions here: More info about TMJ Self Massage
When to Seek Professional Diagnosis
While exploring your own trigger points can be enlightening, certain symptoms warrant professional evaluation. Consider booking an appointment if you're experiencing:
Persistent pain lasting more than two weeks, especially if it's getting worse rather than better. Your body's telling you something needs attention.
Lock-jaw or catching sensations where your jaw gets stuck when opening or closing are red flags that shouldn't be ignored. This could indicate disc displacement within the joint itself.
When significant jaw movement limitations start affecting your ability to enjoy your favorite foods or communicate clearly, it's definitely time for professional help.
Tooth pain that has your dentist stumped might actually be referred pain from trigger points. If your dental x-rays look perfect but you're still hurting, consider a TMJ evaluation.
Tinnitus (ear ringing) or dizziness alongside jaw symptoms can be particularly disruptive to daily life and often respond well to proper TMJ treatment.
Severe headaches that coincide with jaw pain might be connected—many "tension headaches" or even "migraines" can actually stem from TMJ trigger points.
Changes in your bite where your teeth suddenly seem to meet differently can indicate muscle imbalances affecting jaw alignment.
Professional evaluation is crucial because several conditions can mimic TMJ trigger point pain. These include dental problems, trigeminal neuralgia, sinus infections, ear infections, salivary gland disorders, arthritis of the TMJ, and rarely, jaw tumors.
At Evolve Physical Therapy in Brooklyn, our evaluation goes beyond just looking at your jaw. We examine your posture, neck mobility, breathing patterns, and even stress levels to understand the full picture of what's happening. As Dr. Janet Travell, the pioneer of trigger point therapy, emphasized: "A thorough examination is essential, as myofascial pain can mimic many other conditions."
When you're ready to move beyond self-assessment, our team is here to help you steer the path to relief. We're experts at differentiating between primary trigger points and symptoms arising from other sources, ensuring you get the right treatment from the start.
Learn more about myofascial pain from this trusted source: Scientific research on myofascial pain
Evidence-Based Treatments & Home Care
Finding relief from TMJ trigger points doesn't have to be a painful journey. At Evolve Physical Therapy, we've seen countless Brooklyn residents transform their jaw pain through a combination of professional care and simple at-home techniques.
The most effective approach to treating TMJ trigger points combines several evidence-based treatments. Think of it as attacking the problem from multiple angles—what works best is rarely just one technique but rather a thoughtful combination custom to your specific needs.
Manual therapy forms the foundation of most successful treatment plans. This includes gentle hands-on techniques like trigger point release, where your therapist applies precise pressure to those knotted muscle fibers until they relax. Myofascial release techniques address the connective tissue surrounding your jaw muscles, while joint mobilization helps restore proper movement patterns.
"I was skeptical that someone's hands could fix what felt like such a complex problem," shares Maria, a patient from Williamsburg. "But after my first session, I could open my mouth wider than I had in months. It was like magic."
For deeper or more stubborn trigger points, specialized interventions like dry needling or acupuncture can be game-changers. Dry needling involves inserting thin filament needles directly into trigger points, creating a "reset" response in the muscle. TENS therapy uses gentle electrical stimulation to reduce pain and muscle tension, while ultrasound therapy delivers deep warmth to tight tissues.
For severe cases that haven't responded to other treatments, options like trigger point injections or Botox may provide relief. These medical interventions work by either reducing inflammation or temporarily limiting muscle overactivity.
Movement is medicine when it comes to TMJ trigger points. Your physical therapist will design a progressive exercise program including jaw relaxation techniques, controlled opening exercises, and movements that retrain your jaw to move properly. We'll also address any postural issues in your neck and shoulders that might be contributing to your jaw problems.
Recent research strongly supports this comprehensive approach. A 2021 study concluded that "conservative manual techniques of physical therapy, including massage, are highly beneficial in TMJD management, with significant improvements in pain relief and maximal mouth opening." This validates what we've seen at Evolve Physical Therapy—hands-on care combined with targeted exercises creates lasting relief.
Don't overlook the power of behavioral interventions. Stress management techniques, diaphragmatic breathing, and improved sleep habits can significantly reduce jaw tension. Some patients benefit from biofeedback, which helps you become aware of muscle tension you might not even realize you're holding.
More info about Physical Therapy Services for TMJ
Self-Massage & Stretch Routine
You don't have to wait for your next appointment to find relief from TMJ trigger points. These simple self-care techniques can make a huge difference when practiced regularly:
Start with your masseter—that powerful chewing muscle running along your jawline. Make a loose fist and use your knuckles to apply moderate pressure in small circular motions for about 30-60 seconds. This knuckle kneading technique helps break up tension without causing additional irritation.
Next, try some ischemic compression on tender spots. Use your fingertips to press firmly into painful areas until you feel what I call a "good hurt"—about 7 out of 10 on the pain scale. Hold for 30-60 seconds until you feel the tension melt away. The pressure temporarily reduces blood flow, and when released, fresh blood rushes in, bringing nutrients and removing waste products.
"I was amazed how something so simple could work so well," says Tom, a patient from Bay Ridge. "Finding those tender spots and holding pressure for just a minute gave me more relief than the muscle relaxers my doctor prescribed."
Don't forget your temporalis muscle! Use your fingertips to make small circles throughout your temple region, paying special attention to the area near your eyebrows where tension often accumulates.
Gentle stretching complements your massage work beautifully. Try this simple jaw opening stretch: place your thumbs on your bottom teeth and fingers on your top teeth, then gently guide your jaw open to a comfortable position. Hold for 10 seconds and repeat 5 times. This helps restore normal range of motion without forcing your jaw.
For lateral stretches, gently guide your lower jaw to the right until you feel a mild stretch, hold for 5 seconds, then repeat on the left. Five repetitions in each direction is usually enough to feel relief.
Diaphragmatic breathing might seem unrelated to jaw pain, but it's remarkably effective at reducing overall tension. Place one hand on your chest and one on your abdomen, then breathe deeply so your abdomen rises more than your chest. Practice for just 5 minutes, 2-3 times daily, and you'll likely notice less jaw clenching.
Heat and ice can be your best friends during flare-ups. Apply moist heat for 10 minutes before exercises to improve tissue flexibility, then use ice afterward to calm any inflammation. Some of my patients swear by alternating between the two for maximum relief.
More info about Massage for Teeth Grinding
In-Clinic Interventions That Work
While self-care is powerful, sometimes you need professional help to fully resolve TMJ trigger points. At Evolve Physical Therapy in Brooklyn, we offer several evidence-based treatments that provide significant relief.
Manual trigger point release is our bread-and-butter technique. Our physical therapists use specific pressure and release techniques that target the exact source of your pain. It's remarkably effective—many patients report immediate improvement in jaw movement and pain levels after just one session.
For stubborn trigger points that don't respond to manual techniques, dry needling offers a more direct approach. This isn't acupuncture (though that can help too!); it's a precise intervention where thin filament needles are inserted directly into trigger points to elicit a "local twitch response." This microscopic muscle contraction helps reset the dysfunctional area. Research backs this up—a single-blind, randomized controlled trial found that "deep dry needling increased pressure pain threshold and pain-free jaw opening in TMD patients compared to sham treatment."
"I was nervous about the needles," admits Sarah from Prospect Heights, "but I barely felt them going in. What I did feel was relief—for the first time in years, I could open my mouth without that awful clicking sound."
In cases where pain is severe or persistent, trigger point injections may be recommended. These injections deliver a small amount of local anesthetic (sometimes with corticosteroid) directly to the trigger point. Studies show that about 58% of patients report complete pain relief immediately after injection, with many others experiencing significant improvement.
For patients with severe muscle hyperactivity or teeth grinding, Botox therapy offers 3-6 months of relief by temporarily reducing muscle contractions. While we typically try more conservative approaches first, Botox can be life-changing for those who haven't responded to other treatments.
Therapeutic ultrasound uses sound waves to increase blood flow and promote healing in deeper tissues. It's particularly helpful for reaching the pterygoid muscles tucked away inside your mouth—areas that are difficult to access with manual techniques alone.
TENS therapy delivers mild electrical stimulation to reduce pain and muscle spasm. Many patients describe a pleasant tingling sensation during treatment, followed by noticeably reduced jaw tension. We often combine TENS with hands-on work for improved results.
Every patient at Evolve receives an individualized exercise program addressing their specific needs. These aren't generic handouts—they're carefully crafted progressions that build on your in-clinic treatments and help create lasting change in how your jaw functions.
At Evolve Physical Therapy, we believe in combining these approaches for optimal results. Our Mill Basin patient Mark puts it best: "After seeing three different specialists with no relief, the combination of manual therapy and dry needling at Evolve finally gave me my life back. For the first time in two years, I can eat without pain."
Prevention & Long-Term Management
Managing TMJ trigger points isn't just about addressing current symptoms—it's about creating lasting jaw health for the future. At Evolve Physical Therapy, we believe prevention is truly the best medicine.
Think of your jaw health as a house—you need a solid foundation to prevent problems from returning. That foundation starts with proper ergonomics. Something as simple as adjusting your computer monitor to eye level can prevent the forward head posture that strains your jaw muscles all day long. Many of our Brooklyn patients are surprised to learn that their desk setup was a major contributor to their jaw pain!
Working with your dentist is another crucial piece of the puzzle. A properly fitted night guard can significantly reduce the impact of nighttime teeth grinding. We regularly coordinate care with local dentists to ensure our physical therapy approaches complement any dental interventions you might need.
Stress management might sound cliché, but it's absolutely essential for TMJ trigger points. Your jaw is often where tension shows up first when you're stressed. Simple mindfulness practices, even just five minutes of focused breathing each day, can make a remarkable difference. One patient told us, "I never connected my jaw pain to my stressful job until my therapist at Evolve pointed it out. The breathing techniques she taught me have been life-changing."
Don't underestimate the power of good nutrition and quality sleep. Anti-inflammatory foods and proper hydration support muscle healing, while poor sleep can increase pain sensitivity and trigger muscle tension. We work with patients to identify specific dietary triggers and optimize sleep positions that reduce jaw strain.
As you recover, we'll help you gradually return to normal activities. That might mean slowly reintroducing chewy foods or monitoring how your jaw feels after long conversations. This measured approach prevents setbacks and builds confidence.
Regular "tune-up" sessions at Evolve can catch small issues before they become big problems. Research consistently shows that comprehensive management addressing multiple factors yields better long-term outcomes than quick fixes.
Lifestyle Hacks to Keep TMJ Trigger Points Away
The small daily habits often make the biggest difference in preventing TMJ trigger points from returning. Here's what works for our Brooklyn patients:
Your morning coffee might be working against you. Caffeine can increase muscle tension throughout your body, including your jaw muscles. Try cutting back gradually or switching to half-decaf to see if it helps.
That pack of gum in your purse? It might be time to find a new habit. Excessive gum chewing is like making your jaw muscles run a marathon every day. Instead, try sugar-free mints or simply sipping water throughout the day.
Your smartphone could be a major culprit too. When you look down at your phone, your head moves forward, putting strain on both neck and jaw muscles. Try holding your phone at eye level instead—your jaw will thank you! And for those long calls with friends or work colleagues, use a headset rather than cradling the phone between your ear and shoulder.
The "tongue-up, teeth-apart" position should become your new normal. When your jaw is relaxed, your tongue should rest lightly on the roof of your mouth with your teeth slightly separated. This simple position prevents unnecessary muscle tension. As one patient from Park Slope shared, "Just being aware of my jaw position throughout the day reduced my pain by at least 70%."
Take micro-breaks throughout your day. Set a 20-minute timer on your phone and use each alert as a reminder to check your jaw position, do a quick stretch, or practice the "yawn-sigh" technique (yawn gently, then exhale with a sigh to release tension).
Monitoring Progress Over Time
Keeping track of your improvement is both motivating and essential for long-term management of TMJ trigger points. Here's how to monitor your progress effectively:
Start a simple pain diary. You don't need anything fancy—just note your daily pain levels on a scale of 0-10, along with any activities that seemed to increase or decrease your symptoms. This information is incredibly valuable during follow-up appointments at Evolve, helping us pinpoint patterns you might not otherwise notice.
Measure your mouth opening regularly. Use a small ruler to track the distance between your upper and lower front teeth when you open as wide as comfortably possible. Normal opening is typically 40-50mm. Improvements in this measurement provide concrete evidence that your treatment is working.
Pay attention to functional improvements too. Can you now eat an apple without pain? Talk through a long meeting without jaw fatigue? These real-life victories are sometimes more meaningful than numbers on a scale.
Perform a weekly self-check of your key muscles. Using the palpation techniques we teach at Evolve, assess whether your trigger points are becoming less sensitive over time. This self-awareness becomes a powerful tool for early intervention if problems start to return.
Schedule quarterly check-ins with your physical therapist, even after your symptoms resolve. These "maintenance visits" allow us to adjust your home program based on your progress and catch any small issues before they become problematic. Think of these visits like dental cleanings—preventive care that saves you trouble down the road.
As a Williamsburg patient recently told us, "The tracking tools my therapist gave me helped me see my progress when I was feeling discouraged. Now I use them to make sure I stay on track and catch any flare-ups early."
More info about Temporomandibular Joint Dysfunction Relaxation Techniques
Frequently Asked Questions about TMJ Trigger Points
Do TMJ trigger points show on MRI or X-ray?
If you've ever wondered whether those painful knots in your jaw muscles would show up on medical imaging, you're not alone. The truth is, standard X-rays and MRIs typically don't capture TMJ trigger points. While these imaging techniques excel at showing bones, joints, and larger soft tissue structures, the tiny changes in muscle fibers that create trigger points are simply too small to appear.
"It's like trying to see grains of sand from an airplane," explains one of our physical therapists at Evolve. "We don't need expensive imaging to identify trigger points. Our hands are actually the most sensitive and specific tools for detecting these tender nodules in muscle tissue."
In research settings, some specialized techniques like elastography (which measures tissue stiffness) and certain MRI protocols can sometimes visualize trigger points, but these advanced methods aren't typically available in everyday clinical practice.
Instead, diagnosing TMJ trigger points relies on a combination of skilled manual examination by trained clinicians, your detailed symptom history, assessment of your jaw movement, and how you respond to treatment. This hands-on approach has proven to be both effective and reliable.
Can dental issues and TMJ trigger points coexist?
They absolutely can—and often do! This relationship typically works as a two-way street, with each condition potentially influencing the other.
When dental problems contribute to trigger points, it might be because an improper bite forces your jaw muscles to work unevenly. Dental pain can cause protective muscle guarding, while lengthy dental procedures can overload those same muscles. Even missing teeth can change how you chew, creating uneven muscle strain.
On the flip side, TMJ trigger points can wreak havoc on your dental health. Chronic muscle tension increases wear and tear on teeth, while referred pain from trigger points can feel remarkably similar to a toothache (leading to unnecessary dental work). The altered jaw mechanics from muscle dysfunction can affect your bite alignment, and increased clenching or grinding from muscle tension can damage teeth over time.
"My dentist and physical therapist communicated about my case, which made all the difference," shared a patient from Marine Park. "The night guard from my dentist and the trigger point therapy from Evolve worked together to finally solve my jaw pain."
This complex relationship highlights why we often collaborate with local dentists in Brooklyn to coordinate comprehensive care plans. By addressing both dental issues and muscle dysfunction, we can achieve outcomes that neither approach could accomplish alone.
Are trigger-point injections safe?
If you're considering trigger point injections, you'll be glad to know they're generally quite safe when performed by properly trained healthcare providers. That said, like any medical procedure, they do come with considerations worth discussing.
Most people experience only temporary soreness at the injection site—similar to what you might feel after a flu shot. Serious complications like infection, bleeding, or nerve injury are rare, and allergic reactions to the anesthetics used are uncommon but possible.
Some people aren't good candidates for injections, including those with bleeding disorders or who take blood thinners, those with an infection at the injection site, anyone with allergies to the injectable solutions, or people with significant needle phobia.
The good news? Research shows impressive results, with about 58% of patients reporting complete pain relief immediately after a trigger point injection. Most others experience significant improvement, with pain levels dropping dramatically. Some people need a series of injections for the best results.
Interestingly, studies suggest that the mechanical disruption of the trigger point with the needle itself (rather than the medication) may be the primary healing factor. This explains why both dry needling and various injection solutions can be effective.
At Evolve Physical Therapy in Brooklyn, we typically start with gentle, non-invasive approaches like manual therapy and targeted exercises, reserving injections for cases that don't respond to these conservative methods. Many of our patients achieve excellent results without ever needing an injection.
