
Brooklyn Physical Therapy News- Evolve NY
Before the Cut: A Guide to Pre-Surgical Physical Therapy
Why Pre-Surgery Physical Therapy Can Transform Your Recovery

Pre surgery physical therapy, also known as prehabilitation or "prehab," is a program of exercise and education designed to strengthen your body before an operation. Instead of waiting until after surgery to begin rehabilitation, you start building strength and mobility weeks ahead of time, giving your body a head start on recovery.
Quick Answer: What is Pre-Surgery Physical Therapy?
- What it is: A proactive physical therapy program completed before your scheduled surgery.
- What it includes: Customized exercises, strength training, mobility work, and patient education.
- Who benefits: Patients preparing for joint replacement, cardiac surgery, or any major operation.
- Key benefits: Faster recovery, shorter hospital stays, fewer complications, and improved surgical outcomes.
- When to start: Ideally 2-4 weeks before surgery, but even one week can help.
- Goal: To build physical and mental resilience so you enter surgery stronger and recover faster.
Surgery places significant stress on your body. Approaching it without preparation can lead to longer hospital stays, more complications, and a slower return to normal life. Prehabilitation is like training for a marathon—it prepares your body for the challenge ahead.
Research shows that patients who complete pre surgery physical therapy recover more quickly and experience a 29% reduction in post-acute care services. They often go home from the hospital sooner and have lower rates of opioid dependence. This preparation doesn't just strengthen your muscles; it reduces anxiety and gives you a sense of control over your recovery.
The concept is simple: the stronger you are going into surgery, the stronger you'll be coming out. Prehabilitation gives your body the best possible foundation for healing.
I'm Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation in Brooklyn. With nearly two decades of experience, I've seen how pre surgery physical therapy transforms not just surgical outcomes, but patients' entire recovery experiences through hands-on, individualized care.
What is Prehabilitation and Why Does It Matter?
Traditional care is reactive: you wait until after surgery to start healing. Pre surgery physical therapy is proactive: you build strength, mobility, and resilience before you enter the operating room. This simple shift changes everything.
As the American College of Surgeons puts it, "Generally, the more fit and active you are going into a surgical procedure, the more likely you are to retain a higher level of function after." When you're stronger going in, you're stronger coming out.
Prehabilitation builds your physiological reserve—your body's capacity to handle the stress of surgery. An operation triggers inflammation and muscle breakdown. A larger reserve of strength and fitness helps your body absorb these stresses without declining as much. You start from a higher baseline, so even after the temporary setback of surgery, you're in better shape.
Research on prehabilitation for major surgery confirms this approach reduces the body's adverse stress response. By conditioning your body beforehand, you're training it to weather the storm more effectively.
Beyond the physical benefits, prehabilitation puts you back in control. Instead of feeling like surgery is something that happens to you, you become an active participant in your own recovery. At Evolve Physical Therapy + Sports Rehabilitation, we see how this sense of empowerment helps patients approach their surgery with more confidence and less fear.
The Proven Benefits of Pre-Surgery Physical Therapy
Investing time in pre surgery physical therapy sets you up for a smoother, faster recovery. The benefits touch every aspect of your surgical journey, from your hospital stay to your mental readiness.
Improved Physical Readiness and Strength
The primary benefit of prehab is that you'll be physically stronger. We focus on building up the muscles around the surgical site and improving your overall fitness, giving your body the resources it needs to heal.
- Increased Muscle Strength and Mobility: Before a joint replacement, we strengthen surrounding muscles and increase your range of motion. This directly impacts how well you'll move after surgery.
- Reduced Muscle Loss: Inactivity leads to muscle atrophy. Medical research shows this can happen quickly. Pre-surgical exercises help you maintain or even build muscle mass, so you can better resist the natural muscle loss that occurs post-op.
- Better Heart and Lung Function: Aerobic conditioning like walking or cycling boosts your cardiovascular fitness. As The American College of Surgeons emphasizes, higher fitness correlates with fewer postoperative complications.
Faster Recovery and Better Surgical Outcomes
The real payoff of pre surgery physical therapy appears in your recovery timeline. Patients who complete prehab programs often experience:
- Shorter Hospital Stays: Proper preparation can help patients go home sooner, sometimes even the same day, allowing them to recover in the comfort of their own home in Brooklyn.
- Reduced Need for Post-Operative Care: One study found that prehab led to a 29% decrease in post-acute care services. This means less time in rehabilitation facilities.
- Lower Risk of Complications: A stronger body handles surgical stress more efficiently. A comprehensive review of prehabilitation showed a clear trend toward fewer complications among patients who did prehab.
- Reduced Opioid Dependency: Patients who received physical therapy before knee replacement had a lower chance of long-term opioid use. Prehab helps you manage pain naturally through movement.
- Quicker Return to Daily Activities: Research shows that prehab patients recover their baseline function significantly faster, allowing them to get back to work, hobbies, and family life sooner.
Bolstering Your Mental and Emotional Health
Your mental state is crucial for a successful recovery. Prehab addresses this often-overlooked aspect of surgical preparation.
- Reduced Surgical Anxiety: Education about what to expect before, during, and after your procedure reduces fear of the unknown.
- Increased Patient Empowerment: Actively participating in your own care is powerful. You become a partner in your health journey, which can transform your entire surgical experience.
- Positive Mindset for Recovery: Taking action and building strength naturally improves your mood and outlook, creating genuine optimism based on real progress.
- Improved Pain Coping Skills: We teach you safe movement patterns and pain relief techniques, helping you develop better coping strategies for a more manageable recovery.
Your Prehabilitation Game Plan: What to Expect
At Evolve Physical Therapy + Sports Rehabilitation, we build a comprehensive, personalized game plan that fits your body, surgery, and life. Our hands-on approach ensures you have support and guidance every step of the way.

Who is a Candidate for Pre-Surgery Physical Therapy?
Almost anyone facing surgery can benefit from prehab, but it's especially valuable for:
- Joint replacement patients (hip, knee, shoulder): Strengthening surrounding muscles can transform your recovery, helping you heal faster.
- Cardiac and abdominal surgery patients: Improving cardiovascular fitness and core strength helps your body handle the stress of the operation.
- Cancer surgery patients: Prehab addresses the deconditioning and muscle loss that can accompany cancer and its treatments, reducing complications and speeding recovery.
- Frail or deconditioned individuals: Building physiological reserves before surgery is crucial for this high-risk group, often making the difference between a smooth recovery and a difficult one.
- Athletes: For sports-related surgeries (ACL, rotator cuff), we work to maintain overall fitness and strengthen supporting muscles, setting the stage for an efficient return to sport.
Core Components of Your Personalized Plan
Your prehabilitation journey is custom to you and follows a clear path:
- Initial Evaluation: Our licensed physical therapists assess your current strength, stability, range of motion, and overall function. We discuss your medical history, your upcoming surgery, and your personal goals.
- Baseline Measurements: We use objective tests (like the 6-minute walk test) to establish your starting point. This allows us to track your progress and show you tangible proof of your hard work.
- Custom Exercise Program: We design a program specifically for your needs, including:
- Strength Training: Targeted exercises using resistance bands, light weights, or bodyweight to build up key muscles.
- Aerobic Conditioning: Activities like walking or cycling to improve your cardiovascular endurance.
- Balance and Flexibility Training: Exercises to reduce your risk of falls and improve mobility.
- Breathing Exercises: For abdominal or thoracic surgeries, inspiratory muscle training can significantly reduce pulmonary complications.
- Education: We teach you proper body mechanics, pain management strategies, and what to expect post-surgery. For joint replacement patients, this includes practicing with crutches or walkers and learning to steer daily activities safely.
For example, a pre-knee replacement program might include exercises like quad sets, straight leg raises, heel slides, ankle pumps, and gluteal sets.
The Role of Nutrition and Lifestyle
We take a holistic view of pre surgery physical therapy. Exercise is key, but nutrition and lifestyle choices are also critical for healing.
- Nutrition: Your body needs adequate protein (1.2-1.5g per kg of body weight) to repair and build muscle. We'll guide you on incorporating protein-rich foods. Hydration is also vital.
- Smoking and Alcohol: Quitting smoking at least 30 days before surgery can cut wound complication rates by 50%. Reducing alcohol intake also significantly lessens surgical risks. We can provide resources to help, like those from Kaiser Permanente on wellness.
- Stress Management: Chronic stress impacts healing. We encourage mindfulness, meditation, and relaxation techniques to reduce anxiety.
- Sleep: Prioritize quality sleep, as your body does much of its repair work while you rest.
- Chronic Conditions: Work with your physician to optimize conditions like diabetes or anemia before your operation.
Frequently Asked Questions about Pre-Surgical PT
Our patients in Brooklyn often have thoughtful questions about pre surgery physical therapy. Here are answers to the most common concerns.
Can Pre-Surgery Physical Therapy Help Me Avoid the Operation?
Sometimes, yes. For certain conditions like low back pain, knee osteoarthritis, or some meniscus tears, physical therapy is the recommended first line of treatment. We've helped many patients in our Brooklyn clinics improve their symptoms so significantly that surgery could be delayed or avoided entirely.
Whether this is possible depends on your specific diagnosis and its severity. However, even if you ultimately need surgery, the time spent in therapy is not wasted. Every bit of strength you gain becomes part of your prehabilitation, giving you a head start on recovery.
Are There Times When Prehabilitation Isn't Recommended?
While prehab is beneficial for most, your safety is our top priority. Prehabilitation is generally not recommended in a few situations:
- Emergency Surgery: There is simply no time for a prehab program in urgent, life-saving scenarios.
- Unstable Medical Conditions: Patients with severe cardiac instability, uncontrolled diabetes, or acute infections may need to stabilize their condition before starting an exercise program.
We always require your surgeon's approval before beginning a prehab program. We partner with your entire medical team to ensure the best possible outcome for you.
How is Pre-Hab Different from Post-Op Rehab?
This is a great question. While both aim to improve function, they are different in their timing and focus.
Prehab is proactive. It happens before surgery to build up your body's strength and endurance. Think of it as filling your tank before a long trip. We are building resilience to prepare your body for the stress ahead.
Rehab is reactive. It starts after surgery to restore function that was lost. Here, we are refilling the tank from a lower starting point, working to get you back to your baseline.
Prehab and rehab are two parts of a continuous journey. By entering surgery stronger, you experience less post-operative weakness and are primed to respond more quickly to post-op exercises. You start your recovery from a higher point, which makes the entire process smoother and faster.
Conclusion: Take Control of Your Surgical Outcome
Surgery doesn't have to be something that just happens to you. Pre surgery physical therapy gives you the power to actively shape your recovery, starting weeks before your operation.
By building a stronger, more resilient version of yourself, you fundamentally change how your body responds to surgery. Research shows that prehab leads to shorter hospital stays, fewer complications, and a faster return to the life you love. Most importantly, you enter surgery feeling confident and in control.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen our hands-on prehabilitation programs transform surgical outcomes for countless Brooklyn residents. Our individualized approach ensures you get the preparation your body needs, whether you're in Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin.
Remember the proven principle: the stronger you are going into surgery, the stronger you'll be coming out.
Your next step is simple. Talk to your surgeon about prehab. If they agree, reach out to us. We'll create a personalized plan to prepare your body and equip you with the confidence to steer your recovery successfully. Don't wait to start your recovery—be proactive and take control.
Appendix: Relevant Statistics
The research behind pre surgery physical therapy tells a compelling story of faster recovery and better outcomes. Here are some key statistics.
Recovery and Rehabilitation
- Preoperative physical therapy is linked to a 29% decrease in post-acute care services.
- Patients who had PT before and/or after knee replacement had a lower chance of long-term opioid use.
- For colorectal cancer patients, 80% who did prehab recovered baseline function by 8 weeks post-surgery, compared to only 40% in a control group.
Timeline and Hospital Stay
- The optimal prehab program duration is 4 to 8 weeks, but even shorter programs are beneficial.
- Prehabilitation is associated with shorter hospital stays, with some patients going home the same day.
Complication Reduction
- A meta-analysis showed a significant reduction in overall morbidity (OR 0.63) and pulmonary morbidity (OR 0.4) in prehab groups.
Lifestyle Factors
- Quitting smoking 30 days before and after surgery can decrease wound complications by 50%.
- Drinking more than 5 units of alcohol per day can triple the postoperative complication rate.
Nutrition and Medical Optimization
- Recommended preoperative protein intake is 1.2 to 1.5 g/kg/day (compared to 0.8 g/kg/day for healthy adults).
- Preoperative anemia management aims for hemoglobin levels above 13 g/dl.
Mental Health and Patient Satisfaction
- Cognitive prehabilitation programs have been shown to reduce delirium rates from 23% to 13.2%.
- 81.5% of patients would join a prehabilitation program if available, and 60% felt it helped them prepare mentally for surgery.
Muscle Loss
- It only takes a few weeks to lose muscle from inactivity, highlighting the urgency of building strength before surgery.
These statistics paint a clear picture: prehab is a proven strategy for a better surgical journey.
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
Ready to Roll? Pediatric PTA Jobs Await!
Why Pediatric Physical Therapy Assistant Jobs Are Worth Exploring

Pediatric physical therapy assistant jobs offer a unique opportunity to make a meaningful difference in children's lives while building a stable, rewarding career. If you're searching for positions, here's what you need to know:
Quick Facts About Pediatric PTA Jobs:
- Job Outlook: Strong demand with 231+ positions listed in regions like York, PA alone
- Salary Range: National average of $1,549/week ($80,500+/year), with some states like Virginia averaging 1% higher
- Experience Level: Abundant entry-level positions (209 listings in some markets)
- Work Settings: Hospitals, outpatient clinics, schools, early intervention programs, and home health
- Requirements: Associate's degree from CAPTE-accredited program, state licensure via NPTE-PTA exam
- Job Types: Full-time (most common), part-time, PRN, and travel contracts available
The role involves implementing treatment plans under a licensed physical therapist's supervision, using modalities like exercise, neuromuscular reeducation, mobilization, and play-based therapy to help children from infancy through adolescence overcome developmental delays, injuries, and medical conditions.
As Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, I've seen how crucial skilled assistants are in delivering comprehensive care. Pediatric physical therapy assistant jobs are some of the most fulfilling opportunities in our field. Whether you're starting your career or specializing, this growing field offers stability and the chance to celebrate genuine milestones with young patients and their families.

1. The Role: What a Pediatric PTA Actually Does
A career in pediatric physical therapy assistant jobs is dynamic and fulfilling. The core of the role is helping children, from infants to teens, reach their full physical potential. You might help a toddler take their first steps, assist a middle schooler recovering from a sports injury, or support a teen with a chronic condition.

As a pediatric PTA, you implement treatment plans created by licensed physical therapists. You work directly with children, guiding them through therapeutic exercises, using play-based therapy to make movements fun, and applying specialized techniques like neuromuscular reeducation to help them regain motor control. Your toolkit is varied and includes therapeutic exercise, heat or cold therapy, mobilization techniques, taping, and modalities like electrical stimulation and ultrasound. Each intervention is chosen to match the child's specific needs.
A huge part of the role involves patient education and family communication. You partner with the entire family, teaching parents and caregivers home exercises and how to use adaptive equipment. This family-centered approach is key to making progress carry over from the clinic to everyday life. You'll work with children with a wide range of conditions, including neurological disorders like cerebral palsy, sensorimotor delays, musculoskeletal conditions like scoliosis, complex medical conditions, and trauma-related injuries.
What makes this work special is adapting everything to be age-appropriate, which requires creativity and patience. A session with a three-year-old is very different from one with a thirteen-year-old. Learn more about this individualized approach in our insights on Pediatric Physical Therapy.
The Rewards and Challenges
The rewards of this job are profound. You'll witness life-changing milestones, like a child's first independent steps or a teen returning to their favorite sport. You build genuine, trusting relationships with patients and their families, becoming a consistent source of support. Celebrating every small bit of progress makes the work deeply meaningful.
Of course, the job has challenges. It requires emotional resilience for children with significant health issues, and there are physical demands like lifting and assisting children. Creative problem-solving is essential to keep kids engaged. But for those in this field, the rewards far outweigh the challenges.
Collaboration in Care
As a PTA, you work in partnership with a supervising physical therapist (PT). The PT evaluates patients and creates the plan of care, while you implement it. This requires regular communication to review progress and make adjustments. You're also part of a larger interdisciplinary team, collaborating with occupational therapists, speech pathologists, and doctors. In schools, you'll partner with educators to integrate therapy goals into the academic day.
Documenting progress is also essential. Detailed records of sessions, responses, and changes in ability are crucial for team communication, continuity of care, and meeting regulatory standards. This collaborative environment is one of the best parts of the job, as you're surrounded by professionals who share your commitment to helping children thrive.
2. The Requirements: Your Path to Becoming a Pediatric PTA
If you're serious about pursuing pediatric physical therapy assistant jobs, you'll need to follow a clear path of education, training, and certification. This well-established pathway is designed to prepare you for the rewarding work ahead.

