
Brooklyn Physical Therapy News- Evolve NY
An Essential Guide to Pediatric Physical Therapy Options
Why Pediatric Physical Therapy Matters for Your Child's Development

Pediatric physical therapy is a specialized field that helps children from birth to 21 years old develop or regain the skills needed to move, function independently, and participate in daily life. It focuses on improving quality of life through hands-on care and prescribed movement.
Core Elements of Pediatric Physical Therapy:
- Who it serves: Children with developmental, traumatic, or systemic disorders.
- What it addresses: Issues with movement, coordination, balance, strength, and endurance.
- Primary approach: Play-based therapeutic activities, exercise, and functional training.
- Key goal: Promoting independence and participation in home, school, and community life.
- Treatment team: Licensed physical therapists working with families, schools, and medical professionals.
This therapy is distinct in its emphasis on enabling children to enjoy their childhood, not just treating symptoms. Therapists collaborate closely with parents to develop customized treatment plans that fit into a child's daily routines.
As Lou Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades providing pediatric physical therapy services focused on holistic, hands-on treatment. Our approach at Evolve addresses the root cause of movement challenges while empowering families with the tools they need to support their child's progress.
Understanding Who Benefits and Why
Parents often come to Evolve Physical Therapy with concerns about their child's development. Maybe a toddler isn't walking, a teenager has a persistent sports injury, or a new diagnosis feels overwhelming. Pediatric physical therapy serves children from birth through age 21, supporting them through incredible periods of growth.
While every child develops at their own pace, some need extra support to reach milestones like sitting, walking, or riding a bike. Our therapists understand these developmental pathways and create interventions that meet each child where they are. We practice whole-person care, considering the physical, emotional, and social aspects of a child's life, because all these pieces affect their ability to thrive.
Most importantly, we use a family-centered approach. You know your child best, and we see ourselves as partners. We listen to your concerns, involve you in setting goals, and teach you techniques to use at home, because therapy happens in everyday life, not just in our clinic.

Common Conditions Treated with Pediatric Physical Therapy
Each child receives an individualized approach. Some conditions we frequently see in our Brooklyn clinic include:
- Developmental delays: When a child isn't reaching milestones like rolling, sitting, or walking on a typical timeline.
- Cerebral palsy: We work to improve muscle tone, strength, and coordination to help children with this condition achieve greater independence.
- Muscular torticollis: We use gentle stretches and positioning, ideally before 3 months of age, to treat tight neck muscles that cause an infant's head to tilt.
- Autism spectrum disorder: We address motor coordination difficulties and balance issues to help children participate more fully in activities.
- Down syndrome and other genetic disorders: We create programs to build strength and improve balance for children who often have low muscle tone.
- Spina bifida: Therapy focuses on maximizing mobility and functional independence through gait training and other supports.
- Sports-related injuries: We help young athletes recover safely and learn how to prevent future injuries, understanding the unique needs of growing bodies.
- Post-concussion syndrome: Our vestibular therapy programs help relieve lingering symptoms like dizziness and balance problems.
For more information, visit our page on specialized kids physical therapy.
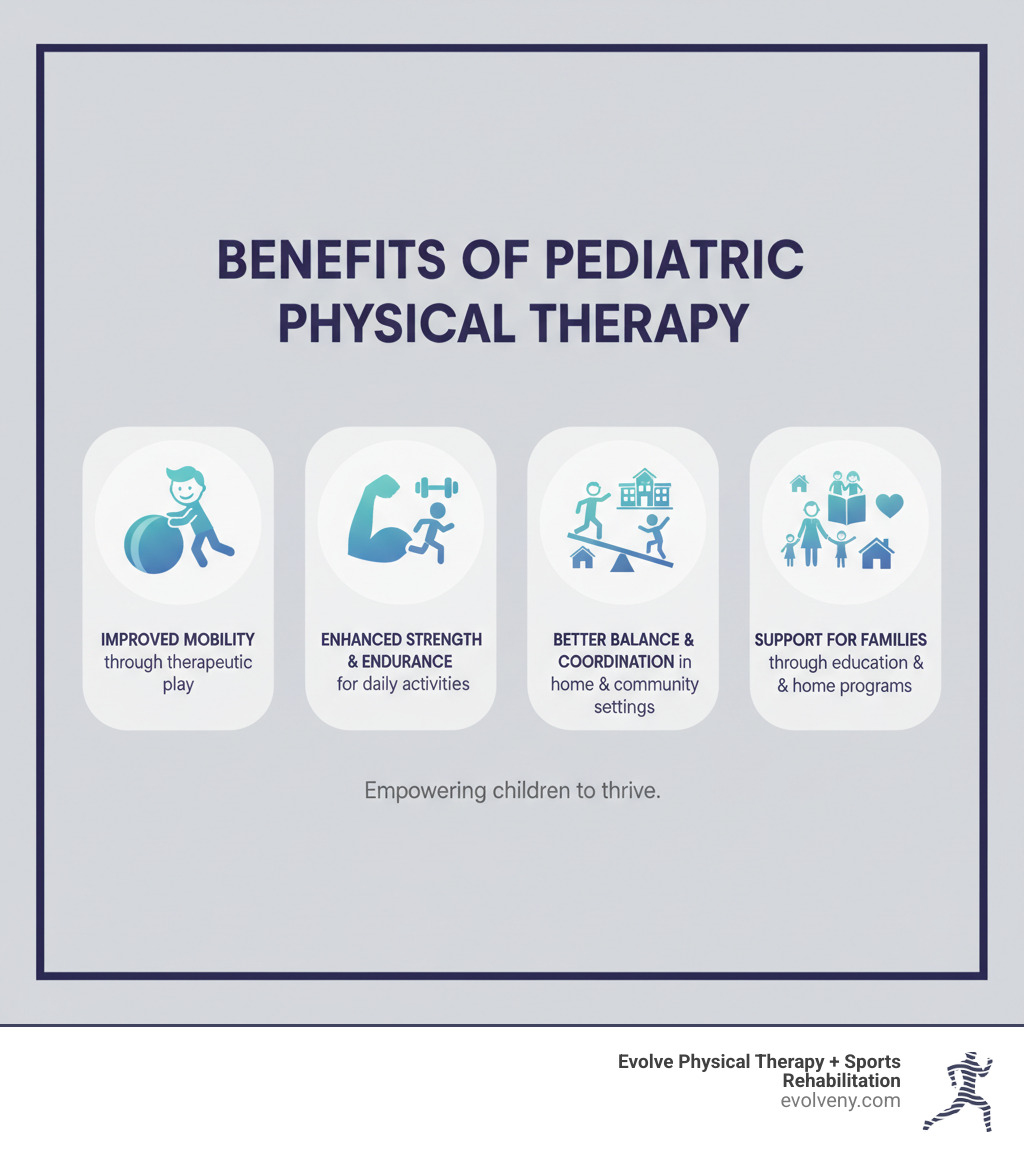
The Primary Goals and Lifelong Benefits
Our interventions aim to help children participate more fully in the activities that matter to them.
- Motor development: We help children acquire and refine the gross motor skills needed to move with confidence.
- Strength and endurance: Building stamina allows children to play longer and keep up with their friends.
- Balance and coordination: Improving these skills boosts confidence and safety in activities from walking to playing sports.
- Participation in home, school, and community: Our ultimate goal is to remove barriers so children can join in with siblings, classmates, and friends.
- Easing daily caregiving: Improved mobility can make daily tasks like dressing and bathing smoother for the whole family.
- Promoting health and fitness: We help children find the joy of movement and build healthy habits for life.
The skills and confidence children develop now shape their entire lives. For additional support, families can explore the Family Resources from APTA Pediatrics.
The Process and Interventions in Pediatric Physical Therapy
When you bring your child to Evolve Physical Therapy, our process is thorough, compassionate, and centered around your family. It begins with a comprehensive evaluation. We discuss your child's medical history, developmental milestones, and your specific concerns. You know your child best, and this conversation is crucial.
During the evaluation, we use careful observational movement analysis and standardized assessments to understand how your child moves and plays. We look for movement patterns and use objective measures to assess motor performance. We also check for any "red flags" that may require follow-up with your pediatrician. Your child's safety and comprehensive care are our top priorities.
From this evaluation, we create a customized treatment plan with specific, meaningful goals custom to your child's needs and your family's priorities. Our treatment blends hands-on care, therapeutic exercise, and functional activities.
We make therapy feel like play. Therapeutic exercise is woven into games and obstacle courses that motivate children to build balance, strength, and coordination. We also emphasize functional activities—the real-world skills your child needs every day, like navigating stairs or carrying a backpack. This ensures that progress in our clinic translates to greater independence at home and school.

The Crucial Role of Parents and Caregivers
You are an essential part of the therapy team. At Evolve Physical Therapy, we see parents as true partners. Your involvement is vital for your child's long-term success.
Our collaboration begins at the first evaluation, where we invite you to observe and ask questions. We provide a clear home exercise program, demonstrating each activity and explaining its purpose. We also guide you in adapting toys and daily routines to incorporate therapeutic benefits throughout the day. Finally, we support you in advocating for your child within the healthcare and education systems. When families and therapists work together, children thrive.
For more insights, explore More on our approach to pediatric physiotherapy.
Specialized Interventions in Pediatric Physical Therapy
Beyond foundational training, pediatric physical therapy offers specialized interventions. At Evolve, we use evidence-based approaches to address specific challenges.
- Aquatic therapy uses the buoyancy and resistance of water to build strength and coordination with less stress on joints, making it ideal for children who find land-based exercises difficult.
- Specialized exercise programs for scoliosis, such as the Schroth Method, use targeted exercises to improve spinal alignment and posture in children and adolescents.
- Serial casting can be a highly effective treatment for idiopathic toe walking. A series of casts is used to gradually stretch tight muscles and encourage a more typical walking pattern.
- Vestibular therapy is an exercise-based program that retrains the brain to process balance information correctly. It is highly effective for children with balance issues, dizziness, or post-concussion syndrome.
- We also assist families with orthotics and adaptive equipment like braces, walkers, or wheelchairs to provide support, improve alignment, and increase participation.
For young athletes, we offer specialized programs to treat and prevent injuries. Learn more at Pediatric sports PT for young athletes.
Where is Therapy Provided?
Pediatric physical therapy is offered in various settings. At Evolve Physical Therapy, we provide services in our welcoming outpatient clinics in Brooklyn, including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin. Other settings include:
- In-home therapy, which integrates interventions into a child's natural environment.
- School-based services, which are provided under the Individuals with Disabilities Education Act (IDEA) to help children access their education.
- Hospitals and NICUs, for medically fragile infants or children recovering from acute conditions.
- Community settings like preschools or recreational centers, to help children generalize their skills.
To learn more about our services, visit Learn about our pediatric physical therapy in Brooklyn.
Finding a Qualified Professional and Key Resources
Finding the right pediatric physical therapist is a crucial step. You want a professional who is not only skilled but also patient and invested in your child's success.
Professional Requirements
All licensed physical therapists (PTs) are graduates of accredited Doctor of Physical Therapy (DPT) programs and have passed a national licensure exam. This ensures they have the foundational skills to treat patients safely and effectively.
Many pediatric physical therapists pursue further specialization. The Board-Certified Pediatric Clinical Specialist (PCS) designation is a respected credential that requires extensive clinical experience with children and passing a challenging board exam. A therapist with a PCS has demonstrated advanced knowledge in the field.
At Evolve Physical Therapy, we are committed to evidence-informed practice. We integrate the latest research with our clinical expertise and your family's values to achieve the best outcomes for your child.
How to Find a Qualified Therapist
Navigating the healthcare system can be challenging. Here are a few tips:
- Start with your pediatrician. They can often recommend trusted local therapists. While New York has direct access (no referral needed to start), some insurance plans may still require one.
- Verify your insurance coverage. Our team at Evolve Physical Therapy can help you understand your benefits and any out-of-pocket costs to avoid surprises.
- Ask questions about their experience. Inquire about their background with children, their treatment philosophy, and how they engage kids in therapy. We welcome these conversations.
To search for therapists yourself, the American Physical Therapy Association (APTA) offers online tools like the Find a PT Directory. You can also search for specialists at Find a Board-Certified Pediatric Clinical Specialist.
The Role of APTA Pediatrics
APTA Pediatrics is an organization of nearly 6,000 members dedicated to advancing the field. It supports research, publishes clinical practice guidelines, and offers professional development for therapists. It also publishes the peer-reviewed Pediatric Physical Therapy journal.
For families, APTA Pediatrics provides reliable information. Their fact sheets explain various conditions and what to expect from therapy, empowering you to advocate for your child. We encourage you to Access APTA Pediatrics Fact Sheets to learn more.
Frequently Asked Questions about Pediatric PT
It's natural to have questions when starting pediatric physical therapy. Here are answers to some of the most common ones we hear from families in Brooklyn.
What is the difference between pediatric physical therapy and occupational therapy?
This is a common question. The key difference is the primary focus:
Pediatric physical therapy focuses on gross motor skills—the large movements of the body. We work on strength, balance, and coordination for activities like sitting, walking, running, and jumping.
Occupational therapy (OT) focuses on fine motor skills and the daily activities (or "occupations") of childhood. OTs help with skills like writing, buttoning a shirt, using utensils, and sensory processing.
Often, a child benefits from both. For example, a physical therapist helps a child gain the core strength to sit up, while an occupational therapist helps them use their hands to play while sitting. The two disciplines work together to provide comprehensive support.
How long will my child need physical therapy?
The duration of therapy is unique to each child and depends on several factors:
- Your child's diagnosis and its severity: A minor delay may resolve in a few months, while a complex condition like cerebral palsy may benefit from ongoing therapy over several years.
- Your child's response to treatment: Some children progress quickly, while others need more time and repetition.
- Your participation at home: Consistently practicing home exercises makes a significant difference and can speed up progress.
- Your family's goals: We work with you until your child achieves the meaningful goals you've set together.
We conduct regular re-evaluations to assess progress and adjust the plan, always with the goal of empowering you to maintain gains independently.
Is a physician's referral required to see a physical therapist?
In New York, you have direct access to physical therapy, meaning you can schedule an evaluation with us at Evolve Physical Therapy without a doctor's referral. This allows families to get help faster.
However, it's important to note that many insurance plans still require a physician's referral to cover the cost of therapy. We strongly recommend checking with your insurance provider, and our team is happy to help you verify your benefits.
Additionally, if our evaluation reveals anything that requires further medical assessment, we will refer you to a physician. We work as part of your child's total healthcare team.
Conclusion
Pediatric physical therapy is a transformative field dedicated to helping children build strength, confidence, and freedom of movement. From addressing developmental delays to recovering from sports injuries, the goal is to help children participate fully in life.
The benefits extend far beyond the clinic. When a child gains the ability to play with friends or master a new skill, they are building a foundation for a lifetime of health and joy. These are the victories, big and small, that drive us every day.
At Evolve Physical Therapy, our hands-on, holistic approach focuses on the whole child. We have been honored to serve families throughout Brooklyn, including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, for nearly two decades. We don't just treat symptoms; we empower families with the tools for long-term success.
If your child is struggling with movement or development, you don't have to steer this journey alone. Our experienced team is ready to partner with you.
Take the first step today. Schedule a consultation for pediatric physical therapy in Brooklyn and let us help your child move toward a brighter, more active future.
Connect and Thrive Discover Parkinson's Support Groups Near You
Why Finding the Right Parkinson's Support Group Matters

A Parkinson's support group connects you with people who understand your journey. These groups offer emotional support, practical advice, and a sense of community that can make living with Parkinson's disease (PD) less isolating.
Quick Guide to Finding a Parkinson's Support Group:
- Ask your healthcare team - Your neurologist, physical therapist, or local hospital can recommend groups
- Contact national organizations - Call the Parkinson's Foundation Helpline at 1-800-4PD-INFO (473-4636) or visit websites like the American Parkinson Disease Association
- Search online - Look for virtual support groups, forums, and community platforms
- Check local resources - Community centers, libraries, and hospitals often host in-person meetings
- Consider your specific needs - Groups exist for caregivers, young-onset PD, newly diagnosed, specific languages, and more
Many people find that support groups help them cope with the day-to-day realities of having Parkinson's disease. The opportunity to swap stories and share resources can be truly therapeutic. Whether you prefer in-person meetings or online forums, formal presentations or casual conversations, there's likely a group that fits your needs.
Support groups aren't just for people with PD. Care partners and family members also benefit from connecting with others who understand their challenges. Some groups welcome everyone affected by Parkinson's, while others focus on specific populations like women, veterans, or those living alone.
You might feel nervous about joining your first group. That's normal. If you don't like the first group you try, keep looking. The right fit makes all the difference.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, and I've worked with many individuals and families navigating Parkinson's disease. I know how valuable Parkinson's support groups can be as part of a comprehensive care plan that includes physical therapy, medical treatment, and community connection.

The Power of Connection: Why Join a Parkinson's Support Group?
Living with Parkinson's disease can present unique challenges, both physical and emotional. It's a journey that no one should have to walk alone. That's why Parkinson's support groups are so vital. They offer a unique blend of emotional well-being, practical advice, and a sense of belonging that can significantly improve quality of life for individuals with PD and their loved ones.
The opportunity to swap stories and share resources can be truly therapeutic. We've seen countless individuals experience reduced stress and a greater sense of connection simply by engaging with others who truly understand their experiences. This extends to care partners and family members, who also benefit immensely from sharing questions and concerns with like-minded others. Support groups help alleviate the feeling of isolation that can make life with Parkinson's more difficult, fostering an environment where understanding and empathy thrive.
Gaining Emotional and Mental Support
One of the most profound benefits of joining a Parkinson's support group is the emotional and mental reinforcement it provides. When you're navigating the complexities of PD, it's easy to feel frustrated or overwhelmed. Being part of a group means you're surrounded by individuals who "get it." This shared understanding is incredibly powerful, helping to alleviate the feeling of isolation that can often accompany a chronic illness.
In these groups, you can find a shoulder to cry on, share your worries, and express your frustrations without judgment. This peer-to-peer encouragement helps build resilience and fosters a sense of hope. You'll likely form new friendships with people who genuinely care about your well-being, creating a vital social network that supports your mental health. This connection reminds us that we are not alone in our struggles, and that there is strength in community.
Sharing Practical Knowledge and Resources
Beyond emotional support, Parkinson's support groups are a treasure trove of practical knowledge. Members often exchange invaluable tips for daily living, offering creative solutions for managing symptoms, navigating medication schedules, and adapting to new routines. Think of it as a living library of experience!
You can learn about different treatment experiences, compare notes on the effectiveness of various therapies, and find local specialists or resources that you might not have found otherwise. This collective wisdom helps individuals and care partners steer the often-complex healthcare system more effectively. From recommendations for adaptive equipment to insights on managing non-motor symptoms, the practical advice shared in these groups can be a game-changer. For more detailed information on available resources, we encourage you to explore More info about what support is available for Parkinson's disease.
Finding Your Fit: Types of Parkinson's Support Groups Available
Just like Parkinson's disease affects each person differently, the ideal support group experience can vary widely. Fortunately, there's a diverse array of Parkinson's support groups designed to meet different preferences and needs. Whether you're looking for face-to-face interaction, the convenience of online forums, or a group custom to specific demographics, options are available.

In-Person vs. Online Groups
The choice between in-person and online groups often comes down to personal preference, location, and accessibility.
In-person meetings offer direct, face-to-face interaction. These local gatherings provide a strong sense of connection, allowing for nuanced communication and shared activities. For those in Brooklyn and surrounding areas like Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, local chapters of national organizations or community centers often host such meetings.
Online groups provide incredible flexibility and accessibility. They include virtual video calls for real-time communication and online forums where you can post and read messages at your own pace. They are great for those with busy schedules, in remote areas, or who prefer anonymity.
Here are some popular online support platforms:
- Parkinson's Buddy Network: From the Michael J. Fox Foundation, this network helps you connect with others, find resources, and build relationships, with software to match members by interests.
- Mayo Clinic Parkinson's Disease forum: A moderated forum with over 2,000 members where Mayo Clinic staff help answer questions.
- PD Conversations: Moderated groups from the Parkinson's Foundation on various topics, including options in Spanish. Helpline staff answer questions.
- HealthOpen uped (Cure Parkinson's community): An unmoderated community with over 21,000 members, run with Parkinson's Movement (UK) and the EPDA, covering many PD topics.
- Parkinson's UK Forum: A moderated forum with sections for daily life, treatments, caregivers, and more.
- PatientsLikeMe Forum: An unmoderated forum with over 20,000 PD members where posts can be tagged and searched.
- Smart Patients Parkinson's Disease Community: A moderated community run in partnership with the American Parkinson Disease Association (APDA).
- NeuroTalk and Caring.com: Both host robust Parkinson's disease communities.
- Facebook groups: A popular option for conversation. Ask your doctor for recommendations or search for groups to join.
A Parkinson's Support Group for Every Need
The beauty of the Parkinson's support group landscape is its diversity. Groups cater to a wide array of specific needs and demographics, ensuring that nearly everyone can find a community where they feel truly understood.
- Caregiver groups: These are crucial for spouses, partners, adult children, and friends who provide care. We know that caregiving can be incredibly demanding, and these groups offer a space to share challenges, coping strategies, and prevent burnout. There are groups for caregivers of those in early to mid-stage PD, as well as those caring for individuals in advanced stages, or even bereavement groups for care partners dealing with loss and grief. We offer more resources for caregivers, including Parkinson's Caregivers Support Groups.
- Young-Onset PD (YOPD) groups: For individuals diagnosed with Parkinson's before age 50, YOPD presents unique challenges. These groups connect younger individuals who may be balancing careers, raising families, and navigating symptoms that differ from later-onset PD. Groups like "YOPD Connections" or "YOPN Monthly Member Community Gathering" offer vital peer support.
- Women-only and men-only groups: Some individuals prefer to connect with others of the same gender to discuss experiences that might be gender-specific. Virtual Women's Parkinson's Support Groups and Men with Parkinson's groups provide these custom environments.
- Newly diagnosed groups: Receiving a PD diagnosis can be overwhelming. These groups offer a safe space for individuals to process their emotions, ask basic questions, and connect with others who are just beginning their journey.
- Advanced stages groups: As PD progresses, new challenges arise. Groups for advanced stages provide support and information relevant to more complex symptoms and care needs.
- Ethnic-specific and language-specific groups: Recognizing the importance of cultural and linguistic comfort, some organizations offer groups custom to specific ethnic backgrounds, or in languages such as Spanish, French, Cantonese, and Mandarin. This ensures that support is accessible to diverse communities.
- Specialized groups: You can also find groups for specific situations, such as:
- DBS recipients: For those who have undergone Deep Brain Stimulation surgery, these groups offer a forum to discuss post-surgical experiences and adjustments.
- "Flying Solo" or "Living Solo" groups: For individuals with PD who are single, divorced, or living alone, offering camaraderie and practical advice.
- Adult children caregivers: Dedicated spaces for adult children whose parents have PD or another movement disorder, recognizing their unique role and challenges.
- Grief support: Groups like "PRO Grief Group" or "Bereavement Support Group for Carepartners" help individuals process loss related to PD.
- Teen support: "Just for Teens" or "Teen Talk" groups offer a safe space for teenagers whose parents or family members have YOPD.
Moderated vs. Unmoderated Online Communities
When exploring online Parkinson's support groups, you'll encounter both moderated and unmoderated communities. Understanding the difference is key to finding the right fit.
- Moderated forums are overseen by administrators or trained volunteers. Posts are reviewed to ensure they are respectful and adhere to community guidelines, and that information is generally reliable. Examples include the forums from the Mayo Clinic and the Parkinson's Foundation. These groups are more structured, provide a safer environment, and are excellent for getting reliable information.
- Unmoderated forums allow members to post freely without review, fostering open discussion. Platforms like HealthOpen uped and PatientsLikeMe are examples. While this allows for a rich exchange of personal stories, the information shared may not be medically accurate. Always consult your healthcare professional about any medical advice found in these groups.
When choosing between the two, consider your priorities: Do you prefer a highly structured, professionally guided environment with vetted information, or do you value a more free-flowing, peer-driven discussion? For reliable information, moderated groups are generally preferable. For broad, diverse personal experiences, unmoderated groups can be valuable, but always cross-reference critical information with your medical team.
How to Find a Parkinson's Support Group
Finding the right Parkinson's support group is a crucial step towards building a robust support network. Whether you're seeking local in-person meetings or online connections, there are several avenues to explore.

Using National and Local Resources
National organizations are often the first and best place to start your search. They typically have vast networks and comprehensive directories:
- The Parkinson's Foundation: This organization provides people with PD and caregivers access to local resources and services through its Chapter network. They offer a toll-free Helpline at 1-800-4PD-INFO (473-4636) for information and referrals. You can search their website by state to find local support groups, health and wellness classes, and education programs.
- The American Parkinson Disease Association (APDA): APDA works tirelessly to support and empower anyone impacted by PD. Their nationwide network provides connection and community, along with information, referrals, education, support programs, and health and wellness activities. Their website also allows you to find local resources by entering your state or zip code. For those in New York City, APDA specifically lists local support groups.
- The Michael J. Fox Foundation: While primarily focused on research, they also offer the Parkinson's Buddy Network, an online community for connection and support.
Beyond these national bodies, don't overlook local community resources in areas like Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin:
- Community Centers and Libraries: Check their calendars or bulletin boards for local support group listings.
- Local Hospitals: Many hospitals offer community outreach programs or host support groups for various conditions, including Parkinson's.
- Online Search Directories: Websites of national or local Parkinson's disease organizations often have online support group resources.
For support resources specifically custom to our community, please visit Find Support Resources | Evolve Physical Therapy.
Asking Your Healthcare Team
Your healthcare team is an invaluable resource for finding a suitable Parkinson's support group. They often have direct knowledge of local groups and can provide recommendations based on your specific needs and situation.
- Neurologist Recommendations: Your neurologist is typically well-connected with the local Parkinson's community and can often recommend specific groups they know to be beneficial. They might even be guest speakers at some of these groups.
- Physical Therapist Suggestions: As physical therapists, we work closely with individuals with PD and their families. We understand the physical and emotional challenges you face and can suggest groups that align with your therapeutic goals and personality. At Evolve Physical Therapy, we are deeply involved in the Brooklyn Parkinson's community and can guide you toward relevant local resources. For more information on how we support individuals with PD, check out More info about physical therapy for Parkinson's.
- Hospital Outreach Programs: Many hospitals have social workers or patient navigators who can connect you with support groups and other community services.
- Social Worker Referrals: Social workers specializing in chronic illness are excellent resources for identifying support networks.
Don't hesitate to ask your doctors, therapists, or other healthcare providers. They are often your best local guides.
Starting Your Own Support Group
What if you've searched diligently and still can't find a Parkinson's support group that perfectly fits your needs in your area, or perhaps you feel a specific demographic is underserved? Don't despair! You're likely not alone, and starting your own group can be an incredibly rewarding endeavor. We've seen the power of community, and sometimes, it just needs a spark.
Here are some tips for starting a new support group:
- Identify a Need and Target Audience: Consider who you want to serve. Is it people with PD, their care partners, young-onset PD individuals, or perhaps a group focused on a specific challenge? Defining your audience will help attract the right members.
- Find a Suitable Location: Choose a private, accessible space. Community centers, local libraries, churches, or even private rooms in medical facilities are often good options. Avoid overly public spaces like coffee shops where privacy might be an issue. In Brooklyn, there are many community venues that could host such a group.
- Determine Meeting Time and Frequency: Decide how often and when your group will meet. Consider what days and times might work best for your target audience (e.g., weekday mornings for retirees, evenings for working care partners).
- Set a Format: Will it be an informal chat, a facilitated discussion with rotating hosts, or will you invite guest speakers? Many groups find a mix works well, allowing for open discussion alongside informative presentations.
- Invite Guest Speakers: Enlisting healthcare professionals can add immense value. Think about inviting neurologists, physical therapists (like us!), occupational therapists, speech-language pathologists, or even exercise group leaders to share their expertise.
- Promote the Group: Spread the word! Create simple flyers and post them in doctor's offices, hospitals, libraries, community centers, and senior centers in Brooklyn and surrounding neighborhoods. Use online platforms like local Facebook groups or create a basic website to announce meetings and communicate with members.
- Share Resources: At each meeting, consider having takeaway resources such as handouts, lists of helpful websites, or contact information for local services.
- Consider Inviting Care Partners: Even if the primary focus is on individuals with PD, inviting care partners and family members can broaden the support network and provide a holistic approach.
Starting a group might seem daunting, but the impact you can have on your community is immense. For more in-depth guidance, explore More info about how to form a support group for Parkinson's.
Frequently Asked Questions about Parkinson's Support Groups
We understand you might have more questions about joining a Parkinson's support group. Here are some common inquiries we hear, along with our insights.
Are Parkinson's support groups free to join?
Generally, most Parkinson's support groups are free to join. Many are volunteer-led and operate on a community-driven model, aiming to provide accessible support to everyone in need. National organizations like the Parkinson's Foundation and the American Parkinson Disease Association (APDA) typically offer their group listings and helpline services without charge.
However, there can be exceptions:
- Donation-based groups: Some groups might accept voluntary donations to cover operational costs, such as room rentals or refreshments.
- Professionally facilitated groups: If a group is led by a paid professional, such as a social worker, therapist, or specialized healthcare provider, there might be a fee per session or a membership cost. For example, some specialized mindfulness groups might charge a small fee. Always check with the specific group organizer regarding any associated costs.
- Online platforms: While reading posts on many online forums is free, some platforms may require membership to actively post questions or comments.
Our advice is always to confirm with the group organizer or check their website if you're unsure about any fees.
What happens at a typical support group meeting?
The structure of a Parkinson's support group meeting can vary, but most share common elements designed to foster connection and provide value.
- Introductions and Check-ins: Meetings often begin with members introducing themselves (if new) and briefly sharing how they're doing or any recent experiences they wish to highlight.
- Sharing Personal Experiences: This is often the core of the meeting. Members take turns sharing their challenges, successes, and insights related to living with PD or being a care partner. This open discussion allows for mutual support and validation.
- Open Discussion: Topics can arise organically from members' shares, or a facilitator might introduce a theme for discussion. This could range from managing specific symptoms to navigating social situations or dealing with emotional impacts.
- Guest Speakers: Many groups regularly invite guest speakers. These might be neurologists, physical therapists (like us at Evolve Physical Therapy), occupational therapists, speech-language pathologists, dietitians, or other allied healthcare professionals. They provide educational presentations on topics relevant to PD management, research updates, or coping strategies.
- Educational Presentations: Sometimes, meetings might involve watching an informative video or discussing articles related to Parkinson's.
- Social Activities: Beyond formal discussions, many groups incorporate social time, allowing members to chat informally, build friendships, and enjoy a sense of community. Some local groups even organize social events and activities outside of regular meetings.
For instance, some groups might start with a lighthearted activity, like a clean comedian to get everyone laughing, followed by an informative video and then open discussion and Q&A. Regardless of the specific format, the goal is always to create a supportive and informative environment.
How do I know if a support group is right for me?
Finding the right Parkinson's support group is a personal journey, and it's perfectly normal if the first one you try isn't the perfect fit. Here's how you can determine if a group is right for you:
- Try a Few Different Groups: Don't feel obligated to stick with the first group you attend. We recommend trying a few different options – perhaps an in-person meeting, an online video call, and an online forum – to see which format and dynamic resonate most with you.
- Consider the Format: Do you prefer a formal, structured meeting with a clear agenda and guest speakers, or a more informal, free-flowing conversation? Some groups are professionally facilitated, while others are peer-led. Think about what kind of interaction makes you feel most comfortable and engaged.
- Group Size and Demographics: Some individuals thrive in larger groups, while others prefer a more intimate setting. Also, consider the group's specific focus – if you're a care partner, a group specifically for caregivers might be more beneficial than a general PD group. Similarly, if you have Young-Onset PD, connecting with peers facing similar life stages can be invaluable.
- Observe the Atmosphere: Does the group feel welcoming and empathetic? Do members listen to each other respectfully? Is there a balance between sharing challenges and offering constructive support or hope? A supportive and safe environment is paramount.
- Your Personal Comfort Level: The right group is one where you feel understood, respected, and comfortable sharing your experiences. If you feel heard and supported, and leave feeling more positive or informed, you're likely in a good place.
There's no pressure to force it if a group doesn't appeal to you. The goal is to find a community that genuinely improves your well-being.
Conclusion: Take the Next Step in Your Support Journey
Navigating life with Parkinson's disease, whether you have a diagnosis or are a dedicated care partner, is a journey best shared. Parkinson's support groups offer an unparalleled opportunity for connection, understanding, and empowerment. From gaining vital emotional support to sharing practical knowledge and finding a community that truly "gets it," these groups are an indispensable part of a holistic care plan.
We, at Evolve Physical Therapy, believe firmly in the power of a comprehensive approach to managing Parkinson's. This includes not just expert physical therapy, but also robust community engagement and physical activity. Our Rock Steady Boxing program, for instance, which has been featured on NBC News, is a fantastic example of how we combine dynamic physical exercise with the camaraderie and support of a group setting right here in Brooklyn. It’s about fighting back against PD in every way possible.
Don't underestimate the profound impact that connecting with others can have on your well-being. Take that next step today. Explore the various types of Parkinson's support groups available, whether in-person in Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin, or through the many online communities. Ask your healthcare team for recommendations, or even consider starting a group if you see a need in your community.
We are here to support you in every way we can. For more information on how our specialized physical therapy services can complement your Parkinson's care plan, please visit More info about Parkinson's physical therapy in Brooklyn. Your journey is unique, but you don't have to walk it alone. Connect, share, and thrive!
Playful Paths to Progress: Expert Physical Therapy for Children
Introduction: The First Steps to a Brighter Future

Physical therapy for kids helps children develop or regain the skills they need to move their bodies, build strength, improve coordination, and participate fully in daily activities at home, school, and in their communities.
Quick Overview: What Physical Therapy for Kids Offers
- Improves Mobility: Helps children crawl, walk, run, and move with confidence
- Builds Strength: Develops muscle strength and endurance through play-based exercises
- Improves Coordination: Addresses balance, motor planning, and body awareness
- Supports Development: Assists children in reaching age-appropriate milestones
- Boosts Confidence: Empowers kids to participate in activities they enjoy
- Prevents Injury: Teaches safe movement patterns and proper body mechanics
Children are not just small adults. They require specialized therapeutic intervention within the context of their development. Whether your child has experienced an injury, is managing a developmental delay, or lives with a physical condition like cerebral palsy or torticollis, the right therapy program can make a world of difference.
Pediatric physical therapy uses play, exercise, and hands-on techniques to help children reach their full potential. Therapists work with conditions ranging from torticollis in infants (ideally starting before 3 months of age for best results) to sports injuries in teens and developmental coordination disorder in school-aged children.
More than 180,000 children and youth with special needs receive these services every year. The goal is always the same: to equip children and families with the knowledge and skills to manage daily challenges and thrive independently.
As Lou Ezrick, founder of Evolve Physical Therapy, I've dedicated nearly two decades to helping patients overcome movement challenges. My team and I use specialized, hands-on approaches to address each child's unique developmental needs, because we believe every child deserves to move with joy and confidence.

Why is pediatric physical therapy for kids so important?
Movement is more than just play for children; it's fundamental to their development, confidence, and independence. In our Brooklyn clinics, we see how physical therapy for kids helps children develop strength, balance, and coordination. It improves posture and mobility, prevents injury, and manages chronic conditions.
At Evolve Physical Therapy, we know children thrive when they can move freely. Our pediatric physical therapists are experts in movement and motor development, assessing a child's flexibility, strength, and gait compared to their peers. This specialized care is essential, as movement problems can limit a child's ability to learn, play, and interact with the world.
The benefits extend beyond physical improvements:
- Gross Motor Skills: We help children master the large muscle movements needed for activities like crawling, walking, running, and jumping.
- Developmental Milestones: We guide infants and children through age-appropriate milestones, helping them build foundational skills for future learning and independence.
- Injury Prevention: For active kids and young athletes in Brooklyn, we teach safe movement patterns and proper body mechanics to help prevent future injuries.
- Functional Independence: Our goal is to empower children to perform daily tasks as independently as possible, from dressing themselves to navigating their school environment.
- Quality of Life: By improving physical function and confidence, we can significantly improve a child's overall quality of life.
We work alongside families, other healthcare professionals, and school personnel to ensure a comprehensive approach. Our aim is to provide children and their families with the knowledge and skills they need to manage challenges and achieve their maximum potential.
Learn About Pediatric Physical Therapy at Evolve Physical Therapy
Signs Your Child Might Need Physical Therapy & Conditions We Address
While an injury is a clear sign a child needs help with movement, other indicators can be more subtle. As a parent, you're often the first to notice if your child is struggling. Here are common signs your child might benefit from physical therapy for kids:
- Developmental Delays: If your child is falling behind on milestones like rolling, sitting up, crawling, or walking.
- Not Meeting Milestones: Every child develops at their own pace, but significant delays in physical milestones should be assessed.
- Clumsiness or Poor Balance: Frequent tripping, falling, or difficulty with coordination, especially for school-aged children, can be a sign of Developmental Coordination Disorder (DCD). This neurodevelopmental disorder affects about 5-6% of school-aged children and is more common in boys. Children with DCD might struggle with activities like riding a bike, handwriting, or participating in sports.
- Posture Issues: Concerns about your child's posture, such as a persistent head tilt or uneven shoulders.
- Injury Recovery: If your child has sustained a sports injury, orthopedic injury, or acute trauma.
- Post-Surgical Rehabilitation: Physical therapy can be important for regaining strength and movement after surgery.
Pediatric physical therapy is proactive, not just reactive. Early intervention can make a significant difference in a child's long-term outcomes.
How Pediatric Sports Physical Therapy Helps Kids Succeed
Common Pediatric Conditions
At Evolve Physical Therapy in Brooklyn, we address a wide range of pediatric conditions, helping children from infancy through adolescence.

- Torticollis & Plagiocephaly (Flat Head Syndrome): Torticollis is a condition where an infant's neck muscles cause their head to tilt persistently to one side. This can often lead to plagiocephaly, or a flat spot on the head, due to sustained positioning. Early intervention for torticollis, ideally before 3 months of age, can lead to better results and fewer therapy sessions. Our therapists help improve neck muscle symmetry and strength, guiding infants to achieve developmental milestones on time.
- Cerebral Palsy: This neurological disorder affects movement and muscle coordination. We work with children with cerebral palsy to improve mobility, strength, and functional independence, sometimes utilizing advanced techniques like gait training.
- Developmental Coordination Disorder (DCD): As mentioned, DCD affects many school-aged children, causing difficulties with motor skills, coordination, and balance. Our therapy focuses on improving motor performance and participation.
- Autism Spectrum Disorder: Children with Autism may experience mobility issues or unique movement patterns. Our therapists provide custom interventions to address these challenges.
- Genetic Disorders (e.g., Down Syndrome): Many genetic conditions can impact a child's physical development. We provide supportive therapy to help children with genetic disorders participate more fully in life.
- Musculoskeletal Injuries: From sprains and strains to fractures, children can experience a variety of musculoskeletal injuries. Our physical therapy helps restore strength, range of motion, and function.
- Sports Injuries: Young athletes, especially in active communities like Brooklyn, are susceptible to sports-related injuries. We provide specialized therapy for recovery, injury prevention, and safe return-to-sport protocols. This can include addressing issues like concussions (through vestibular therapy) and other acute traumas that may affect balance and coordination.
- Effects of Prenatal Drug/Alcohol Exposure: Children affected by prenatal exposure to drugs or alcohol may experience developmental delays that can benefit from early physical therapy intervention.
We also address conditions such as idiopathic toe walking and various heart and lung conditions where physiotherapy can improve cardiorespiratory endurance. Our goal is to provide comprehensive, individualized care for each child's unique needs.
The Pediatric Physical Therapy Journey: From Referral to Results
Starting physical therapy for kids can feel like a big step, but at Evolve Physical Therapy in Brooklyn, we make the process as smooth and supportive as possible. We're here to guide you and your child every step of the way, from the initial consultation to celebrating their progress.
Referral Process and Direct Access in New York
One common question we hear is about referrals. In New York State, you have what's known as "direct access" to physical therapy services. This means that in many cases, you don't need a physician's referral to begin physical therapy. Licensed physical therapists with at least three years of experience can treat patients for up to 30 days or 10 appointments without a referral.
However, some specialized pediatric programs or certain insurance plans may still require a physician's referral. If you have any questions about whether your child needs a referral, we encourage you to contact us directly. If, after 30 days, your child hasn't made significant improvement, we'll recommend a consultation with their physician to ensure they receive the most appropriate care.
Initial Evaluation: Understanding Your Child's Unique Needs
The journey begins with an initial evaluation. During this visit, we will:
- Discuss Medical History: We'll talk about your child's developmental milestones, any previous injuries or conditions, and their overall health.
- Assess Strength and Flexibility: Our therapists will carefully measure your child's muscle strength, range of motion, and flexibility.
- Perform Gait Analysis: We'll observe how your child walks and runs to identify any patterns or imbalances that might be affecting their movement.
- Conduct Motor Tests: We use specialized tests to assess your child's motor skills, balance, and coordination.
- Listen to Your Concerns: Your input as a parent is invaluable. We want to understand your primary concerns, your child's daily activities, and what you hope to achieve through therapy.
Goal Setting and Family Collaboration
A key part of the initial evaluation is collaborative goal setting. We believe that therapy is most effective when it's child-centered and family-driven. We'll work with you and your child to set short-term and long-term functional goals that are meaningful to your family.
Parents and families play the primary role in their child's development. Our pediatric physical therapists collaborate closely with you to promote development and implement an individualized intervention program. We support families through education, hands-on instruction, and coordination of services, recognizing you as advocates and decision-makers in your child's care.
Pediatric Physical Therapy at Evolve Physical Therapy
What to expect during a physical therapy for kids session
Once the evaluation is complete and goals are set, your child will begin their regular therapy sessions. At Evolve Physical Therapy, we pride ourselves on a one-on-one approach, ensuring your child receives our therapist's attention and expertise.