"I was terrified of needles but desperate for relief," one Williamsburg patient told us. "When more conservative treatments weren't enough, I finally tried a trigger point injection. The procedure was much less scary than I imagined, and the relief was almost immediate. I wish I hadn't waited so long!"
Conclusion
Finding relief from TMJ trigger points isn't just about treating symptoms—it's about addressing the root causes of your jaw pain for lasting comfort. Throughout this guide, we've explored how these tiny but troublesome muscle knots can create a cascade of pain that affects your daily life, from speaking and eating to sleeping and concentrating.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we've seen countless patients walk through our doors frustrated after trying numerous treatments without success. Many have been to dentists, doctors, and specialists, only to be told, "We can't find anything wrong." The reality is that TMJ trigger points often fly under the radar of conventional testing, yet they're responsible for so much discomfort.
Our approach combines the science of physical therapy with the art of hands-on care. We don't just treat your jaw—we look at how your neck, shoulders, posture, and even daily habits contribute to your pain. This holistic perspective makes all the difference for our Brooklyn neighbors from Park Slope to Mill Basin.
One patient recently told us, "For the first time in three years, I can eat a sandwich without pain. I didn't realize how much my jaw problems were limiting my life until they were gone."
The journey to jaw comfort typically combines several key elements:
Professional manual therapy to deactivate painful trigger points
Personalized exercises that restore proper muscle balance
Practical lifestyle modifications that prevent recurrence
Stress management techniques that reduce unconscious jaw tension
Healing takes time and consistency. The muscles that developed TMJ trigger points didn't tighten overnight, and they won't completely release in a single session. But with the right approach, most of our patients experience significant improvement within 4-6 weeks.
Whether you're dealing with occasional jaw tension or chronic TMJ pain that's affected you for years, there's hope. Our team at Evolve Physical Therapy is passionate about helping you reclaim comfort and function in your daily life.
Ready to find relief from those stubborn TMJ trigger points? We're here to help you steer the path to recovery with expertise, compassion, and proven techniques that work.
Your Guide to Finding Myofascial Release Therapy in Your Area
Finding Relief: How to Locate Myofascial Release Therapy in Your Area
Looking for myofascial release therapy near me? Here's how to find qualified practitioners:
Use specialized directories: Search the John F. Barnes' Myofascial Release Therapist Directory (1,000+ therapists nationwide) or the National Association of Myofascial Trigger Point Therapists directory
Check credentials: Look for therapists with 100+ hours of specialized training
Search terms: Use "myofascial release therapist" + your city or "remote myofascial therapy" for telehealth options
Verify insurance: Ask if they provide receipts for out-of-network reimbursement
Initial consultation: Most qualified therapists offer a consultation to discuss your specific condition
If you're experiencing persistent pain, restricted movement, or tightness that won't resolve with conventional treatments, myofascial release therapy near me might be the solution you've been searching for. This specialized hands-on technique targets the fascial system—a three-dimensional web of connective tissue surrounding every muscle, nerve, organ, and cell in your body. When this tissue becomes restricted, it can exert up to 2,000 pounds of pressure per square inch on pain-sensitive structures, creating symptoms that often don't show up on standard medical tests.
Myofascial release therapy works differently than massage or standard physical therapy. Instead of focusing solely on muscles, it addresses the entire fascial network through gentle, sustained pressure applied directly to the skin without oils or creams. This approach allows therapists to detect restrictions and gradually release them, providing lasting relief where other treatments may have failed.
I'm Lou Ezrick, a physical therapist specializing in manual therapy techniques including myofascial release therapy near me in Brooklyn, where I've helped thousands of patients with chronic pain and mobility restrictions through customized treatment plans focused on addressing fascial restrictions at their root cause.
Understanding Myofascial Release Therapy
Have you ever felt like your pain has a life of its own, moving around your body and refusing to respond to typical treatments? The answer might be hiding in your fascia—the body's hidden web of connective tissue that most traditional treatments overlook.
Myofascial release therapy (MFR) is a specialized hands-on approach that works directly with this fascial system to eliminate pain and restore movement. At Evolve Physical Therapy, we see fascia as the missing piece in many pain puzzles.
"Think of fascia as the body's internal sweater," explains our physical therapy team at Evolve Physical Therapy + Sports Rehabilitation. "When it gets snagged in one place, it can pull and create tension everywhere else. Releasing these restrictions often becomes the breakthrough moment for patients who've tried everything else."
Fascia forms a continuous three-dimensional web from head to toe, surrounding every muscle, nerve, blood vessel, organ, and cell in your body. When healthy, it's flexible and fluid, allowing everything to glide smoothly as you move. But trauma, inflammation, surgery, poor posture, or even emotional stress can cause this tissue to tighten and restrict.
The most fascinating thing? These restrictions rarely show up on standard medical tests like X-rays or MRIs, yet they can exert up to 2,000 pounds of pressure per square inch on pain-sensitive structures—that's like carrying a small car on your tissues!
The Science Behind Fascia
What makes fascia so special is its unique composition—a beautiful arrangement of collagen and elastin fibers suspended in a gel-like ground substance. This structure gives fascia both incredible strength and flexibility, but also makes it vulnerable to getting "stuck."
Two key scientific properties make myofascial release particularly effective:
Piezoelectric effect: When gentle pressure is applied to fascia, it creates a small electrical charge that actually stimulates tissue healing and remodeling at the cellular level.
Viscoelastic flow: Unlike muscles that respond quickly to pressure, fascia changes states—from a more solid gel to a more fluid sol—when gentle pressure is applied over time. This is why the "time element" in myofascial release (3-5 minutes or longer per technique) is absolutely crucial for lasting change.
Conditions Myofascial Release Can Help
At our Brooklyn practice, we've seen myofascial release therapy near me transform lives by addressing conditions that haven't responded to conventional approaches:
Back and neck pain often resolves when we release the complex fascial restrictions along the spine that pull vertebrae out of alignment. Fibromyalgia symptoms frequently improve as we address the whole-body fascial tension patterns that contribute to widespread pain signals.
For TMJ dysfunction, releasing restrictions in jaw, face, and neck fascia can eliminate years of pain and clicking. Plantar fasciitis responds beautifully when we treat not just the foot, but the connected fascial lines running all the way up the leg.
Headaches and migraines often diminish or disappear when we address fascial restrictions in the neck, shoulders, and cranium. Post-surgical pain and scarring improves as we break down restrictive scar tissue that pulls on surrounding fascia.
Athletes with sports injuries recover faster and perform better once we restore fascial mobility. Carpal tunnel symptoms frequently resolve by releasing fascial restrictions not just in the wrist, but along the entire arm and shoulder pathway. Even chronic fatigue syndrome and pelvic pain respond to comprehensive fascial treatment.
One of our Brooklyn clients shared: "After my car accident, I lived with constant neck pain for three years. Every doctor told me I'd just have to live with it. After my third myofascial release therapy session at Evolve, I finally felt that deep, stuck feeling melt away. It was addressing something that all my previous treatments had completely missed."
Want to learn more about manual therapy approaches? Check out More info about manual therapy or explore the Scientific research on fascia mechanics to understand the growing evidence behind this approach.
How Myofascial Release Works & Why It's Different
When you're searching for myofascial release therapy near me, it's important to understand what makes this approach so unique. Unlike traditional therapies that might focus only on where you feel pain, myofascial release addresses the entire interconnected web of fascia throughout your body.
The magic happens through gentle, sustained pressure applied directly to your skin without oils or lotions. This skin-to-skin contact allows your therapist to feel the subtle restrictions in your fascia and follow them to their true source—which is often nowhere near where you're experiencing pain!
"Many of our clients are surprised to learn that the pain in their shoulder might actually stem from restrictions in their hip or lower back," explains our physical therapy team at Evolve. "That's the fascinating thing about fascia—it's all connected, so problems can manifest far from their origin."
What truly sets myofascial release apart is its respect for your body's natural healing timeline:
The time element is crucial—gentle pressure is maintained for 3-5 minutes or longer, giving your fascia the chance to soften and release through what we call "viscoelastic flow." Your body isn't rushed or forced.
Direct skin contact without slippery products enables your therapist to accurately detect even the subtlest fascial restrictions and changes.
By following the fascial system rather than just focusing on painful spots, we address the true cause of your discomfort, not just the symptoms.
Your conscious awareness of sensations during treatment actually helps facilitate release—this is a collaborative process between you and your therapist.
The whole-body approach recognizes that treating isolated areas often misses the bigger picture of how fascia connects everything in your body.
Gentle Sustained Pressure vs Deep Tissue
"But isn't this just deep tissue massage?" We hear this question frequently, and the answer is a definite no. While both approaches have their place, they work on entirely different principles.
Deep tissue massage typically uses firm, sometimes uncomfortable pressure and strokes to break up muscle tension directly. It's like pressing hard to smooth out a wrinkle in fabric.
Myofascial release, by contrast, uses gentle to moderate sustained pressure that works with your body's natural responses. As one of our Brooklyn clients perfectly described: "I was surprised that such gentle pressure could create such profound changes. It didn't hurt during treatment like deep tissue massage often does, yet the results were much more lasting."
The key difference is that myofascial release allows your tissues to unwind and release naturally, rather than forcing change. It's like holding the wrinkled fabric under gentle tension until it naturally relaxes and smooths out.
At Evolve Physical Therapy + Sports Rehabilitation, we find this gentler approach often yields better long-term results, especially for chronic conditions where aggressive treatment might actually trigger more pain.
Safety and Evidence
Good news—myofascial release therapy is generally very safe when performed by a qualified practitioner. Because we use gentle pressure and work with your body's natural responses rather than forcing change, the risk of injury is minimal.
Some patients experience what we call a "healing crisis" or "therapeutic pain"—a temporary increase in symptoms that typically lasts 2-3 days as your body adjusts to fascial changes. Though it might sound concerning, this is actually a positive sign that the treatment is creating meaningful change in your tissues.
Research on myofascial release continues to grow stronger, with studies showing impressive effectiveness for conditions like fibromyalgia pain, chronic low back pain, plantar fasciitis, post-mastectomy pain, and tension headaches.
One aspect that surprises many clients is the importance of hydration. Water helps your fascia maintain its optimal gel-like state, making it more responsive to treatment. We recommend drinking 12-16 eight-ounce glasses of water daily when undergoing myofascial release therapy. Think of it as helping your fascia stay pliable and responsive to the changes we're creating.
Myofascial Release Therapy Near Me: Step-by-Step Search Strategy
Looking for myofascial release therapy near me doesn't have to feel overwhelming. I've helped hundreds of patients find the right care, and I'm happy to share my insider approach to connecting with qualified practitioners who can truly help you heal.
Let's break down the search process into manageable steps that anyone can follow:
First, start with specialized directories that focus specifically on myofascial practitioners. The John F. Barnes' Myofascial Release Therapist Directory lists over 1,000 therapists nationwide who have completed his specific training methodology. Similarly, the National Association of Myofascial Trigger Point Therapists Directory features practitioners with extensive training—many with 100+ to 600+ hours of specialized education. These resources help ensure you're finding therapists with proper training rather than those who might casually list myofascial release as a service.
Don't forget to explore local resources too! A simple Google search for "myofascial release therapy near me" plus your city name can yield valuable results. Your primary care physician might also have trusted referrals, and local chronic pain support groups often share recommendations based on personal experiences. Here in Brooklyn, you can always contact us at Evolve Physical Therapy + Sports Rehabilitation to discuss our myofascial release services.
"When I first started looking for help, I felt completely lost," shares Maria, one of our patients. "Finding someone through a specialized directory saved me months of trial and error with practitioners who weren't properly trained."
If you live in an area without qualified therapists nearby, consider telehealth options. Search for "remote myofascial therapy" or "telehealth myofascial release" to find practitioners who offer virtual sessions focused on teaching self-treatment techniques you can perform at home.
Criteria for Choosing a Qualified Therapist
Not all myofascial release therapists bring the same level of expertise to the table. When evaluating potential practitioners, look for these key qualifications:
A current state license in physical therapy, massage therapy, or another healthcare profession forms the foundation. Beyond basic licensure, specialized training makes all the difference—seek therapists with John F. Barnes Myofascial Release seminars (ideally 100+ hours), Certification in Myofascial Trigger Point Therapy (CMTPT), or advanced training in fascial techniques.
Experience with your specific condition is invaluable. Don't hesitate to ask if they've successfully treated others with similar issues. Patient reviews and testimonials offer real-world insights into their effectiveness, while a professional approach should include a thorough evaluation and customized treatment plan.
As one of our Brooklyn patients noted, "When I was searching for 'myofascial release therapy near me,' I found that therapists' training varied widely. Finding someone with advanced John Barnes training made all the difference in my treatment outcomes."
How to Verify "myofascial release therapy near me" Listings
Trust but verify! Here's how to confirm a therapist's credentials before booking:
Most state licensing boards offer online verification systems where you can check a practitioner's current status. Legitimate therapists typically maintain memberships in recognized professional associations, which you can verify through organization websites.
Before committing to a full treatment plan, schedule a consultation. Most qualified therapists welcome this opportunity to discuss your condition and explain their approach. During this meeting, ask specific questions about their training—when and where they trained, their continuing education, and their experience with your particular issues.
Red Flags to Avoid
While searching for myofascial release therapy near me, stay alert for warning signs that might indicate less-than-ideal practitioners:
Be wary of anyone promising instant cures or miraculous results—genuine healing takes time. Qualified therapists always perform thorough hands-on evaluations before treatment. They should clearly explain their approach and treatment plan in terms you can understand.
Watch out for practitioners who can't demonstrate specific training in myofascial techniques or who use high-pressure sales tactics to sell package deals. And of course, numerous negative reviews or complaints should give you pause.
Finding the right therapist is worth the effort. Your body deserves care from someone who truly understands the complex nature of fascial restrictions and how to effectively release them.
Preparing for Your First Session & Maximizing Results
Found your perfect myofascial release therapy near me practitioner? Fantastic! Now let's make sure you get the most from your sessions. A little preparation goes a long way toward helping you achieve the relief you're seeking.
What to Wear and Bring
Myofascial release works best with direct skin contact—no slippery oils or lotions involved. This helps your therapist accurately feel fascial restrictions and apply the right amount of pressure.
For clothing, think comfort and accessibility:
"We recommend our Brooklyn patients wear comfortable, minimal clothing that allows access to treatment areas while maintaining modesty," our team at Evolve Physical Therapy + Sports Rehabilitation often tells new patients. "Many clients find that athletic wear works well."
Women typically feel most comfortable in shorts and a sports bra, a two-piece swimsuit, or comfortable underwear with a bra. Men usually opt for gym shorts or comfortable underwear. The key is wearing something that lets your therapist access the areas needing treatment while ensuring you feel at ease.
Don't forget to bring a water bottle—hydration is crucial before and after treatment! And it's best to skip lotions, oils, or heavy perfumes on treatment day, as they can make it harder for the therapist to work effectively with your fascia.
What to Expect During Your First Visit
Your initial appointment is about building the foundation for successful treatment. Most first visits follow a similar pattern:
First, your therapist will conduct a comprehensive evaluation, taking time to understand your history, symptoms, and goals. This typically includes both conversation and hands-on assessment to map out fascial restrictions throughout your body.
Next comes the treatment explanation, where your therapist will share what they've finded and outline their proposed approach. This is a great time to ask questions and make sure you understand the process.
Most practitioners include an initial treatment during your first visit, giving you a taste of the technique and beginning the healing process right away.
Before you leave, you'll receive home care instructions—simple techniques you can perform between sessions to improve your progress. These might include gentle stretches, self-massage with therapy balls, or movement practices.
Plan for 60-90 minutes for your first appointment. This longer duration allows adequate time for both thorough assessment and the slow, sustained pressure that makes myofascial release so effective.
Number of Sessions, Costs, Insurance
"How many sessions will I need?" is probably one of the first questions on your mind. The honest answer is: it depends on your unique situation.
For recent or minor issues, you might find significant relief in just 1-3 sessions. That sprained ankle from last month or tension headache that started last week? These often respond quickly to treatment.
Chronic or complex conditions typically require more time—often 6 or more sessions. If you've been dealing with back pain for years or fibromyalgia for decades, your fascia has likely developed complex patterns of restriction that take longer to unwind.
Many therapists recommend an initial series of 3 visits within a 2-week period. This gives them enough time to assess how your body responds and adjust their approach accordingly.
As for costs, myofascial release sessions typically range from $100-$200 per hour, depending on your location and your therapist's credentials. Many practitioners offer package deals that provide savings when you book multiple sessions.
Insurance coverage varies widely. Many myofascial release specialists operate as out-of-network providers but can provide detailed receipts for you to submit for possible reimbursement. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we're committed to transparency about costs and helping patients maximize their insurance benefits whenever possible.