Your journey begins with an Associate's degree from a program accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE). This ensures your program meets national standards. These two-year programs blend classroom learning with essential hands-on clinical experience through rotations, where you'll work directly with patients under supervision. Many programs offer pediatric rotations, which are invaluable for applying classroom knowledge.
After your degree, you must pass the National Physical Therapy Examination for Physical Therapist Assistants (NPTE-PTA). This comprehensive exam is the key to professional practice. Passing it allows you to obtain your state licensure. Each state has specific licensing requirements, so check them early. The American Physical Therapy Association (APTA) is an excellent resource for national and state-specific regulations.
Essential Skills for Success
Beyond exams, success as a pediatric PTA requires a special set of personal qualities.
- Patience: Children progress at their own pace. Your ability to remain patient and encouraging through repetition is key.
- Creativity: This turns therapy into an adventure. Making exercises into games is essential, as children learn best when having fun.
- Strong communication skills: You must explain exercises to a child, discuss progress with parents, and collaborate clearly with other healthcare professionals.
- Empathy: This allows you to connect with the child and their family, understanding their frustrations and worries.
- Physical stamina: It's an active job that involves being on your feet, demonstrating exercises, and assisting or lifting children.
- Adaptability: You must be ready to adjust your plan based on a child's mood or unexpected progress.
- Observation skills: These are needed to notice small changes that signal progress or problems, helping you modify treatment and inform the supervising PT.
These skills are vital in specialized areas like pediatric sports rehabilitation. At Evolve Physical Therapy + Sports Rehabilitation, we know these qualities create exceptional care, as discussed in Pediatric Sports PT Just What the Coach Ordered.
The combination of formal education, proper licensing, and these essential personal skills creates the foundation for a fulfilling career in pediatric physical therapy assistant jobs.
3. The Market: Exploring Pediatric Physical Therapy Assistant Jobs
The job market for pediatric PTAs is thriving. The Bureau of Labor Statistics projects strong growth for all PTAs, with pediatric physical therapy assistant jobs being no exception. This demand is driven by increased awareness of early intervention, more diagnoses requiring PT, and recognition of specialized pediatric care's value.
Excitingly, there are abundant entry-level positions. This means you can break into the field with the right education, licensure, and passion, without years of prior experience. The variety of positions is also impressive, including full-time, part-time, per diem (PRN), and travel PTA contracts. Travel positions offer competitive pay and diverse experiences, allowing you to find a job that accommodates your lifestyle. You can see how rewarding this work is in our approach to Pediatric Physical Therapy for Kids.
Salary Expectations for pediatric physical therapy assistant jobs
Fair compensation is important, and the salary outlook for pediatric physical therapy assistant jobs is encouraging. The national average is around $1,549 per week (over $80,500 annually), providing a solid income, often with excellent benefits. Salaries vary by region; for instance, PTAs in Virginia earn slightly above the national average. Hourly rates can range widely, from $29.81 to $42.89 in some markets, reflecting factors like experience and specialized skills.
Your experience level is crucial for earning potential. While entry-level salaries are competitive, your compensation increases with experience and specialized skills. The work setting (e.g., hospital vs. school) also affects compensation, though each offers unique non-monetary rewards.
Where to Find pediatric physical therapy assistant jobs
Finding the right job is easier than ever with numerous resources available.
Online job boards like Indeed, Glassdoor, and LinkedIn are a great starting point. A targeted LinkedIn job search can reveal many opportunities. Also, check healthcare-specific sites like Vivian.com and AMN Healthcare for permanent and travel roles.
Check hospital career pages directly. Major children's hospitals and practices like ours in Brooklyn often post openings on their websites first, giving you a competitive edge.
Professional networks are also invaluable. Connect with peers through the American Physical Therapy Association, conferences, or local chapters to find unlisted opportunities. Many positions are filled through referrals. Our team at Evolve Physical Therapy + Sports Rehabilitation has grown this way, through colleagues who share our commitment to patient-centered care.
4. The Workplaces: Diverse Settings for a Rewarding Career
One of the most exciting things about pursuing pediatric physical therapy assistant jobs is the variety of places you can practice. This diversity means you can find a setting that resonates with your personality and professional goals.
Outpatient clinics, like our practice at Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, are a common setting. Here, you build long-term relationships with families, helping children with sports injuries, chronic conditions, or developmental delays.
Children's hospitals offer a , specialized environment. You'll work with children with acute medical needs or those recovering from surgery as part of a large, collaborative team of specialists.
Inpatient rehabilitation facilities provide intensive therapy for children needing concentrated care after a major illness or injury. With multiple daily sessions, you'll help children regain the skills needed to return home.
School systems are another rewarding setting. You'll help children with disabilities participate fully in their education, collaborating with teachers and staff to align therapy with educational goals.
Early intervention programs focus on infants and toddlers (birth to age three). You'll often provide therapy in the child's natural environment, like their home or daycare, teaching parents to incorporate therapeutic activities into daily routines.
Home health services bring therapy to families who face travel challenges. Working in a child's home provides valuable insights for practical recommendations.
The beauty of this career is its flexibility. You aren't locked into one setting and can transition as your interests evolve, allowing you to shape a career that matches your professional and personal goals. Our approach to Pediatric Physical Therapy NYC accepts this diversity, serving communities across Brooklyn, including Marine Park, Gravesend, and Park Slope, and recognizing each family's unique needs.
Frequently Asked Questions about Pediatric PTA Careers
Navigating a career path in pediatric physical therapy can bring up many questions. Here, we address some of the most common inquiries about pediatric physical therapy assistant jobs.
What is the main difference between a pediatric physical therapist (PT) and a physical therapist assistant (PTA)?
Understanding the distinction between these two roles is essential.
Physical Therapists (PTs) hold a Doctor of Physical Therapy (DPT) degree. They are the diagnosticians who evaluate patients, diagnose movement dysfunctions, and create the comprehensive plan of care. PTs set goals, determine interventions, modify plans, and supervise PTAs.
Physical Therapist Assistants (PTAs) earn a two-year Associate's degree from a CAPTE-accredited program. Working under PT supervision, they are essential for implementing the care plan. PTAs spend the most direct time with children, carrying out treatments, monitoring progress, and educating families.
In short, the PT designs the roadmap, and the PTA guides the child on the journey. Both roles are crucial for successful outcomes, with the PT overseeing the child's overall progress. The difference in education level reflects their different scopes of practice, but both share a passion for helping children.
Do I need a special certification to work in pediatrics as a PTA?
The short answer is no, a special pediatric certification is not universally required. Your state license, earned by passing the NPTE-PTA exam after completing an accredited associate's degree, is the legal requirement to practice.
However, specialized knowledge is highly valuable and preferred by employers. Many PTAs deepen their expertise through continuing education in areas like pediatric development and play-based therapy. The APTA Advanced Proficiency Pathway is another option that recognizes PTAs with advanced pediatric knowledge and skill.
Most employers, including Evolve Physical Therapy + Sports Rehabilitation, also provide employer-specific training. This on-the-job training is invaluable for learning the specific protocols of your workplace. Gaining actual pediatric experience is what truly builds your competence and confidence, and many entry-level jobs exist to provide this opportunity under mentorship.
What does a typical day look like for a pediatric PTA?
There's no truly "typical" day, which is part of the appeal. Every child and session is different, offering new challenges and opportunities to witness progress. However, a day has a certain rhythm.
Your day will likely include reviewing patient charts, preparing treatment areas with age-appropriate equipment, and then executing therapy sessions. The heart of the day is spent working directly with a diverse group of children, requiring constant adaptation, creativity, and patience to keep them motivated.
After each session, documenting progress notes is crucial for continuity of care and regulatory compliance. Throughout the day, you'll also be collaborating with the supervising PT and educating families on home exercises and progress. In multidisciplinary settings like ours at Evolve, you'll also coordinate with other specialists like occupational or speech therapists. Every day is a dynamic blend of clinical skill, creativity, and compassionate interaction.
Conclusion
If you've made it this far, you're likely drawn to pediatric physical therapy assistant jobs for good reason. This career path offers the chance to wake up each day knowing your work directly impacts a child's ability to play, learn, and thrive.
This guide has shown what it means to be a pediatric PTA: implementing creative treatment plans, collaborating with families and teams, and celebrating every small victory. We've covered the straightforward educational path, the strong job market with competitive salaries, and the diverse work settings available to you.
At Evolve Physical Therapy + Sports Rehabilitation, we know skilled and compassionate PTAs are essential for our holistic, hands-on care. Our practice was built on treating the whole person, which for children means engaging them through play and supporting their families.
This career offers purpose. While challenging, the moments of joy make it worthwhile. The children we serve in Brooklyn and beyond deserve dedicated professionals with both skill and heart.
If this sounds like the career you've been searching for, we'd love to see you become part of this rewarding field. Take a moment to explore a career in pediatric physical therapy in Brooklyn and find how you can make a genuine difference in the lives of children and their families. The journey starts with a single step—and we're here to support you along the way.
Which Manual Therapy Technique is Right for You? Maitland, Mulligan, or Kaltenborn
Understanding Manual Therapy: Three Proven Approaches to Joint Mobilization

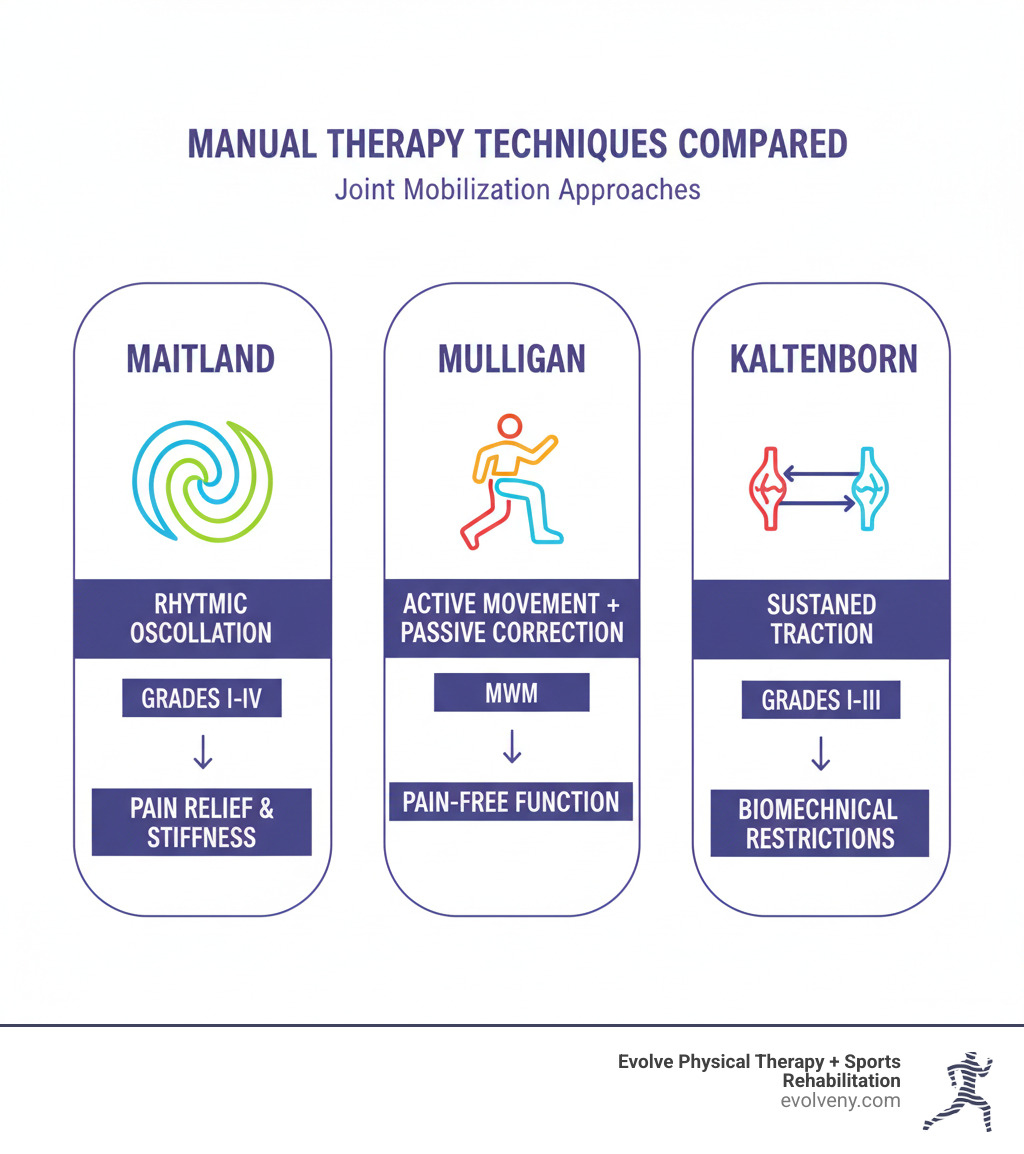
Maitland mulligan kaltenborn techniques are three distinct manual therapy approaches that physical therapists use to restore joint function and reduce pain. Here's how they differ:
| Technique | Core Approach | Best For |
|---|---|---|
| Maitland | Rhythmic oscillatory movements (Grades I-IV) | Pain relief and joint stiffness |
| Mulligan | Active movement + passive joint correction (MWM) | Restoring pain-free functional movement |
| Kaltenborn | Sustained joint traction (Grades I-III) | Biomechanical joint restrictions |
If you're dealing with joint pain or stiffness, you're not alone. Joint mobilization is a cornerstone of manual therapy that offers targeted ways to restore movement and alleviate pain. Understanding the different approaches can feel overwhelming, but each has a unique strength.
The truth is, there's no single "best" technique. Maitland uses graded oscillations to modulate pain and improve mobility. Mulligan emphasizes pain-free movement by combining your active participation with passive joint corrections. Kaltenborn takes a biomechanical approach, using sustained traction to restore normal joint mechanics.
As Lou Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades applying these techniques to help patients overcome complex musculoskeletal challenges. Understanding these three foundational approaches is essential for creating individualized treatment plans that address the root cause of dysfunction—not just symptoms.
The Maitland Concept: A Graded Oscillatory Approach
Developed by Australian physiotherapist Geoffrey Maitland, this technique provides a systematic way to address joint problems. The Maitland approach uses rhythmic, oscillatory movements to restore "joint play"—the subtle gliding and rolling that occurs in healthy joints.
Instead of forcing movement, we apply carefully graded oscillations. These gentle, repetitive movements can either soothe pain or gradually stretch tight tissues, depending on your body's needs. At Evolve Physical Therapy, the Maitland concept is invaluable during assessments, helping us form a hypothesis about why a joint isn't moving properly. For more details, visit our Manual Therapy blog category.
Core Principles and Grading System
The precision of maitland mulligan kaltenborn techniques is exemplified by Maitland's grading system. We use five distinct grades to control the amount and location of movement applied to a joint.
- Grade I: Small, gentle oscillations at the beginning of the joint's range, used primarily for pain relief via the Pain Gate Theory.
- Grade II: Larger oscillations within the available pain-free range, also for reducing pain and muscle guarding.
- Grade III: Large oscillations that move up to the limit of the range, designed to stretch tight tissues and address stiffness.
- Grade IV: Small, precise oscillations at the end of the available range, providing a targeted stretch to stiff joint capsules and ligaments.
- Grade V: A quick thrust technique, though Grades I-IV are the cornerstones of Maitland's oscillatory approach.
Lower grades (I and II) work on a neurophysiological level to reduce pain, while higher grades (III and IV) provide a mechanical stretch to lengthen shortened tissues. A key feature of the Maitland approach is continuous reassessment. We apply a technique, check your response (pain, movement), and adjust our approach accordingly. This feedback loop ensures your treatment is always customized. A comparison of Maitland and Kaltenborn mobilization techniques for shoulder pain has shown its clinical effectiveness in improving range of motion and reducing pain.
When is the Maitland Technique Used?
The Maitland technique excels in specific situations:
- Joint stiffness: Grades III and IV are highly effective for stretching stiff capsules and ligaments in conditions like frozen shoulder or arthritic knees.
- Pain-dominant conditions: The gentler Grades I and II can modulate discomfort without causing more pain, creating a window of opportunity for movement and exercise.
- Spinal and peripheral joints: Its versatility makes it one of the most widely applicable manual therapy approaches for the neck, back, shoulders, hips, and other joints.
- Complex or fluctuating symptoms: The continuous evaluation process makes Maitland ideal for cases where symptoms change, allowing us to adapt treatment quickly based on your response.
The Mulligan Concept: Mobilization with Movement (MWM)
Developed by New Zealand physiotherapist Brian Mulligan, this approach revolutionized manual therapy by involving the patient actively in their recovery. Mulligan's concept addresses minor "positional faults" or tracking issues in joints that cause pain during movement.
The core idea is Mobilization with Movement (MWM): a therapist applies a sustained passive mobilization while the patient actively performs the previously painful movement. This combination often allows the joint to move through its full range without any discomfort, effectively retraining the body's movement patterns in real-time. This active participation distinguishes it from other maitland mulligan kaltenborn techniques.
Core Principles and Application
The magic of Mulligan's approach is the combination of a sustained, corrective glide from the therapist and your own active movement. This "re-tracks" the joint into a more optimal position.
The most important rule is that it must be completely pain-free. If you feel any discomfort, we immediately adjust the technique. The process involves the therapist applying a sustained glide while you move the joint. At the end of your pain-free range, we may add gentle overpressure to improve mobility. This is repeated 6-10 times to reinforce the corrected pattern.
A key component is homework. We often teach "self-MWM" exercises with straps or bands, putting you in control of your recovery, a philosophy that aligns with our Active Release Therapy approach.
For spinal issues, Mulligan developed Natural Apophyseal Glides (NAGs) and Sustained Natural Apophyseal Glides (SNAGs), which apply the same principles to the spine. The immediate feedback is remarkable; restoring pain-free movement on the spot rebuilds confidence in your body.
When is Mulligan's Technique a Good Fit?
Mulligan's approach shines when movement itself is the problem. It is particularly effective for:
- Joint tracking issues: When a joint isn't moving smoothly, like a kneecap that doesn't track correctly, the corrective glide can normalize mechanics almost instantly.
- Pain with specific movements: If you have pain at a certain point when lifting your arm or turning your head, MWM can be transformative.
- Restoring functional movement: Because you are actively moving during treatment, we are retraining the exact patterns you need for daily life or sports.
- Immediate feedback: The pain-free principle provides instant confirmation that we've identified and corrected the issue, which is highly motivating for patients.
The Kaltenborn-Evjenth Concept: A Biomechanical Approach to Traction
If your joint feels "stuck" or hypomobile, the Kaltenborn-Evjenth concept is often the solution. Developed by Norwegian physiotherapists Freddy Kaltenborn and Olaf Evjenth, this approach is distinctly biomechanical, using sustained traction forces to create space and restore joint function.
Unlike the rhythmic oscillations of Maitland or active movements of Mulligan, Kaltenborn's method is rooted in the precise science of how joints move (arthrokinematics). At Evolve Physical Therapy, we find this systematic approach invaluable for stubborn joint restrictions that haven't responded to other treatments.
Core Principles and Traction Grades
The Kaltenborn concept uses translatoric movements—linear gliding, traction, and compression. These are sustained holds, not oscillations, and are graded based on their therapeutic purpose.
- Grade I (Loosen): Applies minimal traction to decompress the joint and relieve pain without separating the joint surfaces. It is ideal for acutely inflamed or irritated joints.
- Grade II (Tighten): Takes up the slack in the joint capsule to the point of tissue resistance. It is used for assessment and maintaining mobility.
- Grade III (Stretch): Applies a sustained stretch to the joint capsule and ligaments to increase mobility and lengthen shortened tissues. This grade is transformative for conditions like frozen shoulder.
This method is guided by the Convex-Concave Rule, a biomechanical principle that dictates the direction of mobilization based on the shape of the joint surfaces. This precision ensures we apply force in the most effective direction. Comparison studies have shown that understanding these mechanics leads to better outcomes. This level of precision is a key part of our Soft Tissue Therapy approach.
When is the Kaltenborn Method Applied?
The Kaltenborn technique is our go-to for mechanically restricted joints. It is ideal for:
- Joint hypomobility (stiffness): Grade III traction and glides systematically stretch the shortened capsule to restore lost motion, as seen in frozen shoulder.
- Pain relief through decompression: Grade I traction gently separates joint surfaces to reduce pressure on nerve endings, which is effective for arthritic or compressed joints.
- Restoring normal joint mechanics: After injury or surgery, this systematic approach corrects compensatory movement patterns and guides the joint back to normal function.
- Tight joint capsules: Sustained Grade III mobilizations provide the necessary low-load, long-duration stretch to improve the extensibility of the tough fibrous tissue surrounding the joint.
Comparing Maitland, Mulligan, and Kaltenborn Techniques
While maitland mulligan kaltenborn techniques are distinct, they are not competing methods. They are different tools in a therapist's toolbox, each designed for a specific purpose. Maitland is like a musician calming the nervous system, Mulligan is a coach retraining pain-free movement, and Kaltenborn is an engineer restoring precise joint mechanics.
Here's how they stack up:
| Feature | Maitland Concept | Mulligan Concept (MWM) | Kaltenborn-Evjenth Concept |
|---|---|---|---|
| Founder | Geoffrey Maitland (Australia) | Brian Mulligan (New Zealand) | Freddy Kaltenborn (Norway) |
| Core Principle | Graded oscillatory movements for pain & stiffness | Pain-free active movement combined with therapist-applied passive mobilization | Graded sustained traction/glides to restore biomechanics |
| Patient Role | Passive | Active (patient performs movement) | Passive |
| Type of Movement | Oscillatory (rhythmic, repetitive) | Active physiological movement with sustained accessory glide | Sustained translatoric traction or glide |
| Primary Goal | Pain modulation, increasing ROM, restoring joint play | Restoring pain-free functional movement | Restoring normal joint mechanics, increasing joint play |
| Theoretical Basis | Neurophysiological (Pain Gate, Descending Inhibition) & Mechanical | Positional fault correction | Biomechanical (Convex-Concave Rule, arthrokinematics) |
Key Differences in Maitland, Mulligan, Kaltenborn Techniques
The fundamental differences lie in their theoretical basis and application.
- Maitland uses a dual approach. Gentle oscillations (Grades I-II) work neurophysiologically to gate pain, while stronger oscillations (Grades III-IV) provide a mechanical stretch to stiff tissues.
- Mulligan is based on correcting minor "positional faults." By holding the joint in a corrected position while the patient actively moves, it retrains the movement pattern to be pain-free.
- Kaltenborn is purely biomechanical. It uses sustained traction and glides, guided by the Convex-Concave Rule, to systematically stretch the joint capsule and restore normal joint play.
The patient experience also differs. Maitland and Kaltenborn are passive treatments, while Mulligan requires active patient participation, which many find empowering.
How Therapists Integrate Maitland, Mulligan, Kaltenborn Techniques
At Evolve Physical Therapy, we don't pick a favorite; we integrate all three approaches based on a thorough assessment. Our clinical reasoning guides us to the right tool for each stage of your recovery.
For example, a patient with a painful shoulder might start with Maitland's gentle oscillations to reduce pain. As pain subsides, we might use Kaltenborn's sustained traction to stretch the tight joint capsule. Finally, to restore pain-free function like reaching overhead, we could apply Mulligan's MWM to correct tracking issues during the active movement.
This integrated approach allows us to address all facets of your problem: pain, mechanical restrictions, and faulty movement patterns. We combine these manual techniques with other interventions like the Graston Technique and targeted exercises to create a comprehensive, flexible plan that adapts to your specific needs.
Frequently Asked Questions about Manual Therapy
It's natural to have questions before starting manual therapy. At Evolve Physical Therapy, we believe understanding the process helps you feel more comfortable and confident.
Does manual therapy hurt?
No, manual therapy should not be painful. You might feel stretching or gentle pressure, but we always work within your comfort zone. Low-grade mobilizations (Maitland Grades I-II, Kaltenborn Grade I) are specifically designed for pain relief. The Mulligan technique's core principle is that all movements must be completely pain-free.
Communication is key. If you feel any sharp or increasing pain, tell us immediately. Your comfort and safety are our top priorities, and we will always adjust our approach.
How do I know which technique is right for me?
You don't have to figure this out alone—that's our job. A skilled physical therapist determines the best approach after a thorough evaluation. At Evolve Physical Therapy, we don't use a one-size-fits-all method. We consider:
- Your symptoms: The nature, triggers, and intensity of your pain.
- Our objective findings: Your range of motion, joint play, and functional movement patterns.
- Your goals: What you want to get back to doing.
- The joint's condition: Whether it's painful, stiff, or has a tracking issue.
Based on this comprehensive picture, we select and adapt the right combination of maitland mulligan kaltenborn techniques for your specific presentation and adjust the plan as you progress.
How many sessions will I need?
Every healing journey is unique, so there's no set number of sessions. The timeline depends on several factors:
- The condition's severity and duration: Acute injuries often respond faster than chronic conditions.
- Your individual response to treatment: Some bodies heal and adapt more quickly than others.
- Your commitment to your home program: Consistently performing your exercises is crucial for faster progress and fewer sessions.
- Underlying causes: Addressing related issues like muscle imbalances or poor posture is key to preventing recurrence.
We continuously reassess your progress and communicate openly about what to expect. Our goal is to empower you with the tools for long-term management, not to create dependency on therapy.
Your Path to Pain-Free Movement in Brooklyn
Understanding maitland mulligan kaltenborn techniques is one thing—experiencing their transformative power in skilled, caring hands is another. At Evolve Physical Therapy + Sports Rehabilitation, we believe in a holistic approach that addresses the root cause of your discomfort, not just the symptoms.
Our therapists are experts in Maitland's oscillations, Mulligan's Mobilization with Movement, and Kaltenborn's traction. More importantly, we know how to integrate these methods into a personalized, hands-on treatment plan that fits your life and goals. We combine these powerful manual therapies with personalized exercises and education to empower you for long-term health.
Whether you're struggling with a frozen shoulder, knee pain, or chronic back stiffness, we're here to help you move forward. Our goal is to give you the tools to take control of your recovery, not create dependency on therapy.
If you're in Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin, you don't have to live with pain or limited movement. Discover our approach to manual physical therapy in Brooklyn and take the first step toward a more active, pain-free life. We're ready when you are.
Senior Strength Secrets: Functional Fitness Exercises You Need
Why Functional Fitness is Essential for Seniors' Independence and Quality of Life