- One-on-One Sessions: You will be evaluated and treated by a licensed physical therapist, ensuring continuity of care throughout your child's journey with us.
- Play-Based Activities: We know that for kids, movement is best learned through play. Our sessions are designed to be fun and engaging, incorporating games, creativity, and positive reinforcement.
- Typical Session Length: Most of our physical therapy for kids sessions typically last around an hour, though this can vary slightly depending on your child's needs.
- Regular Progress Reviews: Your child's progress will be reviewed regularly, often every three months, to ensure we're on track to meet their goals. We'll adjust the treatment plan as needed.
- Home Exercise Programs: We'll provide you with a customized home exercise program, with suggestions for integrating exercises into your child's daily routine.
- Therapy Settings: While our primary services are provided in our Brooklyn clinics, some children may also receive therapy in natural learning environments like schools or at home. We also offer virtual telehealth options for certain situations.
Making Movement Fun: Common Approaches in Physical Therapy for Kids
The magic of physical therapy for kids lies in changing therapeutic exercises into exciting adventures. We leverage a variety of approaches to keep children engaged, motivated, and making progress toward their goals.
- Therapeutic Play: This is at the heart of our approach. We use play activities to build strength, improve balance and coordination, and develop motor skills.
- Task-Oriented Intervention: This approach focuses on practicing specific functional tasks that are challenging for your child. If the goal is to ride a bike, we'll break down the task into smaller steps and practice each one.
- Strength Training: Building strong muscles is crucial for stability and movement. We incorporate age-appropriate strength exercises, often disguised as games or "superhero training" using resistance bands or light weights.
- Balance and Coordination Activities: From walking on a low balance beam to navigating obstacle courses, we design activities that challenge your child's balance and coordination.
- Gait Training: For children with difficulties in walking or running, we focus on gait training to improve their walking pattern, efficiency, and safety.
- Adaptive Equipment: Sometimes, children benefit from adaptive equipment to support their movement or participation. This might include orthotics, specialized seating, or mobility aids, which we can assess and help coordinate.
Pediatric Physical Therapy Resources
List of Fun and Effective Exercises
Here are some examples of the playful exercises we use in our clinics to help children develop strength, coordination, and confidence:
- Animal Walks: Kids love pretending to be animals, and these exercises are useful for building full-body strength, coordination, and flexibility.
- Obstacle Courses: We turn our therapy space into an adventure zone with crawling, hopping, and climbing activities.
- Therapy Ball Exercises: Large therapy balls are versatile for improving core strength and postural control.
- Yoga Poses for Kids: Simple yoga poses like "Tree Pose" or "Downward Dog" help build flexibility, balance, focus, and strength.
- Resistance Band Games: We make strengthening fun with resistance bands, using playful arm and leg exercises.
- Balance Beam Walking: Whether it's a low balance beam or a line taped on the floor, walking heel-to-toe helps children improve their balance and body awareness.
Your Role as a Partner in Progress: Supporting Therapy at Home
At Evolve Physical Therapy, we firmly believe in a family-centered approach. Your involvement as a parent or caregiver is important to your child's success in physical therapy for kids. You are your child's primary advocate and decision-maker, and we consider you a vital part of our team.
- Family-Centered Care: We prioritize your family's values, routines, and goals. Our therapists work collaboratively with you to ensure the therapy plan fits into your family's life in Brooklyn.
- Home Exercise Program Consistency: The progress your child makes in our clinic sessions is significantly boosted by consistent practice at home. We'll provide you with a clear, easy-to-follow home exercise program. Integrate exercises into playtime or daily routines to make them feel natural.
- Adapting Toys and Activities: We can show you simple ways to adapt your child's favorite toys and activities to support their therapeutic goals.
- Creating a Supportive Environment: A supportive home environment encourages movement, exploration, and safety. We can offer guidance on setting up your home to facilitate your child's independence.
- Communication with Your Therapist: Please share any observations about your child's progress, challenges, or discomfort during exercises. This feedback helps us adjust the treatment plan.
- Collaboration with Schools (IEPs): For school-aged children, we can collaborate with school personnel, especially regarding Individual Education Plans (IEPs). This supports their participation and success in school.
- Coordination with Other Healthcare Professionals: We often work as part of a larger interprofessional team, coordinating care with your child's pediatrician and other specialists.
By actively participating in your child's therapy journey, you help them overcome challenges and build skills that can last a lifetime.
Frequently Asked Questions about Pediatric Physical Therapy
We understand that parents often have many questions when considering physical therapy for kids. Here are some of the most common inquiries we receive at Evolve Physical Therapy:
How long will my child need physical therapy?
The duration of physical therapy for kids is highly individualized and depends on several factors, including your child's specific diagnosis, the severity of their condition, their medical history, and their response to treatment.
- Short-Term Goals: Therapy programs are designed with short-term, clearly identified functional goals. Once these are met, the need for continued therapy is re-evaluated.
- Varies by Condition: A child recovering from a sports injury might need therapy for a few weeks or months, while a child with a chronic condition like cerebral palsy might benefit from ongoing, periodic support.
- Regular Re-assessment: We regularly assess your child's progress, typically every three months, to determine if they are meeting their goals and if continued therapy is necessary.
- Intensive vs. Periodic Therapy: Therapy frequency can vary. Some children with acute needs might benefit from "intensive therapy" (three visits weekly). Others may require fewer visits to learn new exercises and establish a home program.
- Focus on Functional Independence: Our ultimate goal is to provide your child with the knowledge and skills to manage daily challenges as independently as possible, even after formal therapy ends.
What is the difference between physical therapy (PT) and occupational therapy (OT)?
While both physical therapy and occupational therapy are important for a child's development and often work collaboratively, they focus on different aspects of function:
- Physical Therapy (PT) Focus: Our pediatric physical therapists at Evolve Physical Therapy primarily focus on a child's gross motor skills, mobility, strength, balance, and coordination. We work to restore, maintain, and optimize how a child moves their body.
- Occupational Therapy (OT) Focus: Occupational therapists help children improve their participation in day-to-day activities. Their focus is often on fine motor skills, visual motor skills, sensory processing, self-regulation, and activities of daily living (ADLs) such as dressing, feeding, and hygiene.
Often, children benefit from a collaborative approach where a PT and OT work together, supporting both gross motor development and functional independence in daily life.
How do I find a qualified pediatric physical therapist?
Finding the right pediatric physical therapist is important for your child's success. Here are some steps you can take:
- Doctor Recommendations: Start by asking your child's pediatrician or family doctor for recommendations.
- Insurance Provider Lists: Contact your medical insurance provider for a list of physical therapists covered under your plan in Brooklyn.
- Specialized Training and Board-Certified Specialists: Look for therapists with specialized training or certifications in pediatric physical therapy. The American Physical Therapy Association (APTA) offers board certification in pediatrics, indicating advanced knowledge and skills.
- Online Directories: You can search online directories such as The American Physical Therapy Association's Find a PT tool to find qualified physical therapists in your area.
- Ask About Our Expertise: At Evolve Physical Therapy, we welcome your questions about our therapists' qualifications, experience, and approach to physical therapy for kids.
Find a Pediatric Physical Therapist at Evolve Physical Therapy
Conclusion: Empowering Your Child to Thrive
The journey of physical therapy for kids is one filled with dedication and joy. Pediatric physical therapy is not just about fixing problems; it's about opening up potential, building confidence, and empowering children to participate more fully in their lives. From helping infants achieve early developmental milestones to guiding young athletes back to their sport, the benefits can be far-reaching.
We believe that every child deserves the opportunity to move with joy and confidence. Our playful, family-centered approach aims to make therapy both effective and engaging for your child. By collaborating closely with you, we help your child build skills that support independence and a love for movement.
At Evolve Physical Therapy in Brooklyn, we are committed to providing expert, compassionate care that sees your child not just as a patient, but as a unique individual ready to thrive. If you've noticed your child struggling with movement, coordination, or developmental milestones, don't hesitate to reach out.
Take the next step in your child's development journey with our expert physical therapy services.
The Ultimate List of Mobility Movements for a Flexible You
Why Mobility Movements Are Essential for Your Body

Mobility movements are exercises that help your joints move freely through their full range of motion with control and strength. They are your foundation for reducing stiffness, preventing injuries, and moving better in daily life.
Quick Answer: What Are Mobility Movements?
Mobility movements are dynamic exercises that improve:
- Joint range of motion - How far your joints can move in all directions
- Motor control - Your ability to actively control movement through that range
- Functional movement quality - How well you perform everyday activities
- Injury prevention - By addressing restrictions before they cause problems
- Pain reduction - Especially in areas like hips, shoulders, and spine
Think of mobility as the difference between being able to reach your toes (flexibility) versus being able to control your body as you squat down to pick something up (mobility). While stretching helps muscles lengthen passively, mobility work trains your joints and muscles to move actively with strength and stability through their full range.
Research shows the impact is real: subjects who scored higher on a mobility screening test were six times less likely to get injured. As we age, maintaining mobility is critical. Joints can become less lubricated, cartilage may thin, and tendons less elastic, all leading to stiffness and reduced movement quality.
Whether you wake up stiff, want to improve athletic performance, or maintain independence as you age, mobility training offers a solution. It's not just about touching your toes—it's about moving through life with freedom, confidence, and less pain.
I'm Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, and over nearly two decades, I've helped thousands of patients improve their quality of life through targeted mobility movements and manual therapy techniques. From treating chronic pain to optimizing athletic performance, I've seen how the right mobility work transforms how people move and feel.
What is Mobility and Why Does It Matter?
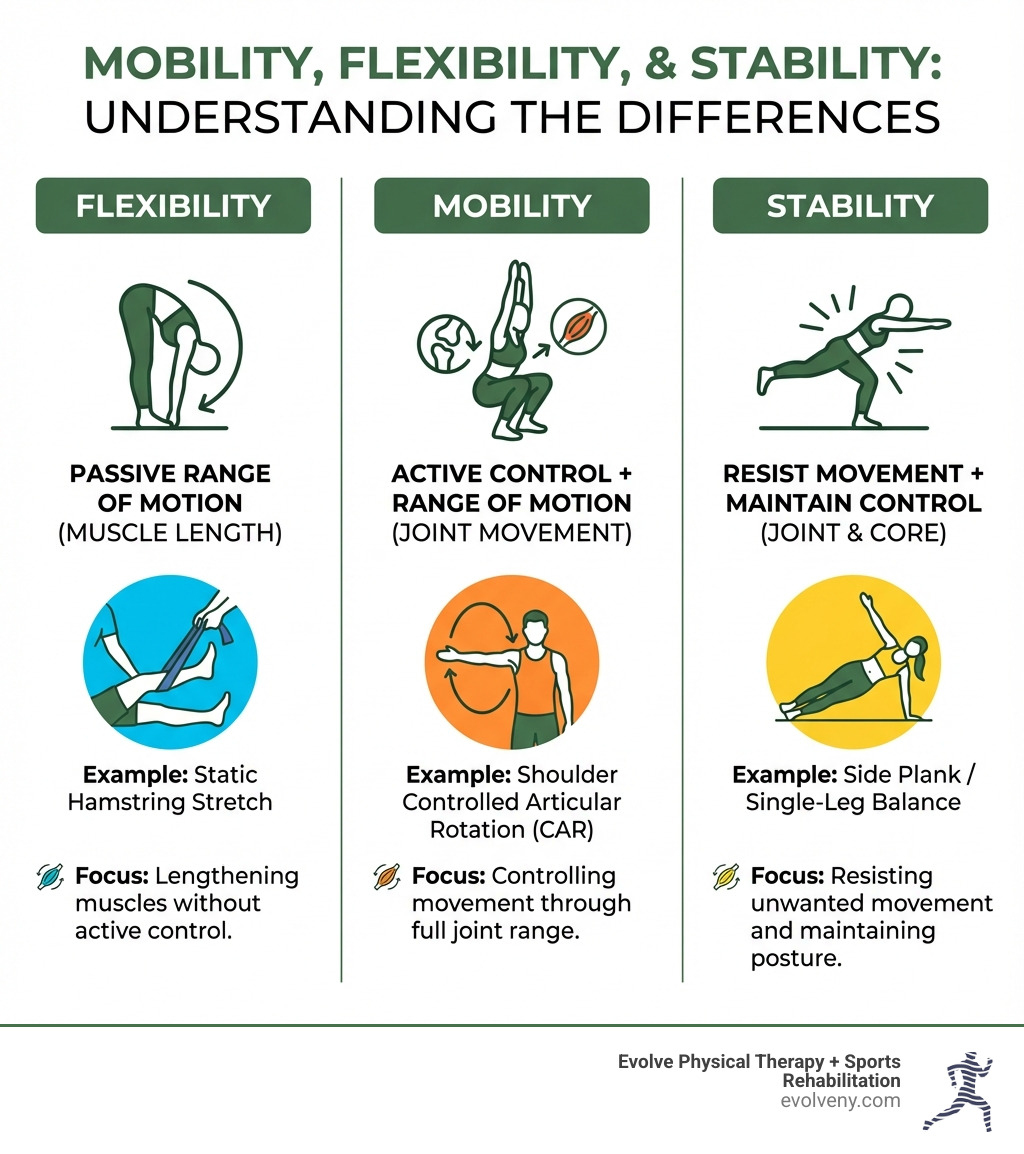
At Evolve Physical Therapy + Sports Rehabilitation, we often clarify the terms mobility, flexibility, and stretching. While related, understanding their distinct meanings is crucial for effective training and health.
Mobility vs. Flexibility: The Key Difference
Mobility is your body's ability to move a joint actively through its full range of motion with control and strength. It's about how much usable movement you have at a joint. Think of it as having the keys to open up your full movement potential.
Flexibility, on the other hand, is the passive ability of your muscles and connective tissues to lengthen. It's how far a joint can move when an external force (like gravity, another person, or a strap) is applied. You might be flexible enough to touch your toes, but without the strength and control, you won't have the mobility to squat deeply with proper form. As a Yale Medicine primary care sports medicine specialist, Samantha Smith, MD, explains, "Mobility exercises... are designed to increase the range of motion of a joint. The joints are the points of motion in our body. So, any time we move, we don’t want a limitation because of..." a lack of mobility.
For example, someone with excellent hip flexibility might have their leg pushed very high but lack the hip mobility to actively lift it to that height without help. Mobility requires both tissue extensibility and the strength and motor control to command the movement. This is why we focus on mobility movements that incorporate active effort and stability.
The distinction is important because while stretching focuses on lengthening muscles, mobility training focuses on improving the dynamic function of the entire joint system. Mobility is a dynamic movement with a strength component, challenging your body to maintain control through a full range of motion.
Active vs. Passive Range of Motion
- Active Range of Motion (AROM): The range of movement a joint can achieve by itself, using only the muscles that act on that joint. This is what mobility movements primarily target.
- Passive Range of Motion (PROM): The range of movement a joint can achieve when assisted by an external force. This is often what flexibility exercises, like static stretching, aim to improve.
True mobility encompasses the health of your joint capsule, the strength of surrounding muscles, and your brain's ability to control the movement (motor control). Without adequate mobility, other muscles might compensate, leading to imbalances and increased injury risk.
Here's a quick comparison:
| Feature | Mobility | Flexibility | Stretching |
|---|---|---|---|
| Definition | Active, controlled movement through a joint's full range of motion. | Passive range of motion of a joint or muscle. | Act of lengthening muscles and connective tissues. |
| Focus | Joint health, motor control, strength, stability. | Muscle length, tissue extensibility. | Increasing muscle length, relieving tension. |
| Goal | Usable range of movement with control. | Ability to achieve certain positions. | Temporary increase in range, relaxation. |
| Type | Dynamic, active. | Passive. | Can be static (held) or dynamic (moving). |
| Benefit | Injury prevention, performance, functional movement. | Improved posture, reduced muscle soreness. | Temporary relief, increased reach. |
To dig deeper into how these concepts intertwine with your overall physical movement, we encourage you to explore our article on the Difference Between Mobility and Movement.
The Science-Backed Benefits of Mobility Training
Incorporating mobility movements into your routine isn't just a trend; it's a fundamental aspect of physical health backed by science. We've seen the transformative effects on our patients at Evolve Physical Therapy + Sports Rehabilitation.
- Injury Prevention: Limited range of motion often leads to compensatory patterns that increase injury risk. For example, poor ankle mobility can strain your lower back during a squat. Improving it allows for a more natural squat, avoiding injury. A study in PeerJ found that subjects with higher mobility scores were six times less likely to get injured. Mobility work reduces injury risk, improves joint health, lessens muscle soreness, and speeds recovery.
- Improved Athletic Performance: For any athlete, better mobility translates to better performance. When joints move through their full range with control, your body generates more power and efficiency. For instance, improved hip mobility allows for a deeper squat with better muscle engagement. Mobility training improves range of motion, blood flow, and neuromuscular control, all contributing to peak performance.
- Reduced Joint Pain: Regular mobility movements can alleviate chronic joint pain and stiffness, especially for those with arthritis. As we age, joints can become less lubricated and tissues less elastic. Mobility training helps counteract these changes, keeping tissues healthy and preventing overuse injuries.
- Healthy Aging: Moving freely is paramount to maintaining independence as we age. The National Institutes of Health emphasizes that maintaining mobility is critical to staying independent as you age. While age-related stiffness is common, it's not inevitable. Consistent mobility movements can lessen its impact, helping you perform daily activities with ease.
- Improved Strength: Mobility and strength are two sides of the same coin. Good mobility lets you access positions for greater muscle activation and force production. This means you can build strength more effectively and safely.
The Ultimate List of Essential Mobility Movements
Now that we understand the profound benefits, let's dive into some of the most effective mobility movements you can incorporate into your routine. These exercises are designed to target key areas of your body, helping you open up better movement and feel fantastic. For even more insights, check out our curated list of the Best Mobility Movements.
Essential Hip Mobility Movements
Our hips are the powerhouses of our lower body, crucial for everything from walking and running to sitting and standing. Restricted hip mobility can impact your lower back, knees, and even your posture. These mobility movements are designed to improve hip internal and external rotation, flexion, and extension.

90/90 Hip Switch
- How to perform: Start seated on the floor with both knees bent at 90 degrees. One leg should be internally rotated in front of you, and the other externally rotated out to the side. Keeping your chest up, slowly lift your knees and switch sides, rotating your hips to bring the opposite leg to the front. Aim for smooth, controlled transitions.
- Targets: Hip internal and external rotation, hip capsule health.
- Why it's beneficial: This move addresses common hip rotation restrictions, improving squat depth, reducing hip pain, and enhancing lower body function.
Frog Stretch
- How to perform: Start on your hands and knees. Slowly widen your knees as far as comfortable, keeping your ankles in line with your knees and your feet flexed. You can lower onto your forearms for a deeper stretch. Gently rock forward and backward to explore the range.
- Targets: Hip adductors (inner thighs), hip external rotation.
- Why it's beneficial: Opens up the hips and inner thighs, which often get tight from prolonged sitting.
Spider-Man Lunge with Thoracic Rotation
- How to perform: Start in a push-up position. Step one foot outside your hand, keeping your back leg straight. From here, take the hand on the same side as your front foot, and rotate your torso, reaching that hand towards the ceiling. Return to the start and switch sides.
- Targets: Hip flexors, hip adductors, thoracic spine rotation, shoulder mobility.
- Why it's beneficial: This compound move improves hip and thoracic spine mobility, essential for good posture and overhead movements.
Hip CARs (Controlled Articular Rotations)
- How to perform: Stand tall or kneel on all fours. Slowly and deliberately move one hip through its largest possible pain-free range of motion in all directions, as if drawing a large circle with your knee. Focus on isolating the movement to the hip joint.
- Targets: All ranges of motion within the hip joint.
- Why it's beneficial: These are fundamental for hip joint health, actively working the joint capsule and surrounding muscles through their full range.
Fire Hydrants
- How to perform: Start on all fours, wrists under shoulders, knees under hips. Keeping your knee bent at 90 degrees, lift one leg out to the side like a dog at a fire hydrant, without letting your hips tilt. Lower with control.
- Targets: Gluteus medius and minimus, hip abductors.
- Why it's beneficial: Strengthens key hip muscles, improving stability and helping prevent knee issues.
For more exercises that focus on improving your movement capabilities, take a look at our guide to Mobility and Movement Exercises.
Spine and Lower Back Mobility Movements
A healthy spine is the foundation of all movement. These mobility movements will help improve the articulation of your vertebrae and reduce stiffness in your lower back and mid-back (thoracic spine). A mobile spine allows for better posture and reduced pain.

Cat-Cow
- How to perform: Start on your hands and knees. As you inhale, drop your belly towards the floor, lift your chest and tailbone (Cow pose). As you exhale, round your spine towards the ceiling, tucking your chin and tailbone (Cat pose). Repeat for 5-10 repetitions, focusing on smooth, flowing movement.
- Targets: Spinal flexion and extension, core engagement.
- Why it's beneficial: This gentle movement mobilizes the spine, reducing stiffness, especially for those who sit for long periods.
Thoracic Spine Windmills
- How to perform: Lie on your side with both knees bent at 90 degrees and stacked. Extend your arms straight out in front of you, hands together. Keeping your bottom arm on the floor, slowly lift your top arm and rotate your torso, opening your chest towards the ceiling until your top shoulder blade touches the floor. Follow your hand with your gaze. Return slowly.
- Targets: Thoracic spine rotation, shoulder mobility.
- Why it's beneficial: Improves mid-back rotation, which is often stiff, enhancing posture and reducing strain on the lower back and shoulders.
Lumbar Rotations (Windshield Wipers)
- How to perform: Lie on your back with knees bent and feet flat on the floor, hip-width apart. Let both knees gently fall to one side, keeping your shoulders on the ground. Hold briefly, then bring them back to center and let them fall to the other side, like windshield wipers.
- Targets: Lumbar spine rotation, lower back extensibility.
- Why it's beneficial: Gently mobilizes the lower back, relieving stiffness and promoting relaxation.
Segmental Cat-Cow
- How to perform: Similar to the regular Cat-Cow, but instead of moving the entire spine at once, focus on articulating one segment at a time. Start from your tailbone, then mid-back, then neck for flexion, and reverse for extension.
- Targets: Individual spinal segment mobility, body awareness.
- Why it's beneficial: This advanced variation improves control over each vertebra for a more resilient spine.
To integrate these into a broader movement practice, explore our insights on Ultimate Primal Movement Mobility.
Upper Body and Shoulder Mobility Movements
Our shoulders are incredibly mobile joints, but they are also prone to stiffness and injury due to overuse or lack of movement through their full range. These mobility movements focus on improving shoulder girdle mechanics, thoracic extension, and scapular control.
Shoulder CARs (Controlled Articular Rotations)
- How to perform: Stand tall with good posture. Keep your core tight and try to isolate the movement to just your shoulder joint. Slowly lift your arm forward and up, externally rotate it at the top, then continue bringing it back and down in a full circle, internally rotating as you lower. Reverse the movement.
- Targets: All ranges of motion within the shoulder joint.
- Why it's beneficial: Training your shoulder CARs safeguards this key joint by actively working it through its largest pain-free range, improving joint health and control.
Wall Angels
- How to perform: Stand with your back against a wall, feet about six inches away. Press your lower back, head, and arms (bent at 90 degrees, elbows and wrists against the wall) against the wall. Slowly slide your arms up the wall, keeping everything in contact, until they are overhead. Lower with control.
- Targets: Thoracic extension, shoulder flexion, scapular control.
- Why it's beneficial: Improves posture and overhead mobility, especially for those with a rounded upper back from sitting.
Thread the Needle
- How to perform: Start on all fours. Lift one hand, and "thread" it under your opposite armpit, palm facing up, lowering your shoulder and head to the floor. Reach the opposite arm forward for a deeper stretch.
- Targets: Thoracic spine rotation, shoulder mobility, upper back extensibility.
- Why it's beneficial: Opens the upper back and shoulders, relieving tension and improving rotational capacity.
Scapular Push-ups
- How to perform: Start in a plank position, hands directly under shoulders. Keeping your elbows straight, allow your shoulder blades to come together (depress your chest towards the floor), then push up, spreading your shoulder blades apart (pushing your upper back towards the ceiling).
- Targets: Scapular protraction and retraction, shoulder stability.
- Why it's beneficial: Strengthens the muscles that stabilize your shoulder blades, which is crucial for preventing shoulder injuries and improving upper body mechanics.
Dead Hangs
- How to perform: Hang from a pull-up bar with an overhand grip, allowing your body to relax and your shoulders to fully decompress. Keep your core gently engaged to prevent excessive arching in the lower back.
- Targets: Shoulder mobility, grip strength, spinal decompression.
- Why it's beneficial: As movement expert Bo Babenko notes, "Accumulating time in a hanging position has all sorts of benefits." Dead hangs improve shoulder mobility and decompress the spine, countering compressive forces.
For those interested in bodyweight training, our article on Calisthenic Movement Mobility offers additional insights.
How to Build Your Own Mobility Routine
Implementing mobility movements effectively requires a thoughtful approach. Here's how we guide our patients at Evolve Physical Therapy + Sports Rehabilitation to build a routine that truly works.
Assessing Your Mobility Levels
Before you can improve, you need to know where you stand. Use these simple self-assessment techniques to identify areas of restriction:
- Deep Squat Test: Can you perform a deep squat with your heels flat, chest up, and knees tracking over your toes? Restrictions here can point to ankle, hip, or thoracic spine mobility issues.
- Overhead Arm Raise: Can you raise both arms directly overhead, keeping your lower back flat against a wall? Limitations might indicate tight lats, limited shoulder flexion, or poor thoracic extension.
- Hip Internal/External Rotation: While seated, can you internally and externally rotate your hips without your torso compensating excessively? This can reveal hip capsule restrictions.
You can also film yourself to track progress, keep a workout journal, or work with one of our physical therapists for a personalized assessment.
Common Mistakes to Avoid
- Pushing into Pain: Mobility work should not be painful. While discomfort is okay, sharp pain means you're pushing too hard. Listen to your body and back off.
- Prioritizing Range Over Form: It's better to use a smaller range of motion correctly than a larger one incorrectly. As we always emphasize, prioritize control and form over all else. Your range will naturally increase as you improve.
- Holding Your Breath: Breathe deeply and rhythmically throughout your mobility movements. Your breath helps relax muscles and facilitate movement.
- Inconsistency: Mobility work requires consistency to show results. The more you do it, the better the results. Improving mobility is a gradual process, so keep your expectations realistic.
- Ignoring Weakness: Sometimes, a mobility issue is actually a stability or strength deficit. Our physical therapists can help distinguish between these and create a comprehensive plan.
Understanding the best primal movements for improving mobility can also guide your routine. Our blog post What is the best primal movement for improving mobility offers further reading.
Integrating Mobility into Your Day
Mobility movements are versatile and can be woven into your day for continuous benefits.
- As a Warm-Up: Dynamic mobility movements are a perfect pre-workout warm-up. They boost circulation and prepare your body for activity. Unlike static stretching, which can reduce power, dynamic mobility primes your nervous system.
- During a Cool-Down: After a workout, your muscles are warm, making it an ideal time for gentle mobility work. Breathe into the stretches to lengthen the muscles you've just worked.
- Active Recovery on Rest Days: Use rest days for dedicated mobility sessions. This promotes blood flow, reduces soreness, and helps maintain your gains.
- "Movement Snacks" Throughout the Day: If you have a sedentary job, break up long periods of sitting with short bursts of mobility movements. Even 5-10 minutes a day can make a significant difference.
- Recommendations for Athletes: For runners, hip and ankle mobility can prevent common issues like runner's knee. Targeted exercises like sciatic nerve flossing can help improve hamstring flexibility and neural mobility.
- Recommendations for Seniors: For seniors, gentle mobility movements help counteract joint stiffness, improve balance, and improve coordination, making daily tasks easier and safer.
- Exercises for Individuals with Arthritis: Gentle mobility movements are beneficial for alleviating arthritis pain and stiffness. For those with arthritis, daily stretching is more effective than less frequent sessions. Consult a physical therapist before starting a new program, but gentle, pain-free movements are generally encouraged. You can find more targeted advice in our recommended resource on Exercises for those with arthritis.
Frequently Asked Questions about Mobility Movements
We often get questions about mobility movements from our patients in Brooklyn. Here are some of the most common ones we address:
How is mobility different from flexibility?
Mobility is your ability to actively move a joint through its full range of motion with control. Flexibility is the passive ability of your muscles to lengthen. Mobility requires strength and stability, whereas flexibility does not. You can be flexible (able to touch your toes) but lack the mobility for a deep, controlled squat.
How often should I do mobility exercises?
For best results, aim for 5-15 minutes of mobility movements daily or before every workout. Consistency is more important than duration; even a few minutes a day is beneficial. If you're new, start with two to three sessions a week and build up. The most effective frequency is what you can consistently manage.
Can mobility training help with joint pain?
Yes. Regular mobility movements can significantly alleviate joint pain and stiffness. They improve joint lubrication, strengthen supporting muscles, and correct movement patterns that cause strain. This is particularly helpful for conditions like arthritis, where gentle movement can reduce discomfort and maintain function.
Move Better, Feel Better
We've explored mobility movements, from their difference from flexibility to their science-backed benefits for injury prevention, performance, pain reduction, and healthy aging. We've also provided a list of essential mobility movements for your hips, spine, and shoulders, with practical advice on integrating them into your daily life.
The key takeaways are consistency, prioritizing proper form over range, and listening to your body. Improving your mobility is a journey of gradual progress. Every step you take towards better movement contributes to a more capable, resilient, and pain-free you.
At Evolve Physical Therapy + Sports Rehabilitation, we believe that movement is medicine. If you're struggling with stiffness, pain, or simply want to open up your full movement potential, our expert physical therapists in Brooklyn are here to help. We offer personalized assessments and hands-on treatment plans designed to address your unique needs and guide you towards a more flexible, functional life.
Unlock Your Best Self: Mastering Ergonomic Body Posture
Why Understanding Ergonomic Body Posture Matters for Your Health

What is the ergonomically optimum body posture? It's a neutral body position where your joints are naturally aligned—head over shoulders, shoulders over hips, with minimal stress on muscles, tendons, and bones. This alignment maintains your spine's natural curves and allows your body to function efficiently whether you're sitting, standing, or moving.
Key principles of ergonomically optimum posture:
- Head: Level and in-line with your torso, ears aligned with shoulders
- Shoulders: Relaxed and pulled back, not hunched or liftd
- Spine: Maintains three natural curves (neck, mid-back, lower back)
- Hips: At approximately 90 degrees when sitting
- Knees: At or slightly below hip level, bent at 90 degrees
- Feet: Flat on the floor or footrest, ankles in front of knees
- Elbows: Close to body, bent between 90-120 degrees
- Wrists: Straight and aligned with forearms
If you work in an office and often use a computer, you've likely experienced the nagging pain that comes with hours at your desk. You're not alone. Nearly 70% of workers in America suffer from back pain, and a staggering 30% of days missed from work in 2018 were due to ergonomics complications. The culprit isn't just hard work—it's how we hold our bodies while we work.
Poor posture doesn't just cause immediate discomfort. Over time, it can lead to musculoskeletal disorders, decreased flexibility, chronic pain, and even breathing difficulties. The good news? Understanding and practicing proper ergonomic posture can prevent these issues and dramatically improve your quality of life.
As Lou Ezrick, founder of Evolve Physical Therapy with nearly two decades of experience treating chronic pain and movement dysfunction, I've helped thousands of patients find what is the ergonomically optimum body posture for their unique needs and watched them reclaim pain-free, active lives. Whether you're dealing with existing discomfort or simply want to prevent future problems, mastering ergonomic principles is one of the most powerful steps you can take.
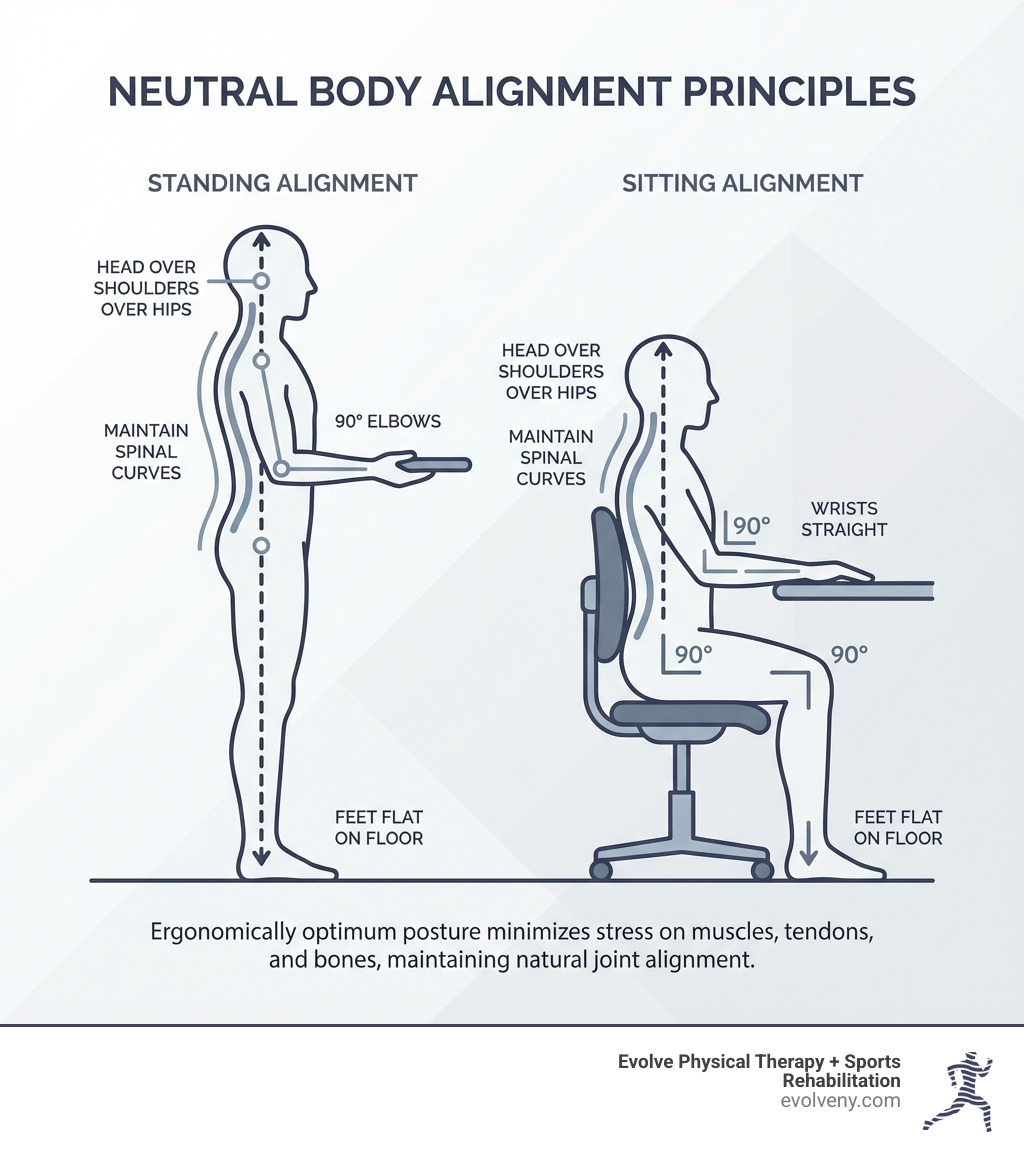
The Foundation: Understanding Neutral Body Posture
At Evolve Physical Therapy, we often talk about "neutral body posture" because it's the starting point for understanding what is the ergonomically optimum body posture. But what exactly is it? Simply put, posture is how we hold our bodies, whether we're sitting, standing, or even lying down. Neutral body positioning refers to a comfortable working posture where your joints are naturally aligned, minimizing stress and strain on your muscles, tendons, and skeletal system.
Our spine naturally has three gentle curves: one in the neck (cervical), one in the mid-back (thoracic), and one in the lower back (lumbar). Neutral posture aims to maintain these natural curves, allowing your body to function at its best. When these curves are protected and not exaggerated, your muscles can produce force efficiently, stress on tissues is minimized, and even your breathing and circulation can be more optimal. This is crucial for overall musculoskeletal health and preventing issues that can arise from bad office posture.
Why Neutral Posture is the Ergonomic Ideal
Why do we strive for neutral posture? It’s not just about looking good; it's about setting your body up for long-term health and peak performance. When your human movement system is in proper alignment, it's like a well-oiled machine. Stress on your tissues is minimized, muscles can produce force efficiently, and even your breathing and circulation of bodily fluids are optimized. This means less fatigue, better concentration, and significantly reduced risk of pain and injury.
Conversely, prolonged periods in an uncomfortable or misaligned posture can lead to a cascade of problems. We're talking increased compressive load on the spine, reduced blood flow to muscles (leading to numbness and pain), and even compromised digestion and breathing difficulties due to a restricted diaphragm. Good posture can help us avoid aches and pains in the back, neck, and shoulders, prevent sports injuries, and reduce wear and tear on our joints, especially the spine. Understanding Posture: What It Is & Why It Matters for Your Health is the first step towards a healthier you.
Static vs. Dynamic Posture: Why Both Matter
When we discuss posture, it’s important to distinguish between two types: static and dynamic.
- Static posture refers to how we hold our bodies when we are still—think sitting at your desk, standing in line, or even lying down.
- Dynamic posture is how we maintain stability and alignment while moving, such as walking, running, or lifting objects.
Both are incredibly important for overall health. While static posture sets the stage for comfort and efficiency in stationary tasks, dynamic posture ensures we move safely and effectively throughout our day. The truth is, even the most ergonomically "perfect" static posture can become detrimental if held for too long. Our bodies are designed for movement! As experts often say, "your best posture is your next posture." This emphasizes the importance of frequent changes in position and incorporating movement into our daily routines, whether we're at a desk or on the go. This approach is key to developing good posture for office workers.
What is the Ergonomically Optimum Body Posture for Sitting?
For many of us in Brooklyn, especially those with desk jobs, sitting is a significant part of our day. But prolonged sitting, if done incorrectly, is a major contributor to discomfort and pain. What is the ergonomically optimum body posture when you're seated? It’s a balanced approach to supporting your body while maintaining those crucial neutral alignments.

Aligning Your Lower Body: Hips, Knees, and Feet
Let’s start from the ground up. Proper lower body alignment is fundamental for good sitting posture. We recommend keeping your joints—hips, knees, and ankles—at an angle of 90 degrees or slightly higher. This helps distribute weight evenly and reduces strain.
- Hips: Ensure your hips are well-supported, ideally with your thighs parallel to the floor. Your knee joints should be at or slightly below your hip joints.
- Knees: Maintain a small gap, about three fingers wide, between the back of your knees and the front edge of your seat. This prevents pressure on nerves and blood vessels.
- Feet: Your feet should be flat on the floor. If they don't reach comfortably, use a footrest. We also advise against crossing your legs for extended periods, as this can compress nerves and restrict circulation. Keep your ankle joints slightly in front of your knees.
These adjustments are crucial for maintaining proper circulation and supporting your spine from its base. For more detailed guidance, check out our insights on the correct way to sit at computer.
Supporting Your Upper Body: Back, Shoulders, and Head
Once your lower body is in place, we move to the core and upper body. The goal here is to support your spine's natural curves and keep your head balanced over your shoulders.
- Back: Use your chair’s lumbar support to fit the small of your back. This helps maintain the natural inward curve of your lower spine, supporting your lower back and pelvis. Your upper body should be straight and upright, not twisted or excessively reclined.
- Shoulders: Keep your shoulders relaxed and low, not hunched up towards your ears. Your upper arms should hang naturally at your sides.
- Head and Neck: Your head should be aligned with your spine, balanced directly over your shoulders. We recommend a gentle chin tuck to keep your ears aligned with your shoulders, avoiding the common tendency to crane your neck forward, often referred to as "tech neck."
By maintaining this alignment, you reduce strain on your neck and back muscles, preventing stiffness and pain often associated with sitting posture at work.
Positioning Your Arms and Wrists for Computer Use
When working at a computer, the position of your arms and wrists is paramount for preventing common overuse injuries like carpal tunnel syndrome.