At-Home Self-Care Between Visits
What happens between sessions can be just as important as the treatment itself. Your therapist will likely recommend several self-care practices to maintain and improve your progress:
Hydration tops the list—aim for 12-16 glasses of water daily. Water helps keep your fascia supple and responsive to treatment. As one of our Brooklyn patients put it, "I never realized how much better I'd feel just by upping my water intake!"
Self-treatment techniques give you tools to address tension between appointments. Your therapist might recommend specific uses for foam rollers or therapy balls, or teach you gentle stretches targeted to your unique restrictions.
Developing body awareness helps you catch tension before it becomes problematic. Many patients find they've been unconsciously clenching their jaw, hunching their shoulders, or holding their breath—simple awareness can help break these patterns.
Stress management practices like deep breathing, meditation, or gentle movement help prevent tension from rebuilding in your fascia. Even five minutes of mindful breathing can make a difference.
Temporary activity modifications might be suggested to give your body space to heal. This doesn't mean stopping everything you love, but perhaps adjusting how you perform certain movements or taking short breaks during activities that typically aggravate your condition.
"I teach all my Brooklyn patients specific self-care techniques," says our physical therapy team. "Those who consistently practice these between sessions typically see faster and more lasting results."
By preparing properly for your sessions and following through with recommended self-care, you'll be giving yourself the best chance for lasting relief. Healing isn't just something that happens to you—it's a process you actively participate in, with your therapist as your skilled guide along the way.
Frequently Asked Questions about Myofascial Release Therapy
Is myofascial release therapy safe for everyone?
When you're searching for myofascial release therapy near me, safety is naturally a top concern. The good news is that myofascial release is generally very gentle and safe for most people. That said, certain conditions do require some special consideration:
Pregnancy isn't a deal-breaker—many pregnant women benefit greatly from modified myofascial techniques that help with changing body mechanics. If you're undergoing cancer treatment, it's best to have a conversation with your oncologist first, as they can advise on timing and appropriate modifications.
"Safety is always our primary concern," explains our team at Evolve Physical Therapy. "We adapt our approach based on each person's unique health situation, which is why that initial evaluation is so important."
For those with recent injuries, osteoporosis, or who take blood-thinning medications, don't worry—treatment is still possible! We'll simply adjust our pressure and techniques to ensure your comfort and safety. The key is open communication—always share your complete health history with your therapist so they can tailor the treatment specifically for you.
How many sessions before I feel results?
This might be the question I hear most often in our Brooklyn clinic! The honest answer is: it depends on your unique situation. Most people notice some kind of change after their very first session—sometimes it's dramatic relief, other times it's more subtle.
Here's what typically happens:
After your first session, you might experience an "ah-ha" moment where your body feels different—perhaps lighter or more balanced. By sessions 2-3, most people notice more substantial improvements that actually last. If you're addressing a complex or long-standing issue, sessions 4 and beyond often bring progressive, deeper changes as we work through layers of fascial restrictions.
One of our clients at Evolve put it perfectly: "I'd been dealing with shoulder pain for years. After my first myofascial release session, I felt something shift—it wasn't gone, but it was different. By my fourth visit, I had 80% less pain and could finally sleep through the night again."
The timeline varies based on how long you've had the problem (newer issues generally resolve faster), how complex your condition is, and how consistently you follow the self-care recommendations between sessions. Your body's natural healing rate plays a role too—we're all unique!
Can I combine MFR with other treatments?
Absolutely! In fact, myofascial release often works beautifully alongside other therapies, creating a synergistic effect. At Evolve Physical Therapy in Brooklyn, we frequently combine myofascial release therapy near me with complementary approaches for comprehensive care.
Myofascial release can prepare your body to respond better to exercise therapy by improving tissue mobility first. Many clients find great success pairing MFR with chiropractic adjustments—the fascia release makes the adjustments more effective and longer-lasting. Acupuncture, yoga, Pilates, and traditional massage can all work harmoniously with myofascial techniques.
The key is communication. Let all your healthcare providers know about your full treatment plan so they can coordinate their approaches. This team approach often leads to the best outcomes, addressing your health from multiple angles.
What if I feel worse after treatment?
Don't panic if you feel a bit sore or experience shifting sensations after your session! This temporary response, sometimes called a "healing crisis" or "therapeutic pain," is actually quite normal. It typically lasts 24-72 hours and is your body's way of adjusting to the fascial changes we've introduced.
"I always prepare my clients for the possibility of post-treatment sensations," shares our physical therapy team. "Think of it like spring cleaning—sometimes things look messier while you're in the middle of reorganizing, but the end result is worth it."
To manage any post-treatment discomfort, stay super hydrated (water helps your fascia maintain its optimal state), take a warm bath, move gently, and rest as needed. If anything feels concerning or lasts longer than a few days, reach out to your therapist—we're here to guide you through the process.
How is myofascial release different from regular massage?
When you're looking for myofascial release therapy near me, understanding this key difference helps set appropriate expectations. While both treatments involve hands-on care, they operate on fundamentally different principles.
Traditional massage primarily targets muscles using rhythmic strokes, kneading, and usually involves oils or lotions. The therapist typically moves relatively quickly from area to area, focusing on muscle relaxation and circulation.
Myofascial release, in contrast, works with your body's connective tissue system using gentle, sustained pressure applied directly to the skin without lubricants. Your therapist might hold a single position for 3-5 minutes or longer—this time element is crucial for allowing the fascia to respond and release.
"The first time I experienced myofascial release, I was surprised how different it felt," recalls a regular client at our Brooklyn clinic. "It wasn't the typical 'pressure and move on' approach I was used to. My therapist stayed in one spot where I felt tightness until I could actually feel something melting and releasing. The results lasted so much longer than regular massage."
While massage feels wonderful and has many benefits, myofascial release specifically targets restrictions in the fascial system that might be creating pain patterns throughout your body. Many people find value in both approaches, either at different times or as complementary treatments in their wellness routine.
Conclusion
Finding effective myofascial release therapy near me can truly be life-changing when you've been struggling with persistent pain or limited movement that just won't respond to conventional treatments. After helping thousands of Brooklyn residents find relief through fascial techniques, I've seen how this specialized approach often provides the missing piece in many healing journeys.
At Evolve Physical Therapy + Sports Rehabilitation, we take pride in offering expert myofascial release therapy that goes beyond simply addressing symptoms. Our hands-on approach looks at your body as an interconnected whole, targeting the underlying fascial restrictions that might be creating pain in seemingly unrelated areas.
"The most rewarding part of practicing myofascial release is watching patients refind activities they thought were lost to them forever," shares our physical therapy team. "Whether it's a grandmother who can finally pick up her grandchild again or an athlete returning to their sport after a stubborn injury, these victories make all the difference."
If you're in Brooklyn—whether you call Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin home—our team is ready to help you move better and feel better through personalized myofascial techniques custom to your unique needs and goals.
Successful treatment involves several key elements: finding a properly trained therapist with specialized fascial training, committing to your recommended treatment plan, practicing your self-care techniques between sessions, and maintaining open communication with your provider about your progress.
The journey to lasting pain relief often begins with a single step. Your fascial system has an amazing capacity to heal when given the right environment and techniques. As one of our long-term patients recently told us, "I wish I'd found myofascial release years ago—it's the difference between managing pain and actually healing."
Ready to experience the benefits of myofascial release therapy for yourself? Contact Evolve Physical Therapy + Sports Rehabilitation today to schedule your initial evaluation. Our Brooklyn team is ready to help you take that first step toward lasting relief and improved function. Your body has been talking to you—now it's time to listen and respond with the care it deserves.
7 of the Best Massage Services in Brooklyn
Brooklyn's Best Massage Therapy Options
Massage therapy Brooklyn offers a wide range of specialized services to help you relieve pain, reduce stress, and improve your overall wellness. Here's a quick overview of the top massage services available in Brooklyn:
Massage Type Best For Average Cost Top-Rated Providers Deep Tissue Chronic pain, tension $120-160/hr Highly-rated clinics (4.9/5 stars) Swedish Relaxation, stress relief $90-130/hr Wellness centers in Williamsburg Prenatal Pregnancy discomfort $160-220/hr Specialized prenatal centers (4.5/5 stars) Sports Athletic recovery $120-150/hr Park Slope wellness studios (4.5/5 stars) Myofascial Release Chronic pain, limited mobility $140-180/hr Specialized myofascial clinics Lymphatic Drainage Swelling, detox $130-170/hr Physical therapy centers Trigger Point Specific pain areas $120-160/hr Evolve Physical Therapy
Finding the right massage therapist in Brooklyn can transform your approach to self-care and pain management. Whether you're dealing with chronic back pain, recovering from a sports injury, or simply need to de-stress after a hectic work week, Brooklyn's diverse massage therapy scene has something for everyone.
The borough's massage offerings range from specialized clinical treatments at physical therapy practices to relaxing spa experiences with extended hours. Many Brooklyn massage centers provide customized sessions that combine multiple techniques to address your specific needs.
I'm Lou Ezrick, founder of Evolve Physical Therapy, with nearly two decades of experience in physical therapy and rehabilitation in Brooklyn, specializing in integrating massage therapy Brooklyn techniques with comprehensive treatment plans for lasting pain relief and improved mobility.
What to Expect on Your First Visit
If you're new to massage therapy Brooklyn, your first appointment will typically begin with a consultation. This is your opportunity to discuss your health history, current concerns, and treatment goals with your therapist. At Evolve Physical Therapy + Sports Rehabilitation, we take this initial conversation seriously, as it helps us create a personalized treatment plan.
You'll be asked to fill out an intake form covering your medical history, current medications, and specific areas of pain or discomfort. Don't hold back—the more your therapist knows, the better they can help you.
Once the consultation is complete, your therapist will leave the room so you can undress to your comfort level. Professional draping techniques ensure you're always covered appropriately, with only the area being worked on exposed. Standard sessions typically last 60, 75, or 90 minutes, though 30-minute targeted sessions are also available at many Brooklyn locations.
"During your first session, communication is key," explains one of our senior therapists at Evolve. "Don't hesitate to provide feedback about pressure, comfort, or areas that need special attention. This helps us tailor the experience to your specific needs."
Qualifications & Credentials to Look For
When seeking massage therapy Brooklyn services, it's important to verify proper credentials. In New York State, massage therapists must be licensed (LMT), which requires completing an accredited program (typically 500-1,000 hours) and passing the state board examination.
For massage provided within a physical therapy practice like ours at Evolve, look for board-certified physical therapists who have specialized training in soft tissue mobilization techniques. Many Brooklyn therapists also hold additional certifications in specialized modalities like prenatal massage, sports massage, or manual lymphatic drainage.
Increasingly important in today's healthcare landscape is trauma-informed training. Therapists with this additional education understand how to work with clients who have experienced physical or emotional trauma, creating a safe and supportive environment.
At Evolve Physical Therapy + Sports Rehabilitation, all our practitioners are fully licensed and certified, with ongoing continuing education to stay current with the latest techniques and approaches in both physical therapy and massage therapy.
Massage Therapy Brooklyn: Deep Tissue Mastery
When it comes to massage therapy Brooklyn, deep tissue work is often the go-to solution for those stubborn aches and pains that just won't quit. Picture this: you've been hunched over your laptop for weeks, and that knot between your shoulders has become your unwelcome companion. That's where deep tissue mastery comes in.
Unlike the gentle, flowing strokes of relaxation massage, deep tissue work means business. At Evolve Physical Therapy + Sports Rehabilitation, our therapists use deliberate pressure, focused forearm glides, and targeted techniques to reach those deeper muscle layers where tension likes to hide. We're essentially having a serious conversation with your muscles, telling those knots it's time to pack up and leave.
"I love watching clients' faces when they stand up after their first deep tissue session," says one of our senior therapists. "That look of surprise when they can turn their head fully for the first time in months? That's why we do this work."
The beauty of deep tissue massage isn't just in the immediate relief (though that certainly feels wonderful). The real magic happens as your body responds over the next few days – improved mobility, decreased pain, and a sense of lightness that makes everyday movements easier.
Want to dive deeper into the specifics of this technique? Check out our detailed guide to Deep Tissue Massage in Brooklyn. And if you're the type who appreciates scientific backing, this research on deep tissue benefits explains why it's more than just a feel-good treatment.
Who Benefits & Why
The list of people who can benefit from deep tissue work is surprisingly diverse. That office worker with the tech neck from endless Zoom meetings? Absolutely. The weekend warrior athlete whose hamstrings scream after Sunday's basketball game? Definitely. But it goes much deeper than that.
Deep tissue work is particularly valuable for those dealing with chronic pain conditions. By breaking up adhesions (those sticky spots between muscle layers) and releasing trigger points, we can help restore normal function to areas that have been compromised for months or even years.
Post-surgical recovery patients often find deep tissue techniques essential for addressing scar tissue. As one client recovering from shoulder surgery shared, "I was shocked at how much mobility I gained after just three sessions focusing on the scar tissue around my incision."
Deep tissue work isn't always comfortable in the moment – there's often that "hurts so good" sensation as we work through restricted areas. But our therapists at Evolve are experts at finding that sweet spot between therapeutic pressure and unnecessary pain. We're constantly checking in, reading your body's signals, and adjusting our approach.
What makes our approach to massage therapy Brooklyn unique is how we integrate deep tissue techniques with our physical therapy expertise. We're not just addressing symptoms – we're looking at movement patterns, posture, and daily habits that might be contributing to your discomfort. This comprehensive approach means longer-lasting results and fewer recurrences of those stubborn problems.
Whether you're dealing with chronic back pain, recovering from an injury, or simply want to move through your day with less discomfort, deep tissue massage might be the missing piece in your wellness puzzle. Your muscles have been working hard – isn't it time you gave them the attention they deserve?
Prenatal & Postpartum Bliss
Pregnancy transforms a woman's body in remarkable ways, and our massage therapy Brooklyn specialists have crafted techniques specifically for mothers-to-be and new moms. Think of prenatal massage as a sanctuary where expectant mothers find relief while nurturing their changing bodies.
At Evolve Physical Therapy + Sports Rehabilitation, we've designed our prenatal massage to address those all-too-common pregnancy discomforts – the nagging lower back pain, sciatic nerve flare-ups, swollen ankles, and that distinctive round ligament pain that can catch you by surprise. Our therapists use specially designed side-lying support systems and cushions that cradle your body safely while allowing for effective treatment.
"What many people don't realize is that prenatal massage goes well beyond physical relief," shares one of our prenatal specialists. "It helps balance those wild pregnancy hormones, calms anxiety, and can significantly improve sleep quality – something every expectant mom treasures."
The journey doesn't end with delivery. Our postpartum massage services help new mothers recover from childbirth's physical demands. We address those upper back and neck tensions that develop from hours of nursing or bottle-feeding, and support your body's gradual return to pre-pregnancy alignment.
Throughout Brooklyn, you'll find dedicated prenatal massage providers with stellar ratings (4.5+ stars from numerous reviews) through trauma-informed, evidence-based perinatal massage approaches. These specialized centers have become trusted havens for expectant mothers across the borough.
Safety & Positioning
When it comes to prenatal massage, safety isn't just important – it's everything. Our Evolve therapists receive specialized training in positioning techniques that accommodate your changing body:
During the first trimester, while some providers avoid massage altogether due to miscarriage concerns, we take a gentler approach with appropriate modifications based on your specific needs and medical history.
As you move into your second and third trimesters, we typically use side-lying positions with supportive cushioning that keeps pressure off your abdomen and major blood vessels – ensuring both comfort and safety.
In late pregnancy, we introduce additional modifications to accommodate increased discomfort and reduced mobility, always prioritizing your comfort.
Working with a certified prenatal massage therapist is essential. Our specialists understand pregnancy's physiological changes and know which techniques to avoid. For instance, we never apply deep pressure on the legs (due to increased blood clot risk) and carefully avoid certain acupressure points that might stimulate uterine contractions.
At Evolve, we ensure our prenatal clients receive care that's not just effective but completely safe for both mother and baby. We maintain open communication throughout your session and adjust our approach based on your comfort level and medical considerations. Our inclusive care approach welcomes all mothers-to-be, regardless of where you are in your pregnancy journey.
For more comprehensive information about our services, visit our More info about Massage Therapy Brooklyn page.
Sports Recovery Power
Brooklyn's runners, cyclists, CrossFitters, and weekend warriors have finded a powerful secret for better performance and faster recovery: sports massage. This specialized form of massage therapy Brooklyn goes beyond relaxation to address the unique demands active bodies face, whether you're training for the Brooklyn Half Marathon or just trying to keep up with your kickball league.