As we age, simple activities like getting up from a chair or carrying groceries can become challenging. The difference between maintaining independence and losing it often comes down to functional strength. Functional fitness seniors programs focus on exercises that mimic these everyday movements, training your body for life, not just for the gym.
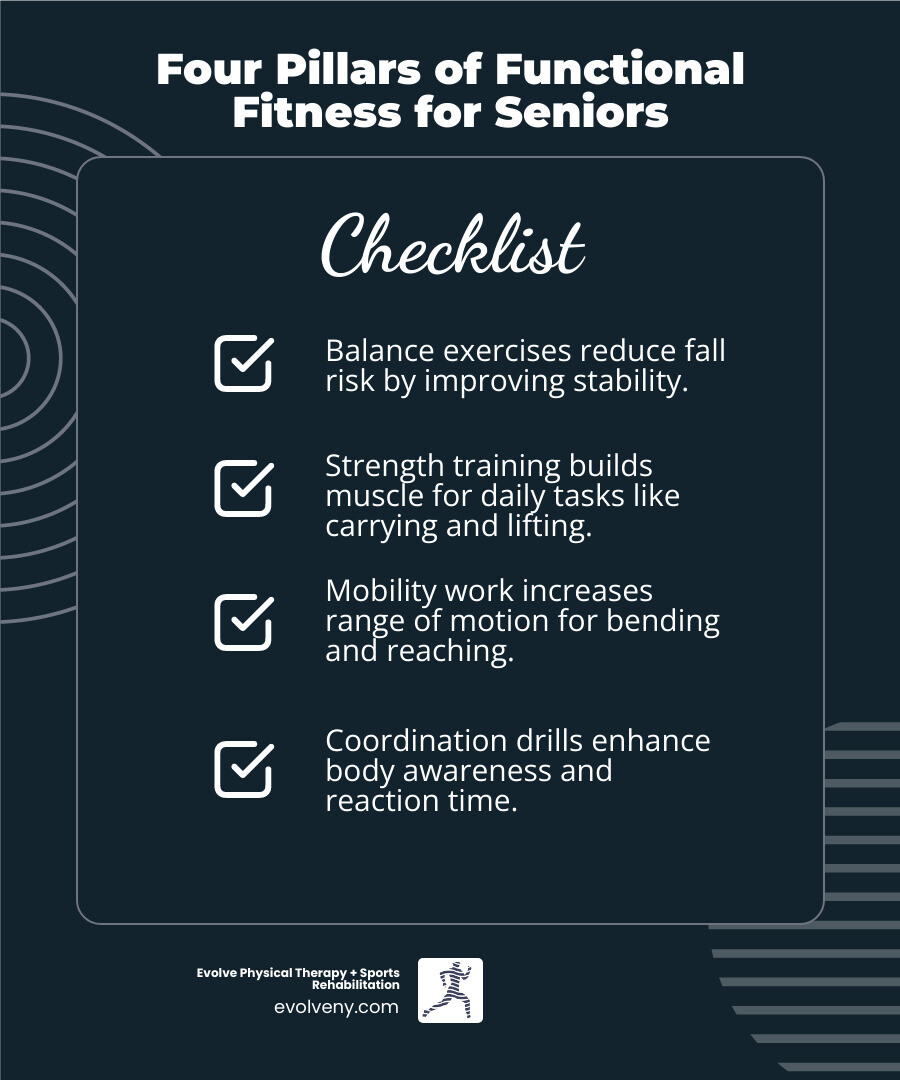
Core Benefits of Functional Fitness for Seniors:
- Improved Balance - Reduces fall risk through stability training
- Increased Strength - Builds muscle for daily tasks like lifting and carrying
- Better Mobility - Improves range of motion for bending and reaching
- Greater Independence - Maintains ability to perform activities of daily living safely
Key Functional Movements to Master:
- Squatting (sitting down and standing up)
- Pushing (opening doors, getting up from the floor)
- Pulling (carrying shopping bags, opening drawers)
- Lifting (picking up objects safely)
- Balancing (walking on uneven surfaces)
More than 25% of adults 65 or older have a fall each year. The good news is that research shows older adults who perform well on functional fitness tests have a significantly lower risk of falling. In as little as eight weeks, functional training can improve physical function and quality of life.
These practical exercises often use just your bodyweight, making them accessible without a gym. Whether you want to prevent falls or keep up with your grandchildren, functional fitness offers a proven path forward.
I'm Lou Ezrick, founder of Evolve Physical Therapy. I've spent nearly two decades helping older adults regain strength and confidence. My work with functional fitness seniors programs has shown me how the right exercises can transform someone's ability to live independently and pain-free.
What is Functional Fitness and Why is it a Game-Changer for Seniors?
Functional fitness is exercise that prepares you for real life. Unlike traditional workouts that isolate one muscle (like a bicep curl), functional fitness trains muscles to work together as a team, mirroring how your body moves every day.
When you lift a bag of groceries, you use your arms, core, back, and legs. That's functional movement. For seniors, this approach is a game-changer. Functional fitness seniors programs strengthen the exact movement patterns you use most—sitting, standing, climbing stairs, and reaching. By training these real-world movements, you directly improve your ability to live independently and safely.
These exercises also improve the coordination between your brain and muscles, which helps you catch yourself if you stumble. This makes functional fitness highly effective for injury prevention. The CDC emphasizes that these exercises help seniors maintain independence by reducing fall risk and improving overall quality of life.
Here's how functional fitness stacks up against traditional exercise:
| Feature | Functional Fitness | Traditional Exercise |
|---|---|---|
| Movement Focus | Compound movements, multi-joint, whole-body | Isolated muscle groups, single-joint |
| Goal | Improve daily activities, prevent injury, independence | Build muscle mass, strength, aesthetics |
| Equipment | Bodyweight, resistance bands, light weights, household items | Machines, heavy free weights |
| Real-World Relevance | High (mimics daily tasks like lifting, squatting) | Lower (may not directly translate to daily tasks) |
| Balance & Coordination | Integral part of training | Often secondary or separate |
Unfortunately, adults over 60 are the least active age group, which contributes to a decline in the very abilities functional fitness preserves. The encouraging news is that it's never too late to start, and the results can be remarkable. Our Physical Therapy for Seniors programs prioritize this approach because we've seen how it transforms people's confidence and safety.
7 Essential Functional Fitness Exercises for Seniors
Here are seven essential exercises that mirror daily activities to help you move with greater ease and confidence. Proper form is crucial, so if you have any health concerns, consult a professional first. Our Therapeutic Exercise Brooklyn services can provide personalized guidance. Most of these movements require only your bodyweight and a sturdy chair.

1. Sit-to-Stand (Chair Squat)
This is arguably the most important exercise for maintaining independence, building the strength needed to get out of chairs, beds, and cars.

Daily task it mimics: Getting in and out of a chair, sofa, or car.
Muscles worked: Glutes, quadriceps, hamstrings, and core.
Sit on the edge of a sturdy chair, feet hip-width apart. Lean your chest slightly forward with a straight back, then push through your heels to stand up without using your hands. Squeeze your glutes at the top. Slowly lower yourself back down with control. Aim for 10-15 repetitions for 2-3 sets. If needed, use your hands for assistance and gradually reduce reliance on them. This exercise is a key part of clinical assessments like the 30-second sit-to-stand test.
2. Step-Ups
Navigating stairs and curbs safely is crucial for independence. This exercise builds the necessary leg strength and balance.

Daily task it mimics: Climbing stairs, stepping over curbs, and getting into vehicles.
Muscles worked: Quadriceps, hamstrings, glutes, and calves.
Use a sturdy, low step or platform. Place one entire foot on the step, then push through that heel to bring your other foot up. Stand tall at the top. Step back down with the first foot, then the second. Alternate leading legs or complete all reps on one side before switching. Aim for 10-12 repetitions per leg for 2-3 sets. Keep a wall or chair nearby for balance. This is a cornerstone of our Physical Therapy for Muscle Weakness programs.
3. Wall Push-Ups
This is a gentle, accessible way to build the upper body strength needed for daily pushing movements.

Daily task it mimics: Pushing open heavy doors or bracing yourself from a stumble.
Muscles worked: Chest, shoulders, triceps, and core.
Stand facing a wall, about an arm's length away. Place your hands on the wall slightly wider than your shoulders. Keeping your body in a straight line, bend your elbows to lower your chest toward the wall. Push back to the starting position. To make it easier, move your feet closer to the wall; for more challenge, step further back. Complete 10-15 repetitions for 2-3 sets. See a visual guide on how to do a wall push-up.
4. Farmer's Walk
This practical exercise mimics carrying heavy items like groceries or luggage, building full-body strength and stability.

Daily task it mimics: Carrying groceries, luggage, or a laundry basket.
Muscles worked: Grip, forearms, shoulders, upper back, core, and glutes.
Hold a light weight (dumbbell, kettlebell, or water bottle) in each hand. Stand tall with shoulders back, chest up, and core engaged. Walk slowly for a set distance (20-30 feet) or time (30-60 seconds), maintaining perfect posture. Rest and repeat for 2-3 rounds. Start with very light weights. This exercise is a great addition to any Strengthening Program Brooklyn.
5. Heel-to-Toe Walk
This exercise specifically targets the coordination and stability needed to walk confidently and stay steady on your feet.
Daily task it mimics: Walking in a straight line and maintaining balance on narrow or uneven surfaces.
Muscles worked: Core, ankles, and small leg stabilizing muscles.
Stand tall and place the heel of one foot directly in front of the toes of the other, as if on a tightrope. Focus on a point ahead of you for balance. Slowly walk forward, taking 10-20 steps. Turn around and repeat. Complete 2-3 sets. Perform this next to a wall or countertop for support if needed. This is a core component of Balance and Gait Training for fall prevention.
6. Bicep Curls
This simple exercise strengthens your arms for all the daily lifting and carrying tasks we often take for granted.
Daily task it mimics: Lifting a gallon of milk, a pot from the stove, or a grandchild.
Muscles worked: Biceps and forearms (grip strength).
Sit or stand holding a light weight (dumbbell, resistance band, or soup can) in each hand, palms facing forward. Keeping your elbows close to your sides, slowly curl the weights toward your shoulders. Squeeze your biceps, then slowly lower the weights back down. Avoid using momentum. Complete 10-15 repetitions for 2-3 sets. You can find suitable Exercise Equipment on our site, but household items work well too.
7. Glute Bridge
This exercise strengthens your glutes and hamstrings, which are crucial for good posture, pelvic stability, and reducing lower back strain.
Daily task it mimics: Getting out of bed, standing up straight, and stabilizing your body while walking.
Muscles worked: Glutes, hamstrings, and lower back.
Lie on your back with knees bent and feet flat on the floor, hip-width apart. Squeeze your glutes and lift your hips until your body forms a straight line from shoulders to knees. Hold for a second, then slowly lower back down. Aim for 10-15 repetitions for 2-3 sets. Focus on using your glutes, not your lower back. This is also excellent for knee stability. Learn more about How to Strengthen Knees if knee health is a concern.
Creating Your Safe and Effective Functional Fitness Seniors Routine
Building a functional fitness seniors routine is about creating sustainable habits. The goal is consistency, not intensity.
- Start Slowly: If you're new to exercise, begin with fewer repetitions (e.g., 5 instead of 10) and focus on proper form. Your body needs time to adapt.
- Be Consistent: Gentle, regular movement is more effective than sporadic, intense workouts. Aim for even 10-15 minutes a day.
- Listen to Your Body: Mild muscle soreness is normal, but sharp pain is a signal to stop. Modify exercises or take a rest day when needed.
- Warm-Up and Cool-Down: Always start with 5-10 minutes of light cardio (marching in place, arm circles) and end with 5-10 minutes of gentle stretching, holding each stretch for 20-30 seconds.
For more on the power of regular movement, read our article Get Movin: The Undeniable Benefits of Exercise. The CDC also provides a great guide, Growing Stronger - Strength Training for Older Adults.
Equipment for Senior Functional Fitness
You don't need a gym. Most of what you need is already in your home.
- Bodyweight: Your most valuable tool for exercises like sit-to-stands and wall push-ups.
- Resistance Bands: Inexpensive, space-saving, and gentle on joints.
- Light Dumbbells: Start with 1-3 pounds for curls and walks.
- Sturdy Chair: Essential for sit-to-stands and balance support.
- Household Items: Soup cans or water bottles work perfectly as light weights.
If you wish to invest, we have a selection of senior-friendly Fitness Equipment.
Modifications for Pre-existing Conditions in functional fitness seniors
Safety comes first. Always talk to your doctor or physical therapist before starting a new exercise program. They can help you modify exercises for your specific needs.
- Arthritis: Move through a comfortable range of motion without forcing it. For example, do partial squats or use a higher step for step-ups. Our Osteoarthritis Physical Therapy Brooklyn program can help.
- Osteoporosis: Avoid heavy twisting or forward bending. Focus on safe, weight-bearing movements like wall push-ups. Professional guidance is key, which our Osteoporosis Physical Therapy Brooklyn services provide.
- Heart Conditions: Start with low intensity and build up gradually. Stop immediately if you feel chest pain, dizziness, or unusual shortness of breath.
- Balance Concerns: Always exercise near a sturdy support like a wall or counter. Prioritize stability over speed.
The Critical Role of Functional Fitness in Fall Prevention
The fear of falling keeps many seniors from living fully. With over 25% of adults 65 or older falling each year, prevention is critical. The good news is that a significant number of these falls are preventable.
Research shows that older adults who perform well on functional fitness tests have a dramatically lower risk of falling. Functional fitness seniors programs are designed to strengthen your body's natural fall-prevention system.
Strength is your foundation. Strong leg, hip, and core muscles provide a stable base, giving you the power to react quickly and catch yourself if you stumble. Exercises like sit-to-stands and step-ups build this essential power.
Balance training is your early warning system. Exercises like the heel-to-toe walk improve your body's awareness in space (proprioception). This helps you make constant, tiny adjustments to stay upright and sure-footed. Our Physical Therapy for Fall Prevention Brooklyn programs focus heavily on this.
Faster reactions save you from injury. Dynamic functional exercises train your body to respond faster when you lose your balance. That split-second reaction can be the difference between a close call and a hospital visit.
Perhaps most importantly, functional fitness builds confidence. When you trust your body's strength and stability, the fear of falling loses its grip. This allows you to stay active and engaged, breaking the cycle of inactivity that ironically increases fall risk. Our specialized Elderly Balance Training programs are built to give you the physical resilience and mental confidence to live freely and safely.
Frequently Asked Questions about Functional Fitness for Seniors
Here are answers to some of the most common questions I hear from older adults.
How often should a senior do functional fitness exercises?
The ideal frequency is 3-5 times per week. This allows for muscle recovery while providing enough consistency to build strength and balance. You don't need long sessions; even 10-15 minutes of focused movement daily can make a huge difference. Consistency is far more important than intensity.
Can functional fitness help with arthritis pain?
Yes. While it seems counterintuitive, the right kind of movement is medicine for arthritis. Strengthening the muscles around a painful joint provides a natural support system, taking pressure off the joint itself and often reducing pain. The key is to use modified, gentle, and controlled movements within a comfortable range of motion. Our Osteoarthritis Physical Therapy Brooklyn program is designed to help you move better with less pain.
Is it ever too late to start functional fitness?
It is never too late. The human body retains a remarkable ability to adapt and get stronger at any age. I've worked with clients in their 80s and 90s who have made incredible improvements in their strength, balance, and independence. You may not become an Olympic athlete, but you can absolutely build enough functional strength to carry your own groceries, play with your grandchildren, and walk confidently without fear. The secret is to start where you are today and build gradually. Your age is a starting point, not a barrier.
Conclusion
The seven exercises you've just learned are more than a workout plan; they are practical tools to prepare your body for real life. This is the core of what makes functional fitness seniors programs so effective. The benefits—improved balance, increased strength, better mobility, and a reduced risk of falls—translate directly to a more independent and confident life.
It's never too late to feel stronger and more stable. At Evolve Physical Therapy, we understand that generic programs don't work for everyone. We take a hands-on approach, creating personalized plans that address your specific needs and goals. We work alongside you, adapting your program as you grow stronger.
The path to a more independent life starts with a single step. You've already taken the first one by learning about these exercises. Now, take the next one.
High Performance Coaching: Turning Good Athletes into Great Ones
Why Coaching for Sports Performance is the Key to Open uping Athletic Potential