- Elbows: Keep your elbows close to your body, bent at an angle between 90 and 120 degrees. This allows your upper arms to be between vertical and 20 degrees forward, reducing shoulder strain.
- Forearms: Your forearms should be roughly parallel to the floor. This ensures a neutral position for your wrists.
- Wrists: Keep your wrists straight and aligned with your forearms. Avoid bending them up, down, or to the side. If you use a wrist rest, remember it’s only for resting between typing, not for supporting your wrists while you type. Never rest your wrists against hard or sharp desk edges, as this can create contact stress.
These small adjustments can make a big difference in preventing discomfort and long-term issues. For more tips on how to position yourself correctly, see our guide on computer sitting ergonomics.
Creating Your Ergonomic Workstation
Even with perfect posture knowledge, your workstation setup plays a monumental role in your comfort and ability to maintain what is the ergonomically optimum body posture. An ergonomically designed workstation isn't just a luxury; it's a necessity for preventing discomfort and promoting productivity. The goal is to tailor your environment to your body, not the other way around. Our guide to desk ergonomics posture guide covers these principles in detail.
The Core Components: Chair, Desk, and Monitor
- Chair: Your ergonomic chair is your first line of defense. It should be fully adjustable, allowing you to control height, backrest angle, lumbar support, and armrest position. Adjust your chair so your feet are flat on the floor (or on a footrest) and your thighs are parallel to the floor. Armrests should gently support your arms, keeping your elbows close to your body and shoulders relaxed.
- Desk: Ensure your desk height is appropriate for your task. If it's too low, you might slouch; if too high, you might shrug your shoulders. If your desk isn't adjustable, you can raise it with sturdy blocks or use a footrest if your chair needs to be higher. Crucially, ensure there's ample legroom and clearance beneath the desk so you can move freely without hitting your knees or feet.
- Monitor: Position your computer monitor directly in front of you, about an arm's length away (typically 20-40 inches). The top of the screen should be at or slightly below eye level. This prevents you from craning your neck up or down, which can lead to neck and shoulder strain. If you wear bifocals, you might need to lower your monitor an additional 1-2 inches.
By setting up these core components correctly, you're well on your way to a comfortable and healthy workspace. For a comprehensive guide, the Office ergonomics: Your how-to guide from Mayo Clinic offers excellent advice, and we also have our own tips for home office ergonomics.
Laptop Ergonomics vs. Desktop Setups
Laptops offer incredible portability, but their integrated design often forces us into poor postures. The screen is too low, and the keyboard is too close, leading to hunching and "tech neck." This is where understanding what is the ergonomically optimum body posture becomes critical, especially for laptop users.
For prolonged laptop use at a desk, we strongly recommend treating it like a desktop setup:
- Laptop Stand: Lift your laptop on a stand so the top of its screen is at eye level, just like a desktop monitor.
- External Keyboard: Use a separate, ergonomic keyboard positioned directly in front of you. This allows your wrists to stay straight and your forearms parallel to the floor.
- External Mouse: A separate mouse ensures your wrist and arm can remain in a neutral, relaxed position, avoiding awkward angles and repetitive strain.
These simple additions can transform a detrimental laptop setup into an ergonomically sound workstation, protecting you from strain and discomfort. Our blog post on ideal computer posture has more insights on this.
Beyond the Desk: Movement, Prevention, and Overall Health
While optimizing your sitting posture and workstation is vital, true ergonomic mastery extends beyond the desk. Our bodies thrive on movement, and understanding what is the ergonomically optimum body posture means embracing dynamic activity and proactive prevention. At Evolve Physical Therapy, we believe in a holistic approach to well-being, where ergonomics and physical therapy go hand-in-hand.
The Dangers of Staying Still and How to Counter Them
Regardless of how good your sitting posture is, staying in any single position for too long is simply not healthy. Prolonged sitting is associated with a range of health issues, from increased back pain (affecting nearly 70% of American workers) and muscle fatigue to reduced blood flow, leading to numbness and discomfort. It increases the compressive load on your spine and can even contribute to conditions like "awkward posture ergonomics."
The solution is simple: move!
- Frequent Breaks: We recommend taking a break from sitting every 30-50 minutes. Stand up, stretch, or take a short walk. Your best posture, as we like to say, is always your next posture.
- Micro-Adjustments: Even while seated, make small adjustments to your position. Shift your weight, stretch your fingers, hands, arms, and torso.
- The 20-20-20 Rule: If you're looking at a screen, every 20 minutes, look at something 20 feet away for 20 seconds. This helps reduce eye strain and encourages a brief mental break.
- Active Choices: Incorporate movement into your daily routine. Take the stairs instead of the elevator, walk to a colleague's desk instead of emailing, or use a distant water fountain.
These strategies are powerful counters to the risks of prolonged sitting and are key to preventing the common ergonomic issues we encounter when sitting for long periods.
How to determine what is the ergonomically optimum body posture for standing
Standing can be a great alternative to sitting, especially with the rise of standing desks. However, just like sitting, standing requires proper form to be truly ergonomic. What is the ergonomically optimum body posture when you're on your feet?
Here are our tips for ideal standing posture:
- Foot Position: Keep your feet about shoulder-width apart, with your weight balanced slightly forward on the balls of your feet. Avoid locking your knees.
- Knees: Maintain a slight bend in your knees.
- Core Engagement: Gently engage your core muscles. This helps support your lower back and maintain a neutral spine.
- Spine and Shoulders: Keep your back straight, stand tall, and let your arms hang naturally at your sides. Your shoulders should be relaxed and pulled back, not hunched.
- Head: Keep your head level, aligned with your spine, and your chin gently tucked.
- Shift Weight: If standing for long periods, shift your weight occasionally or use a low footrest to lift one foot at a time.
- Support: Consider using an anti-fatigue mat, especially on hard floors, to reduce strain on your feet and legs.
Standing desks are excellent tools, but remember to alternate between sitting and standing throughout the day. For more insights, refer to our guide on ergonomics standing desk posture.
What is the ergonomically optimum body posture for common physical tasks?
Not all work happens at a desk. Many jobs and daily tasks involve physical exertion, lifting, bending, and twisting. In these scenarios, what is the ergonomically optimum body posture is about using proper body mechanics to prevent injury. Without correct posture, tasks like lifting can significantly strain muscles, tendons, and discs.
- Lifting:
- Assess the Load: Before lifting, know the weight and plan your route.
- Stance: Stand with your feet shoulder-width apart, close to the object.
- Bend at Knees, Not Back: Hinge at your hips and bend your knees, keeping your back straight and maintaining a neutral spine. Keep your knees in line with (and behind) your toes.
- Engage Core and Legs: Lift by engaging your leg and core muscles, not your back.
- Keep Object Close: Hold the object close to your body.
- Avoid Twisting: Never twist your torso while lifting. If you need to turn, move your feet.
- Bending and Twisting: Avoid extreme bending or twisting of your torso, especially when combined with lifting or reaching. If you need to reach for something, try to move your whole body or use a tool to extend your reach.
- Pushing and Pulling: When pushing, keep your arms bent and use your body weight. When pulling, face the object, bend your knees, and use your body weight to pull.
These principles are critical for preventing strains and injuries. For comprehensive guidance on safe lifting techniques, we recommend consulting resources like How to Lift Safely.
Frequently Asked Questions about Ergonomic Posture
How often should I change my position at work?
We advise changing your position frequently throughout the day. As a general rule, try not to sit for more than 50 minutes at a time. Every 30-50 minutes, stand up, take a short walk, or perform some gentle stretches. Even small adjustments to your chair or backrest can make a difference. "Your best posture is your next posture." This constant, subtle movement helps prevent stiffness, improve circulation, and reduce the cumulative strain on your body.
Can good posture really prevent injuries and pain?
Absolutely! Maintaining what is the ergonomically optimum body posture is one of the most effective strategies for preventing injuries and alleviating pain. When your body is in neutral alignment, stress on your tissues is minimized, and your muscles work efficiently. This reduces the risk of musculoskeletal disorders (MSDs), common aches and pains in the back, neck, and shoulders, and overuse injuries like carpal tunnel syndrome. Good posture is a cornerstone of long-term health, helping to avoid wear and tear on your joints and keep your body functioning optimally.
Is there one single "perfect" posture for everyone?
No, there isn't one single "perfect" posture that suits everyone. Our bodies are unique, and what feels comfortable and sustainable for one person might not for another. The goal isn't rigid perfection, but rather maintaining a neutral, comfortable position that supports your spine's natural curves without increasing them. We encourage you to listen to your body and adjust your angles and positions within the universal principles of alignment. Occasional changes, even slightly outside the "ideal" ranges, can actually be beneficial for your body. The key is balance and movement.
Take Control of Your Posture and Well-being
Understanding what is the ergonomically optimum body posture is a powerful step towards a healthier, more comfortable life. By embracing the principles of neutral alignment, setting up an ergonomic workstation, and prioritizing frequent movement, you can significantly reduce your risk of pain and injury. These practices not only benefit your physical health but also improve your overall well-being and productivity.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we are dedicated to helping our community achieve optimal health. If you're experiencing pain, discomfort, or simply want to perfect your posture and move with greater ease, our expert physical therapists are here to guide you. We offer personalized assessments and hands-on treatment custom to your unique needs, helping you open up your best self.
Learn more about our ergonomic physical therapy services in Brooklyn to start your journey toward a healthier, more comfortable life.
Manual Therapy Techniques 101
Understanding Manual Therapy: A Hands-On Path to Pain Relief

Manual therapy techniques are specialized, hands-on treatments performed by physical therapists and other healthcare professionals to treat pain and improve movement. Here's what you need to know:
What Manual Therapy Techniques Include:
- Joint Mobilization - Gentle, controlled movements to improve joint mobility
- Joint Manipulation - Quick, targeted thrusts to restore joint function
- Myofascial Release - Sustained pressure to release tension in connective tissue
- Trigger Point Therapy - Direct pressure on painful muscle knots
- Soft Tissue Mobilization - Hands-on stretching and manipulation of muscles and ligaments
- Strain-Counterstrain - Gentle positioning to relieve muscle spasm
Primary Benefits:
- Reduce pain without medication
- Improve range of motion
- Decrease muscle tension and inflammation
- Speed recovery from injury
- Restore normal movement patterns
If you're dealing with recurring pain, you're not alone. Approximately 50 million adults in the U.S. are living with chronic pain, and many find relief through manual therapy. Unlike treatments that rely on machines, manual therapy involves a skilled practitioner using their hands to assess and treat your body's soft tissues and joints.
The roots of manual therapy date back to 400 BCE, but today's techniques are refined by modern science. Research shows they work through three main pathways: biomechanical (moving tissues), neurophysiological (changing pain signals), and psychological (the healing power of touch).
While both involve hands-on treatment, manual therapy is a clinical approach focused on diagnosing and treating specific musculoskeletal problems. Unlike a relaxation massage, it aims to identify and address the root cause of dysfunction. Physical therapists combine these techniques with exercise and education to create a comprehensive treatment plan.
I'm Lou Ezrick, founder of Evolve Physical Therapy, and I've spent nearly two decades specializing in manual therapy techniques for complex pain conditions and sports injuries. My approach combines advanced training in osteopathic manipulation with evidence-based physical therapy to help active individuals like you overcome pain and return to peak performance.
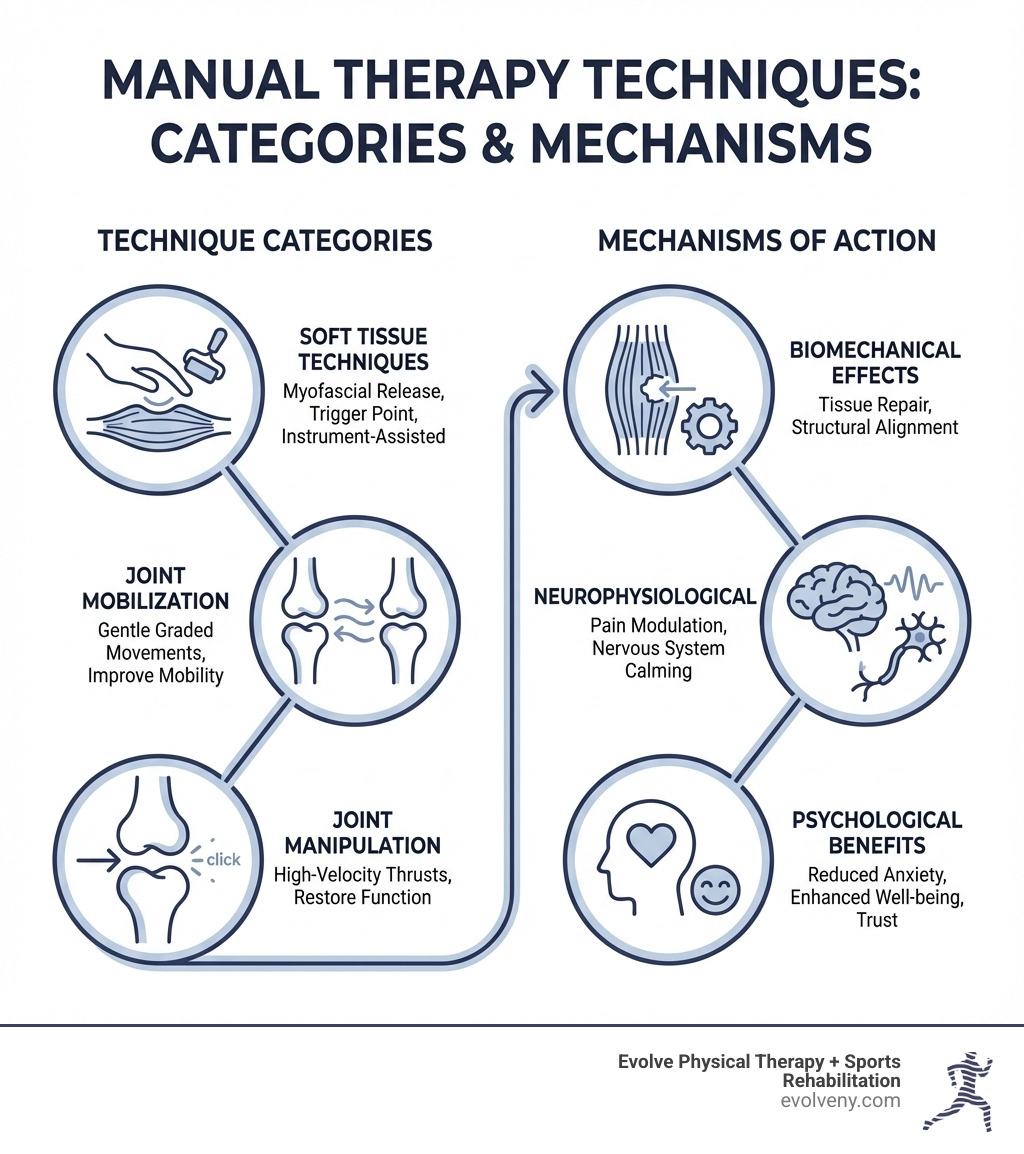
The Goals and Transformative Benefits of Manual Therapy
When you walk into Evolve Physical Therapy, our mission is simple: help you get back to doing what you love, without pain holding you back. Manual therapy techniques offer a powerful way to achieve this, and the results often surprise people who've been struggling for months or even years.
Pain relief is usually what brings patients through our door—and it's where manual therapy truly shines. Whether you're dealing with a nagging ache or sharp pain, these hands-on techniques work to calm muscle spasms, release tension, and restore normal joint function. We address the root cause of your discomfort, not just cover it up temporarily.
Many people living with chronic pain have found relief through manual therapy when other approaches fell short. The skilled, caring touch is also deeply therapeutic. Most patients find the sessions incredibly relaxing, which helps reduce pain by calming the nervous system.
Improved range of motion is another game-changer. When joints get stiff and muscles tighten, daily activities become harder. Through targeted manual therapy and passive stretching, we increase tissue extensibility—helping your muscles lengthen and joints glide smoothly again. This restored flexibility is crucial for everything from reaching a high shelf to training for your next race.
We also focus on reducing inflammation and tissue restriction. While inflammation is part of healing, chronic inflammation gets in the way. Manual therapy helps move excess fluid, decrease swelling, and break down scar tissue or adhesions. By restoring normal tissue texture, we help your body heal itself more effectively.
All of these benefits work together to create faster recovery and a real increase in your day-to-day function. When we combine hands-on manual work with therapeutic exercise and education, patients often see quicker improvements than they expected. This integrated approach can mean fewer treatment sessions, less reliance on pain medications, and in some cases, avoiding surgery.
The bottom line? We're here to empower your body's natural healing abilities and guide you back to a more comfortable, active life.
More info about our approach to Manual Therapy

A Deep Dive into Common Manual Therapy Techniques
When we use manual therapy techniques at Evolve Physical Therapy, we're tapping into something far more sophisticated than simply "rubbing where it hurts." Every technique creates a ripple effect through your body to help you feel better and move more freely.
When we apply manual therapy, three things happen. First, the biomechanical effect: our hands physically move your joints and tissues to improve mobility. Second, the neurophysiological effect: the techniques alter pain messages sent from your nerves to your brain, based on the Gate Control Theory of pain, providing immediate relief. Third, the psychological effect: therapeutic touch can reduce anxiety, promote relaxation, and change your perception of pain, increasing confidence in your recovery.
What ties all of this together is our patient-centered approach. Your body, injury history, and goals are unique. We tailor every technique to what you need for your recovery.
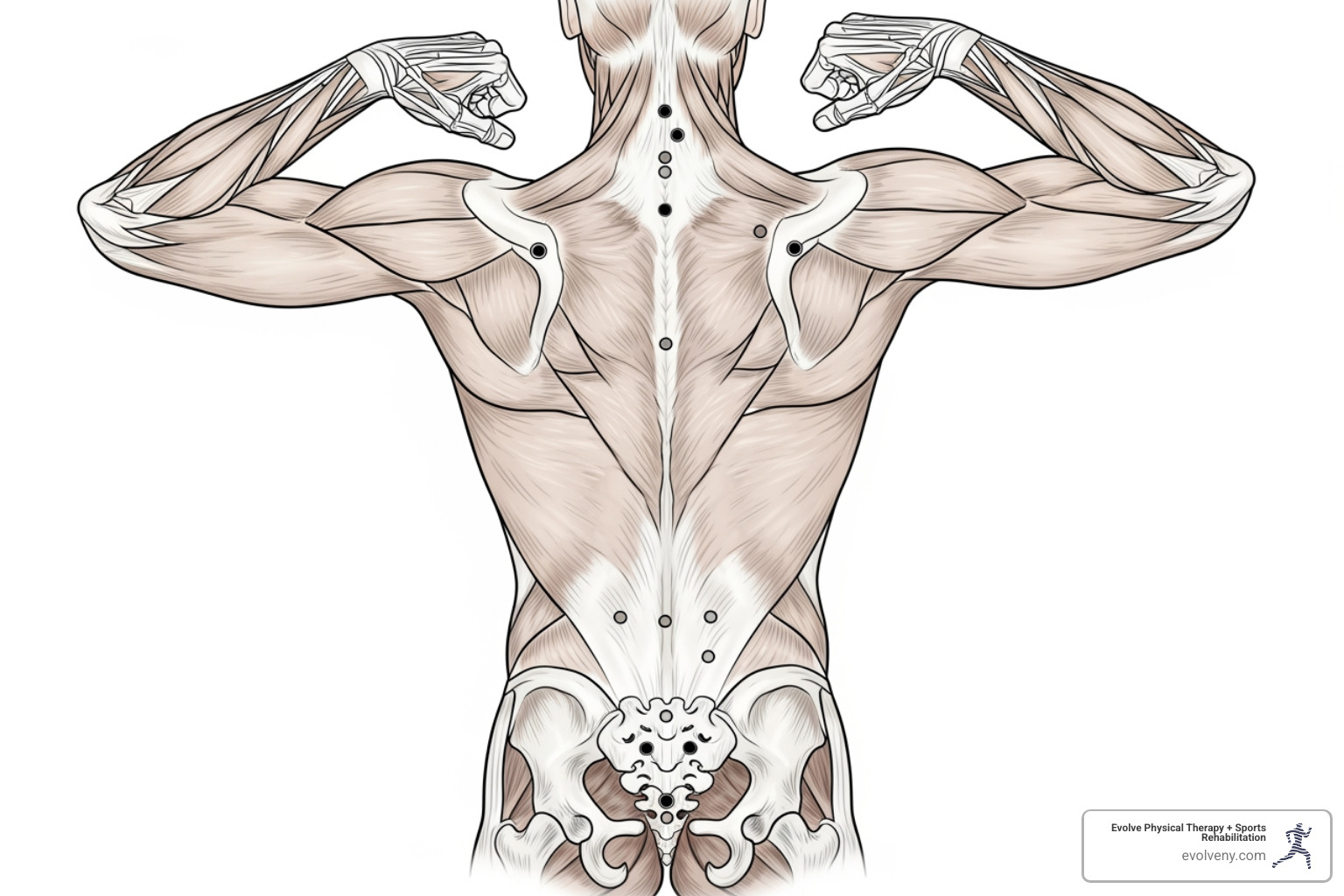
Soft Tissue Manual Therapy Techniques
Most pain and stiffness comes from your soft tissues—muscles, tendons, ligaments, and fascia. When these tissues get tight or develop adhesions, movement becomes a struggle. That's where soft tissue manual therapy techniques come in.
Myofascial Release (MFR) is a favorite for immediate relief. With MFR, we apply gentle, sustained pressure to restricted fascial areas, slowly stretching and lengthening the tissue until it releases.
Trigger Point Therapy addresses those infamous "knots" in your muscles. We apply direct, sustained pressure to these hyperirritable spots, or trigger points, to release the muscle contraction and stop both local and referred pain.
For muscle spasms, Strain-Counterstrain offers a gentle solution. Instead of stretching a tight muscle, we position your body to shorten it. Holding this comfortable position for about 90 seconds "resets" the muscle's stretch reflex, often eliminating the spasm.
Instrument-Assisted Soft Tissue Mobilization (IASTM) uses specialized stainless steel tools to detect and treat fascial restrictions our hands might miss. The tools apply focused pressure to break down scar tissue and promote organized healing by increasing blood flow.
Cross-Friction Massage works across your muscle fibers with firm, transverse pressure. This is powerful for chronic tendon issues, as it helps realign collagen, reduce scar tissue, and bring fresh blood flow to the area.
Active Release Techniques (ART) combines your movement with our precise pressure. As you move the affected body part, we apply targeted pressure to lengthen and release adhesions (scar tissue), often producing rapid improvements in mobility and pain.
Overview of soft tissue techniques used in physical therapy
Joint-Based Manual Therapy Techniques
When a joint becomes stiff or restricted, it throws off your body's mechanics. Joint-based manual therapy techniques target these articulations to restore proper movement.
Joint Mobilization involves skilled, controlled movements applied to joints at varying speeds and depths. We gently oscillate or sustain movements within your joint's available range to improve the subtle gliding and rolling motions necessary for pain-free function. The goal is to gradually coax the joint into moving more freely.
Joint Manipulation, sometimes called a thrust technique, involves a quick, precise thrust applied to a joint to restore motion and reduce pain. The "popping" sound (joint cavitation) is from gas bubbles releasing in the joint fluid and isn't essential for success. The key difference from mobilization is the high speed; once a manipulation begins, it cannot be stopped.
Here's a quick comparison:
| Feature | Joint Mobilization | Joint Manipulation (Thrust) |
|---|---|---|
| Speed | Slower, controlled | High-velocity, rapid |
| Amplitude | Varying, often larger | Low, precise |
| Force | Graded, gentle to moderate | High, targeted |
| Audible "Pop" | Rare | Common, but not essential for effectiveness |
| Control | Can be stopped mid-procedure | Cannot be stopped once initiated |
| Primary Goal | Improve joint play, reduce stiffness, increase ROM | Restore optimal motion, reduce pain, "open up" joint |
Both techniques aim to improve your joint mobility. The choice between them depends on your specific condition, our assessment, and your comfort level.
The American Physical Therapy Association defines manual therapy techniques as "skilled hand movements and skilled passive movements of joints and soft tissue"—and that hands-on expertise is what we bring to every session.
The APTA defines manual therapy techniques
Conditions Treated and What to Expect During a Session
When you step into Evolve Physical Therapy, you’re not just getting a treatment; you’re starting on a personalized journey to recovery. Our approach to manual therapy techniques begins with a thorough understanding of you.
Initial Assessment and Personalized Plan
We start with a comprehensive initial assessment. This full-body evaluation of your muscles, bones, nerves, and movement patterns, combined with your medical history and lifestyle, helps us uncover the root cause of your issue. Based on this, we create a personalized treatment plan outlining the specific manual therapy techniques we'll use, along with therapeutic exercise and education.
What to Expect During a Session
During a session, expect a hands-on experience. We use our skilled hands to apply pressure, stretch tissues, and move your joints. You might feel firm but tolerable pressure during soft tissue work or gentle, measured movements during joint mobilization. Communication is key, and we'll constantly check on your comfort level. Many patients find the experience surprisingly relaxing.
Beyond hands-on treatment, we empower you with knowledge. You'll receive home exercise programs to complement your manual therapy, helping you maintain gains and accelerate recovery. These exercises are crucial for long-term success.
Common Conditions Addressed
Manual therapy techniques are incredibly versatile and effective for a wide array of musculoskeletal conditions. We commonly use them to treat:
- Back and neck pain: Whether it's chronic discomfort or acute stiffness, manual therapy can significantly reduce pain and improve mobility in your spine.
- Headaches: Tension headaches and cervicogenic headaches (originating from the neck) often respond well to manual techniques that address muscle tension and joint restrictions in the neck and upper back.
- Sports injuries: From sprains and strains to tendinitis (like tennis elbow or patellar tendinitis), manual therapy helps facilitate tissue repair, reduce inflammation, and restore athletic function.
- Arthritis: While manual therapy can't cure arthritis, it can greatly alleviate pain, improve joint mobility, and reduce stiffness, enhancing your quality of life.
- Post-surgical recovery: After surgery, manual therapy helps to reduce swelling, break down scar tissue, restore range of motion, and facilitate a smoother, faster rehabilitation process.
- Carpal tunnel syndrome: Manual techniques can help decompress the median nerve, reduce inflammation, and improve the mobility of the wrist and hand.
- Shoulder pain (including frozen shoulder): We use manual therapy to improve range of motion, reduce stiffness, and alleviate pain in the shoulder joint and surrounding tissues.
- Joint stiffness: Any joint that feels "stuck" or restricted can benefit from mobilization and manipulation to restore its natural movement patterns.
These are just a few examples. If you're experiencing pain or limited movement in Brooklyn, including our locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin, manual therapy might be the solution you've been looking for.
Understanding Manual Therapy Frameworks and Application
How do physical therapists decide which manual therapy techniques to use? The answer lies in clinical reasoning—a thoughtful, systematic approach that guides our every decision.
At Evolve Physical Therapy, we don't use a one-size-fits-all protocol. Instead, we draw from various schools of thought, giving us a rich toolkit to address your individual needs.
Our approach uses a biopsychosocial framework, meaning we look at the whole picture. We consider not just your physical injury, but also how psychological and social factors (like stress or fear of movement) affect your recovery. Addressing you as a whole person is key to true healing.
This comprehensive perspective aligns with Orthopaedic Manual Physical Therapy (OMPT), an advanced specialty defined by the American Academy of Orthopaedic Manual Physical Therapists as "an advanced specialty area of physical therapy practice that is based on manual examination and treatment techniques integrated with exercise and patient education." In short, it's about combining skilled hands-on work with movement and knowledge.
More about advanced OMPT practice
How Practitioners Apply and Grade Techniques
Several influential concepts shape how we work. Think of these as different languages we speak when communicating with your body.
The Maitland Concept emphasizes continuous assessment and clinical reasoning. We constantly adjust our approach based on your body's response, carefully grading mobilization intensity to meet your needs.
The McKenzie Method, or Mechanical Diagnosis and Therapy (MDT), uses repeated movements to find a "directional preference"—a specific motion that decreases or centralizes your pain. It empowers you to manage symptoms with targeted home exercises.
The Mulligan Concept combines your active movement with our gentle, corrective force on a joint. These "Mobilizations with Movement" (MWMs) often allow for pain-free motion where it was previously uncomfortable.
When we apply mobilizations, we use the Maitland Joint Mobilisation Grading Scale to apply the right amount of force. Grades I-II are gentle oscillations for pain relief. Grades III-IV push further into the joint's range to address stiffness. Grade V is a high-velocity thrust manipulation.
By carefully considering the force, amplitude, speed, and direction, we can target exactly what needs attention—whether that's calming pain or increasing your range of motion. Our training helps us make these decisions instinctively.
Research continues to support the effectiveness of these approaches. Studies show that manual therapy techniques, when applied with sound clinical reasoning, can significantly reduce pain and improve function.
A deeper look at manual therapy for pain
Integrating Manual Therapy for a Full Recovery
Manual therapy techniques work best when they're part of something bigger. At Evolve Physical Therapy, we take a holistic treatment philosophy that weaves hands-on work together with other essential elements of healing.
Manual therapy prepares your body for recovery. By reducing pain and loosening tissues, we create a window of opportunity. The crucial next step is teaching your body how to maintain that newfound freedom of movement.
That's where therapeutic exercise comes in. These are carefully selected movements designed to strengthen supporting muscles, improve coordination, and retrain your body to move correctly. We're not just fixing the problem—we're giving you the tools to keep it fixed.
Patient education is equally vital. We believe you deserve to understand what's happening in your body, why a certain treatment helps, and how to modify daily activities to avoid re-injury. When you understand the "why," you become an active participant in your healing.
We also address postural correction. Poor habits, like hunching over a computer, can undermine progress. We help you identify these patterns and develop better alignment to support your body.
Research consistently shows that combining hands-on work with exercise and education produces significantly better results than any single approach alone. This integrated strategy can speed up recovery and help you reduce or avoid the need for medications or surgery.
While manual therapy is remarkably safe, it's not without potential risks. You might experience temporary soreness, similar to after a workout. More serious complications are extremely rare.
That's why we start with a thorough initial assessment. We carefully screen for contraindications like active infections, severe osteoporosis, certain cancers, or recent fractures. Your safety is the foundation of everything we do.
This comprehensive, integrated approach is what truly sets Evolve Physical Therapy apart. We're not just treating your symptoms; we're partnering with you to build a stronger, more resilient body.
Manual Therapy as a Physical Therapy Technique
Conclusion: Take the Next Step Towards a Pain-Free Life
As we've explored, manual therapy techniques are a time-tested, scientifically-backed path to healing. These hands-on approaches work on physical, neurological, and psychological levels to relieve pain and restore function.
Whether it's myofascial release for fascial restrictions, trigger point therapy for muscle knots, or joint mobilization for range of motion, each technique serves a specific purpose. The benefits—pain reduction, improved mobility, and faster healing—create lasting change when combined with exercise and education.
Living with chronic pain or injury can feel isolating. You don't have to figure it out alone. At Evolve Physical Therapy, our commitment goes beyond simply applying techniques. We take the time to understand your story and goals, serving our Brooklyn communities in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin with a hands-on approach that puts your needs first.
The importance of working with a skilled practitioner cannot be overstated. In the right hands, these techniques are powerful tools for change. Our team has the training and experience to assess your condition accurately and apply the right techniques safely and effectively.
Your recovery journey is yours. You deserve to take control of it and work with people who genuinely care about getting you back to the life you love. If you're ready to experience what manual therapy techniques can do for you, we're here and ready to help.
Loosen Up! Easy Stretching Routines for Older Adults
Why Gentle Stretching Matters More Than You Think

Gentle stretching for seniors is a powerful tool for maintaining independence and reducing discomfort—and you don't need special equipment to get started.
Quick Guide to Gentle Stretching for Seniors:
- Frequency: 10 minutes daily or 2-3 times per week
- Duration: Hold each stretch for 10-30 seconds
- Key Benefits: Improved flexibility, better balance, reduced pain, fall prevention
- Safety First: Always warm up for 5 minutes before stretching
- Listen to Your Body: Feel a gentle pull, never sharp pain
- Target Areas: Neck, shoulders, back, hips, legs, and ankles
Many believe aches and stiffness are unavoidable parts of aging, but that's not the whole story. Research shows seniors who stretch just twice a week for 10 minutes see real improvements in flexibility.
Stretching helps with everyday movements like turning your head, reaching into a cupboard, or tying your shoes. It improves range of motion, eases joint pain, boosts circulation, and can even help regulate blood glucose and improve mental health.
The best part? You don't need to "feel the burn." The goal of gentle stretching is to help you move more freely. Whether you're dealing with a stiff back, tight hips, or just want to maintain mobility, a simple stretching routine can make a real difference.
I'm Lou Ezrick, founder of Evolve Physical Therapy. For nearly two decades, I've helped thousands of patients improve their mobility. My approach to gentle stretching for seniors emphasizes addressing the root cause of stiffness and pain, not just treating symptoms, helping older adults regain the freedom to do the activities they love.
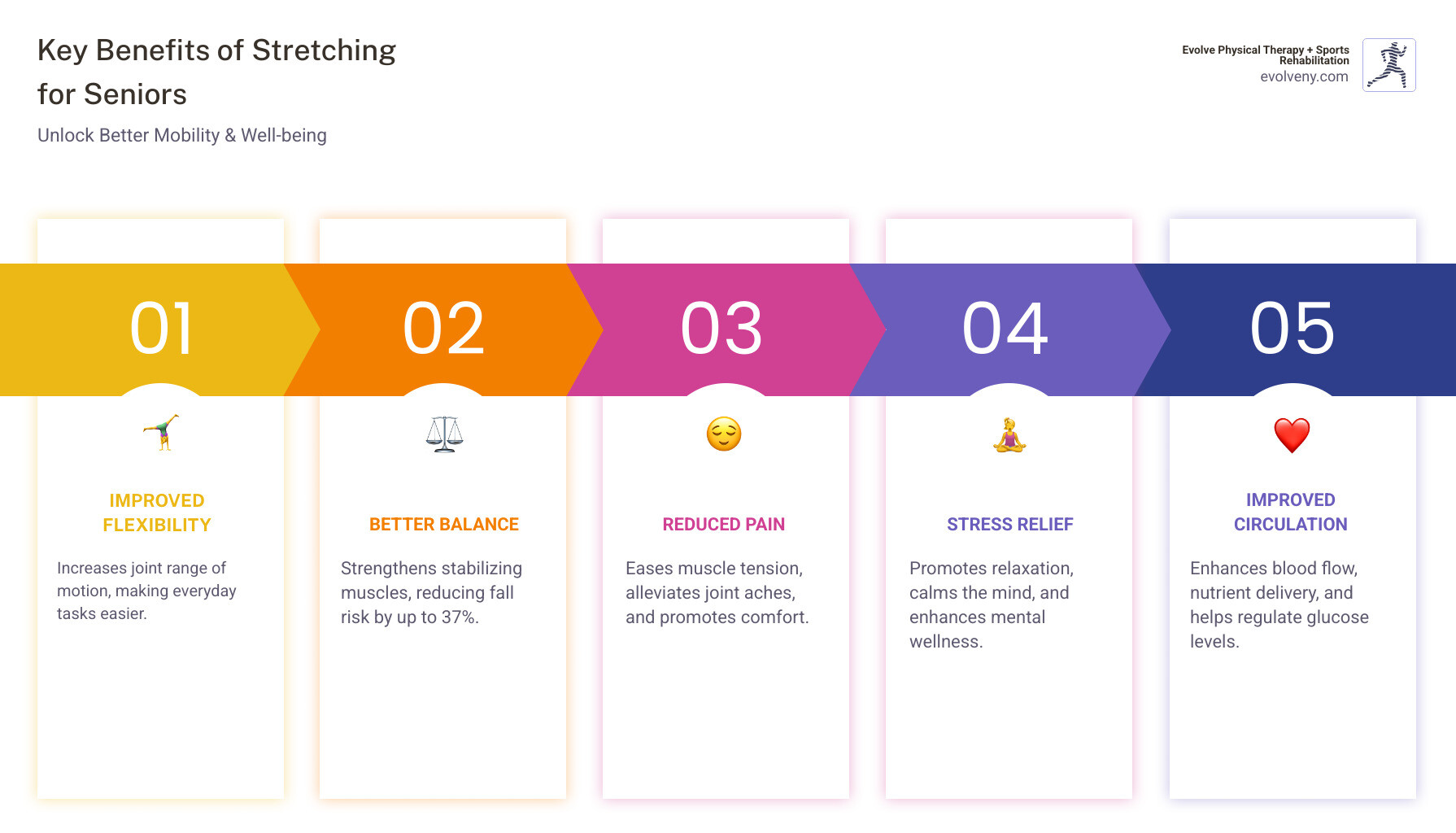
Why Stretching is Key for Healthy Aging
As we age, our muscles can lose mass and stiffen, and ligaments become less elastic. This makes everyday tasks like reaching for a high shelf or bending down feel harder. But here's what I want you to remember: these changes don't have to dictate your quality of life. Regular, gentle stretching for seniors can counteract many of these effects.
Physical Benefits
The physical benefits of stretching are backed by science. Here's what a consistent routine can do for your body:
- Improved Flexibility and Range of Motion: Regular stretching loosens tight muscles and stiff joints, allowing you to bend, reach, and turn with less strain. As Harvard Health Publishing notes, stretching both the upper and lower body is crucial for daily living.
- Better Posture: Easing muscle tension through stretching promotes better posture. This distributes weight more evenly, taking unnecessary strain off your spine and joints.
- Pain and Stiffness Relief: By gently lengthening muscles and improving blood flow, stretching reduces the stubborn stiffness that can build up throughout the day.
- Fall Prevention: Stretching improves balance and coordination, giving you the stability and reaction time needed to prevent falls.
- Improved Circulation: Better blood flow delivers more oxygen to your muscles. This supports recovery and can even help regulate blood glucose levels.
- Injury Prevention: When your muscles are pliable and joints move freely, you're less likely to strain something during everyday activities.
Mental Wellness
The benefits of gentle stretching for seniors are mental and spiritual, too.
When you take a few minutes to stretch, you create a quiet moment to practice mindfulness. By focusing on your breathing as your muscles release, daily worries can fade into the background.
This simple practice offers real stress reduction, can lift your mood, and fosters a sense of well-being. It's an act of self-care that requires no special equipment or gym membership. Just a few minutes of gentle movement can make a meaningful difference in how you feel, both physically and mentally.
Getting Started: How to Stretch Safely
Before you begin, let's cover a few simple guidelines to ensure gentle stretching for seniors is a safe and enjoyable part of your routine.
- Listen to your body. A proper stretch should feel like a gentle pull or tension, never sharp, stabbing, or radiating pain. If you feel pain, ease back until the sensation is mild and you can breathe comfortably. The goal is to gently awaken muscles, not force them.
- Warm up first. Stretching cold muscles is a quick way to get hurt. Take 5-10 minutes for a simple warm-up like light walking, marching in place, or gentle arm swings to increase blood flow and prepare your muscles for movement. The best time to stretch is after exercise when your muscles are already warm.
- Breathe deeply. Holding your breath creates tension. Breathe deeply and consistently throughout each stretch to help your muscles relax. Try inhaling as you prepare and exhaling as you move into the stretch.
- Avoid bouncing. Move into each stretch slowly and smoothly, hold for 10-30 seconds, and then gently release. Bouncing can cause tiny tears in your muscles, leading to more stiffness.
- Protect your joints. Always keep your joints slightly bent—never locked. This applies especially to your knees and elbows. A "soft" knee or elbow takes the pressure off the joint. You can learn more about joint health and helpful equipment for stretching from trusted resources.
You don't need fancy equipment. A sturdy, non-slip chair is helpful for support, and a towel or resistance band can help you reach. Find a quiet, clutter-free, well-lit spot where you can move comfortably.
A Head-to-Toe Guide to Gentle Stretching for Seniors

This section provides step-by-step instructions for safe and effective stretches. Remember to move slowly, breathe deeply, and listen to your body. Each stretch should feel like a gentle release, never a strain.
Upper Body Stretches for Neck, Shoulder, and Back Relief
Tension in the neck, shoulders, and back is common, often caused by prolonged sitting, poor posture, or stress. These gentle stretches can help release that built-up tension.
- Neck Tilts: Sit or stand tall. Slowly tilt your right ear toward your right shoulder until you feel a gentle stretch. Hold for 15-30 seconds, then repeat on the left. You can also gently lower your chin to your chest to stretch the back of your neck.
- Shoulder Rolls: Sit or stand tall. Gently roll your shoulders up toward your ears, then back and down in a smooth circle. Repeat 5-10 times, then reverse direction.
- Chest Opener: Sit or stand tall and clasp your hands behind your back (or hold opposite elbows). Gently pull your shoulder blades together and down, lifting your chest. Hold for 20-30 seconds.
- Upper Back Stretch (Seated Cat-Cow): Sit in a chair with hands on your knees. Round your back and tuck your chin ("cat"), then arch your back and lift your chest ("cow"). Alternate between positions 5-10 times.
- Arm-Across-Chest Stretch: Bring your right arm across your chest. Use your left hand to gently pull your right upper arm closer to your body. Hold for 20-30 seconds, then switch arms.

Lower Body Stretches for Hips, Legs, and Ankles
When your lower body is tight, it affects balance and mobility. These gentle stretching for seniors exercises target the muscles that keep you steady.
- Hamstring Stretch: Sit on the edge of a chair. Extend one leg straight with your heel on the floor. Keeping your back straight, hinge forward from your hips until you feel a stretch. Hold for 20-30 seconds, then switch legs.
- Quadriceps Stretch: Stand near a chair for support. Bend your right knee and grasp your right ankle, gently pulling your heel toward your glute. Keep your knees together. Hold for 20-30 seconds, then switch legs.

- Calf Stretch: Face a wall with hands on it for support. Step your right leg back, keeping it straight with your heel on the floor. Lean forward until you feel a stretch in your right calf. Hold for 20-30 seconds, then switch legs.
- Hip Flexor Stretch: Kneel on your right knee (use a cushion). Place your left foot flat on the floor in front of you. Gently shift your weight forward until you feel a stretch in your right hip. Hold for 20-30 seconds, then switch sides.
- Ankle Circles: Sit and extend one leg. Slowly rotate your ankle in a circle 10-15 times clockwise, then counter-clockwise.
- Seated Figure-Four Stretch: Sit tall in a chair. Cross your right ankle over your left knee. Gently lean forward from your hips until you feel a stretch in your outer right hip. Hold for 20-30 seconds, then switch sides.
The Ultimate Guide to Seated Gentle Stretching for Seniors
Chair-based stretches are a game-changer for those with limited mobility or balance concerns. They provide stability while delivering all the benefits of stretching.
- Seated Spine Twist: Sit tall in a chair. Place your left hand on your right knee and gently twist your torso to the right. Hold for 15-30 seconds, then repeat on the other side.
- Seated Knee-to-Chest Stretch: Sit tall and grasp your right knee. Gently pull it toward your chest while keeping your back straight. Hold for 15-30 seconds, then switch legs.
For a guided experience, consider following a guided seated relaxation routine to connect your breath with movement.
Building a Consistent Stretching Habit
The secret to open uping the full benefits of gentle stretching for seniors is not intensity, but consistency. Small, steady efforts will always beat sporadic ones.
Finding Your Rhythm
Research shows stretching just twice a week for 10 minutes improves flexibility. While a daily 10-minute routine is even better, the key is finding a frequency you can stick with. At Evolve Physical Therapy, we emphasize consistency over intensity. Short, frequent sessions are more effective than one long, exhausting one.
When Should You Stretch?
The best time to stretch is the time you'll actually do it.
- Morning Routine: Ease into the day and loosen up stiff joints.
- Post-Walk Cooldown: Stretch when your muscles are already warm and pliable.
- Evening Wind-Down: Release the day's tension and prepare for restful sleep.
Celebrating Your Progress
Instead of focusing on a timeline, pay attention to small improvements in your daily life.
- Journal Small Wins: Note how long you can hold a stretch or simply how you feel before and after. Did you sleep better? Do you feel less stiff?
- Notice Real-World Victories: Is it easier to tie your shoes? Can you reach a high shelf with less strain? Does getting out of a chair feel less strenuous? These are the true measures of success.
Making It Stick
- Stretch with a Partner: A friend or family member can provide encouragement and accountability, turning your routine into a pleasant social activity.
- Link to an Existing Habit: Attach your new stretching routine to something you already do every day, like while your coffee brews or during TV commercials.
- Set Up Your Environment: Keep a mat or towel visible, or set out your sturdy chair the night before. These small cues make it easier to follow through.
Frequently Asked Questions about Senior Stretching
How do I know if I'm stretching too hard?
A proper stretch should feel like a gentle tension or pull, never sharp, stabbing, or radiating pain. If you feel pain, you've gone too far. Ease back until the sensation is mild and you can breathe comfortably. The "no pain, no gain" rule does not apply to gentle stretching for seniors. If you're grimacing or can't breathe easily, you're pushing too hard.
Do I really need to warm up before I stretch?
Yes, this step is essential for safety and effectiveness. Stretching "cold" muscles increases the risk of strain. A simple five-minute warm-up, like marching in place or a slow walk, increases blood flow and prepares your muscles for movement, allowing for a better, safer stretch.
When should I see a professional for stretching?
While home stretching is beneficial, professional guidance is invaluable at times. Consult a doctor or physical therapist before starting if you have a chronic condition (like arthritis), a recent injury or surgery, or balance issues. Professional guidance is also recommended if you have persistent pain or want a personalized routine. A physical therapist can create a safe, effective program for your unique needs.
Medicare often covers medically necessary physical therapy services, which can include stretching guidance. At Evolve Physical Therapy + Sports Rehabilitation, we create customized programs to help older adults regain mobility and confidence safely.
Take the First Step Towards Better Mobility
Aches, pains, and stiffness don't have to be your new normal. Gentle stretching for seniors is a simple, accessible way to reclaim mobility, reduce discomfort, and improve your quality of life. You can start right now.
Think of stretching as daily self-care. The benefits—improved flexibility, balance, pain relief, and circulation—translate into real-world improvements, like tying your shoes without wincing or reaching for a high shelf with confidence.
The secret is simple: small daily habits lead to big results. Just 10 minutes a day, done consistently, can transform how you feel. Listen to your body, move gently, and be patient. Every stretch is a step toward greater independence.
While home stretching is wonderful, professional guidance is valuable, especially when starting out. For a personalized assessment to ensure you are stretching safely and effectively, consider seeking professional help. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we address the root causes of stiffness and pain, creating customized programs that fit your goals.
If you're in Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin, we're here to support you. Our hands-on approach means you'll receive expert guidance every step of the way. To see how our programs can help you move with more confidence and less pain, learn more about physical therapy for seniors. Take that first step today.
The Road to Recovery: Why Hand Therapy is Crucial After Surgery
Why Post-Surgery Hand Therapy is Essential for Your Recovery

Post-surgery hand therapy is a specialized rehabilitation program designed to restore strength, mobility, and function after hand or wrist surgery. Here's what you need to know:
Key Benefits of Post-Surgery Hand Therapy:
- Faster Recovery - Structured exercises and treatments accelerate healing
- Improved Range of Motion - Prevents stiffness and maintains joint flexibility
- Reduced Pain and Swelling - Specialized techniques manage discomfort effectively
- Restored Strength - Progressive strengthening returns your hand to full function
- Minimized Scar Tissue - Manual therapy prevents adhesions and contractures
Surgery is just the first step in treating hand conditions. While the procedure addresses the underlying problem, the real work of recovery begins afterward.
After hand surgery, you can expect some pain, swelling, and a period of immobilization with bandages or splints. Your doctor may restrict certain activities while your hand heals. But here's what many patients don't realize: rehabilitation may be even more important than the surgery itself.
Recovery after hand surgery depends greatly on the type of procedure you had and your underlying condition. But one thing remains constant—your active participation in therapy directly impacts your outcome. The hand is an intricate and very sensitive part of the body, requiring specialized care to regain its remarkable function.
Progress will be slow but steady. A serious injury or major surgery typically takes about 6 months to really loosen up scar tissue. This isn't a quick fix—it's a commitment to your long-term recovery and quality of life.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, and I've spent nearly two decades helping patients steer complex rehabilitation cases, including specialized post-surgery hand therapy for conditions ranging from carpal tunnel release to traumatic injuries. My approach focuses on hands-on treatment and addressing the root cause of dysfunction, not just managing symptoms.