Unlike traditional massage, sports massage is strategically timed around your activity schedule. At Evolve Physical Therapy + Sports Rehabilitation, we customize each session based on whether you're preparing for competition, recovering from an intense workout, or maintaining peak condition between training sessions.
"The beauty of sports massage is how it adapts to your athletic calendar," explains our sports recovery specialist. "When scheduled before an event, we focus on warming tissues and optimizing blood flow. After competition, our techniques shift to clearing out those metabolic waste products that cause that dreaded day-after soreness."
Regular sports massage creates a powerful ripple effect throughout your training: your muscles recover faster between workouts, that stubborn post-exercise stiffness diminishes, and your range of motion improves noticeably. Many clients report their fascia—the connective tissue surrounding muscles—feels more hydrated and pliable, which translates to smoother movement patterns.
Even more impressive? Athletes who incorporate sports massage consistently tend to experience fewer overuse injuries and enjoy the mental relaxation benefits that come from dedicated recovery time.
Integrated Stretch + Massage Approach
At Evolve, we've developed a comprehensive approach that pairs targeted massage with specialized stretching techniques—a combination that delivers results traditional massage alone can't match.
Our therapists are experts in PNF stretching (that's Proprioceptive Neuromuscular Facilitation for the science-minded), a technique that involves gentle muscle contractions and relaxations to achieve deeper, more effective stretches. We complement this with cutting-edge tools like professional-grade percussive devices that deliver rapid pulses deep into muscle tissue, breaking up adhesions and improving circulation.
For athletes dealing with inflammation, we often incorporate contrast therapy, alternating heat and cold applications to reduce swelling and speed recovery. This integrated approach proves particularly effective for addressing sport-specific problems like the notorious IT band syndrome in runners or the shoulder impingement patterns common in overhead athletes.
"What makes our approach different is that we're not just working on relaxing muscles—we're reprogramming movement patterns," says our lead therapist. "When an athlete leaves our table, they're not just feeling better; they're moving better."
Evidence-Based Performance Boost
The benefits of sports massage aren't just anecdotal—they're backed by solid research. Studies published in the Journal of Athletic Training have demonstrated significant reductions in perceived pain and improved muscle function following exercise-induced muscle damage when sports massage is applied.
Additional research in the Journal of Strength and Conditioning Research found that post-exercise massage improved blood flow and reduced muscle fatigue compared to passive recovery methods, translating to better performance in subsequent training sessions.
At Evolve, we're committed to evidence-based practices, continuously updating our protocols based on the latest sports medicine research. This science-driven approach is why so many Brooklyn athletes—from professional competitors to dedicated amateurs—trust us with their recovery and performance needs.
Our physical therapists and massage therapists collaborate closely to create comprehensive treatment plans that address both immediate recovery needs and long-term performance goals. Whether you're looking to shave minutes off your marathon time or simply want to enjoy your weekend activities without Monday morning pain, our sports recovery massage services deliver results you can feel.
Lymphatic Drainage Detox
Ever noticed how some areas of your body just seem puffy or swollen, even when you're doing everything right? That's where lymphatic drainage massage comes in—one of the most gentle yet surprisingly effective forms of massage therapy Brooklyn practitioners offer.
Unlike the deep pressure you might expect from a typical massage, lymphatic drainage uses feather-light, rhythmic strokes that follow your body's natural lymphatic pathways. The touch is so gentle you might wonder if anything's happening at all—but don't be fooled by its subtlety!
"The magic of lymphatic drainage is in its gentleness," explains our lymphatic specialist at Evolve. "We're not forcefully pushing fluid around—we're creating subtle pressure differentials that encourage your lymph system to do what it naturally wants to do, just more efficiently."
Your lymphatic system works as your body's natural detoxification highway, but sometimes it needs a little help, especially after surgery, injury, or when you're feeling under the weather. The light, rhythmic strokes help move excess fluid, reduce swelling, and support your immune function.
At Evolve Physical Therapy + Sports Rehabilitation, our clients see remarkable benefits from lymphatic sessions, including:
Reduced post-surgical swelling that won't seem to go away on its own Relief from chronic sinus pressure and congestion Decreased puffiness around the face and eyes Improved immune function during cold and flu season Support for general detoxification and wellness
Most sessions last 60-90 minutes, and while you won't feel the muscle soreness associated with deeper work, you might notice increased trips to the bathroom afterward (that's the excess fluid leaving your system!) and a surprising level of relaxation.
Medical vs. Spa Lymphatic Sessions
It's worth understanding that not all lymphatic drainage services are created equal. Here in Brooklyn, you'll find two main approaches:
Medical lymphatic drainage is typically performed by specially certified physical therapists or massage therapists with advanced training. This clinical approach is essential for people dealing with specific medical conditions like post-mastectomy lymphedema, severe post-surgical swelling, or chronic venous insufficiency.
At Evolve, our physical therapists offer this medical-grade lymphatic work, sometimes incorporating compression bandaging as part of a complete decongestive therapy protocol. This comprehensive approach is particularly valuable for oncology patients or those recovering from major surgeries.
Spa-based lymphatic treatments focus more on general wellness and temporary cosmetic improvements. While less medically intensive, these can still offer wonderful benefits for reducing facial puffiness, improving the appearance of cellulite, addressing water retention, and promoting relaxation.
"Many clients start with a spa lymphatic treatment for general wellness, then seek out medical lymphatic drainage when they're dealing with a specific health concern," notes our lymphatic specialist. "Both have their place in a comprehensive wellness routine."
Brooklyn offers excellent options for both approaches. For serious medical conditions like lymphedema, specialized physical therapy centers provide medical lymphatic drainage. Meanwhile, several day spas throughout the borough offer gentler lymphatic facial massages and body treatments focused on cosmetic improvements and general wellness.
Curious to learn more about how lymphatic drainage might help with your specific concerns? Check out our detailed guide to lymphatic drainage massage in Brooklyn for a deeper dive into this fascinating and beneficial therapy.
Myofascial Release Freedom
If you've ever felt "stuck" in your body, like your muscles just won't let go no matter how much you stretch, myofascial release might be your ticket to freedom. This powerful approach has become one of the most sought-after techniques in massage therapy Brooklyn clinics offer, and for good reason.
Myofascial release focuses on something most of us have never heard of but affects everything we do: fascia. This remarkable connective tissue wraps around every muscle, bone, nerve, and organ in your body like an intricate spider web. When healthy, fascia glides and moves with ease. But injuries, stress, inflammation, and even poor posture can cause it to become tight, sticky, and restricted—creating a domino effect of pain and limited movement throughout your body.
"I often explain fascia to my clients using the orange analogy," says our senior therapist at Evolve. "Imagine the thin white membrane that surrounds each orange segment. That's similar to how fascia surrounds your muscles and organs. When that membrane gets tight or twisted in one area, it pulls on everything connected to it."
This whole-body perspective makes myofascial release uniquely effective for conditions that haven't responded to other treatments. At specialized myofascial clinics in Brooklyn, therapists have helped thousands of patients find relief from persistent pain. Many people find that the source of their pain isn't actually where they feel it—it's a fascial restriction pulling from somewhere else entirely.
Myofascial release can be transformative for people dealing with:
Chronic back and neck pain that persists despite other treatments Headaches and jaw tension related to TMJ dysfunction Post-surgical scarring that limits movement and causes discomfort Sports injuries that haven't fully healed with traditional approaches General stiffness that makes you feel older than your years
Beyond just pain relief, clients often report feeling "lighter," more balanced, and more connected to their bodies after sessions. Many describe a sense of release that goes beyond physical—as if emotional tension stored in the tissues has also been set free.
Tools & Techniques
What makes myofascial release different from regular massage? For starters, there's the time factor. While Swedish massage typically uses rhythmic strokes, myofascial work involves sustained pressure held for 3-5 minutes on restricted areas. This gentle but firm pressure gives the fascia time to soften and release naturally, rather than forcing change.
"We're not trying to muscle through restrictions," explains our therapist at Evolve. "We're creating the right conditions and giving the body time to let go on its own terms. It's like slowly melting ice rather than trying to crack it."
Therapists skilled in myofascial release use a variety of approaches. Some use skin rolling techniques, gently lifting and rolling the skin to free up superficial fascial layers. Others employ Instrument Assisted Soft Tissue Mobilization (IASTM), using specialized tools made of materials like stainless steel or jade to detect and treat fascial restrictions with precision.
The benefits don't stop when you leave the clinic. At Evolve, we teach clients foam rolling and self-myofascial release techniques they can use at home to maintain progress between sessions. These simple but effective tools help you become an active participant in your healing process.
Sessions typically last 60-90 minutes and may leave you feeling taller, more open, and more integrated in your movement. While you might experience some tenderness during treatment (we call this "good hurt"), the results are worth it—improved flexibility, reduced pain, and a greater sense of freedom in your body.
For more detailed information about our approach to myofascial release, visit our Myofascial Release Brooklyn page.
Trigger Point & Dry Needling Precision
When you're dealing with persistent pain that just won't quit, trigger point therapy might be exactly what you need. This targeted approach to massage therapy Brooklyn zeros in on those stubborn knots in your muscles that can cause both local pain and referred pain elsewhere in your body.
Think of trigger points as tiny troublemakers within your muscles – tight bands or knots that become hypersensitive. Press on one, and you might feel pain shoot to a completely different area of your body in predictable patterns. That knot in your upper trapezius? It could be the culprit behind your persistent headaches. The tight spot in your glutes? It might be mimicking sciatica symptoms.
At Evolve Physical Therapy + Sports Rehabilitation, we approach trigger point therapy like detectives solving a mystery. Our specialists carefully map your pain patterns, feeling for characteristic tissue changes, and systematically release the points that reproduce your symptoms.
"Understanding the difference between active and latent trigger points helps us target treatment more effectively," explains our lead therapist. Active trigger points cause constant pain and can produce surprising symptoms like goosebumps or watering eyes even when not being touched. Meanwhile, latent trigger points only hurt when pressed directly but still silently limit your movement and weaken muscles.
This specialized therapy works wonders for tension headaches, jaw pain, shoulder and neck issues, lower back discomfort, tennis elbow, knee pain, and even plantar fasciitis. Many of our Brooklyn clients walk out feeling immediate relief, though lasting results typically require multiple sessions to fully resolve the underlying issues.
What Happens During a Session
Your trigger point session at Evolve begins with a thorough assessment to locate those problematic spots. Your therapist will carefully palpate your muscles, feeling for tight bands and tender areas while asking for your feedback about pain and any referred sensations you might experience.
The treatment itself may include several approaches. Manual compression is the cornerstone technique, where we apply sustained pressure directly to trigger points using fingers, thumbs, or elbows. We typically hold this pressure for 30-90 seconds until we feel the tissue release.
For more stubborn trigger points, dry needling might be recommended. This technique, performed by our specially trained physical therapists, involves inserting thin filiform needles directly into trigger points. When the needle hits the spot just right, you might feel a brief "twitch response" – a momentary contraction that signals we've found the trigger point. While this might cause a second of discomfort, it's often followed by immediate muscle relaxation.
We may also incorporate spray and stretch techniques, using a cooling spray followed by gentle stretching to deactivate trigger points, or reciprocal inhibition, which leverages the neurological principle that when one muscle contracts, its opposite relaxes.
Unlike full-body massage sessions, trigger point therapy typically lasts 30-60 minutes and focuses specifically on your most problematic areas. It's targeted, efficient, and designed to give you the most relief in the least amount of time.
After-Care & Prevention
Don't be surprised if you feel a bit sore for a day or two after your trigger point therapy – it's completely normal and similar to how you might feel after a good workout. This temporary soreness is actually part of the healing process as your tissues recover from treatment.
To maximize your results, we'll send you home with specific after-care instructions:
Hydration is absolutely essential after treatment. Drinking plenty of water helps flush out the metabolic waste that gets released from trigger points during therapy. We recommend carrying a water bottle with you for the next 24 hours.
Apply heat for 15-20 minutes several times throughout the day to help maintain muscle relaxation. A warm shower, heating pad, or microwavable heat pack all work well.
Incorporate gentle stretching of the treated muscles to prevent them from tightening up again. We'll show you exactly which stretches will benefit you most based on your specific trigger points.
Pay attention to your posture and ergonomics since poor positioning is often what created those trigger points in the first place. Small adjustments to your workstation, driving position, or sleeping arrangement can make a huge difference.
Learn self-treatment techniques to maintain results between sessions. We might recommend tools like tennis balls or foam rollers to help you address trigger points at home.
"The key to lasting relief isn't just treating trigger points but preventing them from coming back," our specialist emphasizes. "We work closely with clients to identify and modify the activities, postures, and movement patterns that contribute to trigger point formation."
Many of our Brooklyn clients find that scheduling monthly maintenance sessions becomes an essential part of their wellness routine, preventing the return of problematic trigger points and keeping pain at bay. As with many things in health, consistency is key to long-term success.
For more information about our comprehensive approach to massage therapy Brooklyn and physical therapy services, check out our detailed service page.
Holistic Spa Serenity
While Brooklyn offers plenty of medically-focused treatments, sometimes what your body truly craves is pure, blissful relaxation. The borough's spa-based massage therapy Brooklyn experiences provide the perfect counterbalance to our city life, focusing on total-body serenity rather than targeting specific pain points.
Many wellness centers in Williamsburg embody this philosophy beautifully. With extended hours seven days a week, these establishments have made professional relaxation accessible to even the busiest Brooklynites. Their core belief that "self-care is a lifestyle, not a luxury" resonates deeply with locals who understand that regular relaxation isn't indulgent—it's essential.
At the heart of most spa experiences is the classic Swedish massage. This traditional technique uses those long, flowing strokes that feel like heaven on tired muscles. Your therapist will incorporate gentle kneading and circular movements that improve circulation while melting away tension. Unlike deep tissue work, Swedish massage keeps things lighter, perfect for when you need mental decompression as much as physical relief.
"Swedish massage is like pressing the reset button for your nervous system," explains one of our Evolve therapists. "It's not just about the physical benefits—it's about giving your mind permission to completely let go."
Brooklyn spas often improve the basic Swedish experience with sensory elements that deepen your relaxation journey. Hot stone therapy places smooth, warmed basalt stones strategically along your body, allowing heat to penetrate muscle tissue before your therapist even begins hands-on work. The result? Deeper relaxation with gentler pressure.
Many clients at Evolve tell us they particularly love aromatherapy additions to their massages. Whether it's calming lavender to quiet an anxious mind or invigorating eucalyptus to clear congested sinuses, essential oils engage your sense of smell to improve therapeutic benefits. Some Brooklyn spas complete the sensory experience with sound therapy—think gentle singing bowls or carefully curated playlists that help quiet mental chatter.
At Evolve Physical Therapy + Sports Rehabilitation, we understand that healing happens best when both body and mind are addressed. That's why we often incorporate relaxation elements even into our more clinically-focused sessions. That mind-body connection isn't just wellness jargon—it's a powerful healing tool.
Building an Affordable Self-Care Routine
Let's be real—regular massage offers tremendous benefits, but Brooklyn prices can make consistent care seem out of reach. Thankfully, there are smart ways to make this essential self-care more budget-friendly.
Membership plans have revolutionized how many Brooklynites approach massage. Many wellness centers in Park Slope and surrounding neighborhoods offer monthly programs that significantly reduce per-session costs. You'll typically get one monthly massage at a reduced rate, plus member pricing on additional sessions.
Package bundles make perfect sense if you know you'll be coming back. Most Brooklyn massage establishments offer 10-20% savings when you purchase multiple sessions upfront. At Evolve, we've created package options specifically designed to make regular therapeutic massage more accessible to those who need ongoing care.
Gift cards aren't just for giving—they're also perfect for receiving! Don't be shy about suggesting massage gift certificates when friends and family ask what you'd like for special occasions. Many of Brooklyn's pioneering massage wellness centers have built substantial businesses around people sharing the gift of massage with loved ones.
For those with Health Savings Accounts (HSA) or Flexible Spending Accounts (FSA), there's excellent news. When massage is deemed medically necessary and prescribed by a healthcare provider, you can often use these pre-tax dollars to cover sessions. Our team at Evolve is happy to provide appropriate documentation for clients looking to use these funds.
Service Type Average 60-Min Price Monthly Membership Price Package Discount (6+ sessions) Swedish Relaxation $110-150 $85-95 15-20% off Hot Stone $140-180 $110-130 10-15% off Aromatherapy Add-On $15-25 $10-15 Often included free Couples Massage $220-280 $190-230 10-15% off
"The magic happens with consistency," shares our wellness coordinator. "Even monthly sessions create noticeable differences in how people move through their lives—physically and emotionally."