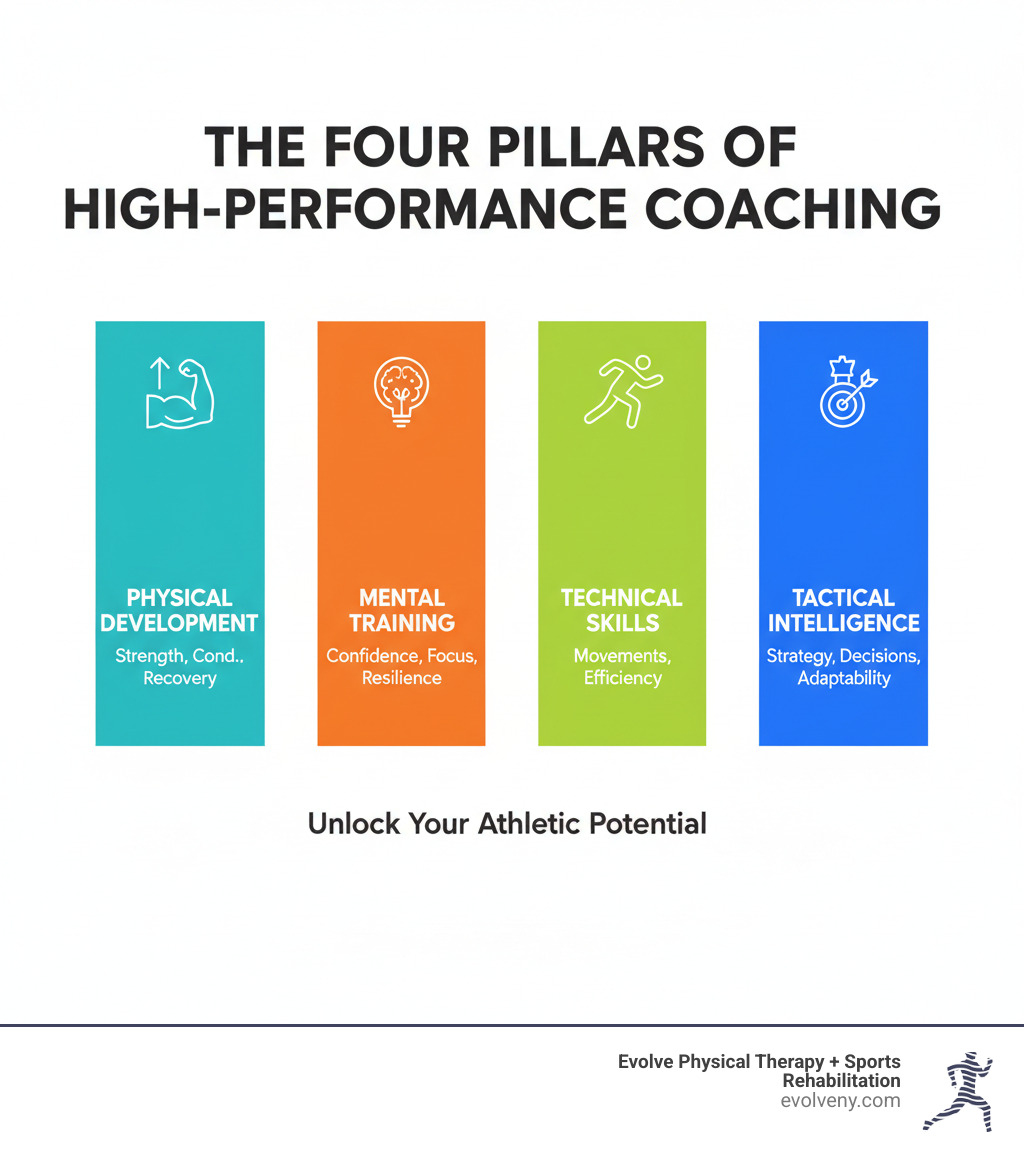
Coaching for sports performance is a comprehensive, science-backed approach that transforms athletic ability by integrating physical training, mental preparation, tactical understanding, and technical skill development. Unlike traditional coaching that focuses solely on drills and game strategy, high-performance coaching addresses every factor that influences an athlete's ability to compete at their best.
Core Elements of Effective Performance Coaching:
- Physical Development - Strength, speed, agility, conditioning, and recovery protocols
- Mental Training - Visualization, goal setting, confidence building, and stress management
- Technical Mastery - Sport-specific skill refinement and movement optimization
- Tactical Intelligence - Strategic thinking, decision-making under pressure, and game awareness
- Holistic Well-Being - Injury prevention, nutrition guidance, and work-life balance
The modern coaching landscape demands more than just physical fitness. Research shows that as much as 90% of sport is mental, yet most athletes spend the majority of their time training only their bodies. The most successful coaches understand that developing a great athlete requires addressing the whole person—not just their physical capabilities.
What separates good athletes from great ones? It's rarely raw talent alone. The difference lies in having a coach who understands how to build a comprehensive development program that addresses physical limitations, mental barriers, technical flaws, and tactical gaps. This holistic approach is what transforms potential into consistent, peak performance.
Studies from elite endurance sports show that world-class coaches share key characteristics: they collect training data systematically, exhibit an experimental mindset when making adjustments, and prioritize training quality over simply logging hours. They understand that effective coaching requires balancing training load with recovery, optimizing key workout sessions, and ensuring athletes peak at the right moments.
The evidence is clear: athletes in positive sport environments—where holistic well-being is supported—achieve better performance outcomes, greater satisfaction, improved resilience, and longer careers in their sport. Even when medals are won in negative environments, research shows athletes specifically note that the performance wasn't worth the cost to their mental and physical health.
I'm Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, and over nearly two decades I've worked with athletes ranging from weekend warriors to elite competitors, helping them overcome physical limitations that hold back their performance. My experience in coaching for sports performance has shown me that the most successful athletic development happens when physical therapy, strength conditioning, and mental training work together as an integrated system.
The Modern Coaching Philosophy: Beyond Wins and Losses
Here's something I've learned after nearly two decades working with athletes: the coaches who produce the most consistent results aren't always the ones with the most trophies on their shelf. They're the ones who understand that coaching for sports performance means caring about the whole person, not just the person who shows up on game day.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen what happens when coaches prioritize wins at the expense of everything else. Athletes burn out. They develop injuries that could have been prevented. They walk away from sports they once loved. The research backs this up—negative training environments might occasionally produce medals, but athletes who experience them consistently say the medal wasn't worth what they sacrificed to get it.
The flip side is just as powerful. When athletes train in positive environments that support their holistic well-being, they don't just perform better—they enjoy training more, bounce back from setbacks faster, and stay in their sport longer. They build resilience that serves them long after their competitive days are over.
Developing Your Coaching Philosophy
Think of your coaching philosophy as your North Star. When you're facing a tough decision—whether to push an injured athlete to compete, how to handle a conflict between team members, or what to prioritize during a crucial training phase—your philosophy is what guides you back to what matters most.
Every effective coach needs to start with self-awareness. What are your core values? What kind of leader are you naturally, and where do you need to grow? Understanding your own strengths and blind spots isn't just helpful—it's essential if you want to build genuine trust with your athletes.
Next comes the hard part: defining success beyond the scoreboard. Yes, winning matters. But is that all that matters? What about an athlete who finally masters a skill they've been struggling with for months? Or a team that learns to communicate better under pressure? These victories might not show up in the standings, but they're often the foundation that future championships are built on.
Your ethical framework needs to be crystal clear and non-negotiable. At Evolve, we believe being called "Coach" is an honor that comes with serious responsibility. That means operating with fairness, respect, and integrity in every interaction. It means putting athlete safety first, even when it's inconvenient. It means being professional, staying current with best practices, and never abusing the trust that athletes place in you.
Finally, effective coaching for sports performance requires thinking about long-term athlete development. The decisions you make today will impact your athletes for years—maybe decades—to come. Are you helping them build a lifelong love of movement and competition? Or are you creating patterns that lead to burnout and injury?
The role of coach education in philosophy development is crucial here. Good coach education programs don't just teach you drills and tactics—they help you articulate your beliefs and translate them into consistent, effective action.
Creating a Safe and Empowering Sport Environment
A safe sport environment isn't just about locking the equipment closet and having a first aid kit handy. Though environmental safety certainly matters—proper equipment maintenance, hazard-free training spaces, and solid emergency protocols are all essential—true safety goes much deeper.
Relational safety is where the real magic happens. This means creating a culture where athletes feel comfortable speaking up, asking questions, and admitting when they're struggling. It means zero tolerance for harassment, abuse, or discrimination of any kind. It means building trust through consistent, respectful communication between coaches, athletes, and support staff.
When we talk about optimizing sport, we're talking about designing training and competition schedules that promote healthy development rather than grinding athletes into the ground. It's about balancing intensity with recovery, challenge with support, and performance goals with the simple enjoyment of playing.
At Evolve, we advocate for the HIGHER method as a framework for creating environments where athletes truly thrive. This approach emphasizes being Holistic in addressing the whole athlete—physical, mental, emotional, and social needs all matter. It requires Individualized coaching that recognizes each athlete's unique circumstances and goals. Good Governance means upholding ethical standards and making decisions transparently. Being Healthy means prioritizing physical and mental health above all else, even when it costs you a win. Empowering athletes to make decisions, develop leadership skills, and take ownership of their development creates more resilient competitors. And treating everyone with Respect—valuing diverse backgrounds and perspectives—builds stronger, more cohesive teams.
This isn't soft coaching. It's smart coaching. Athletes who feel safe, valued, and empowered consistently outperform those who are motivated primarily by fear or pressure.
Measuring Success Holistically
If you're only measuring success by what shows up on the scoreboard, you're missing most of the story.
Don't get me wrong—competitive outcomes matter. We work with athletes because they want to perform at their best when it counts. But the most successful coaches I know also track personal metrics that matter to individual athletes. Did they shave two seconds off their personal best? Finally nail that technique they've been working on? Execute under pressure in a way they couldn't before?
Personal development often provides the most meaningful measures of coaching effectiveness. Has your athlete become more resilient? Can they regulate their emotions better when things get tough? Are they developing leadership skills that will serve them long after their playing days are over? These aren't just nice-to-haves—they're the qualities that separate athletes who peak early from those who sustain excellence over time.
Athlete satisfaction is another crucial metric that too many coaches ignore. How much do your athletes enjoy their sport experience? Do they feel supported? Do they trust your approach? Enjoyment isn't just a feel-good factor—it's one of the most powerful motivators for sustained effort and improvement.
The desire to stay in sport tells you volumes about the environment you've created. Athletes who love what they do and feel supported in doing it don't burn out at 22. They don't develop negative associations with training. They stick around, and that longevity gives them time to reach their full potential.
Resilience—the ability to bounce back from injuries, losses, and disappointments—is perhaps the most valuable quality you can help an athlete develop. This mental toughness doesn't come from being broken down and built back up. It comes from being supported through challenges in an environment where it's safe to struggle and grow.
Finally, performance satisfaction means helping athletes find fulfillment in their effort and progress, regardless of whether they won or lost. When athletes can walk away from a competition feeling proud of how they competed—even in defeat—you've given them something more valuable than any medal: a healthy, sustainable relationship with their sport.
The Science Behind Peak Athletic Performance
Think of athletic performance like a complex machine—every part needs to work in perfect harmony. The best coaching for sports performance isn't based on guesswork or outdated methods. It's grounded in understanding how the human body actually moves, adapts, and grows stronger.
At Evolve Physical Therapy + Sports Rehabilitation, we've seen how applying scientific principles transforms athletic potential into real results. When you understand biomechanics (how the body moves), physiology (how systems respond to training), periodization (smart planning of training cycles), and training load management (balancing stress and recovery), you can help athletes reach levels they never thought possible.

The Four Pillars of Athletic Development
Building an elite athlete requires more than just showing up and working hard. You need a well-rounded physical foundation that addresses every aspect of performance. We focus on four essential pillars that work together to create complete athletes.
Strength training forms the foundation, but it's not about mindlessly lifting heavy weights. It's about building functional strength that directly translates to your sport. A basketball player needs explosive power for vertical jumps. A runner needs efficient stride mechanics. A tennis player requires rotational strength for powerful serves.
Compound lifts like squats, deadlifts, bench press, and overhead press build overall strength and coordination. Olympic lifts—the snatch and clean & jerk—develop explosive power that transfers beautifully to athletic movements. Accessory exercises target specific muscle groups, creating balance and preventing injuries before they happen.
One often-overlooked tool is isokinetic training. These are controlled, speed-specific movements that strengthen muscles through their full range of motion at consistent speeds. Research shows that in just eight weeks, isokinetic training can reduce pain and improve mobility and strength, even for individuals with knee osteoarthritis. For athletes, it's incredibly effective for both rehabilitation and performance improvement.
Cardiovascular conditioning keeps athletes performing at their best from the first whistle to the last. Your heart and lungs are muscles too, and they need training. Aerobic training—think long runs, cycling, swimming, or rowing at a steady pace—builds your endurance base. This is where world-class coaches spend 80-90% of their aerobic training time, in low-intensity zones.
But you also need anaerobic capacity for those explosive moments when the game is on the line. Interval training, tempo runs, and Fartlek workouts train your body to perform when it's running on fumes. Elite coaches typically include 2-3 intensive training days per week, carefully balanced with lower-intensity work.
Speed and agility separate good athletes from great ones. Sports rarely happen in straight lines at predictable speeds. You need to accelerate quickly, change direction on a dime, and maintain control through complex movements. Sprint work develops raw speed. Agility drills—cone drills, ladder work, shuttle runs—train your nervous system to react instantly. These aren't just physical exercises; they're teaching your brain and body to communicate faster.
Plyometric training adds the explosive power that makes athletes look superhuman. Box jumps, depth jumps, and bounds for the lower body. Plyometric push-ups and medicine ball throws for the upper body. These exercises train the stretch-shortening cycle, where muscles rapidly stretch and then contract, generating maximum power. It's how athletes jump higher, throw farther, and move faster.
The magic happens when these four pillars are integrated into a periodized training plan that evolves with each athlete's needs and competition schedule. Great coaches understand that training isn't random—it follows a logical progression from general conditioning to sport-specific preparation, gradually increasing volume before ramping up intensity.
Fueling and Recovery for Optimal Output
Here's a truth that surprises many athletes: you don't get stronger during training. You get stronger during recovery. Training breaks your body down. Recovery builds it back up—stronger, faster, more resilient.
Think of your body like a high-performance vehicle. You wouldn't put cheap gas in a race car and expect it to win, right? Essential sports nutrition provides the fuel your body needs. Carbohydrates give you energy for training and competition. Protein repairs and builds muscle tissue. Healthy fats support hormone production and overall health. Vitamins and minerals enable countless processes that keep you performing optimally.
Timing matters as much as what you eat. The meal before training prepares your body. The snack during competition maintains energy levels. The food after exercise starts the recovery process. As coaches, we guide athletes through these choices, helping them understand how nutrition directly impacts their performance.
Hydration is equally critical. Water enables every function in your body—transporting nutrients, regulating temperature, lubricating joints. Even mild dehydration significantly impairs performance. Athletes need personalized hydration plans, especially during intense training or competition in hot conditions. Thirst isn't a reliable indicator, so coaches help athletes develop consistent hydration habits.
Now let's talk about recovery, which is an active process, not just lying on the couch (though rest has its place). Your body adapts to training stress during recovery periods. Muscles repair. Energy stores replenish. Neural pathways strengthen. Skip recovery, and you're just accumulating damage without reaping the benefits.
Active recovery—light exercise that promotes blood flow—helps clear metabolic waste and reduces muscle soreness. Stretching and foam rolling improve flexibility and release muscle tightness. Massage and manual therapy address imbalances and accelerate healing. At Evolve, we integrate these recovery modalities into comprehensive training programs because we've seen how dramatically they improve outcomes.
Sleep might be the most powerful performance improver available, and it's completely legal. During deep sleep, your body releases growth hormone, repairs damaged tissues, consolidates memories, and resets your nervous system. Athletes who prioritize 8-9 hours of quality sleep consistently outperform those who don't. We educate athletes on sleep hygiene—consistent bedtimes, dark rooms, limiting screens before bed—because the science is undeniable.
Finally, preventing overtraining requires constant vigilance. Elite coaches monitor training load carefully, combining subjective feedback from athletes with objective data like heart rate variability and performance metrics. They understand that more training isn't always better. Most implement recovery weeks every 3rd or 4th week, reducing training volume by 25-35% to allow full adaptation and prevent injury or illness.
The science behind peak athletic performance isn't complicated, but it does require discipline and attention to detail. When you respect how the body actually works—building it up systematically, fueling it properly, and giving it adequate recovery—you create athletes who don't just perform well once, but sustain excellence over entire careers.
Mastering the Game: Advanced Coaching for Sports Performance
The world of coaching for sports performance has transformed dramatically in recent years. Today's coaches need to be adaptable leaders who can seamlessly blend different approaches, leverage technology effectively, and tailor their methods to each athlete's unique needs. It's no longer enough to simply know the sport—great coaches understand how to read situations, adjust their leadership style, and use data to make smarter decisions.