The Vital Role of Hand Therapy in Your Recovery
When we talk about recovery after hand surgery, we often focus on the surgical procedure itself. However, at Evolve Physical Therapy + Sports Rehabilitation, we understand that surgery is truly just the beginning. The journey to regaining full function in your hand and wrist relies heavily on dedicated post-surgery hand therapy.
What Exactly is Hand Therapy?
Hand therapy is a specialized form of rehabilitation focused on the upper extremity—from the shoulder to the fingertips. Our goal is to restore your upper limb's ability and ensure a safe and sustainable return to daily activities. It's not just about addressing the immediate surgical site; it's about optimizing the entire arm's function to support your hand.
A key aspect of specialized hand therapy is the expertise of a Certified Hand Therapist (CHT). A CHT is either an occupational therapist or a physical therapist who has undergone extensive training and accumulated at least 4,000 hours of direct practice in treating hand, wrist, elbow, and shoulder disorders. They must also pass a rigorous certification exam and maintain their credentials through ongoing education every five years. This advanced certification means they possess a deep understanding of the complex anatomy and mechanics of the hand, making them uniquely qualified to guide your recovery. You can learn more about this specialized field through our guide, What is hand physical therapy?.
The Unwavering Benefits of Post-Surgery Hand Therapy
The benefits of engaging in post-surgery hand therapy are profound and multifaceted:
- Regaining Strength: After surgery, your hand muscles may weaken due to disuse or the healing process. Our therapists guide you through progressive strengthening exercises, rebuilding your grip, pinch, and overall hand power.
- Improving Range of Motion: Stiffness is a common and challenging side effect of surgery. Hand therapy exercises are specifically designed to improve your hand's range of motion, preventing contractures and ensuring your joints move freely. This is crucial for performing everyday tasks.
- Managing Swelling (Edema): Swelling can impede healing and cause pain. Hand therapy incorporates techniques like elevation, compression, and specific movements to reduce edema and improve circulation.
- Scar Tissue Management: Surgery inevitably leaves scar tissue. If not properly managed, it can become thick, tight, and restrict movement. Through specialized massage, mobilization techniques, and even silicone applications, we help soften and flatten scar tissue, preventing adhesions and improving flexibility.
- Pain Reduction: While some discomfort is expected, our therapists use various modalities and techniques to manage and reduce your post-operative pain, allowing you to participate more effectively in your rehabilitation.
- Sensory Re-education: Nerves can be affected by injury or surgery. Hand therapy includes desensitization and sensory re-education to help your hand regain normal sensation and prevent issues like Complex Regional Pain Syndrome (CRPS).
Your Active Participation is Key
We cannot stress this enough: your effort and dedication to your daily home therapy program are just as important as the surgeon's skill during the operation. Excellent results are consistently seen in motivated patients who diligently follow their rehabilitation plan. Don't rely solely on scheduled therapy appointments; consistent, daily work is essential. As outlined by Johns Hopkins Medicine, management after surgery is a comprehensive process where patient adherence is paramount. We recommend a minimum of a full half-hour of focused exercises, five times a day, to truly make progress.
Your Guide to Post-Surgery Hand Therapy Treatments and Exercises

At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we believe in a holistic, hands-on approach to your recovery. Every patient's journey is unique, which is why we develop customized treatment plans custom to your specific surgery, condition, and personal goals. We work in close collaboration with your surgeon, ensuring our therapy aligns perfectly with your post-operative protocol. This integrated approach, as highlighted in our guide to hand surgery rehab in Brooklyn, is critical for optimal outcomes. The importance of a specialist cannot be overstated, especially when dealing with the intricate mechanics of the hand.
Common Hand Therapy Treatments
Our comprehensive post-surgery hand therapy programs incorporate a variety of proven treatments:
- Splinting and Bracing: Often, protective orthotics (splints or braces) are custom-made or adjusted to support and protect the healing tissues. They can immobilize specific joints, provide controlled motion, or offer stability during activities, preventing re-injury and promoting optimal healing.
- Manual Therapy: This involves hands-on techniques performed by your therapist to mobilize joints, stretch tight tissues, reduce swelling, and improve circulation. It’s a cornerstone of our hands-on approach.
- Massage Techniques: Targeted massage can help reduce pain, improve blood flow, and, importantly, manage scar tissue. Massaging the surgical scar helps to soften it, prevent adhesions to underlying structures, and improve skin elasticity.
- Heat and Cold Therapy: Heat therapy helps to relax muscles, increase blood flow, and prepare tissues for stretching and exercise. Cold therapy, on the other hand, is excellent for reducing pain and inflammation, especially after exercise or if swelling is present.
- Desensitization for Nerve Sensitivity: After nerve injury or surgery, the hand can become overly sensitive. Desensitization techniques involve exposing the area to various textures and pressures to gradually reduce sensitivity and help nerves interpret sensations normally.
- Nerve Gliding Exercises: These specific exercises are designed to help nerves move freely within their sheaths, preventing adhesions and reducing symptoms like tingling or numbness, particularly after procedures like carpal tunnel release.
- Scar Mobilization: Beyond general massage, scar mobilization focuses on specific techniques to prevent fibrosis (thickening) and adhesions of scar tissue, which can severely limit movement and cause pain.
Essential Exercises for Post-Surgery Hand Therapy
Exercises are the backbone of your post-surgery hand therapy. They are carefully chosen and progressed to meet your healing needs:
- Range of Motion (ROM) Exercises: These are fundamental. They help to restore the flexibility and movement of your joints. We often start with gentle, pain-free movements and gradually increase the range as your healing progresses. Examples include wrist bends (bending your wrist up and down, side to side), finger bends (making a gentle fist and then straightening your fingers), and tabletop exercises (placing your hand flat on a table and lifting individual fingers or gliding them in a wave-like motion).
- Strengthening Exercises: Once sufficient healing has occurred, we introduce exercises to rebuild your hand and forearm strength. This might involve squeezing a soft ball, using putty for resistance, or carefully lifting light weights. Progressive strengthening is vital for returning to daily tasks and activities.
- Functional Task Training: The ultimate goal of therapy is to get you back to doing what you love. Functional task training involves practicing movements and activities specific to your daily life, work, or hobbies. This could include picking up small objects, writing, typing, or simulating work-related movements.
For a deeper dive into how movement helps recovery, explore how post-surgery range-of-motion exercises are crucial for improving flexibility and reducing pain.
Understanding Range of Motion in Your Post-Surgery Hand Therapy
Understanding the different types of range of motion is crucial in your recovery. They dictate how much movement you can achieve and how your muscles are engaged.
- Passive Range of Motion (PROM): In PROM exercises, your therapist, or sometimes a special device, moves your hand or a joint for you. You don't use your own muscles to perform the movement. This is typically done in the very early stages of recovery when active movement might be painful or restricted, helping to maintain joint flexibility and prevent stiffness.
- Example: Your therapist gently bends and straightens your fingers or wrist while you relax your hand.
- Active-Assisted Range of Motion (AAROM): With AAROM, you actively participate in the movement, but with some assistance from your therapist or your other hand. This bridges the gap between passive and active exercises, helping you regain control and build initial muscle strength.
- Example: You use your healthy hand to gently guide your surgical hand through a wrist circle, or your therapist provides light support as you try to make a fist.
- Active Range of Motion (AROM): AROM exercises involve you moving your hand or joint entirely on your own, using only your own muscles. This is a critical step for strengthening and improving coordination.
- Example: You independently perform finger spreads, wrist flexion/extension, or thumb opposition exercises without any external help.
Navigating Your Recovery Timeline and Maximizing Results
Recovery after hand surgery is undeniably a process, not a race. It requires patience, consistency, and a clear understanding that progress will be slow but steady. A bad injury or major surgery will make your hand stiff, and it usually takes about 6 months to really loosen up scar tissue. This is why a comprehensive and phased approach to healing, guided by expert post-surgery hand therapy, is so important. For more insights into the duration of therapy, you can read our article, how long is physical-therapy after hand-surgery.
Typical Recovery Phases After Hand Surgery
While timelines can vary based on the specific surgery and individual healing, we generally follow a phased approach to rehabilitation, often spanning several months:
Phase 1: Inflammatory Phase (Weeks 1-3 Post-Op)
- Principle: Protection of the injured hand to facilitate uneventful healing.
- Focus: Managing pain and swelling, protecting the surgical site, and initiating very gentle, pain-free motion. Your hand will likely be immobilized in a splint or dressing.
- Activities: We emphasize rest, ice, compression, and elevation (RICE). You'll learn how to perform full active/passive range of motion exercises for your shoulder, elbow, and forearm, as well as light, pain-free movements of your digits (fingers and thumb) if permitted by your surgeon. Patient education on self-management is crucial.
- Goal: Healing without complications, limited swelling, and full (or pre-op) ROM in uninjured joints.
Phase 2: Early Repair Phase (Weeks 4-6 Post-Op)
- Principle: Continued protection with promotion of directed tissue repair.
- Focus: Controlled mobilization, scar management, and beginning to restore basic strength.
- Activities: Your splint use may become part-time. We'll introduce tendon and nerve gliding exercises, gentle passive range of motion, and light resisted grip/pinch strengthening using soft objects or putty. We'll also start scar hydration, compression, and mobilization to prevent adhesions. You'll begin using your hand for pain-free, light household activities (e.g., lifting less than 20 lbs).
- Goal: Established tissue healing with isometric strength, flat and minimally sensitive scars, and improved wrist ROM (e.g., >50% of the other side).
Phase 3: Late Repair and Early Tissue Remodeling Phase (Weeks 7-12 Post-Op)
- Principle: Reestablishment of proprioception (your hand's sense of position in space) and encouraging normal tissue structure.
- Focus: Graduated strengthening, improving endurance, and functional reactivation.
- Activities: Daytime splint use is typically discontinued. We progress to more resisted grip/pinch strengthening, isotonic/eccentric wrist strengthening, and workplace-specific functional tasks. You'll gradually increase your lifting capacity (e.g., up to 40 lbs) and participate in more moderate household activities.
- Goal: Normal tissue structure and reinnervation through daily activities, approximately 75% of pre-op wrist ROM, and 50-75% of pre-op grip and pinch strength.
Phase 4: Remodeling and Reintegration Phase (Week 13+ Post-Op)
- Principle: Normalization of proprioceptive function with optimal biomechanics.
- Focus: Maximal medical improvement, endurance training, and full return to activities.
- Activities: We focus on advanced strengthening, power development, and practicing complex functional tasks relevant to your work, sports, or hobbies. This phase emphasizes fine-tuning your hand's capabilities and ensuring optimal endurance. For some, functional bracing might be used during "at-risk" activities.
- Goal: Optimal endurance, normalized tissue structure, and greater than 75% of pre-op wrist ROM and grip/pinch strength, enabling you to meet most critical job demands and return to desired activities.
It’s important to note that while formal therapy might conclude around 8-12 weeks, continued improvements in functional tolerance, mobility, strength, and nerve recovery can be expected for up to nine months post-surgery, largely dependent on your adherence to a home exercise program.
How to Maximize Your Recovery
Maximizing your recovery after hand surgery involves active participation and careful attention to your body's signals. Here's how you can make the most of your post-surgery hand therapy:
- Follow Your Therapist's Instructions Diligently: Your hand therapist is your expert guide. They've crafted a specific plan for you, and adhering to their instructions for exercises, splint wear, and activity modification is crucial. The absolute minimum is a full half-hour of dedicated exercise, five times a day.
- Adhere to Your Home Exercise Program (HEP): Your HEP is designed to reinforce the work done in therapy sessions. Consistency is key. Frequent sets of low-amplitude, high-repetition movements are often safer and more effective than infrequent, high-intensity efforts.
- Manage Swelling with Elevation: Keeping your hand liftd, especially in the early stages, is vital for reducing swelling. When sitting, keep your hand higher than your elbow. When resting or sleeping, use pillows to position your hand above your heart. Even between exercise sets, rest your hand in a posture that avoids dependent swelling.
- Prioritize Proper Nutrition and Hydration: A healthy diet rich in protein, vitamins, and minerals supports tissue repair and overall healing. Staying well-hydrated is also important for cellular function.
- Listen to Your Body: While some discomfort during therapy is normal as you stretch and strengthen, exercises should not provoke sharp or persistent pain. If something feels wrong, communicate it immediately to your therapist. Pushing too hard too soon can lead to setbacks or re-injury.
When to Seek Professional Help
While post-surgery hand therapy is designed to guide you through a smooth recovery, recognize when your body might be signaling a problem that requires immediate professional attention. Contact your surgeon or therapist if you experience any of the following:
- Persistent or Worsening Pain: If your pain doesn't improve with rest, medication, or your rehabilitation program, or if it suddenly gets worse, it's a red flag.
- Severe Swelling That Doesn't Subside: Some swelling is normal, but if it's excessive, doesn't decrease with elevation and ice, or is accompanied by increased pain or tightness, it could indicate a complication.
- Loss of Function or Movement: A sudden or progressive inability to move your hand or fingers, or a significant decrease in your range of motion, is a serious concern.
- Signs of Infection: Look out for increased redness, warmth, pus, foul odor, or fever. These require immediate medical evaluation.
- Numbness or Tingling That Worsens: While some nerve sensations can be normal during healing, increasing numbness, tingling, or weakness could indicate nerve compression or damage.
Frequently Asked Questions about Post-Surgery Hand Therapy
We understand you likely have many questions as you start on your recovery journey. Here are answers to some of the most common inquiries we receive about post-surgery hand therapy:
How long does hand therapy typically last after surgery?
The duration of post-surgery hand therapy is highly individualized and depends on several factors, including the type of surgery you had, the severity of your initial injury, your personal healing rate, and your dedication to your home exercise program.
Generally, you can expect formal, in-clinic therapy to last anywhere from 8 to 12 weeks. For example, after an Open Carpal Tunnel Release, formal therapy might be delayed by 1 to 3 weeks initially and then continue for about 8 weeks. However, this doesn't mean your recovery stops there. Significant improvements, particularly in loosening scar tissue and regaining maximal function, can continue for up to 6 months, and even up to 9 months post-surgery for some conditions, especially with consistent home exercise compliance.
Our goal is to equip you with the tools and knowledge to manage your recovery long-term, ensuring you continue progressing towards your maximal medical improvement even after your formal therapy sessions conclude.
Will hand therapy be painful?
It's a common concern, and we want to be clear: while some discomfort or soreness is a normal part of the healing and rehabilitation process, post-surgery hand therapy should not be excruciatingly painful. Our guiding principle is that exercises should not provoke sharp or unbearable pain.
We work carefully within your comfortable limits, gradually increasing intensity as your body heals and adapts. You might experience some stretching sensations, muscle fatigue, or mild soreness, especially as we work to improve range of motion or strengthen weakened muscles. This is a sign that your tissues are adapting.
Communication with your hand therapist is absolutely key. If you experience pain that feels too intense, persistent, or sharp, tell us immediately. We have various techniques, including manual therapy, modalities like heat or cold, and desensitization for nerve sensitivity, to help manage discomfort and ensure your therapy is effective without causing undue suffering.
What's the difference between a Physical Therapist and a Certified Hand Therapist (CHT)?
The distinction between a general physical therapist (PT) and a Certified Hand Therapist (CHT) is an important one, especially when dealing with the intricate complexities of the hand and wrist.
- Physical Therapists (PTs) are healthcare professionals trained to diagnose and treat movement dysfunctions throughout the entire body. They have a broad scope of practice, helping patients recover from injuries, manage chronic conditions, and improve overall physical function.
- A Certified Hand Therapist (CHT) is a specialized credential held by either a physical therapist or an occupational therapist. To become a CHT, an individual must:
- Be a licensed physical therapist or occupational therapist.
- Accumulate a minimum of 4,000 hours of direct clinical experience specifically in hand and upper extremity therapy.
- Complete extensive continuing education in the field.
- Pass a rigorous certification examination.
- Maintain their certification every five years through ongoing advanced training.
This advanced certification means CHTs possess a unique depth of knowledge in the anatomy, biomechanics, and pathology of the hand, wrist, elbow, and shoulder. They are experts in designing and implementing highly specialized treatment plans for complex upper extremity conditions and post-surgery hand therapy. While all our therapists are highly skilled, a CHT brings a level of focused expertise that is invaluable for optimal hand recovery.
Conclusion: Take the Next Step in Your Hand Recovery Journey
Your hand is a marvel of engineering, essential for nearly every aspect of your daily life. After surgery, starting on a dedicated post-surgery hand therapy program isn't just recommended—it's absolutely critical for restoring its remarkable function. We've seen how a comprehensive, custom approach, combined with your commitment, can make all the difference in achieving the best possible outcomes.
Getting a good result from surgery has a lot to do with the therapy that comes after. Excellent results are seen in well-motivated and dedicated patients who work hard with their daily home therapy. By actively participating, diligently following your therapist's guidance, and understanding the phased nature of healing, you can regain strength, improve flexibility, reduce pain, and ultimately return to the activities you love.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we offer holistic physical therapy services, focusing on thorough evaluation, effective healing, and sustainable strengthening. Our unique hands-on approach ensures personalized care, guiding you through each step of your recovery journey. Don't let stiffness, pain, or limited mobility define your post-surgery experience.
Are you ready to take control of your recovery and open up the full potential of your hand? Start your specialized hand therapy in Brooklyn today with Evolve Physical Therapy + Sports Rehabilitation. We're here to help you evolve past your injury.
Get Strong, Brooklyn Style: A Local's Guide to Strength and Conditioning
Why Brooklyn Strength and Conditioning Is Different

Brooklyn strength and conditioning offers a unique approach to fitness that prioritizes building real strength, understanding your body, and making exercise a sustainable part of your life—not just another item on your to-do list. Whether you're looking to prevent injuries, improve athletic performance, or simply move better in your daily activities, Brooklyn's fitness landscape combines expert coaching with a supportive community atmosphere.
Brooklyn's strength and conditioning scene stands out because it focuses on learning about your body rather than just burning calories. The prevailing philosophy emphasizes getting stronger over getting skinnier. This means you'll work on understanding alignment, building flexibility, and developing body awareness alongside traditional strength gains.
The training programs blend multiple disciplines—kettlebell work, Pilates-based stability, functional movement, and mobility training—creating a holistic approach that reduces injury risk while building real-world strength. Many facilities cap class sizes, ensuring coaches can provide personal attention to your form and progress.
What makes Brooklyn different is the community aspect. These aren't impersonal big-box gyms where you're just another number. You'll find coaches with diverse backgrounds in dance, martial arts, yoga, and physical therapy who take time to understand your specific needs—whether you're dealing with chronic pain, recovering from injury, or training for a specific sport.
I'm Lou Ezrick, a physical therapist with nearly two decades of experience helping Brooklyn residents build strength, recover from injuries, and optimize their movement patterns through Brooklyn strength and conditioning programs at Evolve Physical Therapy. My approach combines manual therapy expertise with functional strength training to address not just symptoms but the root causes of dysfunction, helping active individuals like you maintain your fitness while preventing future injuries.
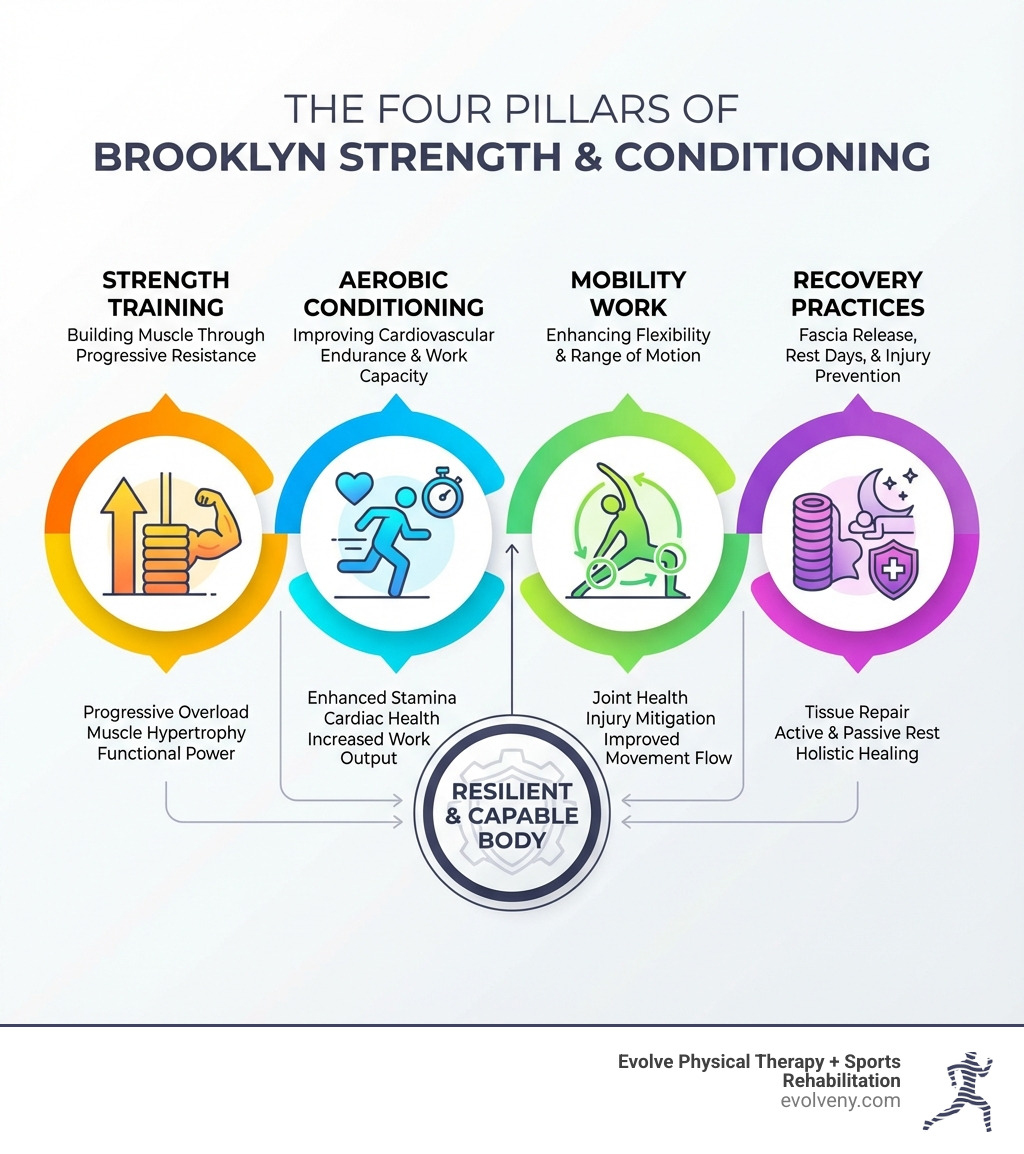
The Core of Brooklyn Strength and Conditioning: What to Expect
When we talk about Brooklyn strength and conditioning, we're not just discussing lifting weights or running on a treadmill. We're embracing a comprehensive philosophy that aims to make you stronger, more resilient, and more confident in your body. This approach integrates various methods to ensure balanced development and long-term health.
At its heart, Brooklyn strength and conditioning is about understanding your body's capabilities and pushing its boundaries safely and effectively. It's about developing strength, improving body awareness, and integrating fitness seamlessly into your lifestyle. The goal isn't just to look good, but to feel good, move well, and perform optimally in all aspects of your life. We believe that structured training, custom to your individual needs, is the cornerstone of preventing injuries and enhancing overall athletic performance. This holistic view ensures that every session contributes to your physical and mental well-being, fostering a supportive community environment where everyone feels empowered.
The Guiding Philosophy: More Than Just a Workout
The philosophy that underpins Brooklyn strength and conditioning champions the idea of "strength over skinny." This isn't about chasing fleeting aesthetic goals, but about building genuine, functional strength that empowers you in your daily life. At Evolve Physical Therapy, we believe the goal should be to make you strong, not just to make you skinny. This sentiment is at the core of our approach.
We believe that true fitness starts with a strong mind-body connection. It's about learning how your body moves, understanding proper alignment, and developing flexibility and stability. This means engaging with fitness as an integral part of your life, not just another chore on your "should list." Our vision at Evolve is to help you cultivate a sustainable relationship with exercise. This involves personalized coaching, fostering accountability, and ensuring that your training program adapts as you progress. We're here to guide you in developing a deeper understanding of your physical self, changing how you perceive and engage with movement.
Key Benefits of a Consistent Program
Starting on a consistent Brooklyn strength and conditioning program offers a wealth of benefits that extend far beyond the gym. We've seen countless individuals transform their lives through dedicated practice, experiencing improvements in both their physical and mental well-being.
Here are some of the profound advantages you can expect:
- Building Muscle and Increasing Endurance: Regular strength training stimulates muscle growth, leading to increased power and a more efficient metabolism. Coupled with aerobic conditioning, you'll find your stamina improving, whether you're tackling a marathon or simply climbing stairs.
- Improved Body Mechanics and Injury Prevention: A well-structured program focuses on proper form and movement patterns, which is crucial for preventing injuries. By strengthening supporting muscles and correcting imbalances, we help you move more efficiently and reduce the risk of strains, sprains, and chronic pain. This is particularly vital for athletes looking to refine their technique and avoid common sport-specific injuries.
- Improved Athletic Performance: For those with athletic aspirations, strength and conditioning is the key to open uping your full potential. Whether you're aiming for faster run times, higher jumps, or more powerful swings, our programs are carefully designed to improve your speed, agility, and explosiveness.
- Increased Confidence and Mental Resilience: There's an undeniable boost in confidence that comes with feeling stronger and more capable. Overcoming physical challenges in the gym builds mental fortitude, teaching you discipline, perseverance, and a positive outlook that spills over into all areas of your life.
- Long-Term Health and Quality of Life: Consistent strength training contributes significantly to bone density, joint health, and overall longevity. It helps manage weight, improves sleep quality, and can even reduce the risk of chronic diseases, ensuring you maintain an active and independent lifestyle for years to come.
Finding Your Fit: Types of Training Programs in Brooklyn
The vibrant Brooklyn strength and conditioning scene offers a diverse array of training programs, ensuring there's a perfect fit for everyone, regardless of your experience level or specific goals. From personalized one-on-one coaching to energetic group classes, we're dedicated to helping you find the environment where you can thrive.

When considering your options, it’s helpful to understand the differences between popular formats like small group training and personal training. Each has its unique advantages in terms of cost, personalization, and the social environment it provides.
| Feature | Small Group Training (SPT) | Personal Training (One-on-One) |
|---|---|---|
| Cost | More efficient; two to three SPT sessions can be less than one personal training session. | Higher per-session cost, but intro packs offer value (e.g., $330 for 3 sessions). |
| Personalization | Capped at 4 people, ensuring significant personal attention and form correction. | Fully individualized program custom exactly to your goals and needs. |
| Social Environment | Supportive community, shared motivation, sense of camaraderie. | Focused, private setting; ideal for specific needs or those who prefer individual attention. |
| Session Length | Typically 55 minutes. | Usually 60 minutes. |
| Progress Tracking | Consistent monitoring through coach feedback and tracking tools. | Direct coach-client feedback and adjustments. |
Functional Strength and Stability
Many of the most respected Brooklyn strength and conditioning programs emphasize functional strength and stability. This approach focuses on movements that mimic real-life activities, improving your ability to perform daily tasks with ease and reducing the risk of injury. We prioritize core strength, flexibility, and proper alignment, which are fundamental to all physical activity.
Our programs often incorporate bodyweight exercises, resistance bands, and other functional equipment to build strength from the ground up. Pilates-based strength and stability training, for example, is a cornerstone of this approach. It's not your typical Pilates class; it integrates elements of Alexander Technique, dance, and yoga to help you connect with your body, improve flexibility, and develop deep core stability. Whether you're just starting out or looking to refine your movement, introductory workshops can address specific concerns like tight hamstrings or low back pain, laying a crucial foundation for more advanced training.
Kettlebell and Free Weight Training
For those looking to build foundational strength, develop power, and improve coordination, kettlebell and free weight training are invaluable components of Brooklyn strength and conditioning. These modalities offer a dynamic and effective way to achieve your fitness goals, from increasing muscle mass to enhancing overall athleticism.
Programs often range from beginner-level classes, which focus on basic movements and proper form, to more advanced sessions for intermediate and experienced practitioners. The beauty of kettlebell training lies in its ability to provide progressive overload, meaning you can continually challenge your body as you get stronger. We guide you through mastering movements and patterns using free weights, machines, and bodyweight, ensuring you build strength safely and effectively. Our programs often combine kettlebell-based strength and conditioning with Pilates-based stability, offering a comprehensive approach that builds physical confidence.
Specialized Offerings at Evolve
At Evolve Physical Therapy, our Brooklyn strength and conditioning offerings are deeply integrated with our expertise in physical therapy and sports rehabilitation. We specialize in catering to individuals with specific needs, whether that's enhancing athletic performance, recovering from an injury, or managing chronic pain.
Our specialized programs include:
- Sports Performance Training: We work with athletes across various disciplines, designing personalized strength and conditioning programs that focus on injury prevention and refining proper mechanics. Our approach involves detailed movement analysis, including gait analysis, to identify and correct technique flaws. We help athletes like baseball players improve their swing power or football players improve leg strength by tailoring exercises to their specific sport and goals. We believe physical therapy isn't just for rehabilitation; it's a proactive measure for performance improvement.
- Post-Rehabilitation Strength Programs: For those recovering from injuries or surgery, we provide a seamless transition from physical therapy to structured strength training. Our hands-on approach ensures that workouts are adapted for any physical restrictions, focusing on scar tissue healing and rebuilding strength safely. We offer pre-operative physical therapy to prepare your body for surgery and comprehensive post-operative rehabilitation to ensure a prompt and lasting recovery.
- Mobility and Flexibility Classes: Recognizing the importance of range of motion and tissue health, we offer classes and techniques focused on improving mobility. These are crucial for preventing future injuries and enhancing overall movement quality.
- Custom Coaching: Our coaches, with diverse backgrounds in physical therapy, sports science, and various movement modalities, provide individualized attention. We create a plan based on your unique needs and goals, ensuring that every session is purposeful and effective.
- Progress Tracking with Evolve’s In-House Tools: We use advanced tools and methodologies to track your progress, allowing us to continuously adapt your program for optimal results. This data-driven approach ensures you're always moving forward efficiently and safely.
Getting Started on Your Strength Journey
Taking the first step into a new Brooklyn strength and conditioning program can feel daunting, but we'vemade it as welcoming and straightforward as possible. Our goal is to understand your unique aspirations and guide you toward a program that will truly make a difference.

The best way to begin is often with an introductory consultation or an "intro pack." These initial sessions are designed for us to get to know each other, discuss your health and wellness goals, and start building a personalized program custom just for you. We believe in setting clear goals from the outset and conducting fitness assessments to establish a baseline. This ensures that your journey is not only effective but also measurable, allowing you to see your progress and celebrate your achievements.
Finding the Right Brooklyn Strength and Conditioning Program for You
Choosing the right Brooklyn strength and conditioning program depends heavily on your current fitness level, personal goals, and any specific needs you might have. Are you a beginner looking to build foundational strength, or an experienced athlete aiming to break through a plateau?
Many facilities offer introductory sessions or consultations to help you determine the best fit. At Evolve, we can help you identify which class series or training style aligns with your objectives. We encourage trying out intro sessions as a "one-off" consultation with a coach. This gives you the opportunity to experience the coaching style, understand the philosophy, and ensure it resonates with you.
The importance of qualified coaches cannot be overstated. Look for coaches with diverse backgrounds—those who bring expertise from physical therapy, sports science, yoga, dance, or martial arts. Their varied knowledge ensures a holistic approach to your training, addressing not just strength but also mobility, stability, and injury prevention. At Evolve Physical Therapy, our team's extensive experience means you're always in capable hands, receiving guidance that is both expert and caring.
Understanding Pricing and Packages
Investing in your health and strength is a decision that pays dividends, and we strive to make our Brooklyn strength and conditioning programs accessible through transparent pricing and flexible package options. While intro packs offer a fantastic way to begin, understanding the full pricing structure helps you plan your long-term fitness journey.
Introductory pricing, such as our 3 One-Hour One-on-One Sessions for $330, is designed to give new clients a comprehensive start. After these initial sessions, you can choose from various packages that offer increasingly better per-session value:
- Single Session: For those who prefer flexibility or want to try a specific class, single sessions are typically $60.
- 6-Pack: A bundle of 6 sessions costs $360, bringing the per-session price to $60.
- 12-Pack: Opting for 12 sessions costs $660, reducing the per-session rate to $55.
- 24-Pack: Our most cost-effective option, a 24-pack is $1,200, making each session just $50.
For those looking for ultimate flexibility, drop-in rates are available for open gym access or single classes, typically priced at $25. Additionally, for consistent, personalized support, monthly private session memberships are available after your initial introductory package. We also offer efficient semi-private training (SPT) where two to three weekly SPT sessions are less than the price of one weekly personal training session, making it a highly effective way to meet your fitness goals with focused attention.
Beyond the Reps: Recovery and Specialized Training
At Evolve Physical Therapy, we understand that Brooklyn strength and conditioning is about more than just pushing your limits during a workout. It's also about what happens between sessions: recovery, restoration, and addressing specific physical needs. True progress and longevity in fitness hinge on incorporating these crucial elements into your routine.
Our holistic approach emphasizes the importance of recovery as an active part of your training. This includes restorative services, dedicated mobility work, and injury prevention techniques that complement your strength building. We also recognize that nutrition plays a vital role, and guidance on eating well can significantly impact your energy levels and results. Whether you're dealing with chronic pain, recovering from surgery, or simply aiming to optimize your well-being, we integrate specialized strategies to support your body's healing and adaptation processes.
Restorative Practices for Longevity
To ensure your body can keep up with the demands of Brooklyn strength and conditioning, we place a strong emphasis on restorative practices. These techniques are designed to improve recovery, reduce muscle soreness, improve flexibility, and ultimately contribute to your long-term physical health.
One highly effective method we champion is the use of myofascial release techniques. This involves guided self-massage using tools like foam rollers and massage balls. It's designed to alleviate chronic tension, improve tissue hydration, and provide significant pain relief and injury prevention. We offer workshops to teach you these valuable tools for ongoing self-care and can demonstrate targeted applications for your specific needs.
Beyond self-massage, we integrate mobility classes into our offerings. These sessions, sometimes as short as 30 minutes, focus on improving your range of motion and joint health. We also explore concepts like "Anti-Anxiety Cardio," which combines gentle movement with mindful breathing to reduce stress and promote overall well-being. These practices are essential for maintaining a supple, resilient body that can withstand the rigors of consistent training. For those looking for props to improve their self-care routine, we can provide recommendations and resources.
Specialized Brooklyn Strength and Conditioning for Recovery
One of the most impactful aspects of Brooklyn strength and conditioning at Evolve Physical Therapy is our ability to cater to individuals with specific needs, such as injury recovery or chronic pain. Our expertise as physical therapists allows us to adapt and personalize programs, ensuring that your strength journey is safe, effective, and truly transformative.
We have extensive experience working with clients experiencing chronic pain and physical restrictions. Our approach often involves movement therapy and neuro-repatterning, which help to retrain the body's movement patterns and alleviate discomfort. We understand the complexities of conditions like sciatica, carpal tunnel syndrome, and various joint pains, and we use advanced technologies and therapeutic modalities to address them. Our philosophy is to empower chronic pain sufferers to be agents in their own breakthrough, rather than solely reliant on medical providers. This is the core of our ethos at Evolve.
For those recovering from surgery, our pre- and post-surgical rehabilitation programs are critical. We address scar tissue healing and adapt workouts to gently rebuild strength and mobility. We can also support clients through significant life changes like pregnancy and birth, ensuring safe and effective movement throughout. Physical therapy is a non-invasive, drug-free method of relieving pain and restoring function, making it an excellent first intervention. We analyze the whole body, not just the area of concern, to create individualized treatment plans for prompt and lasting recovery. With our specialized knowledge, we can help you steer challenges, regain function, and build strength in a way that truly supports your body's healing process.
Conclusion: Build Your Strength, Find Your Community
As we've explored, Brooklyn strength and conditioning offers a distinctive and highly effective approach to fitness. It's a philosophy that champions genuine strength over fleeting ideals, deep body awareness over superficial gains, and sustainable practices over quick fixes. What truly sets it apart is the unwavering commitment to fostering a supportive community, where individuals are encouraged, challenged, and celebrated every step of the way.
At Evolve Physical Therapy, we are proud to embody this Brooklyn spirit. Our mission is to help you build your strength, recover with resilience, and find a lasting sense of well-being. We believe that by understanding your body, engaging in consistent and intelligent training, and embracing personalized care, you can achieve remarkable results and integrate fitness as a joyful, empowering part of your life.
If you're ready to take the first step towards a stronger, more confident you, we invite you to connect with us. Let us guide you on a journey where physical therapy meets cutting-edge strength and conditioning, right here in the heart of Brooklyn.
Learn more about sports rehabilitation physical therapy in Brooklyn
An Essential Guide to Physical Therapy for Herniated Discs
Your Path to Relief: Understanding Physical Therapy for Herniated Discs

If you're dealing with back or neck pain, you might be searching for effective solutions. Physical therapy for herniated discs is often the most recommended first step. It's a non-surgical approach focused on healing and strengthening your spine.
Here’s what physical therapy for a herniated disc aims to do:
- Reduce nerve pressure: Easing pain and discomfort.
- Build strength: Targeting muscles that support your spine.
- Improve flexibility: Restoring natural movement and range of motion.
- Encourage natural healing: Helping your body recover.
- Educate you: Teaching you how to prevent future issues.
Living with a herniated disc can feel like a constant burden. The pain isn't just physical; it brings frustration and worry about long-term limitations. You might wonder if surgery is your only option. However, what some call a "slipped disc" is more accurately a herniated disc. The good news is that many people find relief without surgery. In fact, research shows that 70-90% of patients recover significantly with physical therapy alone. This guide will walk you through how physical therapy can be your path to recovery and a pain-free life.
Louis Ezrick, founder of Evolve Physical Therapy, has nearly two decades of experience helping patients with physical therapy for herniated discs and other complex musculoskeletal conditions. His expertise in manual therapy and holistic movement optimization has guided countless individuals toward pain relief and improved function.
Understanding Herniated Discs: Causes, Symptoms, and Diagnosis
Let's get to know your spine a little better! It's an amazing structure, filled with bones, nerves, and soft tissues that let you move, bend, and twist through life. Tucked between your vertebrae (those bony blocks that make up your spine) are special cushions called intervertebral discs. Think of these discs like little shock absorbers. Each one has two main parts: a tough, outer ring, which we call the annulus fibrosus, and a soft, gel-like center, known as the nucleus pulposus. Imagine a jelly donut – the annulus is the bread, and the nucleus is the delicious jelly inside!
A herniated disc happens when that soft, jelly-like center pushes out through a tear or weak spot in the tougher outer ring. When this happens, it can press on nearby nerves or even the spinal cord, leading to a whole host of uncomfortable symptoms like pain, numbness, or weakness. It's a pretty common issue, and while it can affect any part of your spine, it most often shows up in your lower back (lumbar spine) or your neck (cervical spine). Knowing what's going on is the first step toward feeling better!