Many of our Brooklyn clients find their ideal self-care routine combines targeted clinical massage for specific issues with regular relaxation-focused sessions for maintenance. This balanced approach addresses both immediate physical concerns and long-term stress management, creating a sustainable wellness practice that supports your busy Brooklyn lifestyle.
Frequently Asked Questions About Massage Therapy Brooklyn
How much does massage therapy Brooklyn typically cost?
When exploring massage therapy Brooklyn options, one of the first questions on most people's minds is about cost. Brooklyn offers a wide range of pricing depending on what you're looking for.
Specialized treatments naturally come with a higher price tag. If you're seeking prenatal massage, lymphatic drainage, or medical massage, expect to pay premium rates compared to a standard Swedish massage. Session length plays a big role too—standard sessions typically run from 60 minutes ($90-160) to more indulgent 90-minute sessions ($130-220).
Where you receive your massage matters just as much. Hospital-based or clinical settings often charge more than your neighborhood day spa or standalone studio. And just like in any profession, experience commands a premium—therapists with years of specialized training and certifications typically charge more for their expertise.
From my years working with clients across Brooklyn, I've observed these general price ranges:
Basic relaxation massage will set you back about $90-130 for an hour of blissful Swedish techniques. If you're dealing with deeper issues, deep tissue or sports massage typically ranges from $120-160 for the same time. Expectant mothers should budget $160-220 for prenatal massage sessions, while specialized treatments like lymphatic drainage or myofascial release generally fall between $130-180.
Good news for first-timers—many Brooklyn massage providers offer special introductory rates. For example, many wellness centers in Williamsburg welcome new clients with 60-minute sessions at competitive rates, whether you choose Swedish massage, deep tissue, or facial services.
At Evolve Physical Therapy + Sports Rehabilitation, we understand budget concerns. That's why we work with clients to determine if their insurance might partially cover massage therapy when it's part of a physical therapy treatment plan. Our team is always happy to help steer those sometimes confusing coverage options.
How do I choose the right clinic for massage therapy Brooklyn?
Finding your perfect massage therapy Brooklyn match doesn't have to feel overwhelming. Think of it as dating—you're looking for the right fit for your specific needs and preferences.
Start by checking reputation and reviews. In our digital age, this is easier than ever—look for practices with strong Google ratings that suggest consistent quality care. Many physical therapy clinics in Brooklyn maintain impressive ratings based on hundreds of client reviews, which speaks volumes about their service quality.
Consider specialization next. Are you pregnant? Look for a specialized practice that offers custom prenatal care addressing the unique challenges of pregnancy. Struggling with chronic pain? Seek out clinics with experience helping patients with limited mobility find relief.
Credentials matter tremendously in massage therapy. Always verify that your therapist holds a valid New York State massage therapy license (LMT). If you're seeking specialized services like prenatal massage or lymphatic drainage, ask about specific training in those areas.
Think about the atmosphere that helps you relax. Some people prefer a clinical setting focused on therapeutic outcomes, while others want the dim lighting and soft music of a spa-like environment. There's no wrong answer—just what works best for you.
Practical considerations like location, hours, and booking policies can make or break your massage routine. Many wellness centers in Williamsburg, for example, offer extended hours seven days a week, making it easier to fit massage into even the busiest Brooklyn schedule.
Pay attention to communication style during your initial contact. Does the practice listen carefully to your concerns? Do they clearly explain their approach? This early interaction often reveals how you'll be treated throughout your care.
At Evolve Physical Therapy + Sports Rehabilitation, we always encourage potential clients to call with questions before booking. This helps ensure we're truly the right fit for your specific needs—because massage therapy works best when there's a good match between client and provider.
Can massage therapy be combined with other treatments?
Absolutely! In fact, massage therapy Brooklyn often delivers its most powerful results when combined with other treatments. Think of massage as part of your wellness orchestra rather than a solo performer.
At Evolve Physical Therapy + Sports Rehabilitation, we regularly integrate massage with other approaches for improved outcomes. Our physical therapists often refer to massage as "soft tissue mobilization" and strategically incorporate it into broader treatment plans. This prep work helps relax tight tissues before joint mobilization and therapeutic exercise, making these interventions significantly more effective.
Many Brooklyn wellness centers offer both massage and acupuncture—a powerful combination that works through different body systems. Massage relaxes muscles before acupuncture, creating ideal conditions for effective needle placement. The two modalities complement each other beautifully, often delivering results neither could achieve alone.
For the fitness enthusiasts among us, massage between strength training sessions can be transformative. It improves recovery times, reduces soreness, and maintains tissue quality—a particular benefit for athletes and regular gym-goers who put significant demands on their bodies.
Those dealing with stress and anxiety often find remarkable relief when combining massage with mindfulness practices, yoga, or counseling. This comprehensive approach addresses both physical tension and its mental/emotional components.
The science backs up this integrated approach. A notable study published in the Annals of Internal Medicine found that massage therapy combined with standard medical care produced better outcomes for low back pain than standard care alone.
"We consistently see the best outcomes when massage is part of a comprehensive plan," our clinical director often tells new clients. "The hands-on work of massage complements the active engagement of exercise and the structural approach of joint mobilization."
At Evolve, our collaborative team works together to create treatment plans that leverage multiple approaches, maximizing your results and getting you back to the activities you love more quickly.
Conclusion
Massage therapy Brooklyn has truly evolved into a diverse wellness landscape, offering something for everyone—whether you're nursing a nagging sports injury, easing pregnancy discomfort, or simply needing a mental reset from Brooklyn's non-stop pace. The seven specialized services we've explored throughout this guide represent just how sophisticated and varied massage therapy has become in our borough.
What makes Brooklyn's massage scene so special isn't just the variety of techniques available, but the passionate practitioners behind them. From clinical therapists with advanced medical training to intuitive healers who seem to find tension you didn't even know you had, Brooklyn's massage community reflects the borough itself—diverse, skilled, and always evolving.
At Evolve Physical Therapy + Sports Rehabilitation, we take pride in being part of this vibrant wellness ecosystem. Our approach integrates these various massage techniques into comprehensive care plans that address not just your immediate pain points, but the underlying patterns that created them in the first place. We believe that hands-on care creates a foundation for lasting change in how your body moves and feels.
The beauty of massage therapy Brooklyn is that it can be whatever you need it to be—an occasional luxury when stress peaks, a regular part of your athletic training regimen, or a crucial component of recovering from injury or surgery. Many of our clients begin with a specific issue and find that regular massage becomes an essential part of how they care for themselves.
We often tell our clients that your body carries your life story—the sports you played as a kid, the way you sit at work, the stress you hold in your shoulders. Massage therapy gives you a chance to rewrite some of those patterns and create new possibilities for how you move through the world.
Ready to find which massage approach might be right for you? We'd love to help you steer the options. Visit our Massage Therapy Brooklyn services page to learn more about our specific offerings and how they might fit into your wellness journey. Your path to feeling better doesn't have to be walked alone—we're here to support every step.
Senior Balance Boost: Exercises to Keep You Upright
Why Balance Training Matters for Seniors
Balance training for seniors is a series of specialized exercises designed to improve stability, prevent falls, and maintain independence as we age. Here's what you need to know:
Quick Guide to Balance Training for Seniors
Recommended frequency: 3 sessions per week, 45+ minutes each Basic exercises: Weight shifts, single-leg stands, heel-to-toe walking Safety first: Always have a chair or wall nearby for support Start with: 5-10 repetitions of each exercise, gradually increasing Medical clearance: Check with your doctor before beginning
Falls are the number-one cause of injuries among older Americans, with an older adult falling every single second in the United States according to the CDC. What's encouraging is that a 2016 study found that older adults who performed balance exercises for just 6 weeks significantly improved their stability and confidence.
The good news? Much of the balance decline we experience isn't inevitable—it's often due to inactivity and can be reversed with proper training.
Balance naturally deteriorates as we age due to:
Weakening muscle strength
Changes in vision and inner ear function
Reduced joint flexibility
Slower reaction times
Medication side effects
Starting a consistent balance routine can dramatically reduce your fall risk while improving your overall quality of life.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience specializing in balance training for seniors at Evolve Physical Therapy, where I've helped thousands of older adults regain their stability and confidence through evidence-based balance programs.
Why Balance Training Matters After 60
That moment when you suddenly wobble while reaching for something on a high shelf—it's more than just a fleeting scare as we age. It's a warning sign our bodies are changing.
According to the CDC, more than one in four older adults falls each year, yet fewer than half mention it to their doctor. Even more alarming, falls have become the leading cause of injury-related deaths among adults 65 and older.
"I used to think falls were just part of getting older," shares Margaret, a 72-year-old who visits our Brooklyn facility. "After working with the team at Evolve, I realized most falls can actually be prevented with the right exercises and awareness."
Several natural changes make balance training for seniors so crucial:
Sensory Loss affects how we perceive our surroundings. Vision changes, hearing problems, and decreased foot sensitivity all make it harder to steer even familiar spaces safely.
Muscle Weakness happens gradually but significantly. After 30, we naturally lose 3-5% of muscle mass each decade—a process that speeds up after 60. This means less strength to catch ourselves when we stumble.
Medical Conditions common in older adults often impact balance. High blood pressure affects over 63% of adults over 60 and can cause lightheadedness. About 25% of seniors have Type 2 diabetes, which often leads to peripheral neuropathy—that troublesome numbness in feet and hands that makes it hard to feel the ground properly.
Perhaps most concerning is the Fear of Falling cycle that develops. After one fall or near-miss, many seniors begin limiting their activities out of fear, which leads to further deconditioning and muscle weakness—ironically increasing their fall risk even more.
The good news? Research from 2019 shows that regular balance exercises not only reduce fall risk but also improve overall quality of life and cognitive function. Systematic reviews suggest properly designed balance programs may reduce fall rates by an impressive 46%-48%.
For more information on fall statistics and prevention strategies, see the CDC's comprehensive guide on older adult falls.
Main Causes of Balance Problems in Older Adults
Understanding what's behind unsteadiness helps us address it more effectively:
Your vision changes significantly with age. Depth perception weakens, peripheral vision narrows, and adapting to different lighting becomes harder. Since vision provides about 70% of the sensory input we use for balance, these changes dramatically impact stability.
Your vestibular system—that complex network in your inner ear—gradually loses sensitivity. By age 70, we've typically lost about 40% of the hair cells in this system that help detect movement and position.
"Many clients don't realize their dizziness when turning or looking up relates to age-related vestibular changes," explains Dr. Sarah Chen, one of our physical therapists at Evolve. "Specific exercises can help compensate for these natural losses."
Joint degeneration and arthritis affect proprioception—your body's ability to sense its position without looking. When joints become stiff or painful, they send less accurate information to your brain about where your body is in space.
Medication side effects often include dizziness or lightheadedness. At Evolve, we frequently coordinate with our clients' physicians to review medications that might be contributing to balance problems.
Top Benefits of Consistent Balance Work
Committing to regular balance training for seniors creates remarkable improvements:
Reduced Fall Risk is the most immediate benefit. Studies consistently show that proper balance training can decrease fall likelihood by up to 40%—a life-changing improvement.
Faster Reaction Time develops as you practice. Your body learns to respond more quickly to unexpected movements or position changes, helping you catch yourself before a fall happens.
Stronger Legs and Core naturally develop through balance exercises. These key muscle groups provide the foundation for stability in all daily activities, from walking to reaching to climbing stairs.
Sharper Cognition is an often-overlooked benefit. Research indicates that balance training activates multiple brain regions simultaneously, potentially improving memory and decision-making.
Mood Boost comes from regained confidence. When you feel steady on your feet, you're more likely to participate in social activities and maintain independence—both crucial for mental health.
Robert, a 78-year-old client, recently told us: "After six weeks of balance training at Evolve, I went from being afraid to walk to the corner store to confidently taking my grandchildren to the park. The improvement in my quality of life has been remarkable."
With scientific research on fall prevention continuing to show the effectiveness of targeted balance programs, there's never been a better time to focus on staying steady on your feet.
Balance Training for Seniors: How Often and How Safe?
Finding the sweet spot for balance training for seniors comes down to consistency, not intensity. According to guidelines from the American College of Sports Medicine (ACSM) and the National Institute on Aging, aim for:
Balance sessions 2-3 times weekly, though 3 or more days gives optimal results. Each session should last about 45 minutes, and you'll want to stick with your program for at least 8 weeks to see meaningful improvements.
At Evolve Physical Therapy, we've found something interesting with our Brooklyn clients – adding quick daily "balance snacks" of just 5-10 minutes between longer formal sessions helps people progress noticeably faster.
"Think of balance training like brushing your teeth," says Maria, one of our physical therapists. "A little bit every day creates the habit your body needs to rebuild those stability pathways."
Your balance workout should flow through three phases:
Start with a 5-7 minute warm-up – gentle marching in place, ankle circles, and shoulder rolls wake up your muscles and prepare your joints. Then move into your main balance exercises for 30-35 minutes, mixing both static holds and movement-based exercises. Finally, finish with a 5-minute cool-down of gentle stretching and deep breathing to bring your heart rate back to normal.
What you wear on your feet matters tremendously for safety. Skip the slippers and opt for shoes with non-slip soles and low, wide heels. Make sure they fit properly – not too loose where they might slip off, not too tight where they pinch. Good arch and ankle support are also essential for stable footing.
Setting up your home practice space properly prevents accidents:
Clear away clutter and cords from your exercise area. Ensure you have bright, even lighting so you can clearly see your surroundings. Always keep a sturdy chair or counter within arm's reach for support if needed. Have your phone nearby in case of emergency, and remember to sip water before, during, and after your exercises to stay hydrated.
While balance training is generally very safe, be alert to warning signs that tell you to stop: severe dizziness or spinning sensations, chest pain or pressure, unusual shortness of breath, sudden headache, or nausea with cold sweats. If you experience any of these, stop immediately and consult your doctor.
Precautions Before You Start
Safety first is our motto at Evolve when it comes to balance training for seniors. Before jumping in, take these important precautions:
Get medical clearance, especially if you have a history of falls, high blood pressure, heart conditions, severe osteoporosis, neurological conditions like Parkinson's, or you've recently had surgery or joint replacement. Your doctor knows your specific health situation and can offer personalized guidance.
Check your blood pressure before exercising, particularly if you take medications that might cause dizziness. Many of our clients keep a simple log of their pre-exercise readings to track patterns.
Do a quick dizziness check each time: stand up slowly from sitting and notice if you feel lightheaded. If you do, we'll modify your exercises to keep you safe.
"One of the biggest mistakes I see is people rushing into advanced balance exercises before they're ready," notes Alex, our physical therapist at the Marine Park location. "Balance training isn't a race – it's about building a solid foundation first."
Take a critical look at your home environment. We often help clients spot hidden hazards like loose rugs, poor lighting on stairs, missing grab bars in bathrooms, cluttered walkways, or electrical cords crossing walking paths. Simple fixes can prevent accidents before they happen.
If you use a cane or walker, don't set it aside for your balance exercises. Instead, we'll show you how to safely incorporate it into your routine. As your balance improves, we can gradually reduce your dependence on these devices – but always at a pace that prioritizes your safety.
Equipment & Support You May Need
The beauty of balance training for seniors is its simplicity. You don't need fancy equipment or an expensive gym membership to get started. Here's what we recommend to our Brooklyn clients:
A sturdy chair becomes your best friend when starting balance work. Choose one without wheels, preferably with armrests if you're a beginner. Make sure it's heavy enough that it won't slide when you hold it for support. The dining room chairs in most homes work perfectly.
Your kitchen countertop or a solid wall provides excellent support for standing exercises. At our Park Slope facility, we start many clients along our therapy room walls before progressing to more challenging environments.
A non-slip yoga mat creates a defined space for your practice while providing cushioning for floor exercises. The slight padding also helps reduce impact on your joints.
Light resistance bands add challenge to many balance exercises while strengthening supporting muscles. They're inexpensive, portable, and incredibly versatile.
Once you've mastered the basics, a balance pad (a specialized foam cushion) creates an unstable surface that challenges your balance systems in new ways.
"My client Dorothy started with just a kitchen chair and her hallway wall," shares Lou from our clinical team. "Six months later, she's confidently using a balance pad while doing light hand weights. The progression has been remarkable, and it all started with the simplest equipment."
Other helpful items include a stopwatch to track how long you can hold positions, a full-length mirror to check your posture, and some athletic tape to create floor markers for stepping exercises.
When it comes to physical therapy for balance disorders, starting simply is the key to long-term success. As your confidence grows, we can gradually introduce new challenges to keep improving your stability and independence.