Choosing and Blending Your Coaching Style
There's a common misconception that great coaches need to pick one style and stick with it. The truth? The most effective coaches know how to blend multiple approaches based on what their athletes need in any given moment. Back in the 1930s, psychologist Kurt Lewin identified three fundamental leadership styles that still influence coaching today, but modern sports psychology has expanded our understanding considerably.
Think about it this way: an autocratic style (where the coach makes all decisions and expects athletes to follow instructions) might work perfectly when teaching complex techniques to beginners or during high-pressure game situations where quick decisions are critical. But that same approach can backfire with experienced athletes who need autonomy to develop their decision-making skills. Research on coaching leadership styles shows that matching your style to the situation dramatically improves outcomes.
A democratic style involves athletes in decision-making, fostering ownership and motivation. This approach builds confidence and leadership skills, making it ideal for team settings where buy-in matters. Meanwhile, a holistic style considers the whole person—their physical health, mental state, academic pressures, family life, and personal goals. At Evolve Physical Therapy + Sports Rehabilitation, this is the foundation of everything we do. We don't just treat injuries or improve performance; we understand that an athlete dealing with stress at school or recovering from a setback needs support that goes beyond physical training.
The laissez-faire style gives athletes maximum freedom to make their own decisions, with the coach serving more as a resource than a director. This works beautifully with highly self-motivated, experienced athletes who thrive with independence, but it can leave less mature or confident athletes feeling lost.
Here's what this looks like in practice: a youth soccer coach might use an autocratic approach when teaching proper heading technique (safety first), switch to a democratic style when discussing team formations (building ownership), and adopt a holistic approach when an athlete is struggling with confidence issues off the field. Game-based coaching—where athletes learn through modified games rather than isolated drills—naturally encourages a more democratic, athlete-centered approach that develops tactical intelligence alongside technical skills.
The key insight? There's no single "best" coaching style. The most successful coaches develop a toolbox of approaches and know exactly when to use each one.
Adapting Your Coaching for Sports Performance: Situational Leadership
Situational leadership is where coaching becomes an art form. It's about reading the room—or in this case, the athlete—and adjusting your approach accordingly. A strategy that works perfectly for a professional athlete preparing for competition might completely overwhelm a 10-year-old just learning to love the sport.
Age and developmental stage dramatically influence how you should coach. Youth athletes need coaches who prioritize fun, fundamental skill development, and building a lifelong love of movement. They respond well to encouragement, variety, and game-like activities. Collegiate athletes are typically more focused on performance, capable of handling increased training loads, and developing their competitive identity. Professional athletes require sophisticated programming, data-driven adjustments, and often benefit from greater autonomy in their training decisions.
Skill level matters just as much as age. A beginner needs clear, direct instruction and close supervision. They're building foundational movement patterns and learning the basics of the sport. An intermediate athlete can handle more complexity, benefit from tactical discussions, and start taking ownership of certain training decisions. Advanced athletes often need a coach who acts more as a collaborator, someone who provides expert guidance while respecting the athlete's deep knowledge of their own body and performance.
Context shapes everything. The same athlete might need different coaching approaches during pre-season conditioning (building base fitness, perhaps more structured and directive), in-season competition (balancing performance with recovery, more collaborative), and post-season recovery (focusing on healing and reflection, more supportive and holistic).
Individual needs are perhaps the most important consideration. Some athletes are naturally self-motivated and thrive with independence. Others need more structure and external accountability. Some respond well to direct feedback; others need a gentler approach. Great coaches learn to read these individual differences and adjust accordingly, even within the same team or training group.
The Comprehensive Role of an Athletic Performance Coach
The role of an athletic performance coach extends far beyond just running practices or designing workouts. It's a multifaceted position that requires expertise across several domains, and understanding these distinctions helps athletes find the right support for their goals.
An athletic performance coach differs significantly from a strength coach or personal trainer. While a strength coach focuses primarily on physical conditioning and gym-based training, and a personal trainer typically works on general fitness goals, an athletic performance coach takes a comprehensive approach to sport-specific development. We integrate physical training with technical skill work, tactical understanding, mental preparation, and overall athlete development. At Evolve, this means addressing not just how strong an athlete is, but how that strength translates to their specific sport, how they're recovering, and what might be holding them back mentally or physically.
The modern performance coach also needs a working knowledge of sport management basics—understanding scheduling, program organization, budgeting for equipment and travel, and coordinating with other support staff. You're often the hub connecting athletes, parents, athletic trainers, physical therapists, nutritionists, and sport psychologists.
Media relations have become increasingly important, especially for coaches working with high-level athletes. Knowing how to communicate about your program professionally, protect athlete privacy, and handle public attention is now part of the job description.
Perhaps the biggest evolution in coaching has been the integration of technology for analysis and performance tracking. GPS tracking systems monitor training load and movement patterns. Video analysis software breaks down technique frame by frame. Wearable devices track heart rate variability, sleep quality, and recovery metrics. Force plates measure power output and asymmetries. The challenge isn't accessing this technology—it's knowing how to interpret the data and translate it into actionable coaching decisions.
World-class coaches in endurance sports, for example, systematically collect training data and exhibit an experimental mindset, constantly testing and refining their approach based on objective feedback. They don't just follow a program blindly; they adapt based on what the data and athlete feedback are telling them.
This comprehensive approach to coaching for sports performance is what separates good programs from truly transformative ones. It's about seeing the whole picture, understanding how all the pieces fit together, and having the knowledge and tools to optimize every aspect of an athlete's development.
The Musician's Guide to Healthy Hands and Injury Prevention
Why Musicians' Hands Need Specialized Care
Hand therapy for musicians is a specialized field addressing the unique musculoskeletal demands on performers. It's essential because the repetitive, high-stakes nature of playing an instrument creates extraordinary pressure on nerves and muscles. Standard treatments often fall short for musicians, whose hands are their livelihood.
This specialized care includes instrument-specific rehabilitation, modified return-to-play schedules, neuromuscular reeducation to optimize technique, comprehensive assessments of posture and practice habits, and targeted prevention strategies. The goal is to address the root cause of pain, not just the symptoms.
Many musicians feel a deep connection to their instrument, but hours of daily practice in sustained or awkward positions take a toll. The statistics are sobering: studies show that over 90% of musicians in some groups report play-related pain. These playing-related musculoskeletal disorders (PRMDs) can devastate your physical health, mental well-being, and career.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. For nearly two decades, I've helped musicians recover from complex conditions. Our specialized hand therapy for musicians focuses on restoring the precise motor control and endurance your craft demands, getting you back to playing safely by addressing the root causes of dysfunction.
Understanding Playing-Related Musculoskeletal Disorders (PRMDs)
Playing-related musculoskeletal disorders (PRMDs) are injuries that develop when the body is pushed beyond its limits by the repetitive, intense movements of playing an instrument. These aren't minor aches; PRMDs can derail your career and affect your physical, mental, and financial health. The symptoms often start subtly with pain or fatigue during practice but can escalate to swelling, numbness, or persistent pain affecting the hands, wrists, arms, shoulders, and neck.
Tendinitis and tendinopathy are common overuse injuries. Tendinitis is tendon inflammation, which can progress to tendinopathy—a degeneration of the tendon tissue itself—if not addressed early.
Carpal tunnel syndrome (CTS) occurs when the median nerve in the wrist is compressed, causing numbness, tingling, and weakness in the thumb, index, and middle fingers. Physical therapy is highly effective for mild to moderate CTS, offering improvements comparable to surgery without the risks.
Cubital tunnel syndrome involves compression of the ulnar nerve (the "funny bone" nerve) at the elbow, causing numbness and tingling in the ring and pinky fingers. Instruments requiring prolonged elbow flexion can worsen this condition.
Thoracic outlet syndrome (TOS) happens when nerves and blood vessels between the collarbone and first rib are squeezed, often due to forward head posture common in violinists or keyboardists. Symptoms include pain, numbness, and a heavy feeling in the arm and hand.
Osteoarthritis (OA) can develop in the joints of the hands, wrists, and shoulders from years of cumulative stress. X-ray findings don't always correlate with pain levels.
What is Focal Hand Dystonia?
Among the most devastating conditions is Focal hand dystonia (FHD), or musician's cramp. This is a task-specific neurological movement disorder causing an involuntary loss of finger coordination, but only when playing your instrument. Fingers may cramp, flex, or extend on their own, making precise playing impossible. It is generally painless, which makes it particularly insidious.
FHD is believed to result from use-dependent changes in the brain's sensory cortex—the brain's "map" for the fingers becomes disorganized. Years of intense, repetitive practice contribute to this maladaptive plasticity. While there is no single cure, specialized hand therapy for musicians offers effective management. A promising behavioral treatment is Sensory Motor Retuning (SMR), which involves retraining the dystonic finger by immobilizing others with a splint to perform focused exercises. This and other approaches like sensory discrimination training aim to re-establish normal motor control by essentially retraining the brain to correctly map and control the fingers again. It's a challenging journey, but many musicians successfully manage their symptoms and return to playing.
The Role of Specialized Hand Therapy for Musicians
Your hands are finely tuned instruments, capable of precision and speed that require specialized care. General physical therapy, while valuable, often falls short for musicians. Standard advice like complete rest can be devastating, leading to loss of technique, income, and psychological distress. Our goal isn't just pain reduction; it's achieving full "musical fitness"—the stamina, coordination, and sensory feedback needed for peak performance.
At Evolve Physical Therapy in Brooklyn, our specialized approach begins with a thorough initial assessment. We look at you as a whole musician, analyzing your posture and movement while you play your instrument. We review the specific demands of your instrument, your practice and performance schedule, and broader lifestyle factors like sleep and stress. Your personal musical goals guide every decision, allowing us to create a truly personalized treatment plan.
Your program will be built on several key components. We design individualized home exercise programs to address your specific muscle imbalances and nerve issues, custom to the movements your instrument requires. Our therapists use hands-on manual therapy to reduce pain, improve joint mobility, and release tight tissues. Neuromuscular reeducation is crucial for retraining your body's awareness and control, refining your technique for pain-free efficiency. We also use pain reduction modalities and sensory reeducation to restore the fine tactile feedback that is paramount to your craft.
Crucially, we practice instrument-focused rehabilitation, bringing your instrument into the therapy room. This makes therapy functional and directly relevant to your goals. We develop modified playing schedules to ease you back into playing without re-injury, gradually increasing duration and difficulty. We use your instrument to observe your technique in real-time and integrate therapeutic exercises with actual playing. The results are powerful: a case review found that 97.7 percent of professional musicians returned to full-time playing after using their instrument as a therapeutic tool. At Evolve, we've seen countless musicians return to their craft stronger and smarter than before, equipped for a long and sustainable career.
A Holistic Approach: The Musician's Support System

Recovering from a playing-related injury requires more than just physical exercises. At Evolve Physical Therapy, we believe hand therapy for musicians must address your entire well-being. Your identity, livelihood, and emotional health are all intertwined with your ability to play. That's why we advocate for a multidisciplinary team approach.
Your physician provides the medical diagnosis and foundation for care. Your music teacher offers invaluable insight into your technique, and we collaborate with them to ensure therapeutic changes work in a real-world performance context. A mental health professional is also a key team member. The psychological impact of an injury—anxiety, depression, and even identity crisis—is significant. Managing expectations and developing new, healthier movement patterns is a central part of recovery, and emotional support is vital.
Instrument Modifications, Splinting, and Ergonomics
Sometimes, the most effective treatment involves changing your instrument or environment, not just your body. Musical instruments evolved for sound, not comfort, often requiring awkward postures and excessive force.
Custom splints can be powerful tools. Designed specifically for musicians, they can support an injured joint during modified practice or help retrain movement patterns in conditions like focal hand dystonia.
Instrument adaptations, such as adding padding to reduce pressure points or adjusting straps for better weight distribution, can significantly reduce strain without compromising sound.
Ergonomic practice spaces are critical. We help you optimize your setup by focusing on neutral posture, reducing excessive force, ensuring ease of reach, setting proper instrument height, and minimizing static load and pressure points. These small adjustments compound over hours of practice and can be the difference between a sustainable career and chronic injury.
Proactive Prevention: Strategies for a Long and Healthy Career

While we excel at helping musicians recover, our ultimate goal is to prevent injuries from happening in the first place. Proactive prevention is the foundation of a long and healthy musical career. Good habits are essential, especially when returning to play after an injury.
Start with proper warm-up routines for your back, neck, and arms, just as an athlete prepares for a game. After playing, cool-down stretches help release tension and promote recovery. It's also crucial to take frequent breaks during practice; your body isn't designed for hours of repetitive motion without rest. If you feel pain after 30 minutes, try practicing for 20 and gradually build endurance.
Posture correction is key. Maintaining good upper back and neck posture prevents a cascade of problems. Likewise, stress management is vital, as performance anxiety and other pressures manifest physically as tension. Finally, a healthy lifestyle—sufficient sleep, a balanced diet, and limiting stimulants—supports your body's ability to perform and heal. The best injury is the one that never happens.
5 Essential Warm-Up Stretches for Musicians:
Wrist Flexor Stretch: Extend one arm, palm up. Use your other hand to gently pull your fingers down toward your body. Hold for 15-20 seconds and switch sides.
Wrist Extensor Stretch: Extend one arm, palm down. Gently pull your fingers down toward your body with your other hand. Hold for 15-20 seconds.
Finger Spreads: Place your hand flat on a table. Slowly spread your fingers as wide as is comfortable, hold, then relax. Repeat several times.
Thumb Stretch: Gently pull your thumb across your palm toward your pinky finger. Hold for 15-20 seconds on each side.
Shoulder Rolls: Roll your shoulders forward in a circle several times, then reverse. This releases tension in your neck and upper back.
Frequently Asked Questions about Hand Therapy for Musicians
What is the difference between a regular physical therapist and a therapist specializing in hand therapy?
A Certified Hand Therapist (CHT) represents the highest level of specialization in upper extremity care. A CHT is an occupational or physical therapist who has completed at least 4,000 hours of direct practice in hand therapy and passed a rigorous certification exam. This advanced training provides an in-depth knowledge of the intricate anatomy from the shoulder to the fingertips. For a musician, this expertise is invaluable for diagnosing and treating complex conditions like PRMDs, nerve compressions, and focal dystonia. A specialist can also analyze your unique playing habits and develop a highly personalized prevention program custom to your instrument.
How long does recovery take, and when can I play my instrument again?
Recovery is a unique journey for every musician, and there's no set timeline. The duration depends on the type and severity of your injury, your body's healing process, and the demands of your instrument. The process is phased: we focus on regaining mobility first, then move on to building strength once pain is managed. The most important step is creating a phased return-to-play plan, where you gradually reintroduce playing in a structured way to prevent re-injury. Patience and consistency with your therapy are key to a successful and lasting return to music.
Can hand therapy really help with a neurological issue like focal dystonia?
Yes. While focal dystonia is a neurological condition, specialized hand therapy for musicians plays a crucial role in its management. The condition involves maladaptive plasticity, where the brain's "map" of the fingers becomes disorganized. Our therapeutic approach focuses on neuromuscular reeducation to retrain the brain's motor control and sensory perception. Behavioral treatments like Sensory Motor Retuning (SMR), which have been shown to be effective, work by guiding your nervous system to re-establish normal movement patterns. It is genuine brain retraining. While there is no magic cure, a multimodal approach combining specific exercises, sensory reeducation, and splinting can lead to significant improvement in your ability to play.
Conclusion: Harmonize Your Health and Your Music
Your hands tell the story of your musical journey. For musicians in Brooklyn, they are the bridge between your artistry and the world. When pain threatens that connection, it can feel like losing a part of yourself. But you don't have to choose between your passion and your health.
Playing-related musculoskeletal disorders are common, but they don't have to end your career. Specialized hand therapy for musicians aims for the precision, endurance, and control your craft demands. Through instrument-focused rehabilitation, comprehensive assessments, and a commitment to prevention, we help you steer recovery and build a foundation for a long, healthy career.
The multidisciplinary approach we use at Evolve Physical Therapy means you're never on this journey alone. Whether you're recovering from an injury or facing the challenges of a condition like focal hand dystonia, we're here with the expertise and compassion you deserve.
Your music matters. Your health matters. With the right support, they can coexist in harmony.
Ready to get back to playing pain-free? Contact us for specialized hand therapy in Brooklyn and let's create your personalized path to recovery.
From Sidelines to Success: Brooklyn's Premier Sports Rehab
Why Brooklyn Sports Rehab Matters for Active New Yorkers

Brooklyn sports rehab is specialized physical therapy for athletes and active individuals. It's designed to help you recover from sports-related injuries, regain strength and mobility, and prevent future setbacks. Whether you're a marathon runner, a weekend basketball player, or just want to stay active without pain, sports rehabilitation provides the comprehensive care you need to get back to what you love.
Key services include:
- Injury Recovery and Post-Surgical Rehabilitation
- Performance Improvement and Running Gait Analysis
- Pain Management through Manual Therapy
- Injury Prevention and Core Strengthening
- Advanced Therapies like Blood Flow Restriction (BFR) and Kinesio Taping
Brooklyn's active community needs high-quality rehabilitation. Sports injuries are common, but physical therapy has a high success rate in helping people return to their previous performance level. Starting rehab soon after an injury significantly improves outcomes.
The best approach isn't just treating pain; it's understanding the root cause by analyzing movement patterns, muscle imbalances, and strength. A holistic approach also addresses the mental and emotional frustration of being injured.
I'm Lou Ezrick, founder of Evolve Physical Therapy. For nearly two decades, I've helped active Brooklynites recover and return to peak performance with hands-on, individualized Brooklyn sports rehab programs. At Evolve, we know every patient's journey is unique, and we tailor our care accordingly.