What Causes a Disc to Herniate?
Have you ever wondered why a disc might decide to herniate? It often feels like it comes out of nowhere, but usually, it's the result of several things adding up over time. One of the biggest players is simply aging – a natural process where our discs can lose some of their water content and flexibility, making them a bit more prone to wear and tear. This is often called degenerative changes.
But age isn't the only factor! Improper lifting techniques, like bending from your waist instead of your knees, can put immense stress on your lower back. Sudden twisting or pressure from quick, unexpected movements can also cause the disc's outer layer to tear. Activities that involve repetitive strain or high-impact sports can gradually wear down your discs. Even something as common as poor posture, whether you're sitting or standing, can slowly stretch and weaken the discs over time. And don't forget obesity; carrying extra weight, especially around your tummy, adds more stress to your spinal discs, which can speed up that wear and tear. Research into the mechanical aspects of disc injury further shows us how different forces and movements contribute to disc damage, underscoring the importance of proper body mechanics.
Recognizing the Symptoms
The tricky thing about herniated disc symptoms is how much they can change from person to person. It all depends on where the disc is affected and if it's pressing on a nerve. Some folks are even lucky enough to have a herniated disc and not feel a thing! But for many, the signs are clear and can really impact their daily life.
If your herniated disc is in your lower back (lumbar spine), you might experience:
- Sciatica: This is a classic one! It's when the disc irritates the sciatic nerve, causing radiating pain, numbness, tingling, or weakness that travels from your lower back, through your buttocks, and all the way down one leg. It can feel like a sharp, burning, or electrical sensation.
- Leg pain: This discomfort can sometimes extend right into your foot.
- Numbness and tingling: You might feel "pins and needles" or a loss of sensation in your leg or foot.
- Muscle weakness: You might notice difficulty lifting your foot (sometimes called "foot drop") or general weakness in your leg muscles.
When the herniated disc is in your neck (cervical spine), the symptoms often show up differently:
- Neck pain: You might feel a dull ache or sharp pain right in your neck.
- Arm pain: This pain can travel from your neck, through your shoulder, and down one arm, sometimes even reaching your hand and fingers. It can feel like a shooting pain.
- Numbness and tingling: Similar to the leg, you might get these sensations in your arm, hand, or fingers.
- Muscle weakness: You could find it harder to grip objects or notice weakness in your arm muscles.
Important Red Flag Symptoms – When to Seek Immediate Medical Attention: While most herniated discs respond well to physical therapy for herniated discs and other conservative care, there are some serious "red flag" symptoms that need urgent medical attention. These include:
- Cauda Equina Syndrome: This is rare but serious. It means the nerves at the very end of your spinal cord are being compressed. Watch out for new or worsening loss of bowel or bladder control, numbness in your inner thighs, buttocks, or genital area (this is called "saddle anesthesia"), and severe weakness in both legs. If you notice any of these, please seek emergency medical help right away.
- Progressive weakness: Any rapidly worsening muscle weakness in your arms or legs is also a cause for immediate concern.
If you're ever unsure about your symptoms, or if they feel severe, it's always best to chat with a healthcare professional. For more detailed information on nerve-related symptoms, you can also check out resources like When to see a doctor for a pinched nerve.
How a Herniated Disc Is Diagnosed
When you come to see us at Evolve Physical Therapy in Brooklyn, our first step is always to truly understand your unique situation. Diagnosing a herniated disc is a careful process, and it typically starts with a thorough evaluation, not just a quick glance. Here's what that usually involves:
- Patient History: We'll have a good chat! We'll ask you all about your symptoms – when they started, what makes them better or worse, and how they're affecting your daily life. We'll also cover your general health, lifestyle, and any medications you might be taking.
- Physical Examination: Our expert physical therapists will gently check your back or neck for tenderness, observe your posture, and assess how well you can move. We might ask you to perform certain movements to see how your body responds.
- Neurological Tests: This is a key part! We'll check your reflexes and strength testing, along with sensation in the areas where you're feeling symptoms. This helps us look for any signs that a nerve might be compressed or irritated.
- Range of Motion Assessment: We'll measure how far you can comfortably move your neck or back in different directions.
- Special Tests: Sometimes, we use specific tests, like the Straight Leg Raise for lower back issues, to help pinpoint nerve irritation.
- Imaging Studies: While our detailed physical exam and your medical history often give us a clear picture, sometimes imaging is needed. If your symptoms are severe or persistent, we might recommend working with your physician to get an MRI. An MRI is considered the gold standard because it gives us a clear view of your discs and any nerves that might be affected. X-rays can be helpful to rule out other bone problems, but they don't actually show the discs themselves.
Our goal is to get to the bottom of your pain so we can create the best possible plan for your recovery!
The Core of Recovery: The Role of Physical Therapy for Herniated Discs
When you're dealing with a herniated disc, it can feel like your body is working against you. But here at Evolve Physical Therapy, we believe in empowering your body's natural healing powers. That's exactly where physical therapy for herniated discs truly shines! It's not just a "try it first" option; it's often the first-line treatment recommended by top spine specialists and rehabilitation experts. Why? Because it works, and it's built around your body's ability to recover.
The success rate for conservative treatments like physical therapy is truly impressive. Many studies show that nearly 90% of patients with lumbar disc herniation improve within six weeks using physical therapy. Even better, 70-90% see meaningful recovery without surgery at all. This isn't just about quick fixes; the long-term outcomes for physical therapy and surgery are often quite similar when you look at them one to two years down the road.
Our approach centers on helping you in several key ways:
- Pain Centralization: We work to reduce nerve pressure. This often means encouraging your pain to move away from your arms or legs and back towards your spine. This process, called centralization, is a great sign of recovery!
- Reducing Nerve Pressure: Through specific exercises and gentle techniques, we aim to create more space around those irritated nerves, which helps ease your discomfort.
- Improving Mobility: We help you regain your natural range of motion. This allows you to move more freely and comfortably in your daily life.
- Patient Education: This is a big one! We teach you how to move safely, maintain good posture, and manage any symptoms at home. This empowers you to actively participate in your recovery and learn how to prevent future issues.
For most people, physical therapy for herniated discs is a safer, lower-cost starting point compared to surgery. It comes with minimal risks and gives your body the best chance to heal itself. Many patients start with physical therapy and never need to consider surgery at all!
How a Physical Therapist Creates Your Treatment Plan
When you come to Evolve Physical Therapy, your journey begins with a thorough initial evaluation. We don't believe in one-size-fits-all solutions. Our expert physical therapists will listen carefully to your story, understand your pain, and assess how it affects your life.
Based on this, we'll work with you to set clear, personalized goal settings. Maybe you want to walk without pain, lift your grandchild, or get back to your favorite sport. We'll build a plan to get you there. Your treatment plan will likely include strategies for pain and inflammation control, using gentle methods to calm down irritated tissues. We'll also use manual therapy techniques—think hands-on care like massage, mobilization, or gentle stretches—to improve how your joints and muscles move. Then, we'll carefully design a therapeutic exercise prescription just for you. Finally, we'll provide crucial posture and body mechanics education. Learning how to move correctly can be a game-changer for protecting your spine in the long run.
Finding the right physical therapist is key to your success. If you're ever looking for a qualified professional, resources like Finding a qualified physical therapist can help.
Key Components of Physical Therapy for Herniated Discs
Your physical therapy program will involve a mix of techniques designed to heal and strengthen. We often start with passive treatments to help manage pain and inflammation. This might include applying ice to reduce swelling, heat to relax muscles, or using a TENS unit (Transcutaneous Electrical Nerve Stimulation) for pain relief.
Once pain is better controlled, we move to active treatments. These are exercises you perform yourself, and they're crucial for long-term recovery. We'll focus on core stabilization exercises to build a strong foundation for your spine, as well as flexibility exercises to restore movement. You might learn Directional preference exercises, often part of the McKenzie Method, which involves specific movements that help centralize your pain. Motor Control Exercises help you learn to use your muscles more effectively, and we'll also focus on strengthening supporting muscles around your spine to provide better stability and protection.
Comparing PT to Surgery and Other Options
It's natural to wonder about all your options when facing a herniated disc. As we mentioned, studies have shown that the long-term outcomes of physical therapy versus surgery are often similar at the 1-2 year mark. This is powerful information, suggesting that a less invasive approach can be just as effective for many.
So, when is surgery necessary? Surgery is typically considered when conservative care, like physical therapy, hasn't provided sufficient relief after a reasonable period (usually 6-12 weeks), or if you experience those "red flag" symptoms we discussed earlier, such as rapidly worsening muscle weakness or loss of bowel/bladder control. For most other cases, physical therapy is the recommended first step.
You might also discuss the role of medications and injections with your doctor. These can be helpful tools to manage pain and inflammation in the short term, allowing you to participate more effectively in physical therapy. However, they typically don't address the underlying mechanical issues in the same way that physical therapy does. For more insights on conservative treatment approaches, the WFNS spine committee recommendations on conservative treatment offer valuable guidelines.
Beyond the Break: Your Guide to Orthopedic Physical Therapy
Understanding Orthopedic Surgery Physical Therapy

When recovering from an injury or surgery, understanding the path back to full health is key. Orthopedic surgery physical therapy is a specialized area of physical therapy focused on helping you recover function and reduce pain after injuries or operations affecting your bones, joints, muscles, ligaments, and tendons.
Here's a quick look at what it involves:
- What it is: Specialized physical therapy for your musculoskeletal system. It helps you get back to normal after injuries or surgery involving bones, joints, muscles, ligaments, and tendons.
- Key Goals: To restore strength, increase mobility, manage pain, and improve overall function and quality of life. It also aims to prevent re-injury.
- Difference from General PT: Orthopedic physical therapists have extra training and education beyond a general physical therapy degree. This makes them experts in musculoskeletal conditions and post-surgical care.
Orthopedic conditions can disrupt your ability to move freely and live without pain. Whether it's a sports injury, a fracture, or a joint replacement, physical therapy is a necessary step in getting you back on track.
As Louis Ezrick, founder of Evolve Physical Therapy, I’ve spent nearly two decades helping patients with complex recoveries. My expertise in orthopedic surgery physical therapy ensures patients regain function and quality of life. This guide will walk you through this vital part of your recovery journey.
The Goals and Benefits of Post-Surgical Rehabilitation
The goal of orthopedic surgery physical therapy is to help you emerge from surgery stronger, more mobile, and with a better quality of life. Post-surgical rehabilitation is pivotal for restoring function, optimizing your body's potential, and preventing future issues. It's about not just getting back to where you were, but emerging even better.
The Primary Goals of Orthopedic Surgery Physical Therapy
When you begin your orthopedic surgery physical therapy journey, we'll focus on several key objectives to ensure a comprehensive recovery:
- Restoring Range of Motion: After surgery, joints often become stiff. Our therapists use gentle exercises and manual techniques to restore your full range of motion, which is crucial for everyday activities. Early mobilization is key to regaining safe movement and reduces the risk of complications like blood clots and muscular atrophy.
- Muscle Strengthening: Muscles near the surgical site often weaken from disuse. We design targeted strength training programs to rebuild these muscles, providing stability and support to your joints. Physical therapy can help muscles become stronger than before surgery, preventing future injuries.
- Neuromuscular Re-education: This means retraining your brain and muscles to work together efficiently. After surgery, your body's natural movement patterns can be disrupted. We help you regain balance, coordination, and proper movement mechanics.
- Gait Training: If your surgery affected your lower body, learning to walk properly again is a major step. We guide you through gait training, often starting with assistive devices like crutches or walkers, to ensure you move safely and confidently. Our therapists ensure you use these devices correctly to prevent falls.
- Functional Training: The ultimate goal is returning to your daily activities, hobbies, and sports. Functional training mimics these real-life movements, preparing your body for your unique lifestyle, whether that means playing with your grandkids or getting back on the tennis court.
- Pain and Swelling Reduction: Pain is a natural part of recovery, and we have many tools to manage it. We use various modalities and techniques to reduce pain and swelling, making your rehabilitation more comfortable and effective. This can also reduce reliance on pain medications.
Conditions That Benefit from Orthopedic PT
Orthopedic physical therapists treat a wide array of conditions affecting the musculoskeletal system, both pre- and post-surgery. Surgeons often refer patients for physical therapy, sometimes even before considering surgery, depending on the condition.
Here's a list of conditions where orthopedic surgery physical therapy truly shines:
- Sprains and Strains: From a twisted ankle to a pulled hamstring, these common injuries respond well to targeted rehabilitation.
- Arthritis Management: Whether it's osteoarthritis or rheumatoid arthritis, we help manage pain, improve joint function, and maintain mobility.
- Post-Fracture Care: After your bone has healed, physical therapy helps restore strength, flexibility, and function to the affected limb.
- Joint Replacements: Surgeries like knee and hip replacements require intensive physical therapy to ensure the new joint functions optimally.
- Ligament and Tendon Repairs: From ACL reconstructions to rotator cuff repairs, we guide you through the delicate healing process to regain stability and strength.
- Chronic Back and Neck Pain: Often stemming from disc issues, muscle imbalances, or poor posture, physical therapy provides relief and long-term solutions.
- Sports Injuries: Athletes frequently rely on orthopedic PT to recover from injuries and return to their sport safely and at peak performance.
- Balance/Coordination Problems & Instability: We address issues that can lead to falls or hinder confident movement.
- Spinal/Pelvic Disorders: Conditions affecting the spine and pelvis are expertly managed to reduce pain and improve stability.
- Foot/Ankle Pain: Plantar fasciitis, Achilles tendinitis, and other foot and ankle issues are common conditions we treat.
- Prosthetic Training: We help patients learn to use prosthetic devices effectively, integrating them into their daily lives.
A Look Inside Your Session: Techniques and Modalities
Your first orthopedic surgery physical therapy session is a step into a welcoming environment where skilled therapists blend hands-on care with proven techniques, customized for your recovery. Whether you're visiting our Brooklyn clinics in Park Slope, Midwood, or Mill Basin, you'll find a personalized approach centered on your healing.
Your sessions are active. You'll move, stretch, and work through exercises designed for your condition. You'll also learn about your body, your injury, and how to move in ways that protect and strengthen you long-term.

Common Techniques in Orthopedic Surgery Physical Therapy
The foundation of your recovery rests on time-tested techniques like manual therapy. This is hands-on work where your therapist uses skilled movements to mobilize stiff joints, release tight muscles, and reduce tension. It's highly effective for pain management and restoring normal joint function.
Therapeutic exercise forms the backbone of your treatment plan. These are carefully selected exercises that target your specific needs, like rebuilding strength in a replaced knee. We guide you in the clinic and provide a home exercise program so you can progress between visits. Active participation is key to your recovery.
Joint mobilization involves gentle, controlled movements applied to specific joints to restore their natural mechanics and ease stiffness, coaxing them back into their normal rhythm after surgery.
Soft tissue massage techniques help calm muscle spasms, ease pain, and boost blood flow to areas that need healing.
Strength training exercises focus on building functional strength in surrounding muscles, creating a support system that protects your healing tissues and prevents future injury.
Paired with stretching and flexibility work, these exercises help you regain your full range of motion while reducing that tight, uncomfortable feeling that often follows surgery.
Balance and proprioception drills are crucial for retraining your body's awareness of its position in space. This is especially important after lower extremity surgeries to rebuild confidence in your movement and reduce your risk of falls.
One of the most valuable parts of your session is the patient education on body mechanics you'll receive. We teach you how to move properly during daily activities like bending or sitting. These lessons protect your healing tissues and set you up for long-term success.
Advanced and Emerging Adjunct Therapies
Beyond traditional methods, we incorporate innovative techniques to accelerate healing and improve comfort. An update on physical therapy adjuncts in orthopedics highlights how these approaches are changing rehabilitation.
Blood Flow Restriction (BFR) training is a gentle way to build strength early in recovery. By applying a specialized cuff to a limb to partially restrict blood flow during exercise, you can gain muscle strength using much lighter weights. This is ideal when your tissues aren't ready for heavy loading.
Dry needling involves inserting fine needles into tight muscle trigger points to release tension and reduce pain. It's helpful for post-surgical muscle guarding or spasms, helping them relax and function normally. Many patients find it provides relief when other methods haven't.
Cupping therapy is an ancient technique used in modern rehabilitation. By placing cups on the skin to create suction, we can increase blood flow, reduce inflammation, and address soft-tissue restrictions. Many patients find it helps manage pain and improve mobility.
Light therapy (Photobiomodulation) uses specific wavelengths of light to work at a cellular level, reducing pain and inflammation while promoting tissue healing. Kinesio taping provides support without restricting movement. The elastic tape is applied to support muscles and joints, reduce swelling, and improve body awareness of the area.
Heat and ice application remain staples of pain management—heat relaxes tight muscles and improves circulation, while ice reduces swelling and numbs acute pain. Electrical stimulation uses gentle electrical currents to reduce pain, activate muscles, and promote healing by stimulating nerves and muscle tissue.
Orthopedic surgery physical therapy is never one-size-fits-all. We draw from this full toolkit to create a treatment plan that addresses your specific needs, adjusting as you progress.
Your Role in Recovery: How to Maximize Your PT Experience
Your recovery is a team effort. While our skilled therapists at Evolve Physical Therapy provide expert guidance, your active engagement is the secret to success. We've consistently seen that patients who fully invest in their rehabilitation achieve the best outcomes. Think of us as your coaches and you as the star player.
Preparing for Your First Appointment
Preparing for your first orthopedic surgery physical therapy appointment is straightforward. We want you to feel comfortable and ready to make the most of it from the start.
First, let's talk about what to wear. Choose comfortable, loose-fitting clothing that allows you to move freely. Shorts are a great choice for knee or hip work, while a t-shirt or tank top is ideal for shoulder or back issues. The goal is easy access for your therapist and easy movement for you.
Next, remember what to bring. Please have your doctor's referral ready (if your insurance requires one), any recent imaging reports like X-rays or MRIs, and a list of your current medications. Also, jot down any questions you have—no question is too small. Understanding your diagnosis and treatment is a key part of patient education. The more you know about your recovery path, the more empowered you'll feel.
The Importance of a Personalized Treatment Plan
At Evolve Physical Therapy, we know every recovery journey is unique. A "one-size-fits-all" approach doesn't work in orthopedic surgery physical therapy. We craft highly personalized treatment plans for every patient who walks through our Brooklyn clinic doors.
Your first visit includes a thorough initial evaluation and physical examination. We get to know you, your condition, your limitations, and what you hope to achieve. From there, we work together to set realistic and meaningful goals. Whether it's walking through Prospect Park without pain or getting back on the basketball court, your goals drive our plan.
Recovery isn't always a straight line. We'll be continuously monitoring your progress and adjusting interventions as needed. This ensures your plan is always tuned to help you progress safely and effectively. It’s a true collaboration with your therapist, who acts as your expert guide and motivator.

A significant part of your recovery happens outside our clinic walls, which is why adherence to home programs is so important. We provide clear, customized exercises to do at home, empowering you to maintain momentum between sessions. Your dedication is crucial for maximizing results!
Finding the Right Professional Team
Your recovery from orthopedic surgery is a team effort between your orthopedic surgeon and your physical therapist. At Evolve Physical Therapy, we believe in this partnership, building open communication with doctors to ensure coordinated care that follows all post-surgical protocols.
Assessing a Physical Therapist's Credentials
Before you put your trust and your recovery into anyone's hands, it's wise to check their background. We're all about being open and clear, and we want all our Brooklyn patients to feel good about asking about their therapist's qualifications.
First, know that all licensed physical therapists in the U.S. must have a Doctor of Physical Therapy (DPT) degree from a trusted school. This means they've learned a ton about how your body works and how to help it heal. Next, they must hold a State Licensure, meaning they've passed tough exams and follow high professional standards.
But for something as specific as orthopedic surgery physical therapy, you'll want to look for someone even more specialized. Keep an eye out for a Board-Certified Orthopaedic Clinical Specialist (OCS). This is a big deal! It shows they have extra advanced knowledge and skills just for orthopedic conditions. They've often done extra training, like a residency, and passed a really tough exam. The Academy of Orthopaedic Physical Therapy is a great place to learn more about what this special certification means. Don't be shy about asking if your therapist has experience with your specific condition – like your knee replacement or rotator cuff repair. While all OCS therapists are experts, some might have seen more cases just like yours!
The Surgeon-Therapist Partnership
The bond between your orthopedic surgeon and your physical therapist is super important for a truly smooth and effective recovery. Think of them as two halves of a winning team, both focused on you!
Your therapist needs to know all the details about your surgery. This means sharing surgical notes about exactly what was done, any hardware used, and any special things to watch out for. This helps your physical therapist create a rehabilitation plan that's safe and just right for you. Your therapist will also make sure to follow protocols set by your surgeon. These are like a roadmap for your recovery, ensuring everything goes as planned.
Regular chats and progress updates between your therapist and surgeon are key. This way, everyone knows how you're doing, and if any little bumps come up, they can be handled right away. This team approach truly helps in ensuring a seamless recovery, avoiding confusion and making your healing journey as easy as possible. And as your body heals, your needs will change. That's why they work together to adjust the plan based on healing, making sure your exercises keep pace with your progress and you're ready for every new step forward.
Frequently Asked Questions about Orthopedic Physical Therapy
We know you'll have questions as you steer your recovery. After nearly two decades of working with patients across our Brooklyn clinics in Park Slope, Midwood, and Mill Basin, I've heard just about every concern imaginable. Let's tackle the most common ones head-on.
Is physical therapy after surgery supposed to be painful?
It's understandable to worry about pain. The truth is, some discomfort during orthopedic surgery physical therapy is normal, but it shouldn't be torture. Your body has been through a significant event, and we're asking it to move in new ways, which can be challenging.
What we always teach our patients is the difference between "good pain" and "bad pain." Good pain feels like a stretch, a gentle pulling sensation, or muscle fatigue – the kind you might feel after a workout. Bad pain is sharp, shooting, or gets progressively worse. Bad pain is your body's alarm system telling you something isn't right.
Your job is to communicate with your therapist. Always. If something hurts, tell us immediately. We can adjust the exercise, modify the intensity, or use different modalities for pain relief. We have an entire toolbox at our disposal – heat, ice, electrical stimulation, manual therapy techniques – all designed to make your sessions more comfortable and effective.
The importance of consistency can't be overstated. Yes, pushing through mild discomfort (the "good pain" kind) is often necessary for progress. But you should never feel like you're suffering through your sessions. If you are, we need to know so we can adjust your treatment plan.
How long will I need physical therapy after my orthopedic surgery?
This is a common question, and the honest answer is: it depends. Your recovery is as unique as you are.
Several factors influence how long you'll need orthopedic surgery physical therapy. The type of surgery is a big one – a minor arthroscopic procedure will require far less rehabilitation than a total joint replacement or complex ligament reconstruction. Your overall health matters too. Your age, any pre-existing conditions, and your fitness level before surgery all play a role in how quickly your body heals.
Your adherence to the program is often the biggest factor of all. Patients who diligently do their home exercises, follow precautions, and show up consistently to their appointments typically recover faster and with better outcomes.
For typical timelines with common surgeries, knee or hip replacements can range from a few weeks of intensive therapy to several months. Some research suggests that formal therapy beyond eight weeks for knee replacement may not be necessary for all patients to achieve successful outcomes. For hip replacements, home-based exercise programs can be just as effective as outpatient therapy for many people.
ACL reconstruction is typically a longer journey – often six to nine months, sometimes longer if you're planning to return to cutting and pivoting sports. Rotator cuff repairs usually require three to six months, depending on the size of the tear and the surgical approach.
Fracture rehabilitation varies widely based on which bone was broken, how severe the injury was, and whether surgery was needed. For distal radius fractures (wrist), research shows that early therapy within three weeks can improve outcomes, and supervised therapy is particularly recommended for older individuals or those with complications.
What makes an Orthopedic Clinical Specialist (OCS) different?
This question highlights the level of expertise you should expect when choosing a physical therapist for your recovery.
An Orthopedic Clinical Specialist (OCS) is a physical therapist who has dedicated themselves to becoming an expert in orthopedic care. It's not just a fancy title – it represents years of additional training and a serious commitment to excellence.
After earning their Doctor of Physical Therapy degree, an OCS candidate undergoes extensive post-graduate training in orthopedics, often through a clinical residency or fellowship. This provides intensive, mentored experience, similar to the difference between a general practitioner and a medical specialist.
To earn the OCS credential, therapists must pass a rigorous board certification examination that tests their in-depth knowledge of musculoskeletal conditions, rehabilitation techniques, and evidence-based practice. This isn't a test you can cram for – it requires genuine expertise and extensive clinical experience.
What does this mean for you? When you work with an OCS for your orthopedic surgery physical therapy, you're working with a recognized expert who possesses specialized knowledge in the anatomy, physiology, and pathology of the musculoskeletal system. They can provide highly accurate diagnoses and develop more effective treatment plans because they've seen it all and know exactly what works.
The Academy of Orthopaedic Physical Therapy is an excellent resource if you want to learn more about this specialization and what it takes to achieve this level of expertise.
Your Path to a Stronger Recovery
Recovering from surgery is about reclaiming your life. Orthopedic surgery physical therapy is the bridge from the operating table back to the activities you love, changing pain into strength and limitation into freedom.
Throughout this guide, we've explored how physical therapy restores not just your body, but your quality of life. From managing pain and rebuilding strength to improving mobility and preventing future injuries, every session moves you closer to your goals. The process is comprehensive, addressing your physical needs while also empowering you with knowledge about your body and how to care for it long-term.
At Evolve Physical Therapy + Sports Rehabilitation, we've built our practice on a simple belief: healing happens when expert care meets genuine compassion. Our holistic approach means we're not just treating your surgical site – we're looking at your whole body, your lifestyle, and your personal goals. Whether you're recovering from a knee replacement in our Park Slope clinic, rebuilding shoulder strength in Midwood, or regaining mobility after hip surgery in Mill Basin, our team brings the same hands-on dedication to every patient.
Recovering from surgery can feel overwhelming. On days when progress feels slow, you need a team in your corner—one that understands the journey, celebrates your victories, and adjusts your plan as needed.
Our approach combines cutting-edge techniques with old-fashioned care. We take the time to really listen, to understand what matters most to you, and to create a treatment plan that fits your life. From our specialized programs like Rock Steady Boxing for Parkinson's patients (featured on NBC News) to our advanced orthopedic rehabilitation, we're constantly evolving to serve you better.
You've already taken the hardest step by having surgery. Now it's time to finish what you started. Your body is ready to heal, to grow stronger, and to surprise you with what it can do. All it needs is the right guidance and support.
Take the next step in your recovery with post-op physical therapy in Brooklyn. Let's work together to get you back to living your life fully – whether that means playing with your grandkids, returning to your favorite sport, or simply moving through your day without pain. Your stronger recovery starts here.
Is Pediatric PT Right for Your Child? A Comprehensive Guide
Why Understanding Pediatric PT Matters for Your Child's Development

Pediatric pt (pediatric physical therapy) is a specialized service helping children from birth to 21 improve their movement, strength, and participation in daily activities. Whether a child has a developmental delay, an injury, or a diagnosed condition, a pediatric physical therapist works with the family to help them reach their maximum potential for independence.
Pediatric physical therapy addresses a wide range of challenges, including:
- Developmental delays (e.g., not rolling, sitting, or walking on time)
- Neurological and genetic conditions (e.g., cerebral palsy, Down syndrome)
- Orthopedic issues (e.g., sports injuries, torticollis, gait problems)
- Coordination and balance difficulties
As movement experts, pediatric physical therapists use hands-on care, play-based activities, and family education to improve a child's motor skills, strength, and endurance. The ultimate goal is to promote a child's ability to function independently and participate actively in home, school, and community life.
As the founder of Evolve Physical Therapy + Sports Rehabilitation, I've seen how pediatric pt helps children overcome physical challenges. Our patient-first approach supports families in understanding how physical therapy can make a meaningful difference in their child's development.
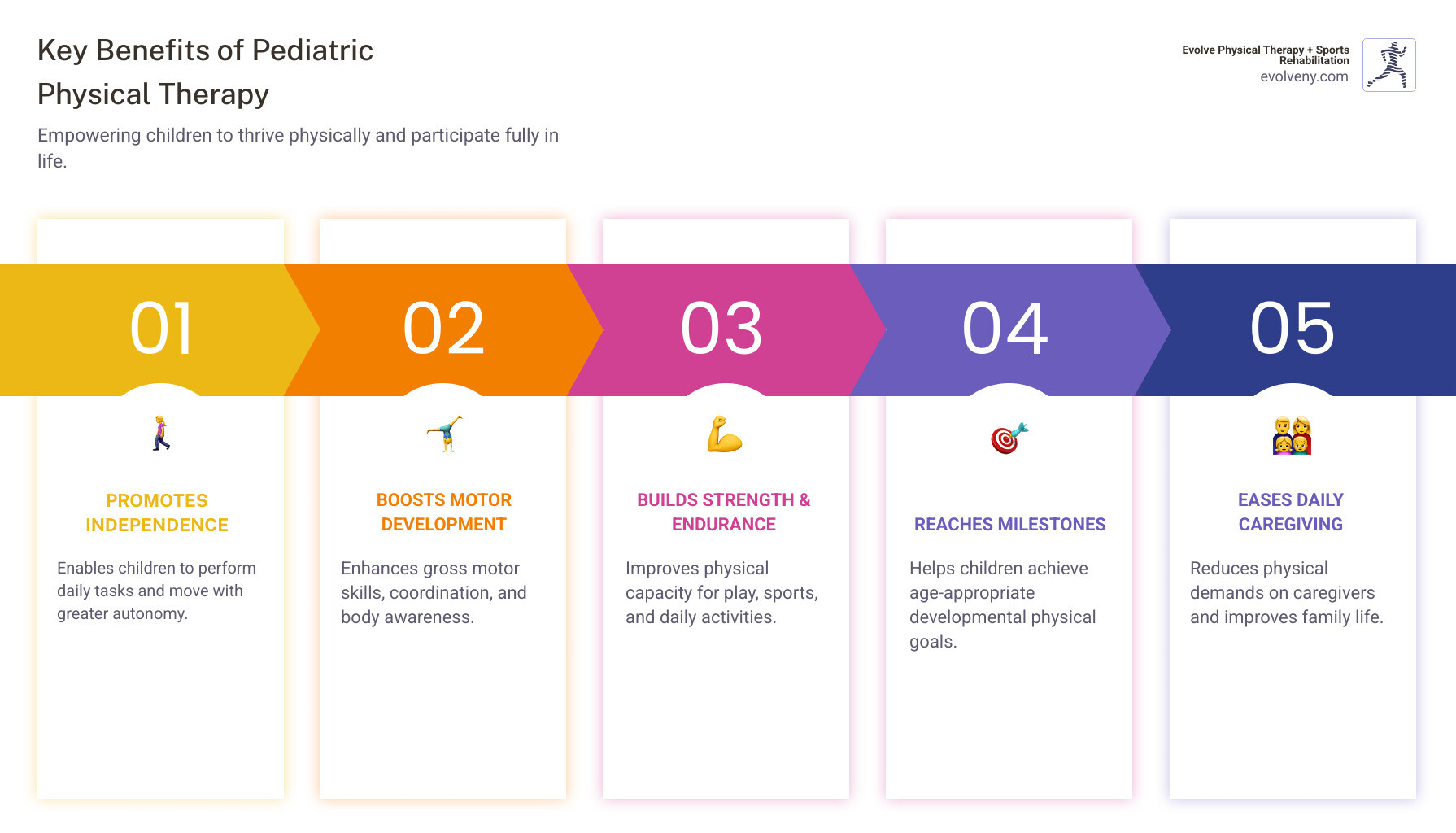
Understanding Pediatric Physical Therapy: Goals and Benefits
While many associate physical therapy with adult rehabilitation, pediatric pt is a specialized field focused on the unique needs of growing bodies. At Evolve Physical Therapy + Sports Rehabilitation, we see ourselves as movement experts for children, from newborns to young adults. Our therapists have specialized knowledge in motor development, body function, and strength, building a foundation for lifelong health.
This specialized care helps children improve range of motion, build strength, and refine movement patterns, making everyday activities easier. In some cases, it can even be an alternative to more invasive treatments. For more general information, you can find resources about pediatric physical therapy at ChoosePT.com.
The Primary Goals of Pediatric PT
The core goal of pediatric pt is to help children reach their maximum potential for independence and participation in life. This is achieved by focusing on several key areas:
- Improving mobility: We help children learn to roll, crawl, walk, and run, building the strength and coordination needed to explore their world.
- Restoring function: After an injury, illness, or surgery, we work to help children regain lost physical abilities.
- Alleviating discomfort: Using hands-on techniques and therapeutic exercises, we help manage pain from injuries or chronic conditions.
- Preventing disability: Early intervention can minimize the progression of disabilities and promote healthier long-term movement patterns.
- Reaching developmental milestones: We focus on fundamental gross motor skills like sitting, standing, and walking, which are the building blocks for all other physical activities.
- Increasing participation: We want children to fully engage in daily life, from playing with friends to keeping up in gym class.
At Evolve Physical Therapy + Sports Rehabilitation, we are committed to helping Brooklyn families achieve these goals. You can find more info about our pediatric physical therapy services on our website.
Long-Term Benefits for Children and Families
The impact of pediatric pt extends far beyond the therapy session, creating lasting positive changes.
Promoting independence is a key benefit, as children gain the self-reliance and confidence to perform daily tasks on their own. This, in turn, leads to easier daily caregiving for families, reducing stress. As children improve their motor skills, they open up new learning opportunities and can better engage in social and academic settings.
Therapy builds strength and endurance, supporting sustained physical activity and preventing fatigue. As children overcome physical obstacles, their confidence soars, making them more willing to try new things. Perhaps most importantly, pediatric pt helps children develop a love for movement, fostering active lifestyles that promote long-term health and well-being.

Does Your Child Need a Pediatric PT? Key Signs and Conditions
As a parent, you are the expert on your child. If you notice they are struggling with movements that seem to come easily to their peers, it may be time to consider pediatric pt. This service is for children from birth to 21 who have developmental delays, injuries, or diagnosed disorders.
In New York, you can often seek a physical therapy evaluation without a physician referral, but it's wise to check your insurance policy's requirements. We offer initial consultations to discuss your concerns and determine if a full evaluation is needed.
Developmental Milestones and Red Flags
While every child develops at their own pace, there are general timelines for key physical skills. Not meeting these milestones can be a red flag.
- Key Milestones: Babies typically roll by 5 months, sit by 7 months, crawl by 8 months, pull to stand by 9 months, and walk independently around 12-15 months.
- When to Seek Help: Consider an evaluation if your child is more than two months behind on a milestone with no sign of attempting it.
Other red flags include:
- Asymmetry or weakness on one side of the body.
- Persistent toe walking after age two.
- Frequent falls or unusual clumsiness compared to peers.
- Difficulty with stairs, climbing, or keeping up during active play.
Trust your instincts. Early intervention can make a tremendous difference, so don't hesitate to ask questions.

Common Conditions Treated by a Pediatric PT
Our therapists in Brooklyn work with children facing a wide variety of physical challenges, tailoring our approach to each child's needs.
- Cerebral Palsy: We work to improve muscle control, improve movement, and prevent joint stiffening.
- Spina Bifida: Therapy focuses on improving mobility, strengthening muscles, and using assistive devices.
- Down Syndrome & Genetic Disorders: We help promote motor development and improve muscle tone.
- Muscular Dystrophy: PT helps maintain muscle function and manage symptoms to improve quality of life.
- Autism Spectrum Disorders: We help improve balance, coordination, and body awareness.
- Torticollis: Gentle stretches and exercises correct an infant's head tilt and prevent related developmental issues.
- Orthopedic Injuries: We help young athletes and active children recover from fractures, sprains, and other injuries. Learn about pediatric sports PT for more on this specialty.
- Developmental Coordination Disorder (DCD): We use task-oriented approaches to improve coordination and motor skills.
- Brain Injuries & Hydrocephalus: Therapy helps restore movement, balance, and coordination.
What to Expect: A Look Inside a Pediatric PT Session
Your first pediatric pt session at Evolve Physical Therapy + Sports Rehabilitation begins with a comprehensive evaluation. Our therapist will observe how your child moves, test their strength and flexibility, and assess their balance and coordination. We'll also discuss your child's health history and your family's specific goals.
Based on this assessment, we create an individualized treatment plan custom to your child. This plan outlines the therapeutic strategies, exercises, and timeline for progress. Our approach centers on hands-on care, where therapists physically guide your child's movements to help them learn new patterns and build strength.
Patient education is also a key component. We'll teach you activities to practice at home, turning daily routines into therapeutic opportunities. This helps ensure progress continues between sessions. For more information, APTA Pediatrics offers family resources that can help you prepare.
The Power of Play in Therapy
The best therapy doesn't feel like work, which is why play is our most powerful tool in pediatric pt. Our therapists are experts at disguising hard work as fun.

We design age-appropriate games that target specific goals. An exercise ball builds core strength, an obstacle course improves motor planning, and tossing bean bags refines hand-eye coordination. These play-based exercises keep children motivated and engaged. By tapping into a child's natural curiosity, we help them build coordination and balance while they are simply having a great time. The skills learned in our clinic, like balance and strength, transfer directly to the playground and home.
Where Does Therapy Happen? From Clinics to Classrooms
While many sessions take place in our welcoming Evolve Physical Therapy + Sports Rehabilitation clinics in Brooklyn—located in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin—pediatric pt is not limited to a clinical setting.
Effective therapy often happens in a child's natural learning environment. This can include:
- Home-based therapy: Especially valuable for infants and young children, allowing therapists to integrate activities into daily routines.
- Child care centers and preschools: Therapists can address needs within the child's educational and social setting.
- School-based services: Under the Individuals with Disabilities Education Act (IDEA), eligible children receive PT at school to help them access their education.
- Hospitals: Critical for children recovering from surgery, illness, or those with complex medical needs.
- Community settings: Therapy can occur in parks or recreational facilities to work on real-world skills.
This flexibility ensures that therapy is a natural part of a child's life, helping skills transfer seamlessly into their everyday world.
The Collaborative Care Model
Effective pediatric pt is a team effort. At Evolve Physical Therapy + Sports Rehabilitation, we use a collaborative care model that brings together families, therapists, and other professionals like pediatricians, teachers, and speech pathologists. This ensures your child receives consistent, coordinated support.
Family-centered care is the heart of our practice. We recognize that you know your child best and view parents as equal partners in the therapeutic process. Through shared decision-making, we develop treatment plans with you, ensuring the goals are meaningful and fit into your real life. Our therapists also serve as advocates, helping you steer healthcare and educational systems to ensure your child's needs are met.
How Therapists Work with Families and Caregivers
You are the most important member of your child's therapy team. We empower you by providing:
- A Home Exercise Program (HEP): We design fun, simple activities that fit naturally into your daily routine, turning playtime or daily tasks into therapeutic moments.
- Guidance on Adapting Toys and Routines: Simple adjustments to how your child sits or plays can significantly impact their development.
- Parent Education: We explain the why behind our methods so you can apply the principles throughout your child's day. We encourage questions and provide clear, jargon-free answers.
- Collaborative Goal-Setting: We work with you to set goals that address your family's priorities and improve your child's quality of life.
We also help coordinate services with other professionals to ensure everyone is on the same page. You can learn more about our approach to pediatric physiotherapy on our blog.
The Experts Behind the Care: Training and Licensing
Providing pediatric pt requires extensive education and specialized training. Every physical therapist holds a Doctor of Physical Therapy (DPT) degree, a three-year post-baccalaureate program. They must also pass a national exam and meet state licensure requirements to practice.
Many therapists pursue further specialization through clinical residencies in pediatrics. The highest level of specialization is becoming a Board-Certified Pediatric Clinical Specialist (PCS), a certification that signifies advanced knowledge and skill. All pediatric physical therapists also engage in ongoing education to stay current with the latest research and best practices. Our team at Evolve Physical Therapy + Sports Rehabilitation brings this expertise and a commitment to patient-first care to every child we see in Brooklyn.
Frequently Asked Questions about Pediatric PT
It's natural to have questions when considering pediatric pt for your child. Here are answers to some of the most common concerns we hear from families in Brooklyn.
What is the difference between pediatric PT and occupational therapy (OT)?
This is a very common question. While pediatric pt and occupational therapy (OT) often work together, they have different focuses.
- Pediatric PT focuses on gross motor skills—the large muscle movements for rolling, sitting, walking, running, and climbing. We work on whole-body movement, strength, balance, and mobility.
- Occupational Therapy (OT) focuses on fine motor skills (like holding a pencil or buttoning a shirt), sensory processing, and activities of daily living (ADLs) like dressing and feeding.
For a child with cerebral palsy, a PT might work on their walking pattern while an OT helps them learn to use utensils. At Evolve Physical Therapy + Sports Rehabilitation, our team coordinates with OTs to provide comprehensive care.
How long will my child need physical therapy?
The duration of pediatric pt is unique to each child. It depends on the condition being treated, its severity, the child's age, and consistency with therapy. A typical frequency is one to two times per week.
Some conditions, like torticollis or a minor sports injury, may only require a few months of therapy. Other children with chronic conditions like cerebral palsy or muscular dystrophy may benefit from ongoing therapy throughout their development to maintain function and adapt to growth.
We conduct regular re-evaluations to track progress and adjust the treatment plan. Consistency with sessions and home exercises is key to making faster progress.
Are pediatric PT services covered by insurance?
Yes, pediatric pt is covered by most private and public health insurance plans, but coverage details vary. It's important to check your specific plan for requirements like co-pays, deductibles, or session limits.
- Private Insurance: Most plans offer coverage, but may require a doctor's referral or pre-authorization. Our administrative team can help you verify your benefits.
- Public Programs: Medicaid and Child Health Plus in New York provide coverage for pediatric PT.
- Educational System: Under the Individuals with Disabilities Education Act (IDEA), eligible children from birth to 21 have a legal right to necessary PT services, often provided through early intervention or in schools at no direct cost to the family.
While New York allows direct access to physical therapy, your insurance plan might still require a physician's referral for reimbursement. We can help you steer these requirements to make care as accessible as possible.
Conclusion
At Evolve Physical Therapy + Sports Rehabilitation, we believe every child deserves to move freely and participate fully in life. Pediatric pt is about more than treating physical issues—it's about opening doors to independence, confidence, and new possibilities.
As we've discussed, skilled therapists use play-based care to help children overcome developmental delays, recover from injuries, and manage chronic conditions. The benefits are profound, building self-esteem, creating learning opportunities, and easing daily challenges for families.
Early intervention makes all the difference. If you've noticed potential red flags in your child's development, trust your instincts. Reaching out for an evaluation is a powerful first step toward helping your child thrive.
Our team at Evolve Physical Therapy + Sports Rehabilitation is dedicated to serving children across Brooklyn, with locations in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin. We are committed to helping your child reach their maximum potential, one milestone at a time.
Take the next step for your child's development with our pediatric physical therapy in Brooklyn
Injury Recovery Unlocked: Your Guide to Physical Therapy
Why Physical Therapy for Injuries Is Essential for Full Recovery