6 Essential Balance Exercises You Can Do Today
Ready to start your balance training for seniors journey? These six exercises form the cornerstone of what we recommend to our clients at Evolve. Each one targets different aspects of balance and stability that naturally decline with age.
The beauty of these exercises is their simplicity—you can begin today with minimal equipment and still see meaningful results. Our physical therapists have carefully selected this sequence based on both scientific research and years of clinical experience.
Aim to practice these exercises three times weekly, gradually building your confidence and capability before progressing to more challenging variations.
Weight Shifts
Think of weight shifts as the foundation of all balance work. This exercise teaches your body to control its center of gravity—exactly what you need to prevent falls in everyday life.
How to perform:
Stand with feet hip-width apart near a counter or sturdy chair for support
Shift your weight onto your right foot, gently lifting your left foot slightly off the floor
Hold this position for 30 seconds, focusing on stability
Return to center, then repeat on the left side
Complete 6 repetitions on each side
"Most of my clients are surprised by how challenging simple weight shifts can be," says Dr. Rachel Kim from our Midwood facility. "This exercise teaches your body to make those tiny adjustments that prevent falls during daily activities like reaching for something in the kitchen."
For best results, keep your core engaged and your posture tall. Fix your gaze on something that doesn't move, and remember to breathe normally throughout. Once you've mastered the basic version, try it without holding onto support, or challenge yourself further by standing on a folded towel to create an unstable surface.
Heel-to-Toe Walk
Remember the childhood game of walking on an imaginary tightrope? The heel-to-toe walk brings that concept into your balance training routine. This exercise improves dynamic balance while walking—essential for navigating narrow spaces like crowded restaurants or busy sidewalks.
How to perform:
Stand near a wall or in a hallway where you can reach for support if needed
Place the heel of your right foot directly in front of the toes of your left foot
Focus on a point in front of you at eye level
Take 10 steps forward in this heel-to-toe pattern, moving deliberately
Turn around carefully and repeat in the other direction
Doris, one of our 83-year-old clients, shared her experience: "The heel-to-toe walk was frustrating at first—I could barely take three steps without losing my balance. After practicing for a month, I can now do 20 steps without touching the wall. It's given me so much more confidence when walking in crowded places."
As you practice, keep your posture tall with shoulders relaxed. This isn't a race—slow, controlled movements build better balance. When you're ready for more challenge, try crossing your arms over your chest or counting backward from 100 by 7s while walking.
Single-Leg Stand
Standing on one leg might seem simple, but it's a powerful exercise that strengthens ankle, knee, and hip stabilizers while challenging your balance system. It's particularly valuable because it mimics real-life situations like stepping into a bathtub or walking up stairs.
How to perform:
Stand behind a sturdy chair or counter, holding lightly for support
Shift your weight to your right foot
Slowly lift your left foot off the floor, bending the knee
Hold for 10 seconds, then lower your foot
Repeat on the opposite side
Complete 3 repetitions on each leg
"The single-leg stand is often where we see the most dramatic improvements," notes Dr. James Wilson from our Gravesend location. "When clients first start, they might need to grip the chair tightly for just a few seconds. Within weeks, many can balance hands-free for 30 seconds or more."
Focus your gaze on a non-moving object and keep your standing knee slightly bent, not locked. As you progress, try increasing your hold time to 30 seconds or attempting a "tree pose" variation by placing the sole of your foot on the opposite inner calf.
For our more advanced clients, we often turn this into a dual-task challenge: "How long can you stand on one leg while naming as many states as possible?" This approach improves both balance and cognitive function simultaneously—a powerful combination for fall prevention.
For more information about how physical therapy can help prevent falls, visit our physical therapy for fall prevention page.
Sit-to-Stand
This functional exercise targets one of the most dangerous moments in daily life—the transition between sitting and standing, when many falls occur. Beyond improving balance, sit-to-stands strengthen the quadriceps and gluteal muscles essential for mobility and independence.
How to perform:
Sit in a sturdy chair with feet flat on the floor, hip-width apart
Scoot forward until you're sitting near the edge of the chair
Lean slightly forward from the hips (this momentum helps with standing)
Push through your heels to stand up slowly
Pause in the standing position, ensuring you're stable
Slowly lower yourself back to sitting
Complete 10 repetitions
"Sit-to-stand is perhaps the most functional balance exercise we teach," says Maria Lopez, DPT at our Mill Basin location. "We all need to get up from chairs dozens of times daily. Strengthening this movement pattern prevents a significant percentage of falls in older adults."
If you find this exercise challenging, it's fine to use your hands at first. As you get stronger, try hovering your hands near the armrests without actually touching them. For an added challenge, hold the standing position for 5 seconds before sitting, or add a biceps curl with light weights once standing.
Side Steps & Grapevine
While we spend plenty of time walking forward, lateral (side-to-side) movement often gets neglected. Yet sideways stability is crucial for preventing falls when turning or stepping to the side—like getting in and out of the shower or navigating around furniture.
How to perform:
Stand with feet together, holding onto a counter if needed
Step to the right with your right foot
Bring your left foot to meet the right
Take 10 steps to the right, then 10 steps to the left
For the grapevine variation: Step right with your right foot, then cross your left foot behind your right, then step right again, then cross your left foot in front
"Lateral stability is often the first to decline with age," explains Dr. Michael Chang at our Brooklyn location. "Yet it's essential for navigating crowded spaces or stepping around obstacles. The side step and grapevine exercises specifically target this crucial movement pattern."
Research from the American Heart Association supports the effectiveness of lateral walking exercises for improving hip strength and overall balance in seniors. For more information, check out the American Heart Association's guide on balance exercises.
As you become more confident, try adding a resistance band loop around your thighs just above the knees for an extra challenge to your hip muscles.
Chair Tai Chi/Yoga Flow
This gentle flowing sequence brings mindfulness into your balance training for seniors routine. By combining elements of tai chi and yoga, you'll improve dynamic balance while also reducing stress and enhancing body awareness.
How to perform:
Sit tall in a sturdy chair with feet flat on the floor
Begin with deep breathing: inhale for 4 counts, exhale for 6 counts (3 times)
Slowly raise both arms out to the sides and up overhead while inhaling
Lower arms back down while exhaling
Gently turn your upper body to the right while extending your left arm across your body
Return to center and repeat on the opposite side
Continue this flowing sequence for 5 minutes
"The mindfulness component of tai chi and yoga movements amplifies their balance benefits," notes Dr. Emily Patel at Evolve. "When clients focus on the mind-body connection, they become more aware of subtle shifts in their center of gravity and respond more quickly to prevent falls."
A 2016 systematic review found that tai chi is particularly effective for balance training, with some studies showing up to a 50% reduction in fall rates among regular practitioners. As you become comfortable with the seated version, try performing the same movements while standing behind a chair for support.
Consistency is key with balance training for seniors. Even five minutes of practice daily will yield better results than an hour-long session once a week. Start where you are, use support when needed, and celebrate each small improvement along the way.
Adapting Balance Work for Different Ability Levels
At Evolve Physical Therapy + Sports Rehabilitation, we firmly believe that balance training for seniors should be accessible to everyone. Your unique health situation shouldn't prevent you from improving your stability and confidence—it simply means we need to customize your approach.
"I've seen remarkable progress in clients with significant physical challenges," shares Dr. Jessica Martin, who leads our specialized senior programs. "The key is meeting people where they are, then building gradually from that foundation."
For those with arthritis, joint pain can make balance work seem intimidating. We recommend performing exercises in our therapeutic pool where warm water reduces joint stress while providing gentle resistance. Many clients find their morning stiffness improves when they schedule sessions later in the day, and using chairs with supportive armrests creates confidence during standing exercises.
Seniors with osteoporosis need special consideration to protect their bone health. We emphasize proper alignment in all positions, avoiding excessive forward bending that might strain the spine. Instead, we focus on gentle weight-bearing exercises that actually strengthen bones while improving balance. Tai chi movements are modified to minimize twisting motions while maintaining their balance benefits.
Post-stroke recovery presents unique challenges that respond beautifully to specialized balance work. We typically begin with seated balance exercises to rebuild core stability, often using a gait belt with therapist assistance when transitioning to standing work. Many stroke survivors have asymmetrical strength and sensation, so we deliberately focus on weight shifting to the affected side, using mirror therapy to improve body awareness and neural reconnection.
For clients with Parkinson's Disease, we've developed specific approaches to address the freezing and shuffling that often compromise balance. Visual cues like colorful floor markers or laser pointers help overcome movement initiation problems. We incorporate rhythmic activities with music to improve timing and flow of movement. Most importantly, we schedule sessions when medication effectiveness is at its peak.
"The change in our Parkinson's clients has been incredible," notes physical therapist Alex Rivera. "One gentleman who could barely stand when he started now confidently performs tai chi sequences that would challenge people half his age."
Peripheral neuropathy creates balance challenges through reduced foot sensation. For these clients, we emphasize visual feedback—often having them watch their feet in a mirror during exercises. Textured mats provide improved sensory input that helps compensate for diminished foot sensation. We place special focus on ankle strengthening exercises and progress very gradually with close supervision.
When to Dial It Back—or Step It Up
Recognizing when to modify your balance training for seniors program is essential for both safety and progress. Your body provides clear signals when you need to make adjustments.
Listen to your body when it suggests you should dial back intensity. Pain during or after exercises (beyond mild muscle soreness) is never something to push through. Excessive fatigue that doesn't improve with rest indicates you may be doing too much too soon. If you notice increased unsteadiness or near-falls, that's your balance system telling you it's overwhelmed. Flare-ups of chronic conditions or feelings of anxiety about exercises are equally important warning signs.
"Many seniors have been taught to 'push through the pain,' but that's outdated and dangerous advice for balance work," explains Dr. Robert Chen at our Marine Park location. "The sweet spot is feeling challenged but confident."
When warning signs appear, we recommend returning to a previous, more comfortable level of exercise. Reduce your repetitions, add more support like a sturdy chair or wall, take frequent rest breaks, and focus on deep, relaxing breaths. There's no shame in stepping back temporarily—it's often the fastest path to long-term progress.
On the flip side, your body also tells you when it's ready for greater challenges. Exercises that feel too easy or boring indicate your balance systems have adapted and need new stimulation. When you can maintain proper form throughout all repetitions without fatigue, and you feel confident and stable after consistent practice for 2-3 weeks, it's time to progress.
Ready to advance? Try these proven techniques for challenging your balance systems:
Eyes-closed challenges eliminate visual input, forcing your vestibular and proprioceptive systems to work harder. Start with just 5 seconds of closed eyes while holding onto support, gradually increasing duration as you gain confidence.
Unstable surfaces like foam pads, pillows, or balance discs create controlled instability that strengthens your balance responses. One client, Margaret, age 75, began by standing on a folded towel and progressed to performing her entire routine on a specialized balance pad.
Dual-task training adds a cognitive component while balancing—try counting backward by 3s or naming animals while performing your exercises. This mimics real-world situations where you need to think and balance simultaneously.
Speed variations between slow and moderate movements during balance exercises help prepare you for unexpected situations in daily life. Start with deliberate, measured movements, then gradually introduce sections of slightly faster (but still controlled) motion.
"Finding your personal balance edge is what creates progress," says physical therapist Sarah Johnson. "At Evolve, we help you find exactly where that edge is—challenging enough to stimulate improvement but safe enough to build confidence rather than fear."
Tracking Your Progress & Knowing When to Seek Help
Watching your balance improve over time can be incredibly motivating. At Evolve, we've seen how tracking progress not only keeps our seniors engaged but also helps them recognize when they're ready for more challenges.
"Last month, I could barely stand on one leg for 3 seconds," shared Eleanor, one of our 68-year-old clients. "Yesterday, I hit 15 seconds! Seeing those numbers improve each week keeps me coming back to my exercises."
Here are simple, effective ways to monitor your balance training for seniors journey:
The 4-Stage Balance Test recommended by the CDC offers a straightforward assessment you can perform weekly. Start with feet side by side (easiest), progress to semi-tandem stance (heel of one foot beside the big toe of other foot), then to tandem stance (heel-to-toe), and finally to single-leg stance (most challenging). Using a stopwatch, record how long you can hold each position, aiming for up to 30 seconds.
The Timed Up and Go (TUG) Test measures functional mobility. Time yourself as you rise from a chair, walk 10 feet, turn around, return to the chair, and sit down. This simple test is remarkably revealing—healthcare professionals consider times over 12 seconds as potentially indicating increased fall risk.
Keeping a Fall Diary might sound discouraging, but tracking any stumbles, near-falls, or actual falls (noting where they happened and what might have contributed) can help identify patterns and specific situations to work on. Many of our clients at Evolve find that most of their balance challenges occur in predictable scenarios—like reaching for items on high shelves or walking on uneven sidewalks.
A simple Exercise Log documenting which exercises you completed, how many repetitions, and any difficulties encountered helps you and your physical therapist fine-tune your program as you progress.
Balance Test Initial Assessment After 4 Weeks After 8 Weeks Goal Single-leg stand 5 seconds 10 seconds 15 seconds 30 seconds Heel-to-toe walk 5 steps 10 steps 15 steps 20 steps TUG Test 14 seconds 12 seconds 10 seconds Under 10 seconds Sit-to-stand (30 sec) 8 repetitions 10 repetitions 12 repetitions 15 repetitions
"The numbers are helpful, but the real victory is in everyday life," explains Dr. Sarah Johnson at our Park Slope location. "When clients tell me they confidently steerd a crowded farmer's market or handled those tricky steps at their grandchild's school without a second thought—that's when I know our balance training for seniors program is truly working."
Consulting a Professional
While home-based balance exercises provide tremendous benefits, partnering with a physical therapist can take your progress to new levels. At Evolve Physical Therapy + Sports Rehabilitation, our specialists provide expert assessment of your specific balance challenges, create customized exercise programs, offer hands-on guidance for proper form, safely progress difficulty levels, and integrate balance work with other aspects of fitness.
"Many people don't realize that balance training isn't one-size-fits-all," notes Dr. Rodriguez, our Clinical Director. "What works beautifully for your neighbor might not address your specific challenges. A physical therapist can identify exactly which balance systems need the most attention in your case."
We recommend consulting with a physical therapist if you:
Have experienced a fall in the past year. Even a single fall significantly increases your risk of falling again. Early intervention can break this cycle.
Use a mobility aid like a cane or walker. We can help you maximize stability with your device while potentially working toward reduced dependence.
Feel unsteady during everyday activities. That feeling of unsteadiness is your body's warning system—don't ignore it.
Live with conditions affecting balance. Conditions like neuropathy, Parkinson's disease, stroke, or vestibular disorders benefit from specialized approaches.
Take multiple medications. Many common medications can affect balance, and a PT can help develop strategies to counteract these effects.
Pay particular attention to these red-flag symptoms that warrant immediate professional attention: sudden severe dizziness, a new pattern of falling consistently in one direction, falls without awareness, loss of consciousness, or significant fear that's limiting your daily activities.
"I always tell my clients that balance training for seniors is most effective as prevention rather than rehabilitation," Dr. Rodriguez emphasizes. "Why wait until after a serious fall to seek help? The work we do proactively can save so much hardship down the road."
For those unable to visit our Brooklyn locations in person, we offer telehealth options where we can observe your balance exercises, make real-time corrections, and progress your program remotely. Technology has made professional guidance more accessible than ever—something our clients particularly appreciated during the pandemic.
Improved balance isn't just about preventing falls—it's about maintaining independence, confidence, and quality of life as you age. And that's a goal worth tracking.
Frequently Asked Questions about Balance Training for Seniors
How soon will I notice improvement?
When clients first come to Evolve for balance training for seniors, they often ask how quickly they'll see results. The good news is that most people notice small improvements within 2-4 weeks of consistent practice. Those initial victories might be as simple as feeling more confident when reaching for something on a high shelf or navigating a curb without hesitation.
The more significant changes, however, typically emerge after 8-12 weeks of regular training. This timeline mirrors what researchers found in a 2019 study, where older adults practicing balance exercises three times weekly showed measurable stability improvements at the six-week mark, with continued gains through their 12-week program.
"Balance improvement follows a pattern similar to strength training," explains Dr. Lisa Chen from our Park Slope location. "You'll likely notice small changes quickly as your nervous system adapts, followed by more substantial improvements as neural pathways strengthen and muscles respond to the new demands."
Many of our clients keep a simple balance journal, noting little victories along the way—like standing on one leg for five seconds longer or walking heel-to-toe across the entire living room. These incremental improvements build both physical stability and psychological confidence.
Can strength, flexibility, and cardio replace balance drills?