Understanding Common Sports Injuries in Brooklyn
Brooklyn is a hub of activity, from joggers on the Brooklyn Bridge to cyclists in Marine Park. This active lifestyle is great for health, but it also means sports injuries are a part of life. When you push your body, whether training for a marathon or in a pickup soccer game, having a solid Brooklyn sports rehab plan is essential.
At Evolve, we treat a wide range of sports injuries affecting active New Yorkers. These include:
- Ankle sprains from awkward landings.
- Hamstring strains, common in runners.
- Knee injuries, from runner's knee to more serious issues like meniscal tears and ACL injuries.
- Shoulder problems like rotator cuff strains, affecting swimmers and weightlifters.
- Tendinitis, such as Achilles tendinitis in runners or tennis elbow in racket sport players.
- Stress fractures from overtraining and concussions from contact sports.
Effective treatment requires understanding why an injury occurred. A runner's knee pain might stem from weak hips, or a shoulder injury from poor posture. At Evolve, we investigate these underlying biomechanical issues to provide a lasting solution. For more on our approach, see our page on sports physical therapy.
Why Early Intervention is Crucial
Many people think an injury will heal on its own, but waiting too long to seek professional help can turn a minor issue into a chronic problem. Starting Brooklyn sports rehab early, ideally within days of an injury or surgery, dramatically improves recovery.
Delaying treatment allows your body to develop compensatory movement patterns. For example, a sore knee can lead to a change in gait that causes hip or back pain. Early intervention stops this cascade. We can manage pain and inflammation, restore normal movement, and begin strengthening while tissues heal. This leads to stronger, healthier tissue and a faster return to your activities. The quickest way back to your sport is to start treatment promptly. Learn more about how sports medicine in Brooklyn can help you recover faster.
The Psychological Impact of Injury
An injury is more than a physical problem; it's an emotional one. For many, sports are a source of stress relief, social connection, and identity. Being sidelined can lead to frustration, anxiety, and even grief.
At Evolve, our approach to Brooklyn sports rehab treats the whole person. We understand the mind-body connection: your mental state affects healing, and physical pain impacts your emotional well-being. We create a supportive environment where you can discuss these frustrations, set realistic goals, and celebrate small victories. Rebuilding your confidence is just as important as rebuilding your strength, ensuring you return to your sport feeling ready, not fearful.
The Modern Approach to Brooklyn Sports Rehab
Modern physical therapy has evolved beyond standard exercises. Today's Brooklyn sports rehab is scientific, tech-powered, and personalized. At Evolve, this modern approach is central to our practice.

Our methods are built on a few key principles:
- Evidence-Based Practices: We use techniques validated by solid research, ensuring you receive the most effective care possible.
- Individualized Treatment Plans: Your body, injury, and goals are unique. We create a custom program for you—no cookie-cutter approaches.
- Holistic Care: We look at the whole picture, identifying the root cause of your injury rather than just treating symptoms. This is central to our "Evaluate, Heal, Strengthen" philosophy.
- One-on-One Attention: You get dedicated time with your therapist for hands-on manual therapy, real-time feedback, and a trusting therapeutic relationship.
Specialized Services for Peak Performance
Effective Brooklyn sports rehab requires specialized services to help you recover fully and perform at your best.
- Running Gait Analysis: We use advanced technology to analyze your running mechanics, identifying inefficiencies to help you run faster and pain-free.
- Post-Surgical Rehabilitation: We work closely with your surgeon to provide structured guidance, rebuilding your strength, mobility, and confidence after surgery.
- Blood Flow Restriction (BFR) Training: This cutting-edge technique helps you build significant muscle strength with lighter weights, reducing stress on healing tissues.
- Manual Therapy and Kinesio Taping: We use hands-on techniques like joint mobilization and soft tissue work to reduce pain and restore movement. Kinesio taping supports injured areas and improves body awareness.
- Virtual PT Sessions: For your convenience, we offer telehealth sessions so you can stay on track with your recovery from home. Explore our offerings on our Sports physical therapy services at Evolve Physical Therapy page.
Custom Brooklyn sports rehab for every athlete
You don't have to be a pro to deserve professional-level care. Our Brooklyn sports rehab programs are for athletes of all levels.
- Professional Athletes: We design programs to meet the intense demands of elite sports, focusing on a safe, rapid return to competition.
- Weekend Warriors: We help you get back to your local softball league or triathlon training with improved resilience.
- Youth Athletes: Our approach focuses on proper movement patterns and age-appropriate strength to build a foundation for a lifetime of healthy activity.
- Recreational Sports Participants: We help dancers, cyclists, hikers, and yoga enthusiasts return to the activities that bring them joy.
All our programs feature sport-specific training, which means we train movements that directly apply to your activity. This targeted approach ensures your body is truly ready when you return to your sport. Learn more on our Physical Therapy for Athletes page.
Your Path to Recovery and Prevention
Stepping into Brooklyn sports rehab is about reclaiming your active life. At Evolve Physical Therapy, we guide you through our refined process to ensure your recovery is effective and empowering.

We use a three-step process: Evaluate, Heal, and Strengthen. This is our roadmap from injury back to the activities you love.
- Evaluate: We begin with a comprehensive assessment to understand not just what's injured, but why. We examine how you move, identify weaknesses, and get the full picture.
- Heal: Next, we use hands-on manual therapy and targeted exercises to reduce pain, ease inflammation, and create the optimal environment for your tissues to repair.
- Strengthen: As pain subsides, we progressively challenge your body to become stronger than before. Our goal is to make you more capable and resilient, not just recovered.
Recovery timelines vary depending on the injury's severity, your overall health, and your consistency with your home exercise program. We'll provide a realistic timeline and set achievable goals together, celebrating each milestone along the way. Your "homework" is crucial—the work you do between sessions is what solidifies your progress and speeds up recovery.
The Role of PT in Preventing Future Injuries
Our mission with Brooklyn sports rehab extends beyond recovery to injury prevention. We help you break the cycle of getting hurt by:
- Identifying Movement Dysfunctions: We spot and correct inefficient movement patterns that put unnecessary stress on your joints.
- Building Core Strength: A strong core provides stability, improves balance, and significantly reduces the risk of back, hip, and knee injuries.
- Improving Flexibility and Balance: We use stretching and mobility work to keep your joints moving freely and balance training to sharpen your body's spatial awareness, preventing falls and twists.
- Providing Patient Education: We teach you proper technique for your sport and how to listen to your body's warning signals. This knowledge empowers you to become your own best injury prevention specialist. Learn more on our Sports physical therapy page.
Finding the Right Brooklyn sports rehab Center for You
Choosing the right clinic is a critical decision. Look for board-certified therapists with specialized training in sports rehabilitation. Prioritize clinics that offer personalized, one-on-one care custom to your specific goals, like we do at Evolve. Positive patient reviews and a strong community focus are also good indicators of quality care. Our team can help you steer insurance questions to maximize your coverage. As a practice rooted in Brooklyn, we serve our neighbors in Marine Park, Gravesend, Midwood, Park Slope, Mill Basin, and beyond.
Ready to start your recovery? Make An Appointment and begin your journey back to an active life.
Frequently Asked Questions about Sports Rehab
When you're dealing with a sports injury, it's natural to have questions. Here are answers to some common concerns about Brooklyn sports rehab.
How long does sports injury rehabilitation usually take?
Recovery time varies greatly depending on the severity of the injury, the type of tissue involved (muscle, ligament, bone), and your individual healing process. Factors like your age, overall health, and nutrition all play a role. However, the one factor you can control is your commitment to your treatment plan. Patients who are consistent with their home exercises typically recover faster. During your first visit, we will provide a personalized timeline based on your specific condition.
Do I need a referral from a doctor for physical therapy?
New York is a "Direct Access" state, meaning you can often see a physical therapist without a doctor's referral. However, your insurance plan may still require one for coverage. For post-surgical or complex cases, a referral helps us coordinate care with your physician. We recommend checking with your insurance provider about their requirements. Our office staff can assist you in navigating your benefits.
What should I wear to my physical therapy session?
The key is comfort and accessibility. Wear loose-fitting, athletic clothing like shorts, sweatpants, and a t-shirt or tank top. This allows you to move freely and gives your therapist easy access to the injured area for assessment and treatment. Also, be sure to wear supportive sneakers for safety during exercises.
Conclusion

The path from injury back to an active life doesn't have to be walked alone. Effective Brooklyn sports rehab is a comprehensive, personalized journey that addresses your physical injury and emotional well-being. At Evolve Physical Therapy, our "Evaluate, Heal, Strengthen" approach is designed to not just get you back to where you were, but to make you stronger and more resilient.
We are committed to getting you "Fit for Life" with one-on-one attention and sport-specific programs. Our practice is proud to serve the active communities of Brooklyn, including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin.
Don't let a nagging injury become a chronic problem. The sooner you start, the better your outcome. Take the first step toward recovery today. Begin your journey with Brooklyn sports rehab physical therapy and let us help you get back to doing what you love—stronger, smarter, and ready for whatever comes next.
Unlock Relief: The Ultimate How-To for Lower Back Herniated Disc Physical Therapy Exercises
Understanding Your Herniated Disc and the Path to Recovery
Lower back exercises for herniated disc physical therapy offer a proven, non-surgical way to manage pain and restore function. These targeted movements can reduce pressure on spinal nerves and strengthen supporting muscles, especially if you have pain radiating down your leg.
Key Exercises for Herniated Disc Recovery:
- Extension-Based Stretches - Press-ups and Sphinx Pose to reduce disc pressure
- Core Stabilization - Bird-Dog and Plank exercises to support your spine
- Gentle Mobility Work - Cat-Cow and Pelvic Tilts to restore movement
- Nerve Relief Stretches - Knee-to-Chest and Piriformis stretches to ease sciatic symptoms
What is a herniated disc? Your spinal discs are gel-filled cushions between your vertebrae. When the tough outer layer tears, the soft inner material can push out and press on nearby nerves, causing pain, numbness, or weakness—often radiating down your leg as sciatica.
Up to 80% of people experience lower back pain, with herniated discs being a common cause. The good news is that patients in an exercise program often report significant pain reduction and improved daily function, typically within 6-8 weeks.
Physical therapy aims to:
- Reduce pain and inflammation
- Centralize symptoms (move pain from your leg back toward your spine)
- Improve flexibility and range of motion
- Strengthen core muscles that stabilize your spine
- Prevent future injury through better movement patterns
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. For nearly two decades, I've helped patients recover from complex conditions by developing customized lower back exercises for herniated disc physical therapy programs. My approach combines manual therapy with progressive exercise to help you return to your favorite activities without surgery or long-term medication.
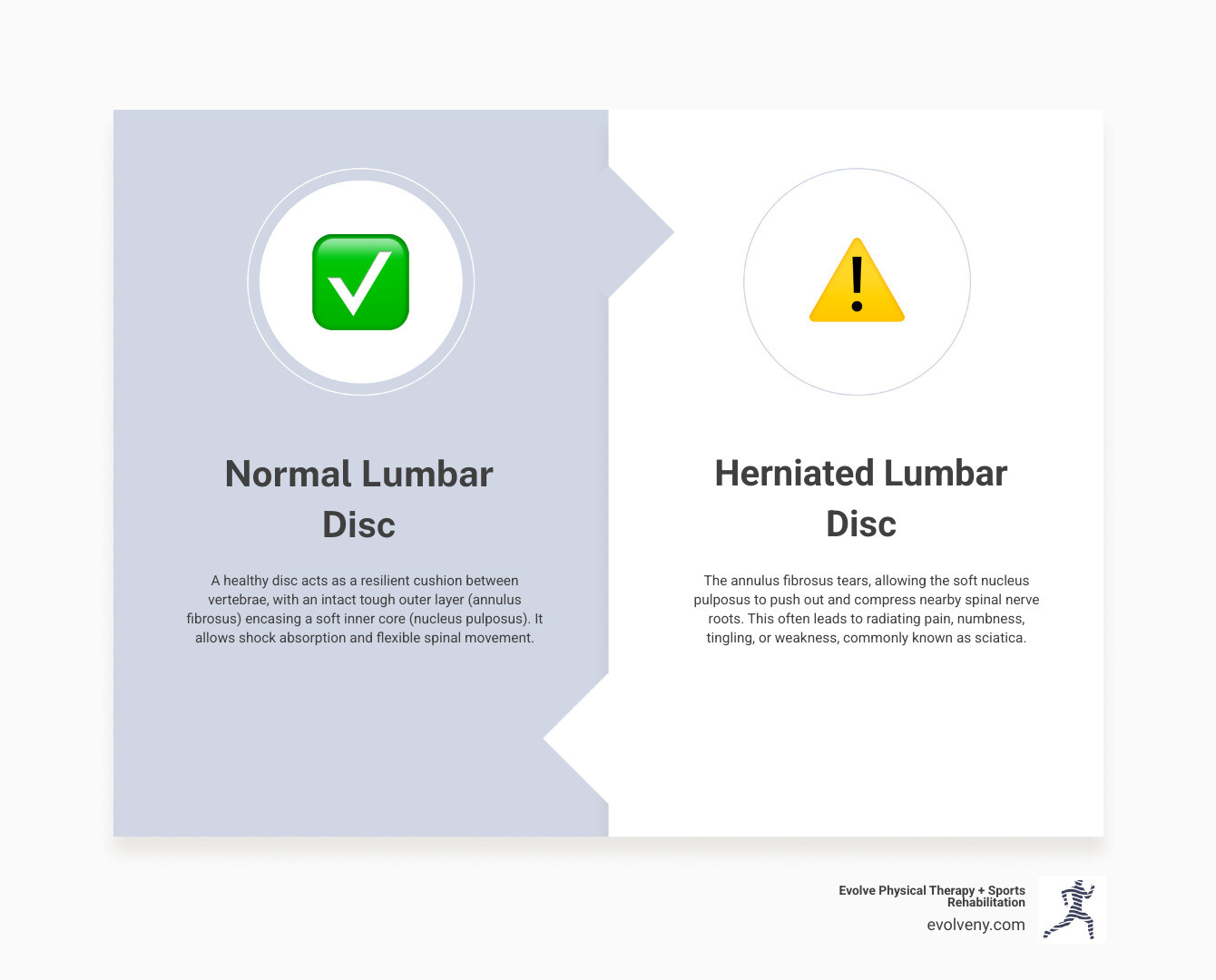
Your Guide to Lower Back Exercises for Herniated Disc Physical Therapy
Think of your spinal disc like a jelly donut. When it gets squished, the jelly can push out through a crack. That's essentially a herniated disc—the soft inner material breaks through the tough outer layer and presses on nearby nerves, causing pain, numbness, or weakness that often shoots down your leg (sciatica).
The good news is that lower back exercises for herniated disc physical therapy can address this problem without surgery. The goal is to help your body heal itself and prevent this from happening again.
Pain centralization is a key concept in your recovery. This is when pain moves from your leg back toward your spine. It's a sign of progress, meaning the exercise is reducing pressure on the irritated nerve root.
This is where the McKenzie Method is often used. According to clinical research, the McKenzie exercise program is believed to be one of the most beneficial for managing lumbar disc herniation. It focuses on specific movements that centralize your pain.
At Evolve Physical Therapy in Brooklyn—serving Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin—we know your injury is unique. We carefully monitor your pain-free range of motion and guide you through gradual progression, always respecting your body's signals.
Core stability is the foundation of our approach. Strengthening the deep muscles around your spine (transverse abdominis and multifidus) builds an internal support system, taking pressure off your injured disc.
Essential Stretches in Your Lower Back Exercises for Herniated Disc Physical Therapy Program
The right stretches can improve blood flow, relieve muscle tension, and gently decompress your spine. The key is to be gentle.

The Knee-to-Chest Stretch is simple and effective. Lie on your back with knees bent. For the single leg variation, gently pull one knee to your chest, holding for 15-20 seconds. Repeat 2-3 times per leg. If comfortable, progress to the double leg variation, pulling both knees to your chest for 15-30 seconds. Aim to do this twice daily.
The Piriformis Stretch targets a deep gluteal muscle that can compress the sciatic nerve. Lie on your back with knees bent. Cross one ankle over the opposite knee and gently pull the uncrossed knee toward your chest. Hold for 15-30 seconds, feeling a stretch in your glute. Repeat 2-3 times per side.
The Cat-Cow Stretch improves spinal mobility. On your hands and knees, inhale to arch your back (Cow Pose), letting your belly drop. Exhale to round your spine (Cat Pose), tucking your chin. Flow between poses for 1-2 minutes, completing 10 reps for 2-3 sets.
The Press-Up or Sphinx Pose is a lumbar extension that often reduces disc pressure. Lie face-down and prop yourself on your elbows under your shoulders (Sphinx Pose). Let your lower back arch gently, keeping your stomach and back muscles relaxed. Hold for 10-30 seconds and repeat 10 times. If comfortable, progress to a full Press-Up by straightening your elbows to push your upper body higher, keeping your hips on the floor. Hold for 6 seconds and repeat 8-12 times. Crucially, monitor your pain. Some back pain is normal, but if your leg pain increases or spreads, stop immediately and consult your physical therapist.
Core Strengthening: The Foundation of Lower Back Exercises for Herniated Disc Physical Therapy
Your core muscles provide essential spinal support. We focus on deep stabilizers like the transverse abdominis and multifidus to prevent recurrence.
The Bird-Dog teaches you to maintain a neutral spine. On your hands and knees, brace your core. Slowly extend your right arm and left leg, keeping your back flat and hips level. Hold for 2-3 seconds, then switch sides. Aim for 10-12 reps per side for 2-3 sets.
The Bridge activates your glutes and stabilizes your spine. Lie on your back with knees bent. Squeeze your glutes to lift your hips, forming a straight line from shoulders to knees. Avoid arching your back. Hold for 5-10 seconds and lower. Repeat 10-12 times for 2-3 sets.
The Plank builds core endurance. On your forearms, form a straight line from head to heels, engaging your core and glutes. For a modified plank, drop to your knees. Prioritize form over duration. Hold for 20-30 seconds, repeating 2-5 times.
Pelvic Tilts teach you to control your lower back. Lie on your back with knees bent. Gently flatten your lower back against the floor by tilting your pelvis and engaging your abs. Hold this small movement for 5 seconds. Repeat 10-15 times for 2-3 sets.
Exercises to Avoid: Protecting Your Spine During Recovery
Knowing what not to do is just as important as knowing the right exercises for a herniated disc. Certain movements can feel like picking at a wound, setting back your recovery.