Physical therapy for injuries helps you recover faster, reduce pain, and prevent future problems through a structured, evidence-based approach. Here's what you need to know:
Key Benefits of Physical Therapy:
- Faster Recovery - Patients regain strength up to 40% faster than those who skip rehabilitation
- Pain Relief - Non-invasive, drug-free treatment that reduces inflammation and discomfort
- Injury Prevention - Reduces re-injury risk by 50% through strengthening and movement education
- Improved Function - Restores mobility, flexibility, and joint function within 12 weeks of structured treatment
- Personalized Care - Customized treatment plans based on your specific injury and goals
Physical therapy is a holistic healthcare approach that uses therapeutic exercises, manual therapy, and specialized techniques to help you recover from injuries that affect your bones, joints, muscles, ligaments, and tendons. Whether you're dealing with a sprained ankle, torn ACL, rotator cuff injury, or chronic back pain, physical therapy focuses on three core goals: alleviating pain, restoring physical function, and preventing further injury.
Too often, people think they can just rest and handle rehabilitation on their own. The reality? Without proper physical therapy, you risk lingering pain, weakness, and even permanent mobility issues. As one expert puts it, those who commit to proper rehabilitation almost always recover faster and stronger.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, and I've spent nearly two decades specializing in physical therapy for injuries, from complex chronic pain cases to post-surgical rehabilitation and sports injuries. My approach focuses on hands-on treatment and addressing the root cause of dysfunction, not just masking symptoms.
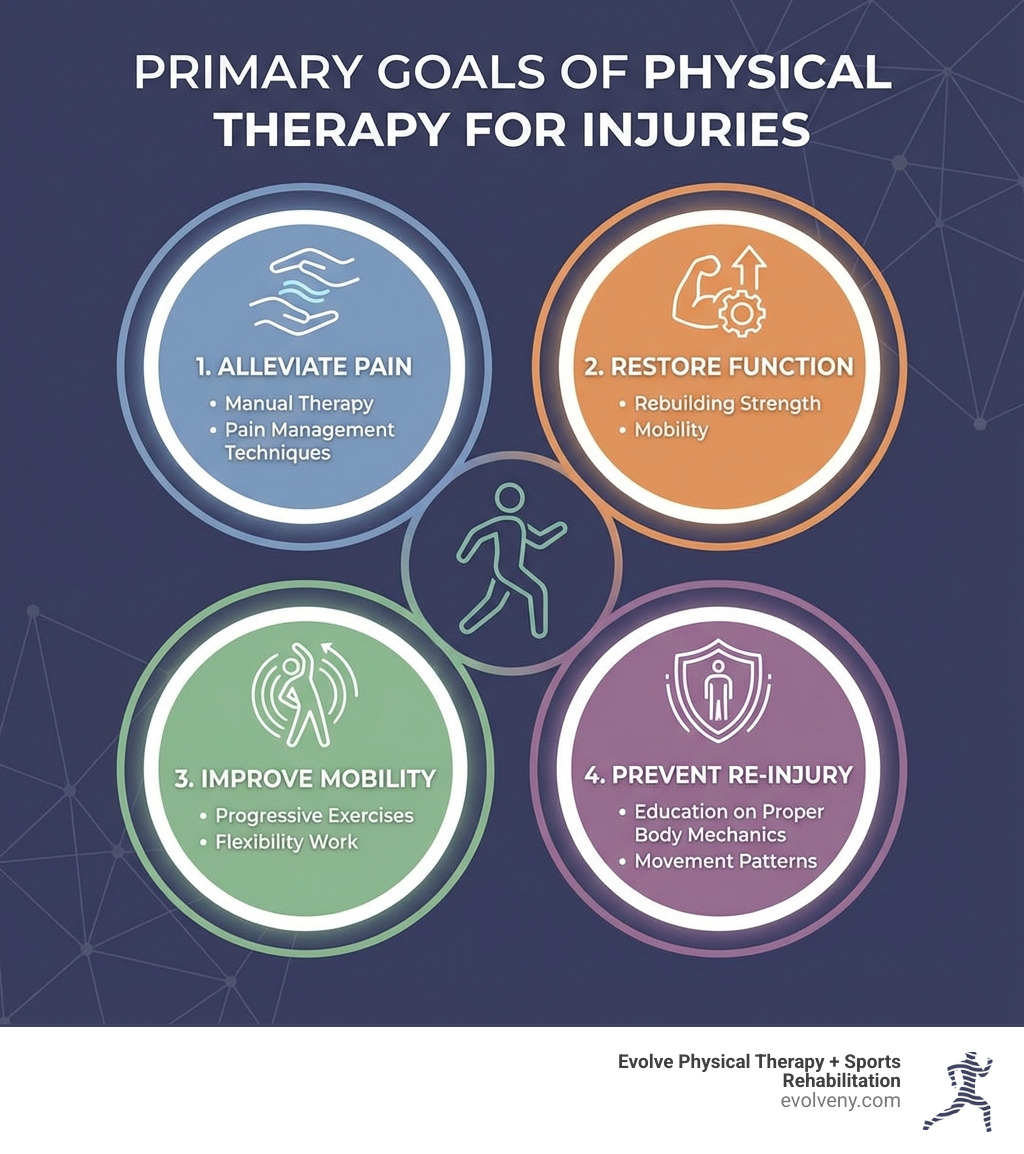
Understanding Orthopedic Physical Therapy and Its Role in Healing
Orthopedic injuries are those that affect your musculoskeletal system—your bones, joints, muscles, ligaments, and tendons. These can range from a sudden sprain on the basketball court to persistent pain from a chronic condition. When these injuries strike, they can significantly impact your mobility and quality of life, making everyday tasks feel like monumental challenges. That's where orthopedic physical therapy steps in.
Physical therapy for injuries is a non-invasive and drug-free approach designed to help you recover, regain function, and prevent future issues. It's not just about addressing the pain; it's about understanding the mechanics of your body and creating a personalized treatment plan that targets the root cause of your discomfort. We develop these plans to restore your physical function, reduce pain, and ultimately improve your mobility, allowing you to return to the activities you love.
How Physical Therapy Helps with Orthopedic Injuries
When you suffer an orthopedic injury, your body's natural response can include pain, swelling, and reduced function. Our physical therapists are highly trained professionals who work to counteract these effects and promote healing through a variety of techniques.
First, we focus on pain management and inflammation reduction. Through gentle techniques and modalities, we help alleviate discomfort and calm irritated tissues. As one study highlights, physical therapy can improve joint function significantly within 12 weeks of structured treatment, directly addressing the pain and stiffness that often accompany injuries.
Next, we work to improve circulation. Increased blood flow to the injured area is vital for healing, as it delivers essential nutrients and removes waste products. This stimulation of natural healing processes can lead to faster recovery times.
Then comes the crucial work of muscle strengthening and increased flexibility. Injuries can lead to muscle weakness and stiffness as your body tries to protect the injured area. Our custom exercise programs gradually rebuild strength in weakened muscles and improve the flexibility of tight tissues. This not only aids recovery but also improves physical performance and reduces the risk of future injuries. We help you restore your full range of motion, ensuring that your joints can move freely and without restriction, which is fundamental for everyday tasks and athletic endeavors.
Who Are the Ideal Candidates for Physical Therapy?
If you're experiencing pain, limited mobility, or recovering from an orthopedic injury or surgery, you're likely an ideal candidate for physical therapy for injuries. We see a wide range of individuals at Evolve Physical Therapy in Brooklyn, including:
- Post-surgery patients: Whether you've undergone a joint replacement, ligament repair, or spinal surgery, physical therapy is a critical component of your rehabilitation. We guide you through the healing process, prevent complications, and help you regain optimal function.
- Athletes with sports injuries: From sprains and strains to more severe issues like ACL tears and rotator cuff injuries, athletes often require specialized rehabilitation. We help restore performance, prevent future injuries, and optimize movement for peak athletic performance. This specialized rehab for athletes is called sports physical therapy, an area where we excel.
- Individuals with chronic pain: Conditions like arthritis, fibromyalgia, or persistent back pain can significantly impact your life. We use therapeutic exercises and manual techniques to alleviate pain and improve your ability to manage daily activities.
- People with joint issues: Whether it's a frozen shoulder, knee instability, or hip discomfort, physical therapy can improve joint function, reduce pain, and increase your mobility.
- Patients with sprains and strains: These common injuries, often dismissed as minor, can lead to chronic issues if not properly treated. We ensure proper healing and provide strategies to prevent re-injury.
Essentially, if you're looking to recover from an injury, reduce pain, improve your physical function, or prevent future problems, we're here to help you get back on your feet and back to living your life to the fullest.
The Road to Recovery: A Step-by-Step Guide to the Stages of Physical Therapy
Recovering from an injury isn't a straight line; it's a journey with distinct stages, each building upon the last. At Evolve Physical Therapy, we guide you through a structured rehabilitation process, ensuring progressive healing and lasting results. This phased approach, from initial assessment to full recovery, is designed to meet your body where it is and safely advance you toward your goals. We also empower you with patient education and home exercise programs so you can take an active role in your recovery.

Stage 1: The Acute Phase (Protection and Pain Relief)
This is the immediate aftermath of an injury, characterized by pain, swelling, and often limited movement. Our primary goals in this phase are to protect the injured area, manage pain, and control inflammation.
- Initial Assessment: Your journey begins with a thorough evaluation. We'll assess the extent of your injury, your range of motion, strength, and identify any contributing factors. This helps us create your personalized treatment plan.
- Pain and Inflammation Control: We often use the R.I.C.E. method (Rest, Ice, Compression, Elevation) to reduce swelling and discomfort. Gentle manual therapy techniques and modalities like cold therapy can also be employed to soothe the area.
- Gentle Movement and Preventing Stiffness: While rest is important, complete immobilization can cause stiffness and muscle atrophy. We introduce gentle, pain-free movements to maintain joint mobility and prevent complications, protecting the injured area while encouraging initial healing.
Stage 2: The Intermediate Phase (Restoring Mobility and Strength)
Once acute pain and swelling have subsided, we transition into rebuilding your body's capabilities. This phase focuses on safely increasing your activity levels.
- Gradual Exercise Progression: We introduce therapeutic exercises that progressively challenge your muscles and joints. These exercises are carefully selected to improve strength, flexibility, and endurance without re-aggravating your injury.
- Restoring Range of Motion: We work on regaining the full, pain-free movement of your affected joints through targeted stretches and mobilization techniques.
- Light Strengthening Exercises: These exercises focus on activating and strengthening the muscles surrounding the injured area, providing crucial support and stability.
- Balance and Stability Training: Crucial for lower body injuries, balance exercises retrain proprioception (your body's spatial awareness) and improve stability, reducing the risk of falls or re-injury.
- Improving Coordination: As your strength and balance improve, we incorporate exercises that improve coordination, crucial for fluid, natural movement.
Stage 3: The Advanced Phase (Return to Full Function)
This is where we fine-tune your recovery, preparing you to return to your desired activities, whether that's daily life, work, or competitive sports.
- Advanced Strengthening: We progress to more challenging resistance exercises, building significant strength, power, and muscular endurance. This phase ensures your body is robust enough to handle the demands of your activities.
- Sport-Specific Drills: For athletes, this involves incorporating movements and drills that mimic the demands of their sport. This might include jumping, cutting, pivoting, and agility training.
- Functional Capacity Testing: We perform assessments to objectively measure your readiness to return to full activity. This helps ensure you're not only strong but also capable of performing complex movements safely and efficiently.
- Endurance Training: Building cardiovascular and muscular endurance is key to preventing fatigue-related injuries and sustaining performance over time.
- Injury Prevention Strategies: We educate you on proper body mechanics, warm-up routines, and stretching techniques to minimize the risk of future injuries. This includes identifying and correcting any movement patterns that might have contributed to your initial injury.
- Mental Readiness: A significant injury can be mentally challenging. We help you build confidence and overcome apprehension about returning to your activities.
Throughout these stages, your progress is continuously monitored, and your treatment plan is adjusted to ensure you're always moving forward safely and effectively.
Common Conditions and Key Techniques in Physical Therapy for Injuries
At Evolve Physical Therapy, we encounter a wide array of orthopedic injuries in our Brooklyn clinics. Our approach is always patient-centered, meaning we tailor our techniques to your specific needs and the nature of your injury.
Common Conditions That Require Physical Therapy for Injuries
Many common orthopedic issues benefit significantly from physical therapy for injuries. Here’s a list of conditions we frequently treat:
- Sprains and strains: These are among the most common injuries, affecting ligaments (sprains) or muscles/tendons (strains). Without proper care, they can lead to chronic instability or weakness. For instance, a sprained ankle often involves a sudden twist that tears ligaments. Early intervention with physical therapy, including the RICE method (Rest, Ice, Compression, Elevation), gentle movements, and progressive strengthening, is crucial. You can find more information about the diagnosis and treatment for a sprained ankle.
- ACL tears: An anterior cruciate ligament (ACL) tear in the knee is a common and serious sports injury. It often results from the knee extending beyond its normal range of motion or twisting sharply. Physical therapy is vital for both non-surgical management and post-surgical rehabilitation, focusing on pain control, swelling management, gait training, range of motion, strengthening, balance, and quadriceps contraction. ACL injuries rarely heal naturally without treatment and can have negative long-term effects. We can help you with rehabilitation for an ACL injury.
- Rotator cuff tendinopathy: This condition affects the tendons around your shoulder joint, causing pain and limiting arm movement. Our approach involves assessment, prognosis, and nonsurgical management to restore shoulder function. There are clinical practice guidelines that provide evidence-based recommendations for this condition.
- Fractures: After a bone fracture, physical therapy is essential to restore strength, range of motion, and function once the bone has healed. We help reduce stiffness, rebuild muscle, and guide you safely back to activity.
- Chronic back pain: Low back pain is a pervasive issue. Physical therapists are experts in using exercise training interventions, including specific trunk muscle activation, strengthening, and endurance exercises, to reduce pain and disability, even for those with leg pain.
- Knee injuries: Beyond ACL tears, we address various knee issues, including meniscus tears, patellar tendinitis, and general knee instability. We focus on strengthening the surrounding muscles and improving joint mechanics.
- Concussions/Mild Traumatic Brain Injury: While not strictly orthopedic, physical therapy plays a crucial role in managing post-concussion symptoms, such as balance issues, dizziness, and headaches. There are specific clinical practice guidelines for physical therapist management of concussive events.
Key Techniques Used in Rehabilitation
Our physical therapists employ a diverse toolkit of approaches and techniques to facilitate your recovery:
- Manual therapy: This hands-on approach involves skilled techniques such as massage, mobilization, and manipulation to reduce pain, improve joint movement, and decrease muscle tension. We use our hands to assess and treat soft tissues and joints, restoring natural movement patterns.
- Therapeutic exercise: This is the cornerstone of physical therapy. We prescribe specific exercises custom to your injury and goals, focusing on strengthening weakened muscles, improving flexibility, enhancing endurance, and restoring coordination. These exercises are progressed gradually to ensure safety and effectiveness.
- Neuromuscular re-education: This technique helps re-establish the communication between your brain and muscles, which can be disrupted after an injury. It involves exercises that improve balance, coordination, and proprioception, essential for stable and efficient movement.
- Gait training: If your injury affects your ability to walk, we provide specialized training to help you regain a normal and efficient walking pattern. This might involve using assistive devices initially and progressing to independent walking on various terrains.
- Modalities: We may use various physical agents, such as heat, cold, and electrical stimulation, to complement your treatment. Heat therapy can relax muscles and increase blood flow, cold therapy can reduce inflammation and pain, and electrical stimulation can help reduce pain and promote muscle activation.
The Critical Role of Early Intervention
We cannot stress enough why early intervention is crucial in orthopedic injury rehabilitation. When an injury occurs, delaying treatment can lead to a cascade of negative consequences that make recovery longer and more challenging.
- Preventing Chronic Pain: Without timely intervention, acute pain can become chronic, leading to long-term discomfort and reduced quality of life. Early physical therapy helps address the pain mechanisms before they become deeply ingrained.
- Avoiding Muscle Weakness and Atrophy: Immobilization or disuse after an injury quickly leads to muscle weakness. Early, gentle exercises help maintain muscle mass and function, making it easier to rebuild strength later.
- Reducing Complications: Early physical therapy can prevent complications such as excessive scar tissue formation, joint stiffness, and compensatory movement patterns that can strain other parts of your body.
- Promoting Faster Healing: By improving circulation and guiding the healing tissues through appropriate stress, early intervention can stimulate natural healing processes, leading to a quicker and more complete recovery.
- Minimizing Scar Tissue: Controlled movement and specific techniques applied early can help organize collagen fibers during the healing process, leading to less restrictive and more functional scar tissue.
- Ensuring Optimal Recovery: Overall, starting physical therapy soon after an injury optimizes your body's healing potential, leading to a more complete restoration of function and a reduced risk of re-injury. Patients who engage in post-injury rehabilitation regain strength up to 40% faster than those who don’t. This statistic alone underscores the immense value of timely care.
The Proven Benefits and Overall Impact of Physical Therapy
The decision to commit to physical therapy for injuries is an investment in your long-term health and well-being. The benefits extend far beyond immediate pain relief, impacting your physical capabilities, mental resilience, and overall quality of life.
Measurable Improvements and Long-Term Gains
The impact of physical therapy on orthopedic injury recovery is profound, backed by clear evidence and tangible results:
- Faster Recovery: As we've mentioned, patients who engage in post-injury rehabilitation regain strength up to 40% faster than those who don’t. This means less downtime and a quicker return to your daily routines and favorite activities.
- Reduced Re-Injury Risk: One of the most significant long-term benefits is the prevention of future injuries. Physical therapy can reduce the risk of re-injury by 50%. We achieve this by strengthening supporting muscles, improving balance and coordination, and educating you on proper body mechanics.
- Improved Joint Function: Many orthopedic injuries affect joint mobility. Through structured treatment, physical therapy can improve joint function significantly within just 12 weeks. This translates to smoother, pain-free movement and greater flexibility.
- Improved Quality of Life: By alleviating pain, restoring function, and increasing your independence, physical therapy directly improves your overall quality of life. Imagine being able to walk, run, lift, or play with your kids without discomfort – that's the goal.
- Long-Term Pain Management: For those with chronic conditions, physical therapy provides tools and strategies for sustained pain management, often reducing reliance on medication and avoiding more invasive treatments like surgery.
The Holistic Approach of Physical Therapy for Injuries
At Evolve Physical Therapy, we believe in a holistic approach to care. This means looking beyond the injured area and considering your entire body and lifestyle.
- Body Mechanics Education: We teach you how your body moves and how to perform daily activities, work tasks, or sports movements in a way that minimizes stress on your joints and muscles. Understanding proper posture and movement patterns is key to preventing future problems.
- Injury Prevention Strategies: Beyond just recovering from your current injury, we equip you with the knowledge and exercises to prevent similar issues from occurring. This includes custom warm-up routines, stretching protocols, and strengthening exercises specific to your activities.
- Empowering Patients: We view you as an active partner in your recovery. By educating you about your condition and providing you with home exercise programs, we empower you to take control of your health and maintain your gains long after your therapy sessions conclude.
- Improving Overall Wellness: Physical activity is a cornerstone of good health. By helping you regain comfortable movement, we encourage an active lifestyle that contributes to your overall physical and mental wellness.
- Creating Sustainable Health Habits: Our goal is to help you build habits that support long-term health, strength, and resilience, reducing the likelihood of future injuries and promoting a vibrant, active life.
Building Your Recovery Team: Orthopedist vs. Physical Therapist
When you're dealing with an orthopedic injury, it's natural to wonder who to see first: an orthopedist or a physical therapist? Both play crucial, often complementary, roles in your recovery journey. Understanding their distinct functions can help you make an informed decision.
| Feature | Orthopedist | Physical Therapist |
|---|---|---|
| Primary Role | Diagnose and treat musculoskeletal conditions (medical/surgical) | Rehabilitate and restore physical function and movement |
| Focus | Medical diagnosis, surgical intervention, medication management | Non-surgical treatment, exercise, manual therapy, education |
| When to Consult | Severe injuries, suspected fractures, persistent pain, surgical needs | Rehabilitation, regaining strength/mobility, chronic pain management, improving movement |
| Intervention | X-rays, MRI, surgery, injections, prescriptions | Therapeutic exercises, manual therapy, modalities, home programs |
| Training | Medical doctor (MD) with specialized surgical residency | Doctor of Physical Therapy (DPT) or licensed physical therapist |
When to See an Orthopedist
An orthopedist is a medical doctor who specializes in the diagnosis and treatment of conditions affecting the musculoskeletal system. You should typically consult an orthopedist if you experience:
- Severe injuries: This includes traumatic injuries where you suspect a fracture, dislocation, or a significant tear (e.g., a complete ACL tear). An orthopedist can order imaging like X-rays, MRI, or CT scans to accurately diagnose the extent of the damage.
- Persistent pain: If you've had pain that doesn't improve with rest or initial self-care, an orthopedist can investigate underlying causes that might require medical intervention.
- Diagnostic imaging: If you need advanced diagnostic imaging to understand the nature of your injury, an orthopedist is the appropriate specialist to consult.
- Surgical consultation: If your injury is severe or hasn't responded to conservative treatments, an orthopedist can discuss surgical options and perform necessary procedures.
- Initial diagnosis: For complex or unclear orthopedic problems, an orthopedist can provide a definitive diagnosis and refer you to the most appropriate course of treatment, which often includes physical therapy.
When to See a Physical Therapist
A physical therapist is a movement expert who focuses on restoring function, reducing pain, and preventing disability. You can often see a physical therapist directly (known as direct access) or with a referral from an orthopedist or other doctor. You should consult a physical therapist for:
- Rehabilitation post-injury or surgery: This is our bread and butter! Whether you're recovering from a sprain, strain, fracture, or surgery, we design and oversee your rehabilitation program to safely guide you back to full function.
- Regaining strength and mobility: If you're experiencing weakness, stiffness, or reduced range of motion after an injury or due to a chronic condition, we'll help you rebuild strength and flexibility.
- Managing chronic pain: For conditions like chronic back pain, neck pain, or arthritis, physical therapy offers non-pharmacological strategies to alleviate discomfort and improve your ability to perform daily activities.
- Improving movement patterns: We identify and correct inefficient or harmful movement patterns that contribute to pain or injury risk, teaching you how to move more safely and effectively.
- Non-surgical treatment: For many orthopedic conditions, physical therapy is the first line of defense, often helping you avoid the need for surgery. We focus on conservative management to achieve optimal outcomes.
Often, an orthopedist and a physical therapist will work together as a team, especially for more complex injuries or post-surgical cases. The orthopedist provides the medical diagnosis and any surgical intervention, while the physical therapist manages the rehabilitative process. This collaborative care ensures you receive comprehensive and integrated treatment.
Conclusion: Take the First Step Towards Your Recovery
We hope this guide has illuminated the vital role that physical therapy for injuries plays in achieving a full, lasting recovery. From managing acute pain and inflammation to restoring strength and preventing future issues, physical therapy offers a structured, evidence-based path back to an active and pain-free life. Patients who engage in rehabilitation regain strength faster and significantly reduce their risk of re-injury.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we are dedicated to helping you open up your recovery potential. Our hands-on approach, personalized treatment plans, and commitment to patient education ensure that you receive the highest quality of care, custom to your unique needs and goals. We believe in empowering you to take control of your health, building not just strength, but also confidence and sustainable health habits.
Don't let an injury hold you back. Taking the first step towards rehabilitation is a proactive choice for your health and well-being. If you're in Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin, we invite you to experience the difference that expert, compassionate physical therapy can make.
Ready to reclaim your movement and get back to living your life to the fullest? Start your physical therapy journey in Brooklyn
Say Goodbye to Stiff Hips: Exercises for Better Internal Rotation
Why Limited Hip Internal Rotation Is Sabotaging Your Movement

Limited hip internal rotation is when your hip joint can't rotate inward properly—and it's likely contributing to your knee pain, back discomfort, or difficulty squatting.
Quick Answer: What You Need to Know
- Normal range: 30-45 degrees of hip internal rotation
- Minimum needed for daily function: 35 degrees for a full squat, 4-6 degrees for walking
- Common signs: Knee pain, low back pain, shortened stride, feet turning outward when you walk
- Main causes: Prolonged sitting, tight hip capsule, weak internal rotators, overactive external rotators
- Solutions: Targeted stretches to create space + strengthening exercises to control the new range
Hip internal rotation happens when your thigh bone (femur) rotates inward within the hip socket. It's not a movement you think about, but you need it constantly—every time you walk, climb stairs, or shift your weight. Without enough internal rotation, your body compensates by overworking your lower back, forcing your knees inward, or flattening your feet. These compensations pile up over time, leading to pain and injury in areas that seem unrelated to your hips.
As Aristotle once said (or at least, something like it): "The hips are the gateway to the soul." While that's a bit dramatic, the research backs up the importance. Studies show that athletes with less than 30 degrees of internal rotation are more than twice as likely to suffer lower extremity injuries. A 30-degree reduction in hip internal rotation increases your odds of an ACL tear by over 4 times in the same leg and over 5 times in the opposite leg.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, and I've spent nearly two decades helping patients resolve chronic pain and movement dysfunction. Throughout my career, I've seen how addressing limited hip internal rotation can eliminate knee pain, reduce back strain, and restore athletic performance that patients thought was gone for good.
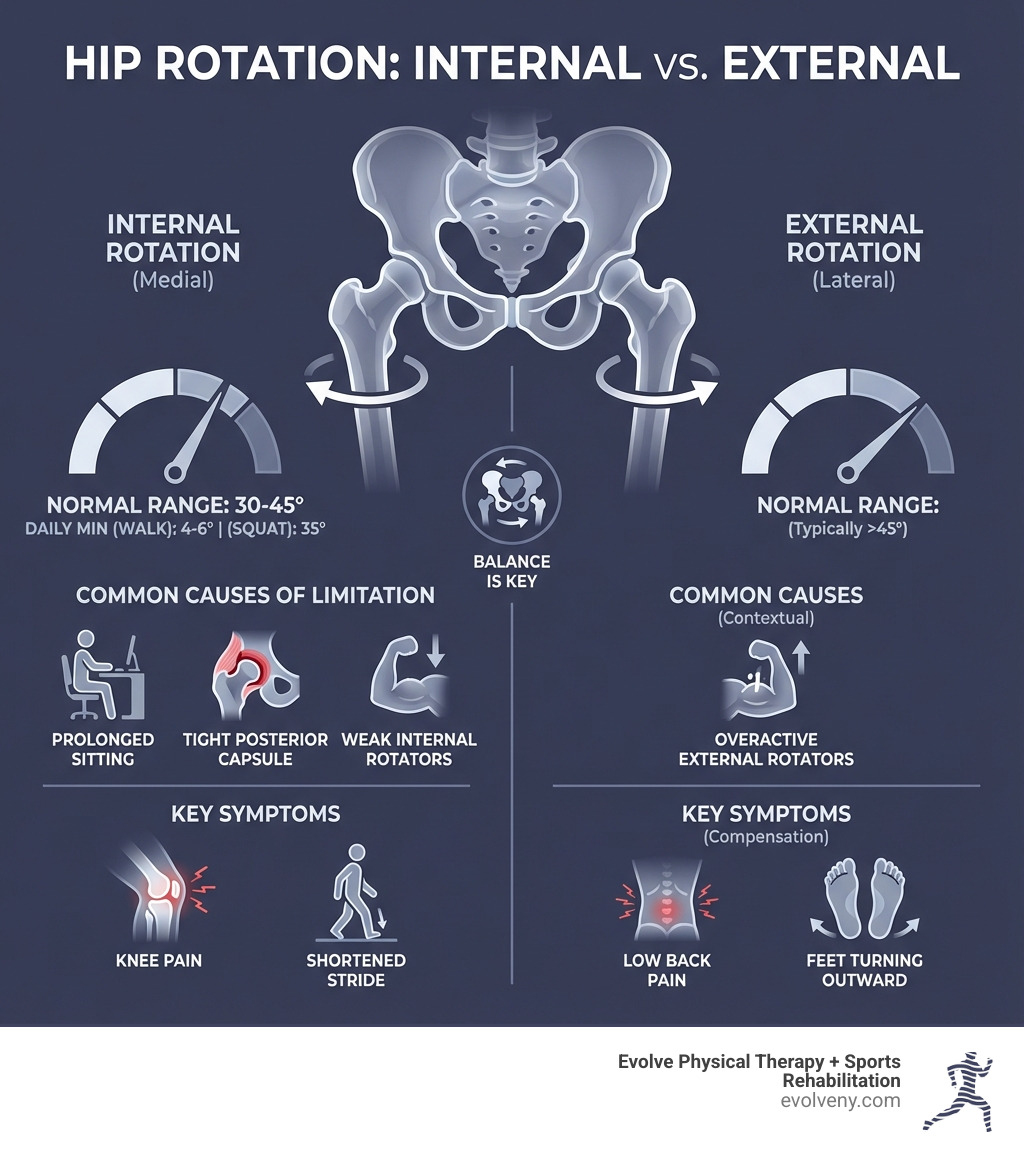
The Hidden Consequences of Poor Hip Mobility
When your hips can't move as they should, your body finds other ways to get the job done. This might sound clever, but it often leads to a cascade of problems throughout your body. Think of your body as a finely tuned machine; if one part isn't working efficiently, other parts have to pick up the slack, leading to overuse and eventual breakdown. This is precisely what happens with limited hip internal rotation.
Why Hip Rotation is Crucial for Your Pelvic Floor
The intricate symphony of the human body means seemingly unrelated areas often impact each other in surprising ways. The relationship between hip internal rotation and pelvic floor health is a testament to this interconnectedness.
- Pelvic Alignment: Our hips are directly connected to our pelvis. When hip internal rotation is restricted, it can pull the pelvis out of its optimal alignment. This misalignment can place undue stress and tension on the pelvic floor muscles, which are designed to function best within a balanced pelvic posture. Proper hip mobility allows the pelvis to maintain a neutral position, creating a stable base for the pelvic floor to operate efficiently.
- Functional Stability: Efficient hip internal rotation is vital for functional stability during movement. Whether we're walking, running, or changing direction, our hips need to rotate internally to allow for smooth transitions and proper weight distribution. Without this, our body compensates, often by gripping or overworking the pelvic floor muscles to create a sense of stability. This constant overactivity can lead to pelvic floor dysfunction.
- Reciprocal Inhibition: This is a fancy term for how our muscles work in pairs. When one muscle contracts, its opposing muscle relaxes. In the context of our hips and pelvic floor, proper hip internal rotation helps to coordinate muscle activity. If certain hip muscles are constantly tight or overactive due to limited hip internal rotation, they can prevent the pelvic floor muscles from relaxing and contracting effectively. This can lead to hypertonicity (excessive tension) in the pelvic floor, which is a common cause of pelvic pain and dysfunction.
- Posture Influence: When our hips lack the ability to internally rotate, we often adopt compensatory postures, such as standing with our feet turned out or excessively arching our lower back. These postural shifts can alter the mechanics of the entire trunk and pelvis, placing increased strain on the pelvic floor. A mobile hip that can achieve full internal rotation encourages a more upright and aligned posture, which, in turn, supports the natural function of the pelvic floor.
- Reducing Strain on Pelvic Floor Muscles: Maintaining optimal hip internal rotation reduces the overall strain on our pelvic floor muscles. By allowing the hips to move freely and efficiently, we prevent compensatory patterns that force the pelvic floor to work harder than it should. This can lead to a healthier, more resilient pelvic floor, capable of performing its crucial roles in continence, support, and sexual function.
Curious about how to improve your hip internal rotation mobility and control and its impact on your pelvic floor? Check out @lpimomsclub for more information.
The Link Between Stiff Hips and Serious Injuries
When our hips are stiff and lack internal rotation, our bodies are incredibly clever at finding workarounds. Unfortunately, these "workarounds" often lead to pain and injury in other areas.
- Low Back Pain: One of the most common complaints we hear is low back pain. When your hips can't internally rotate, your lower back often has to twist or compensate excessively during movements that would normally involve hip rotation. This increased demand on the lumbar spine can lead to muscle strain, disc issues, and chronic pain. The hip joint's limitation causes lumbopelvic compensatory motions, accumulating tissue stress on the lumbar spine.
- Knee Pain: Anterior and lateral knee pain, which many people attribute to a "tight IT band," can often be due to limited hip internal rotation. The IT band is a very thick and strong piece of fascia that has been shown to take ~2,000 lbs of force to deform. Therefore, the IT band being "tight" is highly unlikely. Instead, the pain often comes from overactive muscles (like the glute max/med and TFL) pulling on the IT band because your hip isn't rotating properly. This creates a painful cycle where your knee is taking the brunt of your hip's immobility.
- ACL Tears: The connection between limited hip internal rotation and ACL injuries is significant. Restriction in hip internal rotation is associated with an increased risk of ACL injury. A study found that a 30-degree reduction in left hip internal rotation was associated with 4.06 and 5.29 times greater odds of ACL injury in the ipsilateral and contralateral limbs, respectively. The in silico model simulation predicted an increase in peak AM-ACL strain as the range of hip internal rotation was decreased. This means that if your hip can't rotate internally enough, your knee is put under much greater stress during dynamic movements like pivoting or landing, making it more vulnerable to injury. You can read more about this in the research article, "Restriction in hip internal rotation is associated with an increased risk of ACL injury" on PubMed.
- Femoroacetabular Impingement (FAI): FAI, or hip impingement, is a condition where extra bone grows along one or both of the bones that form the hip joint, giving the bones an irregular shape. This can cause them to rub against each other during hip movements, leading to pain and limiting range of motion, particularly internal rotation. Less hip range of motion is associated with a greater alpha angle in people with longstanding hip and groin pain, where the alpha angle is a marker for cam morphology (a type of FAI).
- Chronic Groin Pain and Osteoarthritis Precursor: Dysfunctional hip internal rotation is a biomechanical fault that can lead to a host of injuries from the lower back to the lower limb. A decrease in hip internal rotation can be a precursor to lower back pain, labral tears, femoroacetabular impingement, and even osteoarthritis of the hip.
Ignoring limited hip internal rotation is like driving a car with misaligned wheels – you might keep going, but you're doing some serious damage along the way.
What Causes Limited Hip Internal Rotation and How to Check Yours
Why do some of us struggle with hip internal rotation while others seem to move effortlessly? The causes are often multi-faceted, ranging from our daily habits to our unique anatomy. Understanding these causes is the first step toward finding effective solutions.
Common Causes of Limited Hip Internal Rotation
- Prolonged Sitting: In our modern world, many of us spend the majority of our waking hours seated. This prolonged static position can lead to shortened and overactive hip flexors, while simultaneously deactivating our glutes. This imbalance restricts the natural movement of the hip, making internal rotation particularly challenging. It’s like your body forgets how to access that range of motion.
- Posterior Hip Capsule Tightness: One of the biggest roadblocks people hit when trying to improve hip internal rotation is the lack of space for the femoral head to rotate within the hip socket. For us to internally rotate our hip, the femoral head needs to push back (posteriorly) within the acetabulum. If the posterior hip capsule (the connective tissue surrounding the joint) is tight or restricted, it can physically block this movement. This is especially true if the femur has been in an externally rotated position for a long time, causing a "capsular restriction" to build up.
- Tight External Rotator Muscles: Our hip's external rotators (muscles that turn the leg outward) can become tight and overactive. Muscles like the piriformis and the deeper gluteal muscles, while crucial for hip stability, can inadvertently limit internal rotation if they're constantly "on" or in a shortened state. This is a common issue with conditions like Piriformis Syndrome, where the piriformis muscle can compress the sciatic nerve, leading to pain and further limiting hip mobility.
- Weak Internal Rotator Muscles: Conversely, the muscles responsible for internal rotation—primarily the TFL (tensor fasciae latae) and some adductor muscles—might be weak or underused. If these muscles aren't strong enough to actively pull the hip into internal rotation, the range of motion will remain restricted, even if the external rotators are released.
- Structural Issues like FAI: Sometimes, the limitation isn't just about soft tissue. Conditions like Femoroacetabular Impingement (FAI), where the bones of the hip joint have an irregular shape, can physically block the normal movement of the hip, making internal rotation difficult or painful.
How to Assess Your Hip Internal Rotation at Home
We can do a simple self-assessment to get a general idea of your hip internal rotation. This isn't a diagnostic tool, but it can highlight potential areas of concern.
- The Seated Hip Internal Rotation Test:
- Sit on the edge of a chair or a sturdy surface, with your knees bent and feet flat on the floor, hip-width apart.
- Place your hands on the chair behind you for support, ensuring your spine is tall and neutral.
- Keeping your thigh stable and your knee pointing forward, slowly lift one foot off the floor and rotate it laterally (outward) as far as you comfortably can without lifting your hip or shifting your body weight.
- Observe how far your foot moves outward. The movement of your shin/foot away from the midline indicates hip internal rotation.
- Repeat on the other side.

**What to Look For:**
* **Normal Range:** Ideally, your foot should rotate out to at least a 30-degree angle, with some individuals achieving 45 degrees or more.
* **Asymmetry:** Do you notice a big difference between your left and right sides? It's common to have a relatively more limited ability to access internal rotation on the left side for many people.
* **Signs of Limitation:** If your foot barely moves, or if you feel a sharp pinch or pain, you likely have **limited hip internal rotation**.
If you're unsure about your assessment or concerned about your hip mobility, we encourage you to book a free movement consultation with our expert physical therapists at Evolve Physical Therapy in Brooklyn.
A Step-by-Step Guide to Improving Hip Mobility
Improving limited hip internal rotation requires a strategic, two-pronged approach: first, we need to release any tightness or restrictions that are physically blocking the movement, and then, we need to strengthen the muscles that control this newly gained range of motion. Consistency is key here; a little bit every day goes a long way.
Stretches to Release Tightness and Create Space
These stretches are designed to address the common culprits of limited hip internal rotation, such as a tight posterior hip capsule and overactive external rotators.
- 90/90 Stretch (Seated Hip Rotation):
- Sit on the floor with one leg internally rotated in front of you (shin parallel to your body) and the other leg externally rotated to your side (shin perpendicular to your body), both knees bent at 90 degrees.
- Maintain a tall, upright posture.
- From this position, gently lean forward over your front leg, feeling the stretch in your hip.
- To target internal rotation, you can also gently rotate your torso towards the internally rotated hip, deepening the stretch.
- Hold for 30-60 seconds, breathing deeply. Repeat 2-3 times per side.

Supine Windshield Wipers:
- Lie on your back with your knees bent, feet flat on the floor, wider than hip-width apart.
- Keep your feet planted and slowly let both knees fall inward towards each other, like windshield wipers.
- Hold the inward rotation for 30 seconds, feeling the stretch in your outer hips and glutes.
- Return to the center and repeat for 2-3 rounds. This is a gentle way to encourage internal rotation.
Posterior Hip Capsule Stretch (Knee to Opposite Shoulder):
- Lie on your back. Bring one knee towards your chest.
- Grasp the knee with both hands and gently pull it across your body towards your opposite armpit.
- You should feel a deep stretch in the buttock and outer hip of the leg you are stretching. This targets the posterior hip capsule and external rotators.
- Hold for 30-60 seconds, taking deep breaths. Repeat 2-3 times per side.
Best Practices for Stretching:
- Hold for 30-60 seconds: This duration is generally effective for increasing tissue extensibility.
- Breathe Deeply: Use your breath to help your body relax into the stretch. Exhale as you deepen the stretch.
- Avoid Sharp Pain: You should feel a stretch or tension, but never sharp, pinching, or burning pain. If you do, ease off or stop.
- Warm-up First: Perform these stretches after a light warm-up or at the end of your day.
Exercises to Strengthen and Control Your New Mobility
Once we've created a bit more space and released some tension, it's crucial to teach our bodies how to actively use and control that new range of motion. These exercises focus on strengthening the internal rotators and improving overall hip stability.
Reverse Clamshells:
- Lie on your side with your knees bent at a 90-degree angle, one leg stacked directly on top of the other. Keep your feet aligned with your hips.
- Keeping your knees together, slowly lift your top foot away from your bottom foot, rotating your top hip internally. Imagine your top thigh bone rotating inward in the socket.
- Control the movement as you lower your foot back down.
- Perform 3 sets of 15 repetitions on each side. A resistance band around your ankles can add challenge.
Prone Frog Internal Rotations:
- Lie on your belly in a "frog" position: knees wide, bent at 90 degrees, and the soles of your feet together.
- Keeping your knees on the ground, slowly lift one foot off the ground by rotating your hip internally.
- Hold for 1-2 seconds at the top, then slowly lower.
- Perform 3 sets of 15 repetitions on each side, focusing on slow, controlled movement.
Wall Bridge with Yoga Block Squeeze:
- Lie on your back with your knees bent and feet flat against a wall, hip-width apart. Place a yoga block or small ball between your knees.
- Squeeze the block gently with your knees.
- Engage your glutes and lift your hips into a bridge position.
- As you hold the bridge, gently shift the hip that feels tighter slightly to the side, pressing that foot into the wall a bit more. This encourages subtle internal rotation.
- Hold for 10 seconds, then lower. Repeat 10-15 times.
Cross-Body Kickstand RDL (Romanian Deadlift):
- Stand in a "kickstand" position with one foot slightly behind the other, heel lifted, for balance. The front leg will be doing most of the work.
- Hold a light dumbbell in the hand opposite your working leg.
- Hinge at your hips, pushing your butt back as you lower the dumbbell towards the instep of your working foot, crossing your body slightly.
- As you hinge, focus on allowing a subtle internal rotation in the working hip.
- Return to the starting position, squeezing your glute.
- Perform 3 sets of 10-12 controlled repetitions on each side.
Consistency is paramount. We recommend performing these exercises once a day, or at least 3-5 times a week, working both sides evenly to prevent imbalances. You should feel tension and muscle activation, but never sharp pain.
Frequently Asked Questions about Hip Mobility
We often get asked specific questions about limited hip internal rotation and how it impacts daily life and athletic performance. Here are some of the most common ones:
How does limited hip internal rotation affect my squat?
Ah, the squat – the king of exercises! To sit into a full, deep squat, you need a surprisingly specific amount of hip internal rotation, typically around 35 degrees. If you lack this crucial mobility, your body will try to find a way down, often by compensating in ways that can lead to problems.
Without enough hip internal rotation, you might notice:
- "Butt Wink": This is when your lower back rounds at the bottom of the squat. It's your lumbar spine compensating for a lack of hip mobility, putting excessive stress on your spinal discs.
- Knees Caving In (Knee Valgus): Your knees might collapse inward as you descend. This places unhealthy strain on your knee ligaments and can lead to conditions like patellofemoral pain.
- Foot Pronation: Your feet might flatten or roll inward excessively, trying to gain mobility from your ankles when your hips aren't providing it.
These compensations not only make your squat less efficient but also significantly increase your risk of injury over time. Improving your hip internal rotation is key to a safer, stronger, and deeper squat.
Are there specific people who should focus on hip internal rotation?
Absolutely! While good hip internal rotation benefits everyone, certain populations have an even greater need or are more susceptible to limitations:
- Athletes in Rotational Sports: Think golfers, tennis players, baseball pitchers, soccer players, and anyone involved in sports requiring powerful twisting motions. These athletes rely heavily on hip internal rotation for generating force and protecting their spine. A body lacking internal hip rotation is like a car with no back wheels – it might keep going, but it’s gonna do some damage along the way.
- Postpartum Individuals: Pregnancy and childbirth place immense strain on the pelvic floor and surrounding structures. Re-establishing optimal hip mobility, including internal rotation, is crucial for supporting pelvic floor health and returning to pain-free movement. The hip-pelvic floor connection is incredibly important during this phase.
- Office Workers and Anyone with Prolonged Sitting: Our sedentary lifestyles are a major culprit. Spending hours seated can shorten hip flexors and create muscular imbalances that directly contribute to limited hip internal rotation. Breaking up sitting time and incorporating hip mobility exercises is vital.
- Individuals Experiencing Hip, Knee, or Low Back Pain: As we've discussed, limited hip internal rotation is often a hidden factor in pain syndromes throughout the lower body and back. Addressing it can be a game-changer for long-term relief and prevention.
How long does it take to see improvement?
We understand you're eager for results, and the good news is that you might feel some immediate, temporary improvements in your range of motion right after a stretching session. That feeling of "more space" is a great motivator!
However, achieving lasting change in limited hip internal rotation requires consistent effort. We're not just stretching muscles; we're also influencing joint capsules and retraining movement patterns that might have been ingrained for years. You can expect to see meaningful, sustained improvements over several weeks to months.
Think of it like building a house – you don't just lay the foundation and expect it to be ready. You need to build the walls, put on the roof, and furnish it. Similarly, we stretch to create the potential for movement, and then we use strengthening exercises to teach your body to "own" and control that new range. Stick with it, and your hips will thank you!
Take the Next Step Towards Pain-Free Movement
We've explored the critical role of hip internal rotation, its far-reaching impact on our bodies, and the steps we can take to improve it. From alleviating nagging low back and knee pain to enhancing athletic performance and supporting pelvic floor health, optimizing your hip mobility is a cornerstone of overall well-being.
Ignoring limited hip internal rotation can lead to a cascade of compensatory movements and potentially more significant injuries down the line. But the good news is that with targeted stretches and strengthening exercises, you have the power to reclaim your hip health.
If you've been struggling with persistent pain, significant limitations, or just want a clearer path to achieving optimal hip mobility, a professional evaluation can identify the root cause and provide a personalized roadmap. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we offer holistic physical therapy services, focusing on evaluation, healing, and strengthening. Our unique hands-on approach and specialized programs, even those featured on NBC News, are designed to get you moving better and feeling stronger.
Don't let stiff hips hold you back any longer. We're here to help you move freely and live fully.
Get a personalized assessment from our Brooklyn physical therapists
Don't Be Awkward: A Guide to Recognizing Poor Posture
Why Your Body Position Matters More Than You Think