I hear this question frequently in our Brooklyn clinics. While strength, flexibility, and cardiovascular exercises are essential pieces of the fitness puzzle for seniors, they don't specifically target the complex neural pathways and sensory integration needed for optimal balance.
"I often see clients who faithfully lift weights at the gym three times a week but still struggle with balance," notes Dr. James Wilson from our Gravesend facility. "That's because balance is a specific skill that requires targeted training of the proprioceptive, visual, and vestibular systems all working together."
Think of it this way: strength gives you the power to recover from a wobble, flexibility allows your joints to move through necessary ranges, and cardiovascular fitness provides the endurance for daily activities. But balance training for seniors teaches your brain how to integrate information from your eyes, ears, and body to maintain stability in the first place.
The most effective approach combines all these elements in a comprehensive program. At Evolve, we design personalized plans that address each component, with particular emphasis on the specific balance challenges each person faces. For some, that might mean more vestibular exercises; for others, proprioceptive training takes priority.
Is it safe to train balance if I use a cane or walker?
Absolutely! In fact, balance training for seniors who use assistive devices isn't just safe—it's especially valuable.
"Using a cane or walker doesn't mean you should avoid balance training—quite the opposite," emphasizes Dr. Maria Gonzalez at our Mill Basin location. "With proper supervision and modifications, balance exercises can help reduce dependence on assistive devices or ensure they're used more effectively and safely."
Margaret, an 81-year-old client who came to us after a hip replacement, was initially concerned that her walker made balance exercises impossible. We started with seated activities and supported standing exercises, always keeping her walker within reach. Six months later, she steers her apartment with just a cane and uses her walker only for longer outdoor excursions.
At Evolve, we take a thoughtful, graduated approach for clients with assistive devices:
We begin with seated balance exercises and fully supported standing activities, ensuring complete safety. As confidence builds, we progress to exercises performed while holding the assistive device, then practice short periods of standing near (but not holding) the device while maintaining safety. Throughout this process, we gradually extend the duration and complexity of exercises based on individual progress.
Some clients ultimately reduce their reliance on assistive devices, while others maintain their use but with greater confidence and stability. Both outcomes represent success in our view—the goal is always improved quality of life and independence, whatever form that takes for each individual.
Conclusion
There's something truly empowering about taking control of your balance and stability as you age. After working with thousands of seniors at Evolve Physical Therapy + Sports Rehabilitation, I've witnessed how balance training for seniors transforms lives—not just by preventing falls, but by restoring confidence and independence.
Think of balance training as an investment in your future self. Like Margaret, who at 79 told me, "I used to think my unsteady days were just part of getting older. Now I'm more stable than I was at 70!" Her story isn't unusual among our Brooklyn clients who commit to regular practice.
The journey to better balance isn't complicated, but it does require commitment:
Start exactly where you are today—not where you think you "should" be. If that means holding onto a chair for every exercise, that's perfectly fine. Safety always comes first, and progress builds from a foundation of confidence.
Consistency truly is the secret ingredient. Even short 10-minute balance sessions three times weekly yield remarkable results over time. As one of our Mill Basin clients puts it, "It's like compound interest for your body—small deposits of effort that create big returns."
Your balance training should evolve as you do. When exercises begin feeling comfortable, that's your body's signal that it's ready for the next challenge. Those moments of progression—when you first stand on one leg without support or walk heel-to-toe across the room—deserve celebration!
What makes me most passionate about our work at Evolve is seeing how improved balance extends beyond physical stability. Our clients report sleeping better, experiencing less anxiety, and participating more fully in family activities. One gentleman recently told me he finally felt confident enough to dance at his granddaughter's wedding—a moment he'd been dreading missing.
While the exercises we've outlined provide an excellent starting point, personalized guidance often makes the difference between good results and transformative ones. Our physical therapists throughout Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin specialize in tailoring balance programs to individual needs, especially for those with specific health concerns or fall history.
Eleanor, an 84-year-old client who started with us after a hip fracture, captures the essence of successful balance training for seniors: "I don't just have better balance now—I have my life back. I garden, shop, and play with my great-grandchildren without that constant fear of falling. These simple exercises have given me freedom I thought was gone forever."
Your journey to better balance starts with a single step—and we're here to ensure it's a steady one. Whether you're proactively working to prevent falls or recovering from a balance-related incident, our team at Evolve Physical Therapy + Sports Rehabilitation is ready to support you with evidence-based, hands-on guidance that builds both stability and confidence.
For more information about our specialized balance programs or to schedule an assessment, contact us today. Your fall-free future is within reach—and it's so worth the effort.
Strengthen and Stretch: Exercises for Hip Labral Tears
Understanding Hip Labral Tears and Recovery
Here are the most effective physical therapy exercises for labral tear hip rehabilitation:
Early Phase (Weeks 1-4)
Hip flexor stretches (30 sec holds, 3x daily)
Glute bridges (10 reps, 3 sets)
Isometric hip exercises
Intermediate Phase (Weeks 5-7)
Single-leg bridges (10 reps/side)
Standing hip abduction with band (3 sets of 10)
Wall sits with clam shells (60-sec holds)
Advanced Phase (Weeks 8-12)
Fire hydrants with resistance (12 reps, 3 sets)
Monster walks (15-20 steps each direction)
Side plank clam shells (8-10 reps/side)
Physical therapy exercises for labral tear hip conditions are vital for recovery, whether you're managing symptoms conservatively or rehabilitating after surgery. A hip labral tear affects the cartilage ring (labrum) that lines your hip socket, potentially causing pain, clicking, and limited mobility. While this might sound alarming, the good news is that many labral tears respond well to targeted exercise therapy.
Contrary to what you might expect, hip labral tears are actually quite common. Studies show that up to 40% of people in their 20s and 30s have labral tears with no symptoms at all. For those experiencing pain, a structured rehabilitation program typically spans 8-12 weeks, focusing on strengthening the muscles around the hip, improving mobility, and restoring proper movement patterns.
The key to successful recovery lies in following a progressive exercise protocol that respects tissue healing timelines while gradually challenging the hip joint. Most importantly, exercises should never cause sharp pain—if they do, it's a sign to modify or consult your healthcare provider.
I'm Lou Ezrick, founder of Evolve Physical Therapy, where I've spent nearly two decades developing specialized physical therapy exercises for labral tear hip rehabilitation programs that have helped thousands of patients return to pain-free activity without surgery.
Standing Hip Abduction
If you're recovering from a hip labral tear, the standing hip abduction exercise might just become your new best friend. This movement specifically targets your gluteus medius—a key muscle that helps stabilize your hip and takes pressure off your injured labrum during everyday activities.
"I recommend this exercise to almost all my hip labral tear patients," says Lou from our physical therapy team at Evolve. "When your lateral hip muscles are strong, they help keep your femoral head properly positioned in the socket, which can significantly reduce labral stress and pain."
Here's how to perform this physical therapy exercise for labral tear hip rehabilitation correctly:
Stand tall with your feet hip-width apart, maintaining good posture
Place a resistance band around your ankles or just above your knees
Shift your weight onto your stronger leg (or less painful side)
Slowly move your other leg out to the side about 12-18 inches
Hold for 2-3 seconds at the top position
Lower your leg with control
Complete 3 sets of 10 repetitions on each side, resting 30-60 seconds between sets
Balance is crucial here—don't hesitate to lightly touch a wall or chair for support if needed. The most common mistake I see patients make is hiking their hip during the movement. The motion should come purely from your hip joint, not by tilting your pelvis.
Keep your toes pointing forward throughout the exercise and maintain a slight bend in your supporting knee to protect the joint. As you lift your leg, you should feel the work happening along the outside of your hip—that's your gluteus medius saying hello!
Sarah, one of our regular patients who came to us with a labral tear from running, shared: "This exercise felt awkward at first, but after consistently doing it for two weeks, I noticed I had way less pain walking up the subway stairs. It was like my hip finally had the support it needed."
Ready to challenge yourself? Once you've mastered the basic movement, try increasing the resistance band strength, holding the abducted position longer, or performing the exercise on a foam pad to improve your balance and proprioception.
This exercise should never cause sharp pain in your hip—a mild burn in the muscles is normal, but anything more intense means you should modify your technique or consult with one of our physical therapists at Evolve.
Single-Leg Bridge
Looking for a powerful physical therapy exercise for labral tear hip rehabilitation that won't aggravate your symptoms? The single-leg bridge deserves a special place in your recovery program.
This exercise is a true multitasker for your posterior chain—those essential muscles running along the back of your body. It specifically targets your glutes and hamstrings while being gentle on the front of the hip where most labral tears occur.
What makes the single-leg bridge so valuable for hip recovery? For starters, it improves pelvic stability during everyday movements like walking and climbing stairs. It also strengthens your hip extensors without compressing the sensitive anterior hip. Perhaps most importantly, it helps establish proper muscle activation patterns that actually protect your labrum from further irritation.
"Many of our patients with labral tears show weakness in their gluteal muscles," explains our physical therapy director at Evolve. "This forces other structures to pick up the slack, potentially worsening the tear. The single-leg bridge addresses this imbalance while keeping the hip in a safe, non-impinging position."
Here's how to do it right:
Lie on your back, knees bent, feet flat on the floor about hip-width apart
Rest your arms at your sides with palms down for stability
Engage your core by gently drawing your belly button toward your spine
Extend one leg straight out while keeping both thighs parallel
Press through the heel of your planted foot, lifting your hips toward the ceiling
At the top, give your glutes a good squeeze, forming a straight line from shoulders to extended knee
Hold this position for 2-5 seconds, breathing normally
Lower with control—no dropping!
Complete 10 repetitions before switching sides
Aim for 3 sets with about 2 minutes of rest between them
When you're ready for more challenge, we often introduce the single-leg bridge with box variation at Evolve. Simply place one foot on a sturdy box or step (12-18 inches high) and extend your other leg. Push through the heel on the box to lift your hips. This increases both the range of motion and the work for your glutes.
One quick but important tip: keep your pelvis level throughout the exercise. If you notice it rotating or tilting as you lift, that's a sign to reset your form. And if you feel any pinching in the front of your hip, lower the height of your bridge or return to regular double-leg bridges until you build more strength.
As Michael, a 45-year-old patient recovering from a labral tear, shared with us: "The single-leg bridge was a game-changer for me. After three weeks of consistent practice, I noticed I could walk longer distances without the nagging pain in my hip. Plus, my balance improved dramatically!"
Fire Hydrants
Ever watched a dog lift its leg at a fire hydrant? That's exactly the movement we're mimicking with this exercise—and it's one of the most effective physical therapy exercises for labral tear hip rehabilitation you can do.
Fire Hydrants target your gluteus medius and external hip rotators, which are crucial muscles for hip stability. These muscles help position your femur (thigh bone) properly in the hip socket, taking pressure off your labrum where it's often irritated.
"I recommend Fire Hydrants to almost all my hip patients," says Lou Ezrick, founder of Evolve Physical Therapy. "They build strength in exactly the right places to help decompress the hip joint where labral tears typically occur."
Here's how to do Fire Hydrants correctly:
Start on all fours in a quadruped position with your hands under your shoulders and knees under your hips
Brace your core—imagine pulling your belly button toward your spine
Keeping your knee bent at 90 degrees, lift one leg out to the side
Raise until your thigh is roughly parallel to the floor (or as high as comfortable without pain)
Hold briefly at the top, then lower with control
Complete 12 repetitions before switching sides
Aim for 2-3 sets total
The key to getting the most benefit is proper form. Keep your weight evenly distributed between both hands and your supporting knee. Your pelvis should stay level throughout—resist the urge to shift your body as you lift your leg. Think about initiating the movement purely from your hip joint.
"After six weeks of doing Fire Hydrants daily, I could finally cross my legs again without that painful catching sensation," shares Mike, a 42-year-old patient recovering from a labral tear. "It was the first exercise where I really felt those side hip muscles working."
For those progressing well, try adding a mini resistance band just above your knees. This increases the challenge to your external rotators and can accelerate strength gains. You can also experiment with extending your leg straight out to the side at the top of the movement for an additional challenge.
Remember to breathe normally throughout the exercise. While you might feel a gentle stretch sensation, sharp pain is a sign to modify or stop. Always prioritize quality over quantity—a few perfect repetitions will benefit you more than many sloppy ones.
Wall Sit with Clam Shell
Remember those wall sits your gym teacher made you do in school? We're bringing them back—but with a therapeutic twist that makes them incredibly effective for hip labral tear recovery!
The Wall Sit with Clam Shell is one of my favorite combination exercises because it works multiple muscle groups simultaneously. This efficient movement strengthens your quadriceps through the isometric wall hold while also targeting those critical external hip rotators that help protect your labrum. As a bonus, your core gets a great workout as it stabilizes your pelvis throughout the exercise.
"What makes this exercise so valuable for my patients with labral tears is how it trains the hip muscles in a functional, weight-bearing position," explains Lou, our director at Evolve. "This translates much better to everyday activities than exercises done lying down."
Here's how to perform this exercise correctly:
Stand with your back flat against a wall
Place a mini resistance band just above your knees
Walk your feet forward about 18-24 inches, keeping them shoulder-width apart
Slide down the wall into that invisible chair position, with knees bent at about 45-60 degrees
While holding this position, slowly open one knee outward against the band
Hold for 2-3 seconds, then return to start
Alternate legs for 10 repetitions per side
Aim to maintain the wall sit for 60 seconds per set
Complete 3 sets, resting between each
Important technique tips: Keep your back flush against the wall and your weight in your heels, not your toes. Don't let your knees collapse inward or push forward beyond your toes. Your feet should stay firmly planted as you open your knees—no rotating!
Too challenging? No problem. Start with a higher wall sit position (less knee bend) and gradually work your way down as you build strength. You can also begin without the resistance band and add it when you're ready for more of a challenge.
I've seen remarkable progress in patients who consistently incorporate this exercise. Jennifer, a 38-year-old dancer with a labral tear, told me: "The Wall Sit with Clam Shell gave me back my confidence. After six weeks, I could finally return to basic dance movements without feeling like my hip might give way."
This physical therapy exercise for labral tear hip rehabilitation is particularly effective because it trains proper muscle activation patterns while in positions that mimic real-life movements—exactly what you need for long-term healing and prevention of future injuries.
Horizontal Squat Stretch
There's something wonderfully restorative about the Horizontal Squat Stretch when you're dealing with a labral tear. This gentle mobility exercise has become one of our patients' favorites at Evolve Physical Therapy because it offers relief while promoting healing.
What makes this stretch so perfect for physical therapy exercises for labral tear hip rehabilitation is how it creates space in the joint. Unlike many stretches that can compress the labrum, this position actually decompresses the hip joint while gently opening up your inner thighs and hip rotators.
"I recommend the Horizontal Squat Stretch to almost all my labral tear patients," shares our lead hip specialist at Evolve. "It's like hitting a reset button for tight hips without aggravating the tear."
Here's my simplified approach to getting this stretch just right:
Start on all fours with your hands directly under your shoulders. Spread your knees wider than your hips—wider than your hands too. Keep your feet in line with your knees, not turned in or out. Now for the magic: slowly sink your hips back toward your heels, moving backward until you feel that "ahh" stretch sensation in your inner thighs. Hold this sweet spot for 30-60 seconds, breathing deeply. Return to start and repeat three times.
The beauty of this stretch is its adaptability. If you're feeling particularly tight, don't force it—just reduce the width between your knees. For those more flexible folks looking for a deeper release, try gently rocking side to side while in the stretched position.
"Before finding this stretch, I couldn't put on my socks without pain," David, our 45-year-old hiking enthusiast patient told me. "After doing the Horizontal Squat Stretch daily for two weeks, not only could I dress without wincing, but the constant clicking in my hip started to disappear."
For knee comfort, I often suggest placing a folded towel underneath for cushioning. If your wrists complain, try lowering to your forearms or using yoga blocks for support.
This stretch works best when you're already a bit warmed up, so consider it after a short walk or gentle movement. Consistency is key—aim to include it in your daily routine for the best results. Your hips will thank you with improved mobility and decreased discomfort as you continue your labral tear recovery journey.
Kneeling Hip Flexor Stretch
If you've been dealing with a hip labral tear, you're probably familiar with that nagging pain in the front of your hip. That's where the Kneeling Hip Flexor Stretch comes to the rescue—it's truly one of the most effective physical therapy exercises for labral tear hip rehabilitation in our toolkit at Evolve.
This stretch targets those pesky iliopsoas muscles (your hip flexors) that tend to get tight and cranky, especially if you spend hours sitting at a desk. When these muscles tighten up, they can actually pull the head of your femur forward in the socket, putting unwelcome pressure right where your labral tear is trying to heal. No wonder it hurts!