High-Risk Movements and Activities
Movements that significantly increase disc pressure or involve excessive spinal flexion can derail your progress.
- Heavy lifting, especially with a rounded back, places enormous compressive force on your discs. A herniated disc can develop from heavy lifting, sudden pressure, or repetitive strenuous activities.
- Twisting motions, particularly while bending or holding weight, create a dangerous shearing force on the disc that can worsen the herniation.
- Toe touches and deep forward bends can be harmful. For a herniated disc, stretches that excessively bend forward are generally not advised because they can push disc material further out.
- Traditional sit-ups and crunches place excessive force on your lumbar spine. Safer, more effective alternatives like planks and bird-dogs are recommended.
- High-impact cardio like running and jumping jars the spine. Instead, choose low-impact alternatives like walking, swimming, or cycling to stay active without aggravating your disc.
Understanding Pain Signals
Learning to interpret your body's signals is crucial when doing lower back exercises for herniated disc physical therapy. Not all discomfort is bad, but some pain requires immediate attention.
- Peripheralization: The most important warning sign is pain moving further down your leg. This means the exercise is worsening nerve compression. Stop immediately and contact your physical therapist.
- Sharp Pain vs. Muscle Soreness: A mild, dull ache or muscle fatigue is often normal. However, sharp, shooting, or intense pain is a warning sign that something is wrong.
- When to Stop an Exercise: Stop any movement that causes increased leg pain, new numbness or tingling, or weakness. This is not a "no pain, no gain" situation; worsening pain can mean you're causing more damage.
At Evolve Physical Therapy, we teach our patients across Brooklyn—from Marine Park to Park Slope—to be their own best advocates. The importance of professional guidance cannot be overstated. It's always better to check in with a question than to push through pain and set back your recovery.
Progressing Safely and The Role of Posture
Recovery from a herniated disc is a gradual process. Lasting relief comes from building strength slowly, listening to your body, and understanding how your daily posture impacts your healing.
How to Safely Progress Your Exercise Program
Approach your lower back exercises for herniated disc physical therapy with patience and awareness, rather than trying to power through discomfort.
- Start Slow: Begin with just a few repetitions. It might feel easy, but you're building a solid foundation. As an exercise becomes comfortable, you can gradually increase the reps over several weeks.
- Use Pain as Your Guide: If pain centralizes (moves toward your spine), you're on the right track. If it increases or radiates down your leg, stop that movement. Differentiate normal muscle soreness from sharp nerve pain.
- Progress in Small Steps: Challenge your body just enough to encourage healing without overwhelming it. For example, hold a modified plank longer before trying a full one, or move from prone press-ups to gentle standing backbends.
- Build a Routine: Consistency is more important than intensity. Aim to do your exercises at the same time each day, even for just ten minutes. This consistency is what creates real change.
The Importance of Posture in Daily Life
You can do perfect exercises for an hour, but if you slouch at your desk for eight hours, you're working against yourself. Good posture is a constant, positive influence on your spine.
- Sitting Posture: Sitting, especially slouching, significantly increases disc pressure. Sit with a neutral pelvis, using a lumbar support roll or towel if needed. Stand up hourly to perform gentle back extensions.
- Standing Posture: When standing, keep your weight even, shoulders relaxed, and head held high. If you stand for long periods, shift your weight or use a small footstool to rest one foot.
- Lifting Technique: To lift, always bend at your knees, not your waist. Keep the object close to your body, engage your core, and use your powerful leg muscles. Never twist while lifting; move your feet to turn.
- Sleeping Position: Use a supportive mattress. Side sleepers should place a pillow between their knees to align the hips and spine. Back sleepers can put a small pillow under their knees. Try to avoid sleeping on your stomach, as this can increase disc pressure.
These posture adjustments, combined with your lower back exercises for herniated disc physical therapy, create an environment where your spine can heal and stay healthy long-term.
Frequently Asked Questions about Herniated Disc Exercises
We hear these questions daily at our Brooklyn clinic. Let's address the most common concerns about lower back exercises for herniated disc physical therapy.
How long does it take to see improvement with exercises for a herniated disc?
While every body heals differently, most patients notice significant improvement within 6-8 weeks of consistent physical therapy. Research supports this timeline, with many becoming symptom-free in 3-4 months.
Your recovery depends on the severity of the herniation, your overall health, and most importantly, your consistency with your exercise program. Active participation is essential for achieving significant pain reduction and returning to the activities you love.
Is walking good for a herniated disc?
Yes, walking is one of the best low-impact activities for a herniated disc. After an initial 2-3 days of rest, gentle walking is encouraged if it doesn't worsen your symptoms.
Walking increases blood flow to the disc, promoting healing and preventing stiffness. It also gently engages your core muscles for support. Start with short 5-10 minute walks around your Brooklyn neighborhood and gradually increase the time as tolerated. Listen to your body; if walking increases leg pain, numbness, or tingling, dial it back. Avoid prolonged bed rest, as studies show it can slow recovery.
When should I see a physical therapist for my lower back pain?
If your back pain is concerning you, it's best to see a physical therapist sooner rather than later.
You should definitely see a PT for:
- Persistent pain that lasts more than a few days.
- Radiating symptoms like pain, numbness, tingling, or weakness down your leg.
- Pain that disrupts your daily life, making it hard to sit, stand, walk, or sleep.
It's also crucial to see a physical therapist before starting any new exercise program for back pain. A proper diagnosis and personalized guidance ensure you perform exercises that help, not harm, your specific condition. Early intervention with physical therapy often leads to better outcomes than medication or surgery for many herniated disc cases. We've helped hundreds of patients in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin avoid surgery and get back to their lives.
Take Control of Your Recovery
Living with a herniated disc is overwhelming, but your body has an incredible capacity to heal when given the right support and guidance. At Evolve Physical Therapy + Sports Rehabilitation, we've seen this firsthand.
We've helped hundreds of patients from Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin who thought they'd never get back to their normal lives. The difference is a personalized approach to lower back exercises for herniated disc physical therapy that addresses the root cause of your pain, not just the symptoms.
Movement is medicine, but it must be the right movement. A qualified physical therapist can provide the guidance you need to ensure your efforts promote healing.
Listen to your body's signals. Pain moving down your leg (peripheralization) is a sign to stop and adjust. This is where our hands-on guidance becomes invaluable.
Consistency beats intensity. You don't need to push through excruciating pain. Daily gentle exercises, good posture, and trusting the process are what lead to long-term relief.
I've seen patients who could barely walk into our clinic return to running, playing with their kids, and enjoying life without constant pain. It's the result of evidence-based physical therapy, targeted exercises, and a partnership between therapist and patient.
You don't have to steer this journey alone. Our team at Evolve is passionate about empowering you to take control of your recovery. We combine manual therapy with progressive exercise programs customized to your condition and goals.
Ready to start feeling better? Learn more about our specialized physical therapy for herniated discs in Brooklyn and let us help you find lasting relief. Your future self is waiting.
Beyond the Blade: Your Timeline for Hand Surgery Physical Therapy
Understanding Your Recovery Journey After Hand Surgery
How long is physical therapy after hand surgery depends largely on the type of procedure you've had. Here's what you can typically expect:
| Surgery Type | PT Duration | Examples |
|---|---|---|
| Minor Procedures | 4-6 weeks | Carpal tunnel release, trigger finger release, ganglion cyst removal |
| Moderate Procedures | 6-12 weeks | Tendon repairs, ligament repairs |
| Complex Procedures | 8 weeks - 6+ months | Fracture fixation, joint replacement, severe nerve damage |
Hand surgery is the first step in your recovery, but the real work begins afterward. Recovery time varies based on the surgery's complexity, your overall health, and your commitment to therapy. While some patients heal in weeks, others may need months of rehabilitation to regain full function.
The rehabilitation process can range from several weeks to several months, with therapy sessions and home exercises being crucial. Most people can return to work within 6 to 14 weeks, but full recovery can take over a year for complex procedures.
As Lou Ezrick, founder of Evolve Physical Therapy, I've spent nearly two decades guiding patients through this process. My approach focuses on addressing the root cause of dysfunction with hands-on, customized treatment plans and realistic timelines.

The "Why" Behind Hand Therapy: Goals and Foundations
Your hands are essential for connecting with the world. When surgery for carpal tunnel, a fracture, or tendon damage makes everyday activities impossible, physical therapy is crucial for getting your life back. At Evolve Physical Therapy + Sports Rehabilitation, our central goal is to help you regain optimal function and return to the activities you love.
Understanding how long is physical therapy after hand surgery begins with knowing the goals of rehabilitation:
- Pain and Swelling Management: Immediately after surgery, our priority is to control discomfort and swelling. We use techniques like proper ice application, elevation, compression, and gentle movements that reduce pain and move fluid out of your hand, speeding up the healing process.
- Restoring Range of Motion: To prevent stiffness and permanent limitations from scar tissue, we start with careful exercises. This often begins with passive motion (where the therapist moves your hand) and progresses to active motion as you heal, protecting the surgical repair.
- Regaining Strength: A hand that can move but lacks strength isn't functional. We introduce progressive resistance exercises, starting with light movements and gradually building up to prepare your hand for real-world demands.
- Scar Tissue Management: Excessive or poorly managed scar tissue can restrict movement. We use specialized techniques like scar massage and tissue mobilization to soften scars and prevent adhesions, improving long-term function.
- Functional Recovery: All therapy serves to restore your ability to perform daily tasks. We tailor exercises to mimic your real-life activities, from writing and dressing to using tools at work.
Hand therapy is a highly specialized field requiring advanced training in the complex anatomy of the hand, wrist, and forearm. Our therapists, including Certified Hand Therapists (CHTs), have this expertise. Unlike general PT, hand therapy provides precise, nuanced care that addresses the delicate structures in your hand. At Evolve, we integrate perspectives from both Occupational and Physical Therapy to ensure a comprehensive recovery that addresses mobility, strength, and functional tasks.
Key Factors That Determine Your Recovery Timeline
Your recovery timeline is as individual as your fingerprint, but we can create a personalized rehabilitation plan by looking at several key variables. How long physical therapy after hand surgery will take depends on these factors:
- Type and Complexity of Surgery: A simple carpal tunnel release has a much shorter recovery than a complex joint replacement. Each procedure affects different tissues—bones, tendons, nerves—that heal at different rates. More intricate surgeries with extensive hardware naturally require a more cautious and lengthy rehabilitation.
- Severity of the Original Injury: A clean break heals faster than a shattered bone with significant soft tissue trauma. The more damage your body needs to repair, the longer your recovery will be.
- Overall Health and Age: Conditions like diabetes or vascular disease can slow healing. Conversely, good general health provides a strong foundation for recovery. While younger patients often heal faster, dedicated older patients can also achieve excellent results.
- Lifestyle Habits: Your habits can support or sabotage recovery. Smoking is a major offender, as it restricts blood flow and slows healing. A nutritious diet, adequate rest, and stress management all contribute to better outcomes.
- Patient Compliance: This is often the deciding factor. Following your home exercise program, respecting activity restrictions, and attending all appointments are crucial. Patients who are committed to their therapy consistently have faster, more successful recoveries.
- Surgeon's Protocol: Every surgeon has specific post-operative guidelines. At Evolve Physical Therapy + Sports Rehabilitation, we work closely with your surgeon to ensure your therapy plan aligns perfectly with their recommendations, creating a unified team approach to your recovery.
How Long is Physical Therapy After Hand Surgery? A Timeline Guide
While every recovery is unique, how long is physical therapy after hand surgery generally falls into predictable timelines based on your procedure. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we've guided hundreds of patients through these journeys.
How Long is Physical Therapy After Hand Surgery for Minor Procedures?
These procedures involve less invasive techniques and offer a relatively quick recovery.
- Carpal Tunnel Release: Therapy typically lasts 4-6 weeks. We focus on reducing swelling, restoring motion, managing the scar, and rebuilding grip strength.
- Trigger Finger Release: Recovery is often speedy, requiring just 2-4 weeks of therapy to get the finger moving smoothly without catching.
- Ganglion Cyst Removal: A similar 2-4 week timeline is common. We work on wound healing, reducing swelling, and restoring normal joint movement.
Most patients can return to daily activities within a month or two after these minor procedures.
Timelines for Moderate Procedures (Tendon & Ligament Repair)
These repairs are more involved and require more patience, as tendons and ligaments need careful protection while they heal.

- Flexor and Extensor Tendon Repairs: This is a challenging recovery, often requiring 6-12 weeks of therapy. Tendons are prone to forming adhesions (internal scar tissue), so we follow a strict, phased approach. This starts with a protection phase in a splint, followed by supervised passive motion within days of surgery to prevent stiffness. Around the 4-week mark, you'll begin active motion, with lifting restrictions that may last up to 3 months. This detailed flexor tendon repair protocol offers a comprehensive look.
- Ligament Repairs: Therapy typically requires 4-8 weeks. The approach is similar: protect the repair, then gradually restore motion and build stability.
The key is respecting biology. Pushing too hard, too soon can undo the surgical work.
Recovery Duration for Complex Procedures (Fractures, Joint Replacement)
These surgeries involve extensive reconstruction and the longest rehabilitation commitment.
- Fracture Fixation: Expect 8-12 weeks of physical therapy. While the bone heals (a process that takes 8-12 weeks), we protect the fracture site while keeping other joints mobile. Once the bone is stable, we work aggressively to restore full motion and strength.
- Joint Replacement Surgery: Therapy for a finger or wrist joint replacement typically spans 3-6 months. We focus on restoring smooth, pain-free movement and functional strength.
- Severe Nerve Damage: This requires the most patience, with therapy lasting 6 months or longer. Nerves regenerate very slowly. Therapy focuses on nerve gliding, sensory re-education, and maintaining joint mobility while the nerve regrows.
These recoveries follow distinct biological healing phases, which guide the intensity of your exercises. You can learn more from this overview of post-operative treatment phases. The journey is long, but significant improvement is achievable with consistent effort.
Your Road to Recovery: What to Expect in Therapy
Recovery isn't just about healing an incision; it's about restoring movement, strength, and confidence. At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, our programs guide you through each stage of healing.
The Initial Phase (Weeks 1-3): Protection and Early Movement
The first few weeks are critical for protecting your surgeon's work while encouraging healing.
- Splinting and Protection: Your hand will likely be immobilized in a splint or cast to allow the surgical site to heal without disruption.
- Swelling and Pain Management: We'll teach you to manage swelling with elevation, ice, and compression. Gentle therapeutic techniques will help control discomfort.
- Wound Care: Keeping your incision clean and dry is vital to prevent infection and support the body's natural healing process.
- Early Gentle Motion: Depending on your surgery, we may begin passive range of motion exercises (where the therapist moves your hand) within days. This controlled movement is crucial for preventing stiffness.
The Repair Phase (Weeks 4-8): Regaining Motion and Function
Now, we shift to helping you actively reclaim your hand's movement.
- Weaning Off the Splint: You'll gradually transition from full-time splinting to more freedom of movement.
- Active Range of Motion: You'll begin moving your hand yourself with specific exercises to prevent permanent stiffness.
- Scar Massage: We'll teach you how to massage your scar to prevent adhesions and improve mobility.
- Light Functional Use: You'll start reintroducing your hand into very light daily activities, with gradual lifting restrictions (e.g., 2-4 pounds) introduced as you progress.
The Strengthening Phase (Weeks 9-12+): Building Back Strength
This phase focuses on building robust strength and preparing you for a full return to your life.
- Progressive Resistance: We'll use therapy putty, grip strengtheners, and light weights to rebuild muscle strength and endurance.
- Fine Motor Skills: Exercises like picking up small objects will help restore dexterity.
- Return to Work and Hobbies: We create a realistic plan for returning to your job, sports, or hobbies, often involving activity-specific drills. Most people can return to work within 6 to 14 weeks, though demanding jobs require more time.
Challenges That Can Affect Your Timeline
While we aim for a smooth recovery, challenges can arise and extend your therapy timeline.
- Infection: A risk with any surgery that delays healing. Contact your doctor for fever, worsening pain, or drainage.
- Complex Regional Pain Syndrome (CRPS): A rare but serious condition of chronic, disproportionate pain that requires specialized treatment.
- Excessive Scar Tissue or Stiffness: Sometimes, despite best efforts, stiffness or scar tissue can restrict movement and may require more intensive therapy or even a second procedure.
- Delayed Healing: This can result from poor nutrition, smoking, or chronic health conditions.
Your active participation is paramount. Patients who consistently perform their home exercises and follow restrictions have the best outcomes. You are the most important member of your recovery team.
Conclusion: Partnering for a Successful Recovery
Recovering from hand surgery is a process with a unique timeline for every patient. While we've explored how long physical therapy after hand surgery typically takes, what matters most is your patience, commitment, and partnership with the right therapy team. Each session and exercise brings you closer to regaining independence and returning to the activities you love.
At Evolve Physical Therapy + Sports Rehabilitation in Brooklyn, we are your partners in this journey. Our specialized therapists use a hands-on approach, creating customized programs for the intricate needs of hand recovery. We guide you from your initial evaluation to your final strengthening session, adjusting your plan and celebrating every milestone.
The most powerful tool in your recovery is you. Your dedication to home exercises and adherence to activity restrictions make all the difference. We've seen patients exceed expectations simply by trusting the process and putting in the daily effort. We are here to guide you, but your participation drives the healing.
If you are preparing for hand surgery or are currently in recovery, our team has the specialized knowledge and compassionate care to help you move forward with confidence. Your hand is remarkable, and with the right rehabilitation, we can help you open up its potential once again. Learn more about our post-operative physical therapy programs in Brooklyn and take the first step toward reclaiming the function you deserve.
Move Better, Live Better: Physical Therapy for Movement Disorders
Why Movement Disorder Physical Therapy is Essential for Better Living