Awkward body posture refers to positions where your body deviates from its neutral alignment while performing work or daily activities. Instead of your joints resting in their natural, comfortable mid-range, awkward postures force your body into bent, twisted, or extended positions that require extra effort and strain.
Key Characteristics of Awkward Body Posture:
- Bent neck – Looking down at screens or documents for extended periods
- Rounded shoulders – Hunching forward while sitting or standing
- Twisted torso – Reaching behind or to the side without turning your body
- Extended arms – Working with hands above shoulder height
- Bent wrists – Typing or using tools with your wrists flexed or extended
- Forward head position – Also known as "tech neck"
Why It Matters:
When you hold awkward postures, your muscles work less efficiently and require more force to complete tasks. This leads to faster fatigue, increased strain on joints and tendons, and compressed nerves and blood vessels. The statistics are striking: more than half of all workers deal with neck problems, 30% suffer from shoulder tension, and 26% experience wrist and arm pain.
The further your body deviates from neutral alignment, the more your muscles must work to maintain that position. Static awkward postures – where you hold the same position for long periods – are particularly problematic because they restrict blood flow and prevent muscles from recovering.
What is Neutral Posture?
Neutral posture is your body's natural resting position where joints are at their mid-range of motion. In this position, your ears align over your shoulders, shoulders over hips, with minimal muscle tension required to maintain balance. It's the position where your body can produce maximum force with minimum effort.
I'm Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, and over nearly two decades I've helped thousands of patients address pain and dysfunction caused by awkward body posture. My work began in Tel Aviv treating complex injuries, and today I specialize in helping active professionals and athletes restore proper movement patterns and eliminate chronic pain at its source.
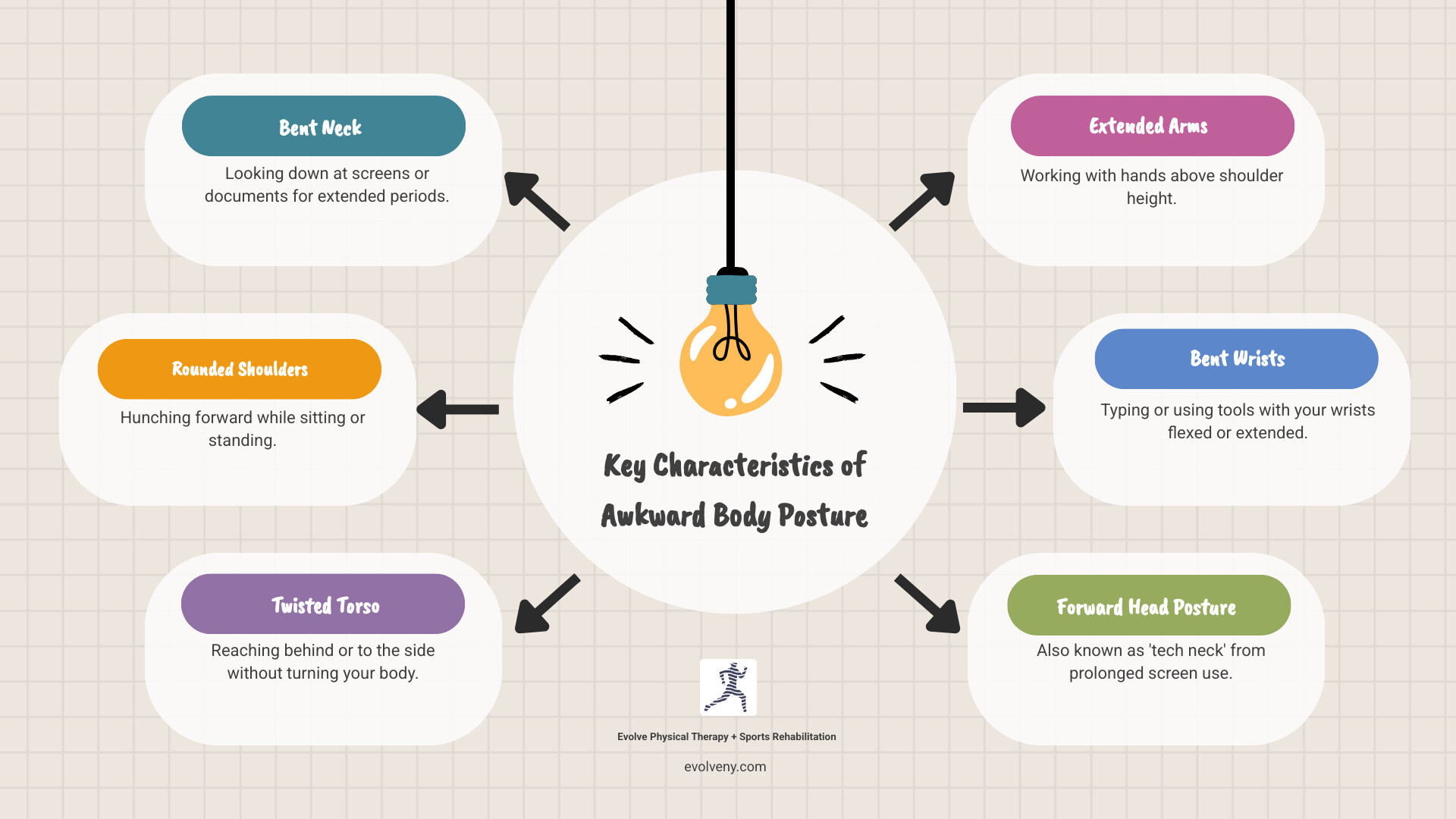
What is the Difference Between Awkward and Neutral Posture?
At Evolve Physical Therapy + Sports Rehabilitation, we often start by helping our patients understand the fundamental difference between neutral and awkward body posture. Think of neutral posture as your body's happy place – a state of balance and ease. It's when your body parts are positioned at their natural, mid-range of motion with minimal strain. In this alignment, your muscles are at their resting length, joints are aligned, and no conscious effort is needed to hold the position. This allows your muscles to work with maximum efficiency, making tasks feel lighter and less taxing. For a deeper dive into proper spinal alignment, consider exploring resources on proper alignment of the spine.
Conversely, awkward body posture is any deviation from this ideal neutral alignment. When your body is bent, twisted, or extended away from its natural curves, your muscles have to work harder to maintain that position. This increased effort leads to greater fatigue and strain, making you more susceptible to injury. Imagine trying to lift a heavy box while twisting your back versus lifting it with a straight spine and engaged core. The latter is far more efficient and safer. Understanding this distinction is the first step toward preventing pain and improving overall well-being, especially when considering your Ideal Desk Posture.
The Hidden Dangers of Awkward Body Posture
Prolonged exposure to awkward body posture isn't just uncomfortable; it's a significant contributor to serious health issues, primarily musculoskeletal disorders (MSDs). These conditions affect your muscles, nerves, tendons, joints, cartilage, and spinal discs. When your body is forced into unnatural positions, muscles operate less efficiently, requiring more force to complete tasks. This increased exertion leads to fatigue, which, if unaddressed, can cause chronic pain and injury.
Beyond muscle fatigue, awkward postures can compress nerves and reduce blood flow, leading to numbness, tingling, and even conditions like carpal tunnel syndrome. The continuous strain can cause fatigue failure in the spine, resulting in chronic pain and degeneration. This is why addressing awkward postures is crucial for the reduction of musculoskeletal disorders. Research consistently shows that good posture is key to reducing these debilitating conditions. In many workplaces, MSDs are a leading cause of sick leave and absenteeism, impacting both individual well-being and productivity.
Key Risk Factors for Injury
Not all awkward body posture carries the same risk. Several factors determine how likely an awkward posture is to lead to injury:
- Duration: How long are you maintaining the awkward position? The longer you hold a position that deviates from neutral, the greater the strain on your body. Static postures, where muscles are tensed without movement for extended periods, are particularly problematic as they restrict blood flow and nutrient delivery.
- Frequency: How often do you repeat the awkward posture? Even if a posture is held for a short duration, frequent repetition can lead to cumulative trauma over time.
- Degree of Deviation: How far does your body part deviate from its neutral, mid-range position? The more extreme the bend, twist, or reach, the more force your muscles need to exert, and the less efficiently they can perform. For example, working with your back bent more than 30 degrees without support significantly increases risk.
- Static Loading: Holding a position without movement, such as standing or sitting in the same spot for hours, can lead to muscle fatigue, reduced blood flow, and increased pressure on spinal discs.
- Repetitive Motions: Performing the same movements repeatedly, especially if they involve awkward joint angles, can lead to overuse injuries in tendons and muscles.
- Forceful Exertions: Combining awkward postures with tasks that require significant force (e.g., lifting heavy objects, gripping tools tightly) dramatically amplifies the risk of injury. Muscles working at awkward angles are weaker and more prone to strain when exerting force.
These factors often combine, creating a synergistic effect that accelerates the development of MSDs.
The Path to Chronic Pain: The Three Stages of Injury
The development of musculoskeletal injuries from awkward body posture is often a gradual process, not a sudden event. It typically unfolds in three distinct stages, each signaling increasing severity:
Stage 1: Early Discomfort (Pain During Work) In this initial stage, you might experience pain, stiffness, or fatigue during working hours. This discomfort usually subsides or disappears completely after work, during your evening rest, or overnight. It's your body's subtle way of telling you that something isn't quite right. At this point, the damage is often minor and reversible with simple changes and rest.
Stage 2: Persistent Symptoms (Pain After Work) If Stage 1 signals are ignored, the discomfort progresses. Pain and fatigue may begin to persist even after you've stopped working. You might find it affects your sleep, making it harder to get a good night's rest. Your work capacity might diminish, and you may notice a decrease in performance or an increased need for breaks. Intervention in this stage, through ergonomic changes and Physical Therapy for Posture Training, can still prevent chronic pain.
Stage 3: Chronic and Debilitating Pain (Pain at Rest) This is the most severe stage, where pain becomes chronic and debilitating. Symptoms persist even during rest periods, making it difficult to perform basic daily tasks, impacting your quality of life significantly. At this point, the injury has become more ingrained, potentially involving structural damage to tissues. While recovery is still possible, it often requires more intensive and prolonged treatment.
The progression through these stages in the development of injuries isn't inevitable. Listening to your body's early signals – those subtle aches and pains – is invaluable. Ignoring them can lead to a long and challenging road to recovery.
Identifying Awkward Postures in Your Daily Life
Recognizing awkward body posture is the first step toward correcting it. Often, we unconsciously adopt poor postures, especially during repetitive tasks or when we're focused on work. That's why self-awareness and careful observation are key. We encourage our patients in Brooklyn to develop a keen sense of their body's alignment throughout the day.
Look for signs of strain, tension, or discomfort. If a position requires conscious effort to maintain or leaves you feeling sore and stiff, it's likely awkward. Pay attention to how your body feels at the end of the day or after specific tasks. Is your neck aching from looking down at your phone? Are your shoulders tense from typing? These are all cues your body is giving you. For more insights on recognizing problems, the identify ergonomic problems resource can be very helpful.
Common Examples of Awkward Body Posture at Work
In our diverse community, from busy offices in Park Slope to workshops in Marine Park, we see common patterns of awkward body posture:
- Working Overhead: Whether you're reaching for tools on a high shelf, painting a ceiling, or simply putting away supplies, keeping your arms above your head or elbows above your shoulders for extended periods strains your neck, shoulders, and upper back.
- Bending Forward: This is one of the most common culprits. Bending your back forward more than 30 degrees without adequate support, especially when lifting or working at low surfaces, places immense pressure on your spinal discs and lower back muscles. Think of mechanics working under a car or someone constantly picking items off the floor.
- Reaching and Over-reaching: Constantly reaching far in front, to the side, or behind your body, even for lightweight items, forces your spine and shoulders into extended, unsupported positions. This increases the moment arm, requiring more muscular effort and increasing strain.
- Twisting the Torso: Twisting your back while lifting, carrying, or even sitting and reaching for something behind you can lead to significant spinal strain. It's often combined with bending, creating a particularly risky combination.
- Kneeling and Squatting: While sometimes necessary, prolonged kneeling or squatting puts considerable pressure on your knees, hips, and ankles. Without proper support or breaks, this can lead to joint pain and muscle fatigue.
- Forward Head Posture (Tech Neck): A ubiquitous issue today, this occurs when your head juts forward, often from looking down at phones, tablets, or computer screens. For every inch your head moves forward, it adds about 10 pounds of pressure on your neck and upper back. This can lead to chronic neck pain, headaches, and rounded shoulders.
- Bent Wrists: Typing, using a mouse, or operating tools with your wrists flexed, extended, or deviated (bent sideways) places stress on tendons and nerves in the wrist and forearm, contributing to conditions like carpal tunnel syndrome or tendonitis.
These postures, when sustained or repeated, are recipes for discomfort and potential injury. Many of these issues are exacerbated by Bad Office Posture.
The Science of Prevention: Ergonomic Strategies and Solutions
The good news is that awkward body posture is largely preventable through thoughtful ergonomic design and practices. At Evolve Physical Therapy + Sports Rehabilitation, we advocate for a proactive approach, following the hierarchy of controls—a systematic way to eliminate or reduce hazards.
- Elimination: The most effective control is to eliminate the need for the awkward posture entirely. Can the task be done differently to avoid the posture?
- Substitution: If elimination isn't possible, can you substitute the task or equipment to reduce the awkwardness? For example, using a lifting device instead of manual lifting.
- Engineering Controls: These involve modifying the workstation, tools, or equipment to support neutral postures. This is often the most impactful long-term solution.
- Administrative Controls: These are changes to work practices, such as job rotation, mandatory breaks, or training on proper body mechanics.
- Personal Protective Equipment (PPE): While less effective for posture, things like knee pads for kneeling can reduce direct impact but don't correct the underlying awkward posture.
Our goal is always to move as high up this hierarchy as possible to create safer, more efficient work environments.
Mulligan's Manual: The Essential Guide to MWM Techniques
Understanding the Mulligan Concept Manual: What You Need to Know

The manual of mulligan concept is a comprehensive guide for physical therapists on using pain-free, hands-on techniques to restore movement and reduce pain.
Quick Answer: What is the Manual of Mulligan Concept?
The Manual of Mulligan Concept refers to the textbook "The Mulligan Concept of Manual Therapy: Textbook of Techniques," which covers:
- 250+ specific techniques for treating joint restrictions.
- Step-by-step instructions with annotated photos for hand placement and positioning.
- Evidence-based applications organized by body region.
- Clinical reasoning frameworks to guide technique selection.
- Home exercises and taping methods to support lasting results.
The core principle is simple: a therapist applies a gentle, sustained glide to a joint while the patient actively moves it. This combination often produces an immediate, pain-free improvement known as the "PILL response" (Pain-free, Instant, Long Lasting).
Who Developed It? New Zealand physiotherapist Brian Mulligan created this approach in 1983. It is now used worldwide to treat conditions like frozen shoulder, tennis elbow, and cervicogenic headaches.
The Mulligan Concept stands apart from traditional manual therapy by requiring active patient participation. Instead of passive manipulation, you are actively involved in your recovery, performing functional movements while the therapist guides your joints into better alignment.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, and I've used techniques from the manual of mulligan concept for nearly two decades. This patient-active approach aligns perfectly with our philosophy of addressing root causes, not just symptoms.
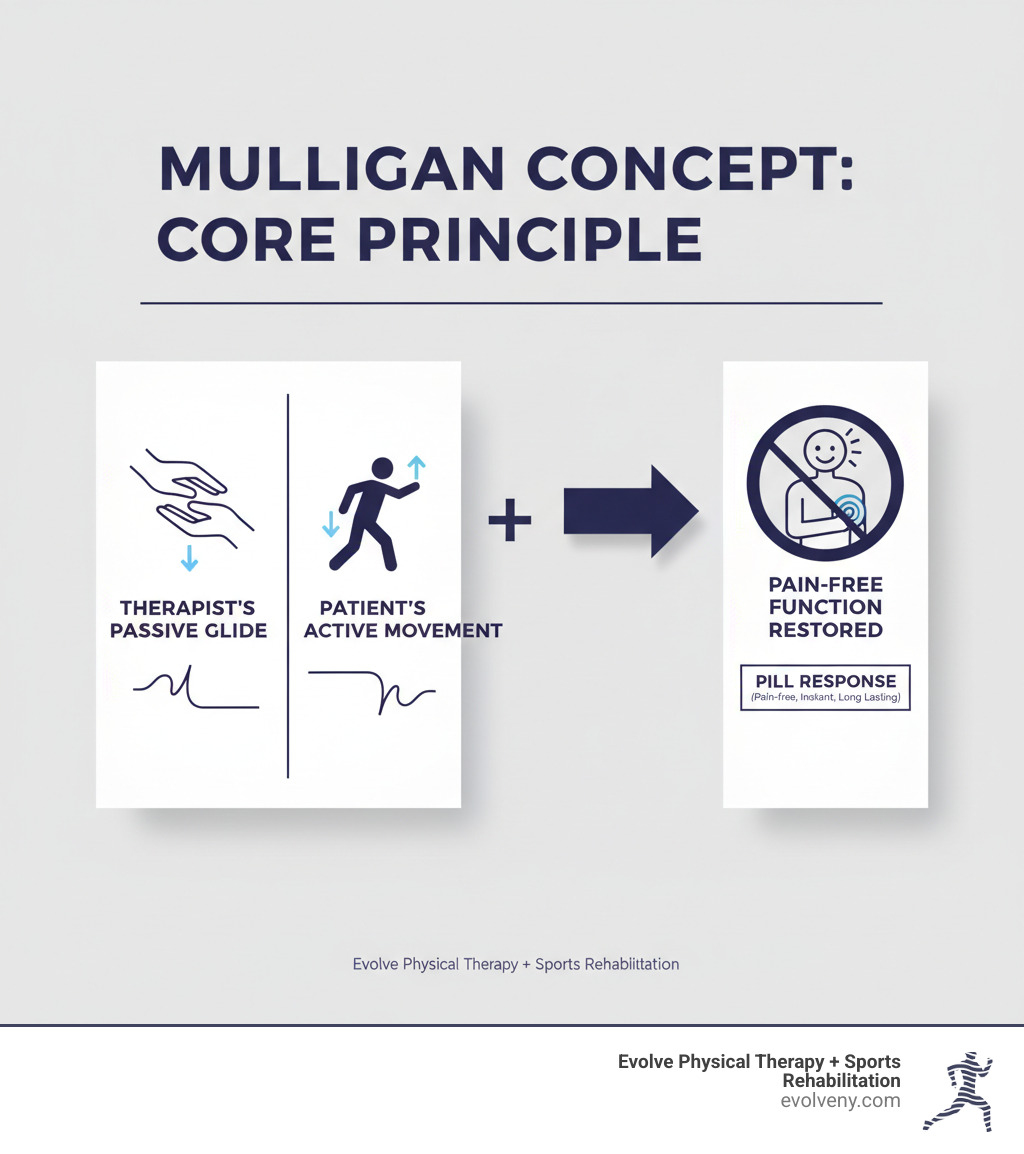
Core Principles and Foundations of the Mulligan Method
The Mulligan Concept is a philosophy of joint function that places you, the patient, at the center of your healing. Unlike passive treatments, it requires your active participation, providing instant feedback on what works.
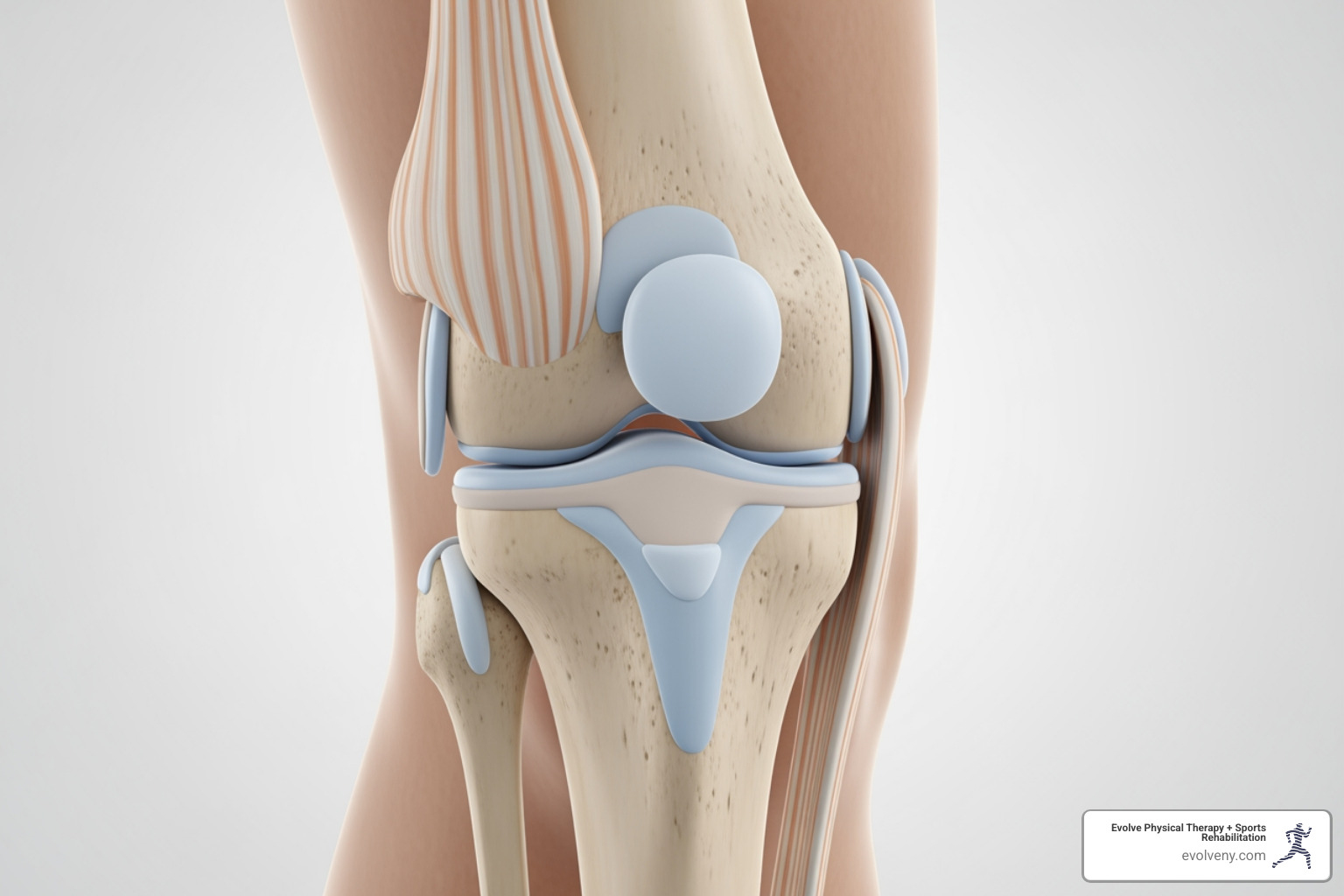
At its core, the manual of mulligan concept addresses what Brian Mulligan called "positional faults." These are minor joint misalignments, often resulting from injury or repetitive strain, that disrupt normal movement. While often invisible on X-rays, these subtle tracking errors can cause significant pain and restricted motion. The goal of a Mulligan technique is to correct this fault.
At Evolve Physical Therapy, our benchmark for success is the PILL response: Pain-free, Instant, and Long Lasting. If a technique doesn't yield immediate, pain-free improvement, we adjust our approach. This instant feedback ensures your treatment is always on the right track. To ensure safety and effectiveness, practitioners also follow the CROCKS mnemonic: a checklist for Contra-indications, Repetitions, Overpressure, Communication, Knowledge, and Sustained mobilization.
How Mulligan Differs from Other Manual Therapies
The biggest difference is active patient participation. With traditional methods, you might lie passively while a therapist performs oscillations or stretches. With the Mulligan approach, you actively perform the very movement that causes pain while we apply a sustained, corrective glide to the joint. This concurrent application of a passive glide with your active movement is what produces the pain-free result.
We focus on restoring functional movements—the specific actions that are painful in your daily life. This makes the treatment immediately relevant. Because you feel the biomechanical change in real-time, you're not just getting a joint moved; you're retraining your brain and body to accept pain-free motion, which helps make the results last. For more background on how hands-on therapy works, you can find more info about manual therapy techniques on our blog.
Key Techniques: NAGs, SNAGs, and MWMs Explained
The manual of mulligan concept details a toolkit of powerful, pain-free methods. At Evolve Physical Therapy + Sports Rehabilitation, we use these to help our Brooklyn patients achieve immediate improvements in movement. The three core techniques are NAGs, SNAGs, and MWMs, each designed for different body regions but sharing the same goal of pain-free function.

Beyond these, the approach includes Spinal Mobilization with Limb Movement (SMWLMs) and the Pain Release Phenomenon (PRP), which can produce rapid pain relief. The beauty of these methods is their versatility and focus on getting you back to doing what you love. For a deeper understanding, you can Learn more about the Mulligan Concept through additional educational resources.
NAGs (Natural Apophyseal Glides)
NAGs are gentle, rhythmic mobilizations used on the cervical (neck) and upper thoracic (upper back) spine. A therapist applies these passive, oscillating glides to the small facet joints to restore their natural movement. NAGs are ideal for highly irritable or severely restricted spinal conditions, as they are pain-free and help ease the spine into movement without causing aggravation.
SNAGs (Sustained Natural Apophyseal Glides)
SNAGs are applied to the spine, rib cage, and sacroiliac joint and require your active participation. While you perform a painful or restricted movement (like turning your head), the therapist applies a sustained glide to the joint, rendering the movement pain-free. A common example is the Headache SNAG, which provides immediate relief for cervicogenic headaches by applying a glide to the upper neck during head rotation. Repetitions are typically 6-10 but are adjusted for highly sensitive conditions.
MWMs (Mobilisation with Movement)
MWMs are the cornerstone of the Mulligan Concept, used for peripheral joints like the shoulder, elbow, knee, and ankle. The process involves the therapist applying a sustained accessory glide to a joint while you actively perform the painful or limited movement. The key is that the movement must become instantly pain-free. For example, with a painful shoulder, a therapist might apply a glide as you lift your arm, resulting in a sudden, pain-free increase in motion. Gentle overpressure may be added at the end of the movement to further improve range. Your immediate feedback guides the therapist to find the precise glide needed, making MWMs a truly patient-driven technique.
Understanding the Manual of Mulligan Concept Textbook
The primary resource for practitioners is "The Mulligan Concept of Manual Therapy: Textbook of Techniques," often referred to as the manual of mulligan concept. Authored by Brian Mulligan with experts like Wayne Hing and Toby Hall, this textbook is the definitive guide to the philosophy and application of these techniques. At Evolve Physical Therapy + Sports Rehabilitation, we use it to ensure our hands-on treatments are current and effective.

This guide recognizes that healing doesn't stop when you leave our clinic, which is why it includes detailed home exercises and taping techniques. This aligns with our belief at Evolve that you should be an active participant in your healing journey.
Key Features of the Manual of Mulligan Concept
The manual of mulligan concept is a highly practical guide for therapists. Its key features include:
- Over 250 techniques for treating joint issues throughout the body.
- Step-by-step instructions with annotated photographs showing precise hand placement, patient positioning, and mobilization direction.
- Clear organization by body region (spine, shoulder, knee, etc.), allowing for quick reference.
- A strong focus on clinical reasoning and assessment to help therapists choose the right technique for each patient.
- Guidance on home exercises and taping strategies to support and maintain progress between sessions.
This framework ensures the treatment you receive is thoughtfully selected and expertly applied. For a broader look at how we integrate various hands-on approaches into your care, you can explore More info about manual physical therapy on our site.
Who Should Read the Manual of Mulligan Concept?
The manual of mulligan concept is an essential resource for a range of healthcare professionals. Its primary audience includes:
- Physical therapists, especially those specializing in manual therapy.
- Osteopaths and chiropractors, as the techniques complement their focus on alignment and joint mechanics.
- Students of physiotherapy, osteopathy, and chiropractic, bridging the gap between theory and practice.
Any clinician who uses a hands-on, patient-active approach to treat movement restrictions and pain will find this manual invaluable. At Evolve Physical Therapy, our use of these evidence-based techniques demonstrates our commitment to providing the highest standard of care.
Conditions, Benefits, and Contraindications
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we use techniques from the manual of mulligan concept to treat a wide range of musculoskeletal issues. This versatile approach is effective for many conditions, including:
- Cervicogenic headaches and dizziness (originating from the neck)
- Lateral elbow pain (Tennis Elbow)
- Adhesive capsulitis (frozen shoulder)
- Chronic ankle sprains and stiffness
- Lumbar spine pain and sacroiliac joint dysfunction
- Pain and restricted mobility in the hip, knee, wrist, and hand
If you have pain with a specific movement or a joint that feels stuck, the Mulligan Concept may offer a solution.
Benefits and Indications
The primary benefit of the Mulligan Concept is the immediate, tangible difference patients feel. Key advantages include:
- Instant and Lasting Results: The PILL response (Pain-free, Instant, Long Lasting) is the goal. You should feel immediate pain reduction and improved movement during the session.
- Non-Invasive and Gentle: Techniques are performed without pain. If a movement hurts, the technique is adjusted or stopped. This makes treatment comfortable yet highly effective.
- Functional Restoration: We focus on restoring real-world movements that are important to you, like reaching, bending, or walking, ensuring clinic improvements translate to daily life.
- Patient Empowerment: By actively participating in your treatment, you gain confidence and a better understanding of your body, which is a powerful motivator for recovery.
Contraindications and Limitations
While highly effective, the Mulligan Concept is not appropriate for everyone. Your safety is our priority, and we adhere to strict guidelines. The main limitation is the PILL response itself: if a technique does not produce immediate, pain-free results, we stop and reassess. We proceed with caution for highly irritable conditions.
Absolute contraindications, where manual therapy is not used, include:
- Malignancy (cancer in the treatment area)
- Acute fractures
- Systemic inflammatory diseases (e.g., rheumatoid arthritis flare-up)
- Severe bone pathologies (e.g., severe osteoporosis)
- Significant ligamentous instability or vascular issues
A thorough evaluation is always performed first to ensure the Mulligan Concept is a safe and appropriate choice for your care.
Frequently Asked Questions about the Mulligan Concept
Here are answers to some of the most common inquiries we receive about the Mulligan Concept at Evolve Physical Therapy + Sports Rehabilitation.
What is the evidence base for the Mulligan Concept?
The Mulligan Concept is supported by a growing body of scientific evidence. It originated from clinical reasoning and the observation of immediate patient improvement (the PILL response). Since its development, numerous randomized controlled trials (RCTs), case studies, and systematic reviews have validated its effectiveness.
Strong evidence supports the use of Mulligan techniques for conditions affecting the cervical spine, shoulder, elbow, and lumbar spine. It is particularly well-regarded for treating cervicogenic headaches and dizziness. Research suggests the techniques work by providing altered mechanoreceptive input to the brain, essentially 'resetting' the nervous system's perception of a joint and breaking the pain-movement cycle. This combination of clinical results and scientific backing gives us confidence in using this approach.
What is the PILL response?
The PILL response is the defining principle of the Mulligan Concept. It's an acronym for Pain-free, Instant, and Long Lasting.
- Pain-free: The previously painful movement must become completely pain-free during the technique.
- Instant: The improvement in pain and motion occurs immediately.
- Long Lasting: The positive effects should persist after the treatment.
The PILL response serves as a diagnostic tool and a key indicator that the technique is being applied correctly. If there is no PILL response, the therapist immediately stops and reassesses, ensuring treatment is always safe and effective.
Where can I find training on the Mulligan Concept?
Practitioners seeking to master these techniques can find training through the Mulligan Concept Teachers Association (MCTA), the official global accrediting body. Training is offered in accredited courses, typically divided into Upper and Lower Quadrant seminars, which provide the essential hands-on instruction and clinical reasoning skills for safe and effective application. You can Find course information on official Mulligan Concept websites. At Evolve Physical Therapy, our commitment to continuous education in advanced techniques like the Mulligan Concept ensures our Brooklyn patients receive the highest quality of care.
Integrating the Mulligan Concept into Your Practice
The manual of mulligan concept provides a powerful, patient-centric approach to manual therapy that delivers immediate, pain-free results. By correcting subtle 'positional faults' with techniques like MWMs and SNAGs, therapists can restore function and empower patients in their own recovery.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we have integrated these gentle yet profound techniques into our holistic treatment plans. Our philosophy is to actively involve you in your recovery, address root causes, and work together to achieve lasting outcomes. The instant relief and collaborative nature of the Mulligan Concept align perfectly with this goal.
Whether you're dealing with a frozen shoulder, tennis elbow, or cervicogenic headaches, the techniques from the manual of mulligan concept may be what you need. Combined with our other specialized services, we can create a comprehensive treatment plan custom to your goals.
For expert, hands-on care that incorporates advanced manual therapy techniques like the Mulligan Concept, the specialists at Evolve Physical Therapy are here to help you refind pain-free movement. Learn more about our manual physical therapy services in Brooklyn and start your journey to recovery.
Soft Moves, Big Benefits: Gentle Senior Exercises
Why Movement Matters More Than Ever

Gentle exercises for seniors are low-impact activities designed to improve strength, balance, and flexibility without straining joints. Effective types include:
- Seated exercises: Ankle rotations, seated marching, arm circles
- Standing exercises: Wall push-ups, chair squats, supported leg raises
- Walking and balance exercises: Heel-to-toe walking, single-leg stands
- Flexibility work: Gentle stretches for the neck, shoulders, and legs
Around a third of people over 65 experience a fall each year, and that number jumps to half for those over 80. Regular physical activity can significantly reduce fall risk while also lowering the chances of developing chronic diseases like heart disease, diabetes, and dementia.
Even light activity matters. Adults 65 and over should aim for daily physical activity. The official recommendation is at least 150 minutes of moderate activity per week, plus strength, balance, and flexibility work on at least two days. While many older adults don't meet these guidelines, starting small makes a real difference.
Lack of physical fitness may be responsible for about half of the physical decline associated with aging. The good news is that sedentary older adults have the most to gain from increasing their activity levels.
At Evolve Physical Therapy, we've spent nearly two decades helping older adults maintain their independence through targeted movement. We've seen how gentle exercises for seniors can transform quality of life by improving balance, preventing falls, managing chronic pain, and maintaining strength for daily activities.
Why Gentle Exercise is a Game-Changer for Health and Independence
Staying active as we age isn't just about fitness; it's about holding onto the life you want to live with independence and confidence. The right kind of movement can slow or even reverse many changes we associate with aging. Even a single session of physical activity can offer health benefits like improved sleep and lower blood pressure.
A challenge is the natural loss of muscle and bone mass that increases with age. This decline can make everyday tasks harder, but gentle exercises for seniors actively combat this, helping you maintain the strength you need for daily life. The benefits are physical, mental, and emotional—a true game-changer.
The Physical Payoffs
Regular movement offers real, measurable benefits for your body.
- Stronger muscles make everything from getting out of a chair to carrying groceries easier, helping you live independently.
- Better balance is critical for preventing falls. Exercises that challenge your stability help you feel more confident on your feet. Our specialized Physical Therapy for Fall Prevention in Brooklyn program focuses on this because staying upright is that important.
- Increased flexibility means less stiffness and greater range of motion, making tasks like reaching for a high shelf or tying your shoes easier.
- Improved cardiovascular health from gentle aerobic activities like walking helps reduce the risk of heart disease, stroke, and type 2 diabetes.
- Stronger bones result from weight-bearing and strength exercises, which stimulate bone growth and density. For osteoporosis management, gentle movements strengthen supporting muscles and improve posture.
- Arthritis pain relief is another key benefit. Contrary to what some believe, gentle movement increases blood flow to joints and strengthens supporting muscles, leading to less pain. Our Physical Therapy for Arthritis programs can make a real difference.
The Mental and Emotional Boost
The mental and emotional changes from exercise are often the most surprising.
- Improved mood comes from the release of endorphins, your body's natural mood elevators, which can reduce symptoms of depression and anxiety.
- Better sleep quality is a common benefit, as physical activity helps regulate sleep cycles for more restorative rest.
- Reduced stress and anxiety can be achieved through mindful movements like yoga and Tai Chi. Yoga can reduce anxiety and chronic pain, helping you feel more centered.
- Increased self-confidence is a natural result of moving more freely and tackling daily tasks without fear.
- Cognitive function support is an exciting benefit, as studies show physical activity can improve memory, attention, and problem-solving skills.
Together, these benefits lead to a better quality of life and greater independence for years to come.
Getting Started Safely: Your Pre-Exercise Checklist
Before you begin a new exercise routine, a little preparation goes a long way in preventing injury. Think of this as your personal safety checklist.

Consult a healthcare professional. This is your most important first step. Before starting a new routine, especially with chronic conditions, talk to your doctor or a physical therapist. They can provide personalized recommendations. At Evolve Physical Therapy, we create safe and effective therapeutic exercise programs custom to your needs.
Listen to your body. It's essential to distinguish between normal muscle fatigue and sharp, stabbing, or persistent pain. Mild discomfort is a sign your muscles are working, but pain is a red flag. Stop if an exercise hurts.
Warm up and cool down. Always start with a 5-10 minute warm-up of gentle movements like marching in place or arm circles to increase blood flow and reduce injury risk. Afterward, a 5-10 minute cool-down with gentle stretches helps your body recover and improves flexibility.
Stay hydrated. Drink water before, during, and after your gentle exercises for seniors, even if you don't feel thirsty. Dehydration can cause fatigue, dizziness, and muscle cramps.
Focus on supportive nutrition. A balanced diet with lean protein, fruits, vegetables, and whole grains provides energy for exercise and nutrients for recovery. Protein is key for muscle repair, and vitamin D supports bone strength.
Choose a safe environment. Exercise in a well-lit, clutter-free space. Have a sturdy chair or counter nearby for support during standing exercises.
Wear proper footwear and clothing. Supportive shoes with good grip are crucial for preventing slips and falls. Avoid exercising in slippers or socks. Wear loose, breathable clothing for comfort and freedom of movement.
A Guide to the Best Gentle Exercises for Seniors
Here are some fantastic, low-impact gentle exercises for seniors that can be modified to your fitness level. Many can be done using a chair for support, and you can start with just your body weight. Consistency is more important than intensity when you're beginning.

Seated Gentle Exercises for Seniors
Seated exercises are perfect for those with limited mobility or who are just starting out, providing stability and security. They are a cornerstone of programs in PT for Seniors - Elderly & Senior Living Facilities.

- Seated Marching: Sit tall and alternate lifting your knees. This improves circulation and strengthens hip flexors. Aim for 20-30 reps per leg.
- Ankle Rotations: Lift one foot and gently rotate your ankle clockwise and counter-clockwise to improve flexibility and balance. Do 5-7 rotations in each direction.
- Heel and Toe Raises: With feet flat on the floor, lift your heels, then lower them and lift your toes. This strengthens lower leg muscles. Aim for 10-15 reps.
- Seated Leg Extensions: Extend one leg straight out, hold for a moment, then lower it. This builds thigh strength for walking and standing. Repeat 8-12 times per leg.
- Arm Circles: Extend arms to the sides and make small circles forward and backward to improve shoulder mobility. Do 10 circles in each direction.
- Shoulder Rolls: Shrug your shoulders up toward your ears, then roll them back and down to relieve tension. Repeat 8-10 times.
- Seated Torso Twists: Gently twist your upper body from side to side to improve spinal mobility. Do 5-8 twists per side.
Standing Gentle Exercises for Seniors
Use a chair or wall for support as you progress to these standing movements to build functional strength and balance.