"I often tell my patients that tight hip flexors are like a constant tug-of-war on your hip joint," says our hip specialist. "This simple stretch can provide almost immediate relief by releasing that forward pressure."
Here's how to do this stretch properly:
Start in a half-kneeling position with one knee on the floor
Position your other foot flat on the floor in front of you, knee at a 90-degree angle
Place a cushion or folded towel under your kneeling knee (your joints will thank you!)
Keep your torso upright with your core gently engaged
The magic happens when you tuck your tailbone under (posterior pelvic tilt) while gently shifting weight forward
You'll feel a stretch along the front of your hip and thigh on the kneeling leg
Hold for 30 seconds, breathing normally
Release and repeat 3 times on each side
The most common mistake I see patients make is arching their lower back instead of tucking the pelvis. It's not about leaning forward—it's about that subtle pelvic tilt that targets the right muscles.
One of our patients, Lisa, works full-time at a computer and was diagnosed with a labral tear after months of hip pain. "This stretch has been a game-changer for me," she shared. "I do it three times a day, especially after long meetings. The relief is almost immediate, and that annoying clicking sound has significantly decreased."
For those of you who've mastered the basic version, try raising the arm on the same side as your kneeling leg overhead. This creates a gentle spinal rotation and deepens the stretch through your entire front body chain.
To get the most benefit, consistency trumps intensity. We recommend performing this stretch at least three times daily, especially after you've been sitting for a while. Your hip flexors will gradually lengthen, taking pressure off that sensitive labral area.
This stretch should feel good—a gentle pulling sensation is normal, but if you feel any sharp pain, ease up and consult your physical therapist about modifying your technique.
Monster Walks
If you've ever seen someone shuffling sideways with a mini-band around their legs looking a bit like Frankenstein's monster, you've witnessed one of the most valuable physical therapy exercises for labral tear hip rehabilitation in action!
Monster Walks are a fan favorite at Evolve Physical Therapy because they target those crucial hip stabilizers—particularly the gluteus medius and minimus—that often become weak in patients with labral tears. These muscles are your hip's natural "security guards," keeping your femur properly centered in the socket where the labrum lives.
"What makes Monster Walks so effective is that they train your hip muscles in a functional, weight-bearing position," explains our hip specialist. "Unlike isolated exercises where you're lying down, Monster Walks challenge your hip stabilizers while you're upright and moving—just like in real life."
Here's how to perform this exercise with proper form:
Loop a resistance band just above your knees (for beginners) or around your ankles (for more challenge)
Stand with feet hip-width apart, creating slight tension in the band
Bend your knees slightly and hinge forward at the hips about 15-20 degrees
Engage your core—imagine drawing your belly button toward your spine
Step sideways with one foot while maintaining tension in the band
Follow with your other foot, keeping the same distance between your feet
Continue stepping sideways for 15-20 steps in one direction
Reverse direction and return to your starting point
Complete 2-3 sets in each direction
Remember to keep your toes pointing forward throughout the movement—no duck-walking allowed! The resistance should feel challenging but not painful. If your knees start collapsing inward or your form breaks down, it's a sign the band resistance might be too strong.
"I recommend Monster Walks to almost all my labral tear patients," says our PT director. "They're simple but incredibly effective for improving hip stability and proprioception—your body's ability to know where it is in space."
One of our patients, James, a 40-year-old recreational basketball player, found Monster Walks particularly helpful: "After six weeks of consistent Monster Walks, I noticed a huge difference when playing basketball. That feeling of my hip 'giving way' when I changed direction disappeared almost completely."
As you progress, we can make this exercise more challenging by increasing band resistance, adding a backward walking component (taking diagonal steps backward), or performing the exercise in a deeper squat position. The key is consistent practice—aim for Monster Walks 3 times per week, focusing on quality over quantity.
For optimal results, pair Monster Walks with the other exercises in your hip labral tear rehabilitation program. Together, they create a comprehensive approach that strengthens all the muscle groups supporting your hip joint, potentially speeding your recovery and preventing future issues.
Side Plank Clam Shells
If you're looking for a challenge that really ties your hip and core strength together, Side Plank Clam Shells might just become your new favorite exercise. This movement combines two powerhouse exercises into one advanced physical therapy exercise for labral tear hip rehabilitation.
Think of this as the graduate-level exercise in your hip recovery journey – one that simultaneously works your hip rotators and core stability in a way that mimics real-life movements.
"What I love about Side Plank Clam Shells is how they teach your body to coordinate between core and hip strength," explains our hip specialist at Evolve. "In everyday life, your core and hips don't work in isolation – they work together. This exercise trains that connection."
Here's your step-by-step guide to performing Side Plank Clam Shells correctly:
Start in a side plank position, resting on your forearm with elbow directly under your shoulder
Stack your feet, knees, hips, and shoulders in one straight line
Place a mini resistance band just above your knees (optional for beginners)
Bend both knees to about 45 degrees
While maintaining your side plank position, slowly lift your top knee away from the bottom one
Keep your feet touching throughout the movement (this is key!)
Hold at the top for a brief 1-2 second count
Lower with control back to the starting position
Aim for 8-10 repetitions before switching sides
Complete 2-3 sets per side
Your body will try to find the path of least resistance during this exercise – don't let it! Keep your body in a straight line from head to feet, engage your core throughout, and resist the urge to rotate your hips backward as you lift your knee. Your shoulder should stay stable too – don't let it roll forward.
"I remember struggling with this exercise when I first tried it," shares Emma, a 32-year-old yoga instructor who came to us with a labral tear. "But it became a turning point in my recovery. Once I mastered Side Plank Clam Shells, I could return to challenging yoga poses that had previously triggered my hip pain."
If you find this movement too difficult at first, don't worry! We recommend mastering regular side planks and standard clam shells separately before combining them. You can also modify by keeping your bottom knee bent on the floor for extra support.
This exercise typically enters your routine during the advanced phase of rehabilitation (around weeks 8-12), once you've built a solid foundation of hip and core strength. One perfect rep is worth more than ten sloppy ones – focus on quality over quantity.
At Evolve Physical Therapy, we've found that this exercise particularly helps patients preparing to return to more demanding activities like sports, dance, or advanced fitness classes. The combination of anti-rotation core work with hip external rotation creates the perfect preparation for multidirectional movements in daily life and athletic activities.
Physical Therapy Exercises for Labral Tear Hip: Progression & Safety
Moving through hip labral tear rehabilitation is a bit like climbing a mountain—you need the right pace, equipment, and strategy to reach the summit safely. At Evolve Physical Therapy, we've guided countless patients through this journey using evidence-based approaches that respect your body's healing timeline.
"The biggest mistake I see patients make is rushing through their rehab," shares Lou Ezrick, our clinical director. "Recovery isn't about racing through exercises—it's about thoughtfully loading the hip to encourage proper healing while listening to your body's feedback along the way."
When should you progress to the next phase of physical therapy exercises for labral tear hip rehabilitation? We follow these clear guidelines:
Your pain should stay at 3/10 or less during and after exercises. Think of pain as a traffic light—mild discomfort is a yellow light (proceed with caution), while sharp pain is definitely a red light (stop).
There shouldn't be a "pain hangover" the next day. If Tuesday's exercises leave you limping on Wednesday, that's your body saying "too much, too soon."
Quality matters more than quantity. Before adding weight or repetitions, make sure your form is spot-on. As my grandmother used to say, "If something's worth doing, it's worth doing right!"
Your range of motion should be stable or improving—never decreasing. Backwards progress is a clear sign to reassess.
Daily activities like walking and climbing stairs should feel progressively easier. These functional improvements are the true measure of successful rehabilitation.
Research published in the Journal of Orthopaedic & Sports Physical Therapy backs our approach, recommending a 10-12 week phased protocol for conservative management of labral tears. The key insight? Your body's response—not the calendar—should guide your progression. For more detailed information on hip labral tear healing timelines, you can review Mayo Clinic's comprehensive guide on hip labral tears.
While we're eager to get you back to your favorite activities, certain movements are definite no-gos during early healing. Avoid the FADIR position (flexion, adduction, internal rotation), which can pinch the labrum. Skip prolonged sitting without breaks, high-impact exercises, and aggressive stretching that causes pain.
When to Begin Physical Therapy Exercises for Labral Tear Hip
"When can I start exercising?" is often the first question patients ask after a labral tear diagnosis. The answer depends on several factors we carefully evaluate at Evolve Physical Therapy.
For non-surgical management, you can typically begin gentle exercises soon after diagnosis, once initial pain management strategies are in place. We look for your ability to bear weight on the affected leg with minimal pain—a good indicator that basic exercises won't overwhelm the joint.
We'll start with isometric exercises—gentle muscle contractions without joint movement—which strengthen surrounding muscles without stressing the labrum. As your symptoms allow, we'll carefully introduce more dynamic movements.
If you've had surgery, your timeline will follow your surgeon's specific protocol. Most patients begin protected weight-bearing and gentle range of motion exercises within days after surgery. The type of procedure matters too—a labral repair typically requires more protection than a debridement.
"What many people don't realize," explains our hip specialist, "is that the average person experiences symptoms for over two years before receiving a proper diagnosis. During this time, your body develops compensatory movement patterns that need to be addressed alongside the tear itself."
Your starting point will be influenced by whether your injury is fresh or long-standing, how much swelling is present in the joint, and your weight-bearing status. This is why cookie-cutter exercise programs often fall short—your rehabilitation should be as unique as you are.
Red Flags: Stop Physical Therapy Exercises for Labral Tear Hip If...
While some muscle soreness is normal during rehabilitation, certain symptoms are like warning lights on your car's dashboard—ignore them at your peril.
Contact your healthcare provider immediately if you experience:
Sharp, catching pain in the groin that feels like something is being pinched inside the joint. This could indicate the labrum is getting caught between bone surfaces.
Locking or giving way of the hip joint, which might suggest a mechanical problem that needs medical attention.
Increasing night pain that interrupts your sleep. Rehabilitation should improve sleep, not worsen it.
Progressive loss of motion despite consistent exercises. You should be gaining mobility, not losing it.
Pain radiating down your leg, which might signal nerve involvement beyond the labral issue.
Noticeable swelling around the hip joint, potentially indicating inflammation that needs to be addressed.
Pain that hangs around more than 24 hours after exercise or causes you to limp.
"There's a big difference between productive discomfort and problematic pain," notes our senior therapist. "Productive discomfort feels like muscles working hard and fades relatively quickly. Problematic pain feels sharp, lingers for hours, and often causes you to alter how you move."
If these red flags appear, temporarily modify or pause your exercise program and check in with your physical therapist. Sometimes we need to adjust your plan or your physician might want additional imaging to ensure optimal healing.
Listening to your body isn't being weak—it's being wise. The most successful recoveries come from patients who partner with their healthcare team and respect the healing process every step of the way.
Frequently Asked Questions about Hip Labral Tear Rehab
How long does conservative recovery usually take?
When patients first learn they have a hip labral tear, their most pressing question is almost always about timeline. At Evolve Physical Therapy, we typically see conservative recovery taking 8-12 weeks with dedicated physical therapy exercises for labral tear hip rehabilitation.
That said, recovery isn't one-size-fits-all. Your personal journey depends on several factors: the size and location of your tear, whether it happened suddenly or developed gradually, any underlying hip conditions like impingement or dysplasia, plus your age, activity level, and overall health. And let's not forget one of the biggest factors – how consistently you perform your home exercise program!
"The labrum will take approximately 8-12 weeks to heal on its own in a perfect world with conservative management and physical therapy," I often tell my patients. I always make sure to explain that the labrum has limited blood supply, which is why patience is so important during recovery.
The good news? Many of our patients at Evolve start noticing significant symptom improvement within 4-6 weeks of beginning appropriate exercises, even though the tissue itself is still healing. Research published in the American Journal of Sports Medicine found that about two-thirds of patients with labral tears became symptom-free with conservative treatment including physical therapy – that's encouraging!
I've noticed over my years of practice that the patients who consistently show up for themselves – doing their exercises regularly and respecting activity modifications – tend to recover more quickly than those who take a more casual approach to their rehab program.
Which movements should I avoid early on?
During early rehabilitation, certain movements can put extra stress on your healing labrum. Think of these as the "not yet" movements – ones you'll likely return to eventually, but need to avoid while healing begins.
Deep squatting beyond 90 degrees of hip flexion is a common culprit for irritation. Similarly, excessive hip rotation, especially when combined with flexion, can aggravate a labral tear. I always caution my patients to temporarily pause high-impact activities like running or jumping, as these can delay healing.
"Sitting is the new smoking" takes on extra meaning with labral tears – prolonged sitting without position changes can increase pressure on the labral tissue. Set a 30-minute timer to remind yourself to stand and move around. Also on the avoid list: heavy lifting that causes hip strain, aggressive stretching that produces groin pain, and pivoting or cutting motions on your affected leg.
"The position that typically reproduces labral symptoms combines flexion, adduction, and internal rotation – what we call the FADIR position," I explain to patients. "Listen to your body – avoid hip motions that create intense pain or pinching."
The good news is that as your rehabilitation progresses, we can gradually reintroduce many of these movements under proper guidance. Your physical therapist will help determine when it's safe to begin challenging your hip in more demanding positions.
When is surgery the better option?
While many hip labral tears respond beautifully to conservative management with physical therapy exercises for labral tear hip rehabilitation, there are situations where surgery may be the better path forward.
If you've diligently completed 3-6 months of appropriate physical therapy without significant improvement, it might be time to consider surgical options. Similarly, large, unstable tears – especially those causing mechanical symptoms like catching or locking – often respond better to surgical intervention.
Tears associated with significant bony abnormalities, such as severe femoroacetabular impingement (FAI) or hip dysplasia, frequently benefit from addressing both the labral tear and the underlying structural issue. High-level athletes sometimes opt for surgical repair to facilitate a quicker return to their sport. And if your symptoms are progressively worsening despite appropriate conservative management, that's another indication surgery might be warranted.
"There's no one-size-fits-all answer here," I explain to my patients at Evolve. "The decision between conservative care and surgery should be individualized based on your specific tear characteristics, activity goals, and response to initial treatment. Surgery isn't necessarily better or worse—it's about matching the right treatment to the right patient."
If you're weighing surgical options, I recommend consulting with both a hip preservation specialist (orthopedic surgeon) and a physical therapist experienced in hip rehabilitation to understand all your options. Many patients benefit from "prehabilitation" physical therapy even when surgery is planned – stronger muscles and better movement patterns before surgery often lead to better outcomes afterward.
Conclusion
Rehabilitating a hip labral tear is a journey that demands patience, consistency, and a thoughtful approach to exercise. The physical therapy exercises for labral tear hip rehabilitation we've explored together form a comprehensive roadmap to recovery that addresses all the key elements: restoring mobility, building stability, developing strength, and relearning functional movement patterns.
As you work through your own rehabilitation process, keep these essential principles close to heart:
First and foremost, listen to your body and respect pain signals. A good challenge feels productive, but sharp pain is your body's way of saying "not yet." Quality always trumps quantity—one perfect bridge is worth more than ten sloppy ones. Consistency beats intensity every time; your hip will respond better to daily gentle care than occasional heroic efforts.
"The most common mistake I see patients make is rushing to advanced exercises before mastering the basics," shares our senior therapist at Evolve. "Your rehabilitation is a staircase, not an elevator—and each step needs to be solid before you climb to the next."
Your glutes are your greatest allies in this recovery. These powerful muscles, when properly engaged, take tremendous pressure off your labrum during everyday activities. Equally important is maintaining balanced mobility; regular, gentle stretching prevents the compensatory patterns that can reinforce pain cycles.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we've guided countless patients through this exact journey. Our approach isn't just about treating the tear—it's about understanding how your entire body moves and creating personalized treatment plans that address the root causes of your pain.
"I came in thinking I needed surgery," recalls Michael, a 43-year-old runner we treated. "Six weeks later, I was back on the trails. The team at Evolve didn't just fix my hip—they taught me how to move better than I did before the injury."
Research consistently shows that many labral tear patients become completely symptom-free with dedicated physical therapy alone. Whether you're hoping to avoid surgery or recovering from a procedure, the structured exercise program we've outlined provides a proven path forward.
Your journey to recovery begins with understanding your condition and committing to the process. By following the principles and exercises we've shared, you're already taking meaningful steps toward restored hip health and pain-free movement.
For personalized guidance custom to your unique needs and goals, contact Evolve Physical Therapy + Sports Rehabilitation to schedule an evaluation with our specialized team. We're here to help you move beyond your hip labral tear and back to the activities you love.