- Wall Push-ups: Stand an arm's length from a wall and place your palms on it. Bend your elbows to lean in, then push back. This strengthens the upper body. Try for 10-15 reps.
- Chair Squats: Stand before a sturdy chair and lower yourself as if to sit, then stand back up just before touching the seat. This strengthens legs and glutes. Aim for 8-12 reps.
- Standing Back Leg Raises: Holding a chair, lift one leg straight back without arching your back. This strengthens glutes and hamstrings. Do 8-12 reps per leg.
- Side Leg Raises: Holding a chair, lift one leg out to the side to improve hip stability. Do 8-12 reps per leg.
- Heel-to-Toe Walk: Walk by placing the heel of one foot directly in front of the toes of the other. Use a wall for support. This improves balance and coordination. We focus on this in our Balance Training for Seniors.
Flexibility and Mobility Stretches
Perform these stretches after your muscles are warm to maintain range of motion and prevent stiffness. Explore more options with our guide to Mobility and Movement Exercises.
- Neck Stretch: Gently tilt your head from side to side, holding for 15-20 seconds to relieve tension.
- Chest Stretch: Stand in a doorway with forearms on the frame. Step forward gently to feel a stretch across your chest. Hold for 20-30 seconds.
- Seated Hamstring Stretch: Sit on a chair's edge, extend one leg, and lean forward from your hips until you feel a stretch. Hold for 20-30 seconds per leg.
- Calf Stretch: Facing a wall for support, step one foot back, keeping the leg straight and heel down. Lean forward to feel a stretch. Hold for 20-30 seconds per leg.
Building a Consistent and Enjoyable Routine
Real change happens when movement becomes a natural part of your life. Building a routine with gentle exercises for seniors is about planning and finding what you enjoy.
- Make it a habit. Start with just 10-15 minutes at a time that fits your daily schedule. Consistency will make it feel automatic.
- Set realistic goals. Aim for achievable targets, like exercising three times a week for 15 minutes. Small wins build confidence and momentum.
- Find a partner. Exercising with a spouse or friend provides accountability and makes the time more enjoyable.
- Join a class. Senior fitness programs at community centers or our specialized programs at Evolve offer structure, expert guidance, and a sense of community.
- Incorporate activity into daily life. Every movement counts. Take the stairs, do calf raises while washing dishes, or march in place during TV commercials. These mini-movements add up.
- Track your progress. Keep a simple notebook to log your activities and celebrate how far you've come. Seeing your progress is a powerful motivator.
Beyond structured exercises, many enjoyable low-impact activities count as gentle exercises for seniors:
- Walking: It's free, accessible, and offers numerous health benefits, including improved circulation and stronger bones.
- Water aerobics: The water's buoyancy supports joints while providing resistance, making it ideal for those with arthritis.
- Tai Chi: These slow, flowing movements improve balance, flexibility, and mental focus.
- Dancing: A fun way to boost heart health and lift your spirits.
- Gardening: Digging, planting, and weeding engage multiple muscle groups while you enjoy the fresh air.
Specialized programs can also help you stay active. Our Rock Steady Boxing program in Brooklyn, for example, helps individuals with Parkinson's fight back through non-contact boxing, demonstrating how targeted movement can manage chronic conditions. The secret is finding activities you genuinely enjoy.
Frequently Asked Questions about Senior Fitness
Here are answers to some of the most common questions we hear from our senior clients at Evolve Physical Therapy about starting gentle exercises for seniors.
How much exercise should a senior do each week?
The official AHA recommendations for physical activity suggest at least 150 minutes of moderate-intensity aerobic activity per week, plus strength, balance, and flexibility work on at least two days.
If that sounds overwhelming, don't worry. The most important rule is that any movement is better than none. Start with 10-minute sessions and gradually increase as you feel stronger. Breaking up long periods of sitting with even a minute of movement also makes a big difference. Consistency is more important than hitting a specific number right away.
Can I still build strength if I have joint pain?
Yes! In fact, movement is often the best medicine for joint pain. The key is choosing the right kind of low-impact exercises that strengthen the muscles around your joints without causing irritation. Stronger muscles act as shock absorbers, taking pressure off the joints and reducing pain.
Water aerobics is an excellent choice, as the water's buoyancy reduces stress on your joints. Resistance bands and stationary cycling are also great low-impact options for building strength gently.
At Evolve Physical Therapy, we specialize in creating safe programs for individuals with joint pain, including those with degenerative joint disease. The right guidance is crucial, so always consult a professional. Learn more about our approach to Physical Therapy for Degenerative Joint Disease.
What are the most important types of exercise for seniors?
A balanced routine is key for overall health and independence. Your program should include a mix of the following:
- Strength Training: Combats age-related muscle loss (sarcopenia) and strengthens bones. This can be done with bodyweight exercises, resistance bands, or light weights.
- Balance Exercises: Crucial for preventing falls. Activities like Tai Chi, heel-to-toe walking, and single-leg stands improve stability and confidence.
- Flexibility and Mobility: Prevents stiffness and makes everyday movements easier. Gentle stretching, yoga, and mobility drills are excellent for maintaining range of motion.
- Aerobic Activity: Vital for heart health, endurance, and mood. Brisk walking, swimming, and dancing are great options.
Incorporating elements from all these categories throughout the week will provide the most benefit. For more details, MedlinePlus offers valuable info about exercise for older adults.
Accept a Stronger, More Active You
You've just found a wealth of information on how gentle exercises for seniors can genuinely transform your daily life. From strengthening muscles and improving balance to lifting your spirits, the benefits touch every corner of your well-being. We've seen it at our Brooklyn clinics: even light, consistent movement makes a world of difference.
While physical inactivity contributes to many health challenges, you have the power to change that starting today. Your journey begins not with a dramatic overhaul, but with a single, simple movement.
Empowerment through movement is a real feeling you'll experience as you grow stronger. Listen to your body, respect its signals, and celebrate every small victory. Consistency is key—not perfection. Some days will be easier than others, and that's okay.
Don't let age or physical limitations hold you back from living the vibrant, active life you deserve. Every person's journey is unique, and finding the right approach for your individual goals is what matters most.
We at Evolve Physical Therapy are passionate about helping seniors in Brooklyn—from Marine Park and Gravesend to Midwood, Park Slope, and Mill Basin—move with confidence and joy. Our expert physical therapists create personalized, safe exercise plans that meet you where you are and guide you toward where you want to be.
Start today. Your future self will thank you. For a personalized and safe exercise plan custom to your specific needs and goals, the experts at Evolve Physical Therapy can create a program designed just for you.
Learn more about our Physical Therapy for Seniors program and let us help you accept a stronger, more active you.
Strengthen and Restore: Effective Physical Therapy for Your Hands
Why Your Hands Deserve Specialized Care

Your hands perform thousands of precise movements daily. When pain, stiffness, or weakness makes simple tasks like opening a jar or typing a challenge, physical therapy for hands can help. This specialized care uses targeted exercises, manual techniques, and custom treatments to restore function and improve your quality of life.
Hand and wrist symptoms are common, with work-related issues accounting for nearly one-third of all missed work days. Hand therapy effectively treats a range of conditions, including:
- Arthritis: Reduces pain and can improve grip strength by up to 25%.
- Carpal Tunnel Syndrome: Relieves nerve compression and numbness.
- Post-Surgery Recovery: Guides healing and restores mobility.
- Fractures and Injuries: Rebuilds strength and movement.
- Stroke Recovery: Retrains coordination and movement patterns.
- Repetitive Strain Injuries: Addresses work-related disorders.
I'm Lou Ezrick, founder of Evolve Physical Therapy. For nearly two decades, I've helped patients restore hand function with personalized, evidence-based rehabilitation. My experience shows that a custom approach to physical therapy for hands is the key to regaining the strength and dexterity you need.
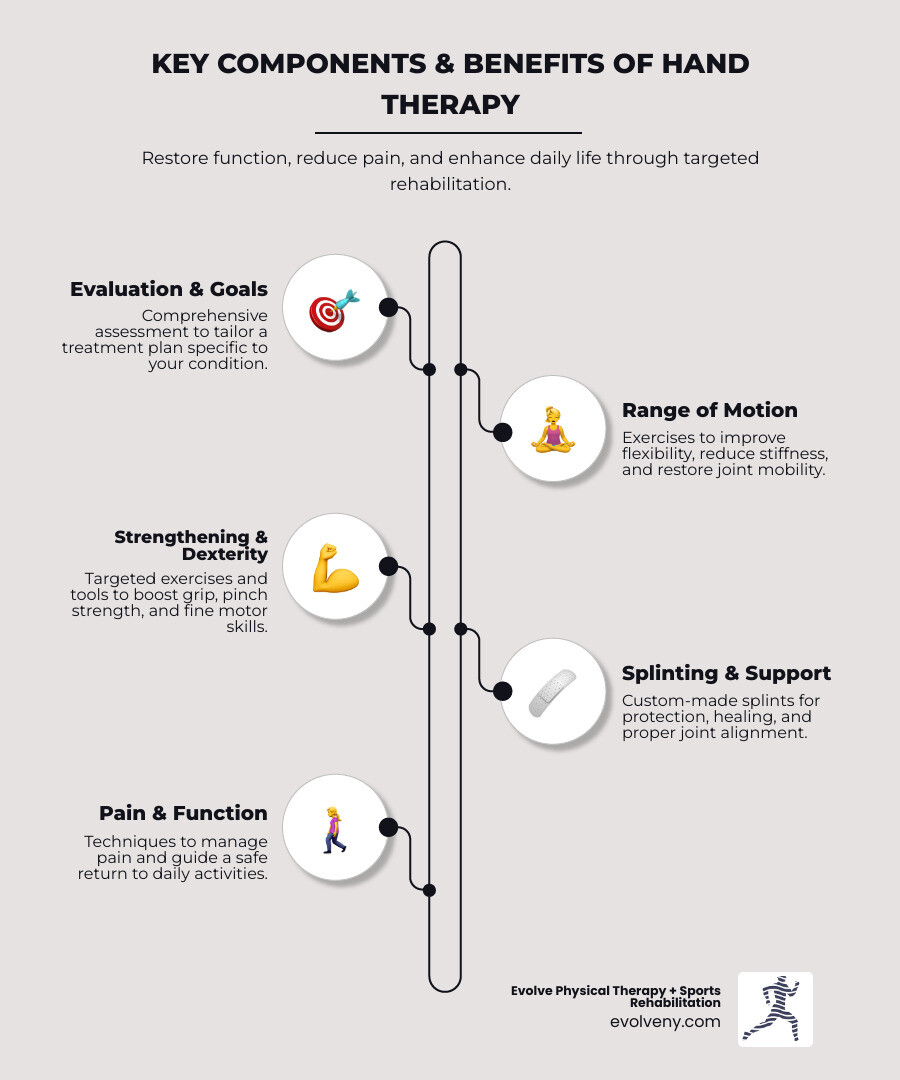
Understanding Hand Therapy and Who It Helps
Physical therapy for hands is a specialized field of rehabilitation focusing on the entire upper extremity—from your shoulder to your fingertips. It combines detailed evaluation with targeted treatment to help you return to the activities that matter most.
At Evolve Physical Therapy + Sports Rehabilitation, we see patients from Marine Park, Gravesend, and across Brooklyn with a wide range of challenges. Common conditions we treat include:
- Arthritis: Both osteoarthritis and rheumatoid arthritis cause pain and stiffness. Targeted exercises can improve grip strength by up to 25% and significantly reduce pain.
- Carpal Tunnel Syndrome: This condition causes numbness and weakness from nerve compression. Therapy can alleviate symptoms and strengthen wrist-supporting muscles.
- Post-Surgery Recovery: After procedures like tendon repair or fracture fixation, therapy is crucial for managing scar tissue and restoring movement.
- Fractures and Tendon Injuries: Specialized rehabilitation helps regain range of motion and strength after a bone has healed or a tendon is injured.
- Stroke Recovery: We work to retrain movement patterns and improve coordination, tapping into the brain's ability to relearn skills.
- Work-Related Disorders: Upper limb disorders are a leading cause of missed work, and government data shows they are among the most common work-related health issues. We address repetitive strain injuries and provide ergonomic guidance to prevent future problems.
What is a Certified Hand Therapist (CHT)?
A Certified Hand Therapist (CHT) is a physical or occupational therapist with advanced expertise in treating upper extremity conditions. Becoming a CHT is a demanding process that requires:
- At least three years of practice.
- A minimum of 4,000 hours of direct, hands-on treatment for hand and upper extremity disorders.
- Passing a comprehensive certification exam.
- Ongoing education to recertify every five years.
CHTs are uniquely qualified to evaluate and treat complex conditions, design custom interventions, and work closely with physicians to optimize your recovery.
The Benefits of Hand Therapy for Arthritis and Other Conditions
Specialized physical therapy for hands offers significant advantages that directly improve your function and quality of life.
- Pain Reduction: Targeted exercises and manual techniques decrease inflammation and alleviate discomfort.
- Improved Range of Motion: Stretching and mobilization exercises loosen stiff joints and increase flexibility.
- Increased Grip Strength: Strengthening programs are proven to build muscle, which can be transformative for daily tasks. For those with hand osteoarthritis, exercises can improve grip by up to 25%.
- Improved Dexterity: Therapy improves fine motor skills and coordination for intricate tasks.
- Joint Protection Education: Learning proper body mechanics helps manage chronic conditions like arthritis and prevent flare-ups.
- Injury Prevention: By strengthening muscles and improving movement patterns, hand therapy reduces the risk of future injuries.
The Core Components of Physical Therapy for Hands
Your journey with physical therapy for hands at Evolve Physical Therapy is entirely personalized. We begin with a comprehensive evaluation to review your medical history, assess your physical condition, and understand your goals. We test your range of motion, strength, and sensation to identify specific limitations.
Based on this evaluation, we create a personalized treatment plan that may include:
- Manual Techniques: Skilled, hands-on therapy to mobilize stiff joints, massage tight tissues, and reduce swelling.
- Therapeutic Exercises: Carefully selected movements to rebuild strength, restore flexibility, and improve coordination.
- Modalities: Tools like heat, ice, or electrical stimulation to manage pain and promote healing.
Range of Motion and Stretching Exercises
Before you can build strength, your hand must move freely. Stretching improves flexibility, reduces stiffness, and ensures tendons glide smoothly.

We guide you through gentle, effective movements. Examples include tendon gliding exercises to help tendons move freely, the prayer stretch to release wrist tension, and wrist bends to restore flexibility in all directions. The key is to move slowly and smoothly, without sharp pain.
Strengthening and Dexterity Exercises
Once your range of motion improves, we focus on building strength to improve your grip and pinch. For stroke survivors, these exercises also stimulate neuroplasticity—the brain's ability to rewire itself and relearn skills. We often use functional tasks like unscrewing caps or manipulating coins to make therapy directly applicable to your daily life.
Common tools we use in our Brooklyn clinic include:
- Therapy putty and stress balls for grip strength.
- Hand grippers and elastic bands for adjustable resistance.
- Household items like coins, clothespins, or beads to sharpen dexterity and coordination.
We carefully match the resistance to your ability, ensuring you are challenged but never overwhelmed.
The Role of Custom Splints and Orthotics
Sometimes, your hand needs extra support to heal or function correctly. Custom splints (orthotics) can provide protection after surgery, support weak joints, or reduce stress on painful areas, which is especially helpful for arthritis.
Unlike off-the-shelf braces, our Certified Hand Therapists fabricate custom orthotics in our Brooklyn clinics. We mold materials directly to your hand and arm, ensuring a comfortable and precise fit. This custom approach maximizes your recovery by holding your hand in the optimal position for healing and function, making it a vital tool in your rehabilitation.
Your At-Home Hand Exercise Program: Safety and Technique
An effective physical therapy for hands program continues at home. Consistency is key—regularly performing your exercises, even for a few minutes daily, yields better results than infrequent, long sessions.

Proper technique is just as important as consistency. Always warm up your hands first by soaking them in warm water or rubbing them together. As you exercise, remember the golden rule: if it causes sharp, shooting, or increasing pain, stop. A gentle stretch or mild muscle fatigue is normal, but pain is a warning sign.
Safe and Effective Physical Therapy for Hands at Home
To make your home program successful, follow these guidelines:
- Start slowly. Don't do more than your therapist recommends. Your tissues need time to adapt.
- Listen to your body. Differentiate between a productive stretch and harmful pain.
- Focus on smooth, controlled motions. Avoid jerky movements, which can cause injury.
- Exercise both hands. This helps maintain balance and can even help your injured hand recover faster through a process called cross-education.
Research shows that patients who stick to their home programs see significant improvements in hand function. You are an active participant in your recovery.
Sample Exercises for Common Hand Conditions
Your program will be customized, but here are some examples of the types of exercises we might recommend. Always follow your therapist's specific instructions.
- For Arthritis: Gentle exercises like fist making, finger lifts, and thumb stabilization help maintain flexibility and reduce stiffness.
- For Post-Stroke Recovery: Passive stretches (using your unaffected hand to move the affected one) prevent stiffness, while object manipulation tasks help retrain the brain.
- For Carpal Tunnel Syndrome: Tendon glides and wrist extensor stretches help nerves and tendons move more freely through the wrist.
When to Seek Professional Help for Hand Pain
While minor aches may resolve with rest, certain warning signs indicate it's time to see a professional. Early intervention often leads to a faster, more complete recovery.
Seek professional help if you experience:
- Persistent pain or stiffness that doesn't improve after a few days.
- Numbness or tingling, especially if it follows a pattern in your fingers.
- Noticeable weakness that makes it hard to grip objects or perform daily tasks.
- A significant injury or recent surgery on your hand or wrist.
- Interference with your daily life, work, or hobbies.
- No improvement from home exercises, or if they make your symptoms worse.
Our team at Evolve Physical Therapy in Brooklyn is here to help you reclaim your function and comfort.
What to Expect During Your First Hand Therapy Visit
Your first appointment is about understanding your unique situation and creating a clear path to recovery. We start with a comprehensive conversation about your medical history, symptoms, and goals.
Next is a physical assessment where our therapist examines your hand, wrist, arm, and even your shoulder. We will test your range of motion, measure your grip and pinch strength, and may check your sensation and coordination.
By the end of the visit, you will have a personalized treatment plan. We'll explain our findings, discuss realistic goals, and start you with your first exercises and education, ensuring you feel informed and empowered.
How a Therapist Adapts Physical Therapy for Hands
Professional hand therapy is not a one-size-fits-all solution. We customize every treatment plan to your specific diagnosis, ability level, and goals. A pianist with a tendon injury requires a different approach than a construction worker with arthritis. We adapt exercises for your limitations, such as severe stiffness or pain, and may recommend adaptive equipment to help you maintain independence. Most importantly, we provide hands-on guidance, correcting your form and ensuring you perform each movement safely and effectively for the best possible outcome.
Frequently Asked Questions about Hand Therapy
We understand you have questions about physical therapy for hands. Here are answers to some common concerns we hear at our Brooklyn clinics.
How long does hand therapy take to show results?
There is no single timeline. Recovery depends on your condition, its severity, and your consistency with treatment. A simple strain might improve in a few weeks, while post-surgical or stroke recovery can take several months. Patients who consistently attend sessions and perform their home exercises typically see better, faster results. Your therapist will set realistic goals and track your progress.
Can hand therapy help me avoid surgery?
In many cases, yes. For conditions like carpal tunnel syndrome, trigger finger, and mild to moderate arthritis, therapy is a powerful conservative treatment. By strengthening supporting muscles, improving movement patterns, and reducing inflammation, we address the root causes of your pain. Many of our patients have successfully avoided surgery, and even if it's eventually needed, pre-surgical therapy can improve your outcome.
Do I need a doctor's referral for hand therapy?
In New York, you have direct access to physical therapy, meaning you can schedule an evaluation with us without a doctor's referral. However, your insurance plan may have different rules and might require a physician's prescription to cover treatment. We recommend calling your insurance provider to confirm their requirements for physical therapy coverage before your first visit. Our team can help you steer this process.
Begin Your Path to Stronger, Healthier Hands
Your hands allow you to work, create, and connect with the world. When pain or weakness gets in the way, it can be frustrating and isolating.
As we've explored, physical therapy for hands offers a clear path toward relief and restored function. Through targeted exercises, manual therapy, and personalized guidance from a skilled therapist, you can regain strength, reduce pain, and improve your quality of life.
At Evolve Physical Therapy + Sports Rehabilitation, our specialists in Brooklyn create personalized programs to help you recover from injury, manage chronic conditions, and return to the activities you love. We serve patients throughout Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin with a hands-on, evidence-based approach.
You don't have to live with hand pain. Take the first step toward stronger, healthier hands today.
Helping Kids Soar: A Parent's Guide to Pediatric PT in Brooklyn
Why Brooklyn Pediatric Physical Therapy Matters for Your Child's Development

Brooklyn pediatric physical therapy helps children overcome physical challenges, reach developmental milestones, and build the strength and coordination they need to thrive. Whether your child is an infant with torticollis, a toddler with developmental delays, or a teen recovering from a sports injury, specialized pediatric PT can make a profound difference.
Quick Answer: What You Need to Know About Brooklyn Pediatric Physical Therapy
- What it treats: Developmental delays, torticollis, cerebral palsy, autism spectrum disorder, sports injuries, balance issues, and orthopedic conditions
- How it works: Play-based, individualized therapy sessions (typically 45-60 minutes) that make progress feel like fun
- Who provides it: Licensed physical therapists trained in pediatric development and movement
- Where to find it: Clinic-based therapy, home visits, and school-based services across Brooklyn neighborhoods
- Cost: Most insurance plans accepted; Early Intervention services available for children ages 0-3 through NYS Department of Health
Why Brooklyn Families Need Specialized Pediatric Care
Brooklyn's active lifestyle demands that children can run and play with confidence. When physical challenges hold a child back, pediatric physical therapy provides the targeted support they need.
Unlike adult therapy, pediatric PT requires specialized knowledge of child development and uses play-based techniques to make exercises feel like games. Early intervention is especially critical. Addressing motor delays in the first few years of life, when a child's brain is most adaptable, leads to better long-term outcomes. This is why programs like New York State's Early Intervention services focus on children ages 0-3.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. While my practice primarily serves adults, I've seen how crucial specialized Brooklyn pediatric physical therapy is for our community. Understanding the pediatric landscape helps me guide parents toward the care their children need to reach their full potential.

Is PT Right for My Child? Common Signs and Conditions Treated
As a parent, you know your child best. If you notice your baby struggling with tummy time, your toddler delaying walking, or your school-aged child seeming unusually clumsy, it's worth paying attention. These can be early signs that Brooklyn pediatric physical therapy could make a meaningful difference.

Physical therapists look for specific indicators like missing developmental milestones (not rolling, sitting, or walking on time), difficulty with balance or coordination, weakness on one side of the body, or pain during movement.
Common conditions treated in pediatric physical therapy include developmental delays, where a child needs extra support to catch up. Torticollis (tight neck muscles causing a head tilt) and Plagiocephaly (flat head syndrome) respond very well to early physical therapy. Other frequent concerns include persistent toe walking, low muscle tone that affects posture, and general coordination issues. The goal is always to empower your child to move freely and confidently. You can see how therapists work with children through engaging activities by visiting our page on Pediatric Physical Therapy for Kids.
Helping Children with Neurodevelopmental Disorders
For children with neurodevelopmental disorders, physical therapy is essential for improving function and quality of life. Conditions like Cerebral Palsy, Autism Spectrum Disorder, Spina Bifida, and Down Syndrome present unique physical challenges.
Brooklyn pediatric physical therapy for these conditions focuses on managing symptoms like muscle stiffness (spasticity) or low muscle tone (hypotonia). For a child with Cerebral Palsy, therapy can improve motor skills and manage pain. Children on the autism spectrum often benefit from therapy that addresses motor planning and coordination. For kids with Down Syndrome, PT can improve strength and stability. The goal is to help each child function at their highest potential. You can learn more about developmental disabilities from the CDC to better understand what your child might be experiencing.
Addressing Orthopedic Conditions and Sports Injuries in Youth
Active kids and young athletes in Brooklyn also face physical challenges, from orthopedic conditions to sports injuries.
Scoliosis (abnormal spine curvature) can benefit from PT to improve posture and strengthen core muscles. Pediatric fractures require careful rehabilitation to restore full function. Conditions like Osgood-Schlatter disease (knee pain) and Sever's disease (heel pain) in active kids respond well to targeted exercises.
Overuse injuries from youth sports are also a major concern. For adolescent athletes dealing with injuries like an ACL tear or a concussion, the goal is a safe return to play. This involves not just healing the injury but also teaching proper movement patterns and implementing injury prevention strategies to avoid future problems. A good physical therapist helps young athletes understand their bodies, learn proper warm-ups, and develop fitness habits for life.
The Journey of Brooklyn Pediatric Physical Therapy: What to Expect
Starting pediatric physical therapy can feel overwhelming, but the journey is designed to help your child gain confidence and skills at their own pace. A Brooklyn pediatric physical therapy clinic is a space designed for fun, with colorful mats, swings, balance beams, and therapeutic toys.

The journey begins with a comprehensive initial evaluation, typically lasting 75-90 minutes. The therapist will observe your child play to assess their strength, coordination, balance, and range of motion, sometimes using standardized tests like the Peabody Motor Development Scales (PDMS-3). A key part of this session is discussing your observations and goals for your child.
From this information, the therapist creates an individualized treatment plan with specific, achievable goals, creating a roadmap for your child's progress. To prepare, dress your child in comfortable clothes and bring any relevant medical records. Most importantly, come ready to share your insights—you know your child best. You can learn more about how we approach this process in our blog post: Pediatric and Adolescent Physical Therapy.
Making Therapy Fun: The Power of Play-Based Techniques
The secret to pediatric physical therapy is that kids don't know they're doing therapy—they're just playing. Play-based therapy is grounded in the understanding that children learn and develop through play. When a child is engaged and having fun, they work harder and make faster progress.
For example, a child needing to strengthen their core might swing on a platform swing while reaching for colorful balls. They are so absorbed in the game that they don't realize their core muscles are working overtime. That's the magic of play-based techniques.
Sensory gyms with swings, climbing structures, and ball pits become the stage for therapeutic activities. Crawling through a tunnel builds upper body strength, while walking on a balance beam develops postural control. These engaging activities target gross motor skills, balance, and coordination while feeling like pure fun. This approach also builds confidence and a sense of competence. You can see examples of these dynamic sessions in our Pediatric Physical Therapy gallery.
The Structure of Brooklyn Pediatric Physical Therapy Sessions
Once a treatment plan is set, your child will likely attend weekly sessions, with the frequency adjusted to their needs. Each session typically lasts 45-60 minutes—long enough for meaningful work without causing fatigue.
During these sessions, the therapist continuously monitors progress and adjusts the plan over time to ensure it remains effective and appropriately challenging. Collaboration with families is essential to this process. Your child spends most of their time with you, so your therapist will provide a home exercise program and guidance on how to integrate activities into daily routines.
This partnership accelerates progress and helps skills generalize beyond the clinic. The structure provides consistency, while a skilled therapist offers the flexibility to adapt to your child's energy and motivation each day. For a deeper look at how we approach Brooklyn pediatric physical therapy with this balance of structure and flexibility, visit our page on Pediatric Physical Therapy in Brooklyn.
A Parent's Role: Choosing a Provider and Supporting Progress
As a parent, you are your child's most powerful advocate. Your involvement in Brooklyn pediatric physical therapy is crucial at every stage, from selecting a provider to supporting progress at home. A strong partnership between parents and therapists, often as part of a multidisciplinary team with other specialists, creates the best outcomes for your child.

How to Choose the Right Pediatric PT Provider in Brooklyn
Finding the right provider is manageable when you know what to look for. Prioritize a licensed physical therapist with specialized pediatric experience relevant to your child's condition. The clinic environment should be welcoming and equipped with age-appropriate, sensory-rich equipment. Ensure the provider creates individualized care plans based on thorough assessments and family input.
Strong collaboration with families is non-negotiable; a good therapist empowers you with strategies and values your insights. Also, consider the provider's specializations and the location and accessibility of the clinic. Therapy works best when it fits into your life without adding stress. Whether you're in Park Slope, Mill Basin, Marine Park, Gravesend, or Midwood, a convenient location helps maintain consistency.
When interviewing potential therapists, ask key questions to find the right fit:
- What is your experience with my child's specific condition?
- How do you make therapy engaging and fun?
- What does parent involvement and communication look like in your practice?
- What is the typical frequency and duration of therapy sessions?
Navigating Costs, Insurance, and Therapy Settings
Understanding costs is essential. Most Brooklyn pediatric physical therapy providers accept a range of insurance plans. Before your first visit, verify your benefits, including co-pays, deductibles, and in-network status. Our team at Evolve Physical Therapy can help you steer these details.
For children aged 0-3, the NYS Early Intervention Program is a valuable state-funded resource providing services at no direct cost to eligible families. Therapy can occur in different settings. Clinic-based therapy offers access to specialized equipment and sensory gyms. We have two convenient Brooklyn locations in Mill Basin and Park Slope. Home-based services can be ideal for infants, while school-based services can be integrated into an older child's school day.
To learn more about our approach and locations, visit our page on Pediatric Physical Therapy Brooklyn.
How Parents Can Support Their Child's Progress at Home
What happens between sessions is just as important as the sessions themselves. Your active support at home can make a remarkable difference.
Follow the home exercise program your therapist provides. Even 5-10 minutes of daily practice reinforces skills and accelerates progress. Integrating activities into daily routines—like balancing on a curb or crawling through a box tunnel—makes practice feel natural. Maintain open communication with therapists, sharing what's working and what's not. Your observations are invaluable. Finally, create a supportive environment that encourages movement and celebrate small victories. Your enthusiasm fuels your child's motivation and builds their confidence.
Frequently Asked Questions about Pediatric Physical Therapy
Parents often have thoughtful questions when considering pediatric physical therapy for the first time. Here are answers to some of the most common concerns.
Why is early intervention so critical for infants and toddlers?
The first three years of a child's life are a critical window for development due to high brain plasticity. Early intervention in Brooklyn pediatric physical therapy takes advantage of this period to build a strong foundation for motor skills like rolling, sitting, crawling, and walking. Addressing challenges early helps prevent secondary issues, such as muscle imbalances or compensatory movements that can cause problems later. Research consistently shows that children who receive early intervention have better long-term developmental outcomes and often require less support as they grow.
What is the difference between pediatric physical therapy (PT) and occupational therapy (OT)?
While PT and OT often work together, they focus on different areas. Pediatric physical therapy (PT) centers on gross motor skills—the large movements needed for mobility. PTs work on walking, running, jumping, balance, and overall strength and coordination.
Occupational therapy (OT), in contrast, focuses on fine motor skills and the activities of daily living. OTs help children with tasks like writing, using scissors, dressing, self-feeding, and sensory processing to foster independence in school, play, and self-care. Often, children benefit from both disciplines.
What are the long-term benefits of consistent physical therapy?
Consistent Brooklyn pediatric physical therapy is an investment in your child's future. The long-term benefits include improved mobility and independence, allowing children to steer their world with confidence. This physical competence boosts self-esteem, encouraging them to try new things and participate more fully in school, sports, and social activities.
From a medical standpoint, consistent therapy can reduce the need for future interventions like surgery by addressing issues early and preventing secondary complications. The greatest benefit is an improved quality of life. Pediatric PT empowers children to live active, fulfilling lives and builds a foundation for a healthy, independent adulthood.
Conclusion: Taking the Next Step for Your Child's Health in Brooklyn
This guide shows how Brooklyn pediatric physical therapy can transform a child's life. Whether for an infant with torticollis, a toddler with developmental delays, or a teen with a sports injury, the right intervention builds physical strength, coordination, confidence, and independence.
The journey of pediatric physical therapy is a partnership. It works best with an individualized, play-based plan and your active involvement at home. As a parent, your willingness to seek help and support your child's progress makes all the difference.
At Evolve Physical Therapy, we believe in a hands-on, personalized approach. While my practice primarily focuses on adults, I am committed to ensuring Brooklyn families have the resources for their children's physical development. If you have concerns about your child's movement, balance, or strength, I encourage you to reach out to a specialized pediatric physical therapist.
We understand that physical health is a family matter. Many principles we use with adults—functional movement, injury prevention, and building strength for real-life activities—also apply to children. To learn more about our approach to sports rehabilitation and how we help patients of all ages return to the activities they love, please visit our page: Learn more about our approach to sports and pediatric rehab in Brooklyn.
Every child deserves to explore their world with confidence. If you're ready to empower your child, don't wait. Reach out to a qualified pediatric physical therapist today to start this important journey.
Heal Your Neck: A How-To Guide for Cervical Herniated Disc Physical Therapy
Relieving Neck Pain: Your Introduction to Cervical Disc Herniation and Physical Therapy Exercises

If you're seeking relief for a cervical herniated disc, here are some commonly recommended physical therapy exercises:
- Chin Tucks (Neck Retraction): Gently tuck your chin towards your throat to align your head.
- Neck Extensions: Carefully extend your head backward, often supported by a towel.
- Shoulder Retractions (Scapular Squeeze): Squeeze your shoulder blades together to improve posture.
- Lateral Bends: Gently tilt your head side-to-side to stretch neck muscles.
- Scalene Stretch: Isolate neck side muscles for relief of tension.
Struggling with neck pain that radiates into your arm? You might have a cervical herniated disc. This occurs when a disc between your neck vertebrae presses on a nerve, causing pain and limiting movement. The good news is that conservative treatment, like the physical therapy exercises for cervical disc herniation in this guide, is often highly effective.
This guide will show you how specific movements and stretches can empower you to manage your symptoms, strengthen your neck, and improve your well-being from home.
As Louis Ezrick, MSPT, founder of Evolve Physical Therapy, I've spent nearly two decades helping patients with conditions like cervical disc herniation. My expertise in movement optimization and chronic pain management allows me to guide you through these effective exercises.
Understanding Your Cervical Herniated Disc: Causes, Symptoms, and Key Principles
Your spine is a stack of vertebrae with soft, cushiony discs between them that act as shock absorbers. Each disc has a soft, gel-like center (nucleus pulposus) and a tough outer ring (annulus fibrosus). A herniated disc occurs when the inner gel pushes through a tear in the outer ring, which can then press on or "pinch" a nearby nerve root in your neck.
This condition, called cervical radiculopathy, often causes symptoms that travel down your arm. The American Academy of Orthopaedic Surgeons notes that cervical radiculopathy symptoms include burning sensations, tingling, and weakness in the arm, shoulder, or hand.
What causes a disc to herniate? Aging is the most common factor, as discs lose flexibility over time, typically affecting people in their 30s to 50s. Trauma from accidents or injuries can also cause a sudden herniation. A major contributor for many is poor posture.
The common forward head position from phone and computer use puts immense stress on your neck. This chronic strain can lead to herniation over time. Good posture is essential for protecting your neck from unnecessary strain.
Symptoms of a cervical herniated disc vary but often include:
- Radiating arm pain that is sharp or burning.
- Numbness or tingling ("pins and needles") in your arm or fingers.
- Weakness in arm or hand muscles, affecting grip strength.
- Neck pain, muscle spasms, and stiffness.
A key principle in physical therapy exercises for cervical disc herniation is centralization of symptoms. This means we want exercises to move your symptoms from your arm or hand back toward your spine. This is a good sign. If symptoms spread further down your arm (peripheralization), it's a red flag to stop the exercise as it may be irritating the nerve.
Posture and ergonomics are also vital. Adjusting your computer screen to eye level, using a supportive chair, and keeping your head balanced over your shoulders are essential parts of your healing process.
Your Guide to Physical Therapy Exercises for Cervical Disc Herniation
Beginning your recovery with physical therapy exercises for cervical disc herniation requires a thoughtful and consistent approach. Before starting, warm up gently with shoulder rolls or a warm compress to prepare your muscles. As you perform each exercise, move slowly and deliberately, as jerky movements can aggravate your condition.
Consistency trumps intensity. Daily, correct exercise for 10 minutes is more effective than one intense weekly session. Research supports this, with a 2009 randomized clinical trial showing that patients who actively participated in physical therapy and home exercises had significantly better outcomes. The exercises below are categorized into foundational movements, stretches, and strengthening to provide a comprehensive approach to healing.
Foundational Physical Therapy Exercises for Cervical Disc Herniation
These movements are designed to decompress your cervical spine and improve alignment. Remember the centralization principle: symptoms moving toward your neck is a positive sign.
Chin Tucks (Neck Retraction)

This is one of the most powerful exercises for correcting forward head posture.
How to perform: Sit or stand tall. Gently tuck your chin straight back, as if making a double chin, feeling a stretch at the base of your skull. Keep your eyes level. Hold for 5-10 seconds, then release slowly.
Reps and sets: Start with 2-3 sets of 10 repetitions. Aim to do them frequently throughout the day (10-15 times).
Purpose: This exercise strengthens deep neck flexors, promotes proper head alignment over your shoulders, and relieves pressure on cervical discs.
Neck Extensions (Supported or Supine)
This exercise gently opens the front of your neck to reduce disc pressure.
How to perform (Supported with a towel): Sit upright. Place a rolled-up towel behind your neck, holding both ends. Gently extend your head backward over the chair's backrest, using the towel for support and control. Perform 5-10 slow extensions.
How to perform (Supine – lying on your back): Lie on a bed with your head hanging gently off the edge. Slowly lower your head backward to feel a stretch. For less intensity, place a pillow under your upper back. Hold for 1 minute, rest for 1 minute, and repeat 5-10 times.
Purpose: Neck extensions counteract forward bending, release tension in front neck muscles, and can help guide disc material away from irritated nerves.
Stretches to Complement Your Physical Therapy Exercises for Cervical Disc Herniation
Stretching addresses the muscle tension that accompanies a herniated disc. Stop if you feel sharp pain or symptoms spreading down your arm.
Lateral Neck Bend

This targets the muscles on the sides of your neck.
How to perform: Sit tall and gently tilt your head, bringing your ear toward your shoulder without shrugging. For a deeper stretch, use your hand to apply very light pressure. Hold for 20-30 seconds. Repeat on the other side.
Purpose: Improves side-to-side flexibility and releases tension.
Upper Trapezius Stretch
This stretch targets the muscles running from your neck to your shoulders.
How to perform: Sit comfortably and place one hand behind your back to anchor the shoulder down. With your opposite hand, gently pull your head down and toward your shoulder in a diagonal direction. Hold for 20-30 seconds. Repeat on the other side.
Purpose: Releases chronic tightness in the upper trapezius, which can contribute to neck pain and headaches.
Scalene Stretch
This targets deep muscles in the front and sides of your neck, which can contribute to nerve irritation.
How to perform: Sit tall and grasp the bottom of your chair with one hand to anchor your shoulder. Gently tilt your head to the opposite shoulder, then rotate your head slightly upward. You should feel a stretch in the front/side of your neck. Hold for 20-30 seconds. Repeat on the other side.
Purpose: Lengthens the scalene muscles to reduce pressure on nerves traveling to your arm.
Pectoral (Chest) Stretch
Tight chest muscles pull shoulders forward, worsening neck strain.
How to perform: Stand in a doorway. Place one arm on the frame with your elbow bent at 90 degrees. Step forward gently with the opposite foot until you feel a stretch across your chest. Hold for 30-60 seconds. Repeat on the other side.
Purpose: Opens the chest to improve shoulder posture, which indirectly supports better neck alignment.
Strengthening for Long-Term Support
Once initial pain subsides, strengthening exercises provide long-term stability and protection for your cervical spine.
Scapular Retraction (Shoulder Blade Squeeze)

This strengthens the muscles between your shoulder blades, which are essential for good posture.
How to perform: Sit or stand tall. Squeeze your shoulder blades back and down, as if holding a pencil between them. Avoid shrugging your shoulders up. Hold the squeeze for 3-5 seconds, then release slowly.
Reps and sets: Start with 2 sets of 10 repetitions, gradually increasing to 3 sets of 10-15. You can add a resistance band for more challenge.
Purpose: Strengthens key postural muscles to counteract the forward shoulder position from daily activities.
Isometric Neck Holds
These exercises build strength by contracting muscles without movement, which is safe for your discs.
How to perform: Sit or stand tall. For each direction, gently press your head against your hand while your neck muscles resist the movement. Your head should not move. Hold each contraction for 5-10 seconds.
- Forward: Place your palm on your forehead and press forward.
- Backward: Clasp hands behind your head and press backward.
- Side: Place your hand on the side of your head and press sideways. Repeat on the other side.
Reps and sets: Perform 3 repetitions for each of the four directions, twice daily.
Purpose: Builds muscular endurance and stability in all supporting neck muscles without stressing the discs, serving as a bridge to more advanced strengthening.
Movements to Avoid and When to See a Professional
Knowing what not to do is as important as knowing which physical therapy exercises for cervical disc herniation to perform. Protecting your neck during healing is crucial.
Exercises and Activities to Skip
To prevent worsening your symptoms, avoid these activities for now:
- High-Impact Activities: Running, jumping, and other jarring movements can compress the spine and aggravate a herniated disc.
- Heavy Lifting and Powerlifting: Straining, especially with overhead lifts, puts significant pressure on cervical discs. Holding your breath during exertion can also worsen the issue.
- Sudden, Sharp Movements: Avoid quick twists, jerks, or abrupt neck movements. Stick to gentle, controlled motions.
- Full Neck Circles: These can put unnecessary strain on an injured disc. It's better to perform specific, controlled stretches.
- Any Exercise Causing Peripheralization: This is the most important rule. If an exercise causes pain, numbness, or tingling to spread down your arm or hand, stop immediately. This signal means the nerve is being irritated.
Understanding Other Treatments and Red Flags
Beyond exercises, other treatments can support your recovery.
Cervical Traction
Cervical traction gently stretches your neck to create space between vertebrae, which can relieve pressure on compressed nerves. At Evolve Physical Therapy, we use advanced, non-surgical spinal decompression that incorporates active movements to isolate specific spinal segments for improved relief. We generally advise against home-based, over-the-door traction units, as they can sometimes stress the jaw (TMJ) and may only provide temporary relief. Professional, controlled methods are safer and more effective.
Ice and Heat Therapy
- Ice Therapy: Use for 15-20 minutes at a time during the acute phase (first 48-72 hours) or after an activity that causes a flare-up to reduce inflammation and numb pain.
- Heat Therapy: After the initial inflammation subsides, use a moist heat pack for 15-20 minutes to relax tight muscles and promote healing by increasing blood flow.
When to Seek Professional Help
Always consult a physician or physical therapist before starting a new exercise program, especially if your pain is from an accident or is worsening. Certain red flag symptoms require immediate medical attention:
- Worsening Weakness: Progressive loss of strength in your arm or hand.
- Loss of Coordination: Difficulty with fine motor skills (like buttoning a shirt) or balance issues.
- Severe, Unrelenting Pain: Pain that doesn't improve with rest.
- Bowel or Bladder Changes: Any new incontinence or difficulty with urination/defecation.
These symptoms could indicate significant nerve or spinal cord compression (cervical myelopathy) and require prompt medical evaluation.
Frequently Asked Questions about Neck Pain from a Herniated Disc
We hear these questions often from our patients across Brooklyn, from Marine Park to Park Slope. Here are answers to the most common concerns.
How long does it take for exercises to help a cervical herniated disc?
Healing time varies for each person. Some notice improvement within a few days, while for others, it may take several weeks to feel significant relief. There is no one-size-fits-all timeline.
Consistency is crucial. Performing your physical therapy exercises for cervical disc herniation regularly is key to success. Research on cervical radiculopathy shows that active treatment, including physical therapy, has a significant positive impact on pain and disability at the 6-week mark. While immediate results aren't guaranteed, many people see measurable progress within a month to six weeks of consistent effort. Patience and persistence are your allies.
Should I feel pain when doing these exercises?
It's important to distinguish between discomfort and sharp pain. A gentle stretch or muscle fatigue is normal and expected. However, sharp, shooting, or stabbing pain is not okay.
If an exercise intensifies your pain or causes symptoms to spread down your arm (peripheralization), stop immediately. This is a red flag that the movement is irritating the nerve. The goal is for symptoms to move closer to your neck (centralization). The point of these exercises is to reduce your pain, not add to it.
Can these exercises make my herniated disc worse?
When performed correctly and with attention to your body's feedback, the risk of worsening your condition with these specific exercises is very low. They are designed to be gentle and promote healing.
However, improper form or pushing through sharp pain can aggravate your condition. Ignoring peripheralization (symptoms spreading down your arm) is also counterproductive. This is why starting gently and moving slowly is so important.
If you are ever unsure about an exercise or if a movement consistently worsens your symptoms, stop and consult with a physical therapist. At Evolve Physical Therapy, we ensure your form is correct and tailor your program to your specific needs, making sure every movement is safe and effective for your recovery.
Take the Next Step in Healing Your Neck
Living with a cervical herniated disc is challenging, but you now have a roadmap to recovery. The key takeaways are to understand your condition, follow safe exercise principles, and stay consistent. Evidence shows that conservative treatment, especially physical therapy exercises for cervical disc herniation, is remarkably effective for most people, often avoiding the need for surgery.
At Evolve Physical Therapy + Sports Rehabilitation, we treat the whole person, not just the symptoms. Our Brooklyn team, serving Marine Park, Gravesend, Midwood, Mill Basin, and Park Slope, uses a hands-on approach to guide you through recovery. We'll evaluate your unique situation and give you the confidence to take control of your health. From our innovative Rock Steady Boxing program for Parkinson's patients (featured on NBC News) to our comprehensive disc rehabilitation, we are passionate about helping you move better and live fully.
Your neck pain doesn't have to be a constant. You've learned the exercises and principles; now it's time to take action. We're here to create a plan customized for you.
Get a personalized physical therapy plan for your herniated disc in Brooklyn
