Movement disorder physical therapy is a specialized form of rehabilitation for people with neurological conditions that affect the brain's control of movement. It helps improve mobility, balance, and quality of life for those with symptoms like tremors, stiffness, or uncontrolled movements.
Quick Answer: What can movement disorder physical therapy do for you?
- Improve balance and coordination to reduce fall risk
- Increase strength and flexibility for better daily function
- Retrain movement patterns using specialized techniques
- Manage symptoms of conditions like Parkinson's, dystonia, and tremors
- Maintain independence longer through targeted exercises
- Reduce pain and stiffness associated with movement disorders
According to research, physical rehabilitation based on understanding of functional neurological disorders can result in symptom improvement in 60 to 70 percent of people. For Parkinson's disease, studies show that at least 2.5 hours of physical activity per week can slow symptom progression. The key is finding a specialized approach, as physical therapy for movement disorders isn't one-size-fits-all.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. With nearly two decades of experience helping patients with complex neurological conditions, I know that effective movement disorder physical therapy requires both hands-on expertise and a deep understanding of the brain-body connection.
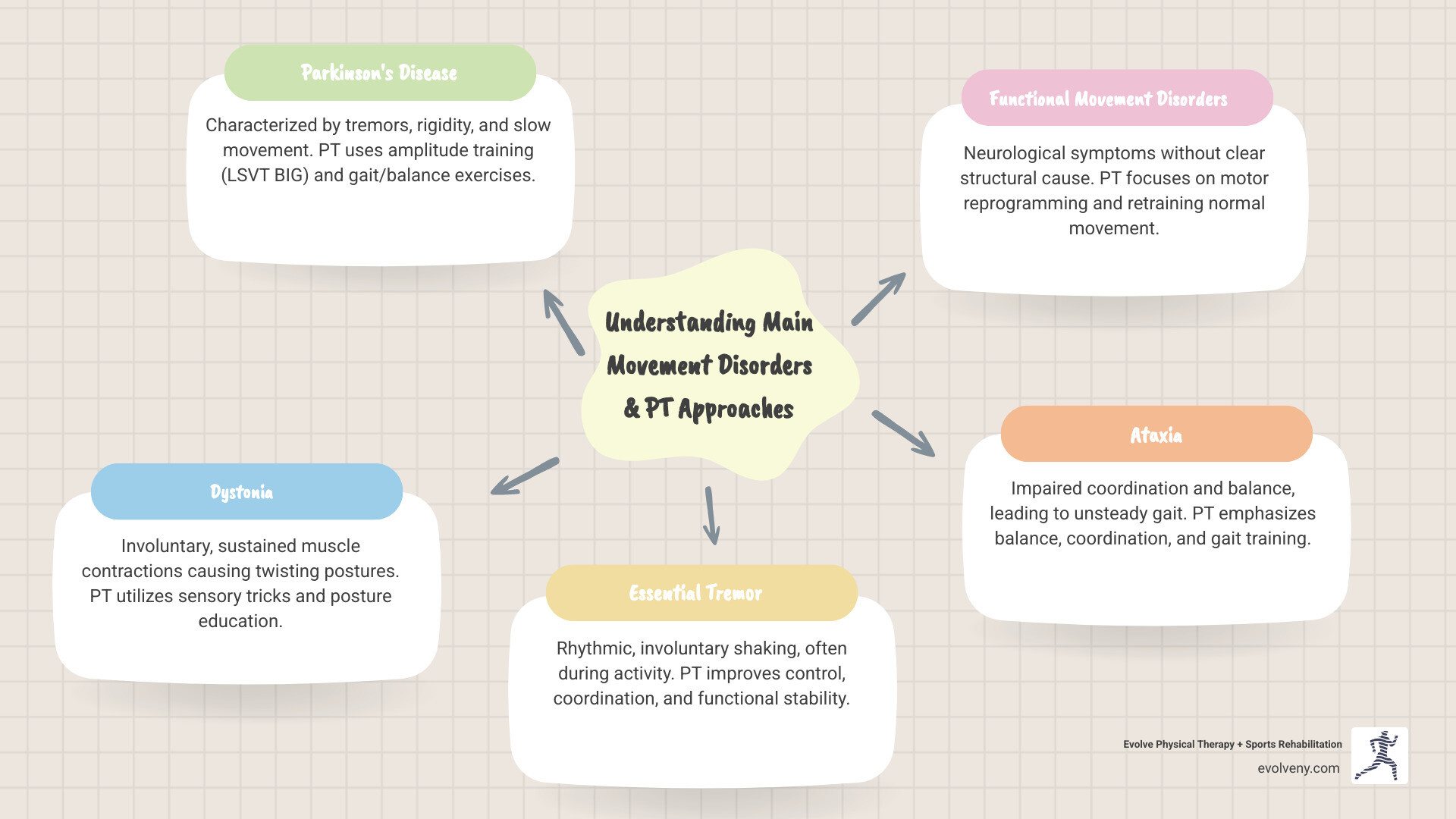
Understanding Movement Disorders
A movement disorder is a neurological condition that impairs the control and coordination of movement. The signals between the brain, nerves, and muscles don't flow smoothly, leading to movements that are either too much, too little, or abnormal.
Movement disorders are broadly categorized into two groups:
- Hypokinetic disorders: Characterized by slowness, stiffness, or loss of movement.
- Hyperkinetic disorders: Involve excessive, involuntary movements like tremors, tics, or jerks.
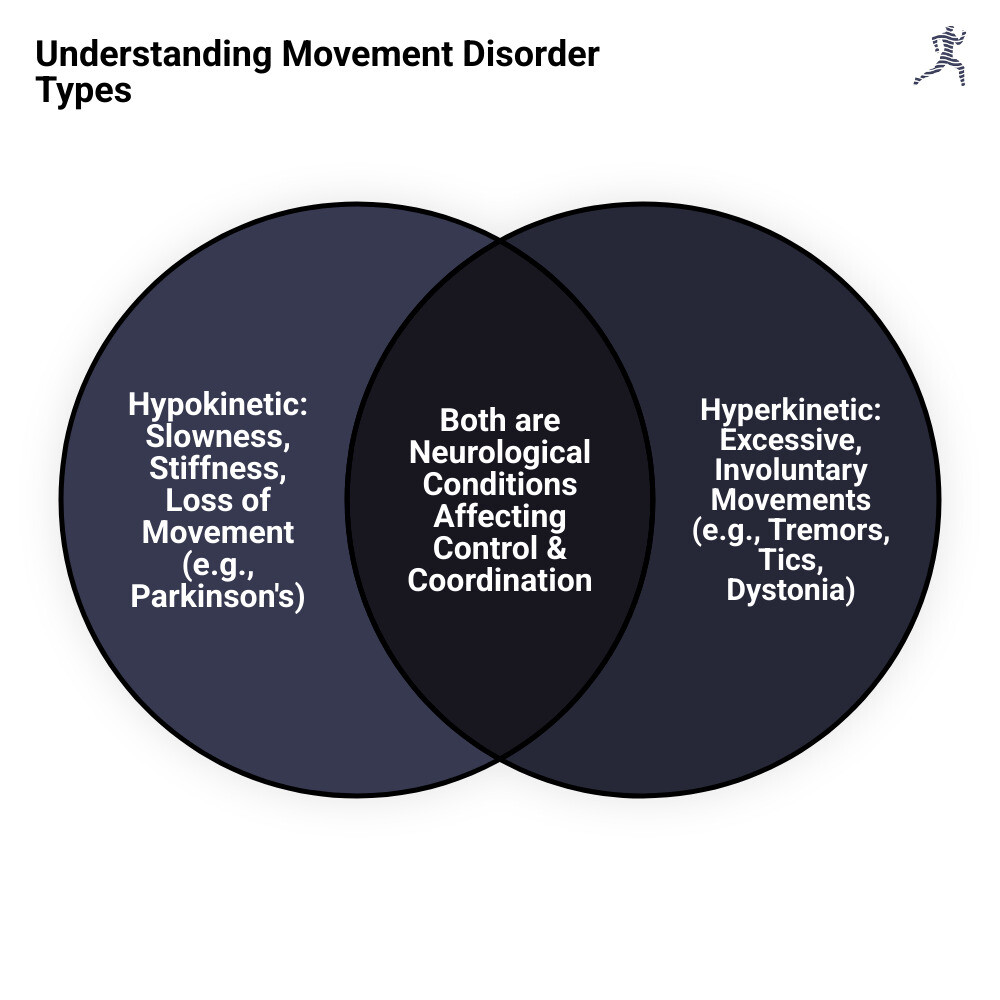
Understanding this distinction is crucial because it directly informs the type of movement disorder physical therapy interventions we use.
Main Types of Movement Disorders
A thorough neurological examination is key to diagnosing these conditions. Some of the more common types include:
- Parkinson's Disease (PD): A well-known hypokinetic disorder, Parkinson's is characterized by tremors, bradykinesia (slow movement), rigidity, and postural instability. It is the second most common degenerative brain disorder in adults.
- Dystonia: This condition causes uncontrollable muscle contractions, leading to repetitive, twisting movements and painful postures. It can be localized or generalized.
- Essential Tremor: The most common movement disorder, it causes rhythmic, involuntary shaking, most often in the hands during voluntary movements like writing.
- Huntington's Disease (HD): A hereditary disorder combining cognitive issues, psychiatric disorders, and hyperkinetic movements such as chorea (involuntary jerking or writhing).
- Functional Movement Disorders (FMD): Also known as Functional Neurological Disorder (FND), FMD involves real symptoms like weakness or tremor that are not caused by structural damage but by a problem with how the nervous system functions. Specialized rehabilitation offers significant hope.
- Ataxia: This refers to a lack of muscle coordination during voluntary movements, resulting from damage to the cerebellum. It leads to an unsteady gait and difficulties with fine motor skills.
- Tics and Tourette Syndrome: Tics are sudden, repetitive movements or vocalizations. Tourette Syndrome is characterized by multiple motor tics and at least one vocal tic.
Understanding these conditions is the first step in providing effective movement disorder physical therapy. For a more general overview, you can find more information about What are movement disorders?.
The Crucial Role of Movement Disorder Physical Therapy
For those with a movement disorder, movement disorder physical therapy is a central part of regaining control and improving daily life. At Evolve Physical Therapy, our science-based approach focuses on preventing further issues, treating symptoms, and rebuilding physical abilities to maximize your independence and quality of life.
Our work is guided by neuroplasticity—the brain's ability to rewire itself. Through specific, repeated exercises, we help your brain improve movement control. This pairs with motor learning, where we help you refine physical skills through practice and feedback.
At Evolve Physical Therapy + Sports Rehabilitation, we create highly individualized treatment plans because there is no one-size-fits-all solution. To understand more about our general philosophy, visit our page on More info about Neurological Physical Therapy.
Goals of Movement Disorder Physical Therapy
We work with you to set clear, meaningful goals. Common objectives include:
- Improve balance and coordination to feel more stable and secure.
- Increase strength and flexibility to combat stiffness and weakness.
- Reduce fall risk by improving balance, gait, and reaction time.
- Maintain independence in daily activities and hobbies.
- Manage pain resulting from abnormal postures or muscle stiffness.
- Improve gait patterns for a safer, more efficient, and confident walk.
Our commitment to keeping you safe is a big part of what we do. For more details, check out our page on More info about Physical Therapy for Fall Prevention.
The Physical Therapy Evaluation Process
Your journey with movement disorder physical therapy at Evolve begins with a thorough evaluation to understand your unique challenges and strengths. This comprehensive first step includes:
- Initial Assessment: We discuss your medical history, current symptoms, and what you hope to achieve.
- Movement Analysis: Our expert therapists observe you performing activities like walking and reaching to pinpoint problematic movement patterns, whether they are hypokinetic (too slow) or hyperkinetic (involuntary).
- Strength and Balance Testing: We use objective tests to measure muscle strength and assess fall risk, identifying specific weaknesses or balance system issues.
- Flexibility and Range of Motion Assessment: We check your joints and muscles for stiffness that may limit movement and cause pain.
- Goal Setting: Based on all findings, we collaborate with you to create realistic and meaningful goals for your therapy.
- Functional Outcome Measures: We use standardized tests to track your progress over time, ensuring our treatments are effective and allowing us to adjust your plan as needed.
Common Physical Therapy Interventions and Techniques
After your evaluation, we develop a personalized treatment plan using evidence-based techniques. Our hands-on approach combines remediation (restoring normal movement) with compensation (teaching adaptive strategies) to maximize your function.

A core part of our methodology is task-specific training. We practice movements relevant to your daily life with high repetition and intensity, leveraging neuroplasticity to optimize recovery.
Interventions for Parkinson's Disease
We use specialized techniques to address the challenges of Parkinson's disease:
- Amplitude Training (LSVT BIG): This program uses large, exaggerated movements to retrain muscles and help the brain recalibrate its sense of normal movement size.
- Reciprocal Pattern Exercises: We use activities like cycling or focused walking to reinforce natural, reciprocal movements like arm swing.
- Gait and Balance Training: We focus on improving walking speed and stability, using cueing strategies to overcome freezing of gait and reduce fall risk.
- Flexibility and Stretching: Regular stretching is emphasized to counteract stiffness in key muscle groups and maintain range of motion.
- Strength Training: Resistance training is used to build strength and power, which can reduce the severity of motor symptoms.
We offer specialized programs like Rock Steady Boxing for Parkinson's, which uses intense, varied exercise to combat PD symptoms. Learn more about our approach to More info about Physical Therapy for Parkinson's Disease.
Interventions for Functional Movement Disorders (FMD)
Our movement disorder physical therapy for FMD focuses on "motor reprogramming" to help the brain unlearn abnormal patterns and relearn normal, automatic movement.
- Retraining Normal Movement: We use exercises that progress from simple to complex to re-establish typical movement patterns.
- Distraction Techniques: We use distraction during motor tasks to help bypass the conscious effort that can worsen symptoms.
- Positive Reinforcement: We focus on and celebrate therapy-related improvements to reinforce desired movement patterns.
- Avoiding Adaptive Equipment (when appropriate): To prevent deconditioning, we encourage independent movement, avoiding over-reliance on assistive devices.
Our approach aligns with Consensus Recommendations for FND Physiotherapy.
Interventions for Balance and Dystonia
These conditions require specific, targeted interventions:
- Vestibular Rehabilitation: For dizziness or vertigo, we use exercises to improve the inner ear system and gaze stabilization.
- Sensory Tricks (Alleviating Maneuvers): For dystonia, we teach gentle touches or positions that can temporarily alleviate involuntary muscle contractions.
- Posture Education: We work on retraining posture to improve alignment, reduce discomfort, and improve mobility.
- Prolonged Stretching and Splinting: For severe muscle overactivity, we may use prolonged stretching or splinting to increase flexibility.
For more details on how we address these issues, please visit our page: More info about Balance and Vertigo Physical Therapy.
Benefits, Evidence, and the Multidisciplinary Team
Starting movement disorder physical therapy opens the door to profound benefits that can touch every part of your life. The power of this therapy lies in improved mobility, improved safety, and increased confidence. As you become more independent, caregiver burden is often reduced. Our ultimate goal is to improve your quality of life and empower you with strategies for long-term management.

Evidence-Based Movement Disorder Physical Therapy for Specific Conditions
The effectiveness of movement disorder physical therapy is strongly supported by research. We rely on science to ensure you receive the best possible care.
For Functional Movement Disorders (FMD), studies show that specialized physical therapy can lead to symptom improvement for 60 to 70 percent of individuals. Intensive, goal-oriented programs have demonstrated significant, long-lasting success. One study found that after a one-week program, 73.5% of patients were "markedly improved," with 60.4% maintaining that improvement years later.
For Parkinson's Disease (PD), the evidence is just as compelling. High-intensity training is proven to improve walking and movement, and inpatient rehabilitation can slow the decline in motor function. The American Physical Therapy Association (APTA) provides evidence-based guidelines to ensure top-notch care. You can explore their recommendations here: APTA Clinical Practice Guideline for Parkinson Disease.
The Role of PT in a Multidisciplinary Team
Managing a movement disorder is a team effort. Movement disorder physical therapy is most effective when integrated with other healthcare professionals to provide holistic care. Our physical therapists work closely with:
- Neurologists: To align therapy with your medical plan, including medications or treatments like Deep Brain Stimulation.
- Occupational Therapists (OTs): To help with daily activities like dressing, cooking, and managing fatigue.
- Speech-Language Pathologists (SLPs): To address difficulties with speech and swallowing.
- Physiatrists: Rehabilitation doctors who often oversee the entire rehabilitation plan.
- Neuropsychologists: To help with the cognitive and emotional challenges of living with a movement disorder.
This integrated care approach leads to better results and a stronger support system, a model supported by research such as this Systematic review of integrated care in Parkinson's.
Finding a Therapist and Future Directions
Choosing the right physical therapist is a critical step. You need a specialist who understands the nuances of neurological conditions and can address both the physical and psychological impacts of a movement disorder.
How to Find a Specialist Physical Therapist
When looking for an expert in movement disorder physical therapy, we recommend the following:
- Get Recommendations: Ask your neurologist for referrals to physical therapists specializing in neurological conditions.
- Ask About Experience: Inquire about the therapist's specific experience and training with conditions like Parkinson's, dystonia, or FMD.
- Check for Credentials: Look for board-certified clinical specialists in neurologic physical therapy (NCS) or those with relevant residency/fellowship training.
- Use Online Directories: The APTA's "Find a PT" tool can help you locate qualified professionals. You can find their tool here: Find a PT Near You with APTA's tool.
- Communicate Your Goals: Discuss your concerns and goals during an initial consultation to ensure a good fit.
At Evolve Physical Therapy + Sports Rehabilitation, our team in Brooklyn (Marine Park, Gravesend, Midwood, Park Slope, Mill Basin) is experienced in treating complex neurological conditions.
Advancements in Neurorehabilitation
The field of neurorehabilitation is constantly evolving, bringing exciting new tools to movement disorder physical therapy:
- Wearable Technology: Smart sensors provide real-time feedback on movement for more precise, personalized interventions.
- Virtual Reality (VR): VR creates immersive, safe, and motivating environments for practicing complex movements and balance tasks.
- Noninvasive Brain Stimulation: Techniques like TMS and tDCS are being studied to improve motor learning and neuroplasticity alongside physical therapy.
- Telerehabilitation: Remote therapy sessions increase access to specialized care for those who have difficulty traveling to a clinic.
These advancements promise to improve the effectiveness and accessibility of therapy. For more information, you can refer to relevant Research on neurorehabilitation advancements.
Conclusion: Take Control of Your Movement
Living with a movement disorder is challenging, but you are not alone, and there is significant hope for improvement. Here at Evolve Physical Therapy + Sports Rehabilitation, we want you to know that you can feel better and move more freely.
Movement disorder physical therapy is a partnership. We provide the tools, strategies, and personalized guidance to empower you to take charge of your movement, manage your symptoms, and maintain your independence. Our unique approach to evaluation, healing, and strengthening is designed to help you move better, so you can live better.
Whether you're navigating Parkinson's disease, FMD, dystonia, or another condition, proactive, specialized physical therapy can make a huge difference. Our innovative programs, like our popular Rock Steady Boxing for Parkinson's patients, show our dedication to providing effective care.
Don't let your symptoms dictate your life. Take the first step toward feeling more in control and improving your well-being.
If you're in Brooklyn—including Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin—we invite you to find how our specialized movement disorder physical therapy can help. Ready to start your journey? Learn more by visiting our page on Parkinson's Physical Therapy in Brooklyn. We're excited to help you evolve!
How Much Do Pediatric Physical Therapy Assistants Really Make?
Understanding the National Pediatric Physical Therapy Assistant Salary

Becoming a Pediatric Physical Therapy Assistant (PTA) offers a rewarding career helping children improve their movement, balance, and coordination. For those considering this path, understanding the financial landscape is a crucial first step. This guide explores the earning potential for this specialized role, from average salaries to the factors that influence your income.
If you're wondering about the pediatric physical therapy assistant salary in the United States, here’s a quick overview:
- Average Salary: Approximately $66,064 per year
- Salary Range: From $59,406 to $72,361 annually
- Highest Paying States: District of Columbia ($73,146), California ($72,868), and New Jersey ($71,606).
Louis Ezrick, founder of Evolve Physical Therapy, has nearly two decades of experience in chronic pain management and movement optimization. His patient-first approach informs his understanding of what makes a physical therapy career, including that of a pediatric PTA, both rewarding and well-compensated.
On average, a Pediatric Physical Therapy Assistant in the United States earns approximately $66,064 per year, which translates to roughly $29.17 per hour, according to 2025 data. This respectable wage reflects the specialized skills and dedication required for the role.
The Typical Pediatric Physical Therapy Assistant Salary Range
While the average provides a good overview, the full salary range gives a more complete picture. For a Pediatric PTA, salaries typically range from $59,406 to $72,361 per year. This highlights that factors like experience, location, and specific responsibilities play a significant role in determining earnings.
At the lower end, a Pediatric PTA might earn around $42,244 annually (10th percentile). At the higher end, earnings can reach about $81,328 (90th percentile). This broad spectrum shows substantial room for growth as your career progresses.
Average Pediatric Physical Therapy Assistant Salary vs. General PTA
Aspiring PTAs often wonder if specializing in pediatrics impacts earning potential. The average pediatric physical therapy assistant salary of $66,064 per year is slightly higher than the median for general physical therapist assistants, which was $65,510 in May 2024 according to the U.S. Bureau of Labor Statistics. This subtle difference suggests that the specialized knowledge and unique demands of working with children can command slightly higher compensation.
This isn't surprising, as the demand for pediatric PTAs is rising due to advancements in medical technology that expand treatment options for children with physical disabilities. At Evolve Physical Therapy, we deeply appreciate the specialized care required for pediatric patients. This expertise often translates into a competitive edge in the job market, potentially leading to better compensation and more fulfilling career opportunities.
Key Factors That Influence Your Earning Potential
Your pediatric physical therapy assistant salary isn't a fixed number; it grows and changes throughout your career. Several key factors come into play, and understanding them can help you maximize what you earn. Let's explore what moves the needle on your paycheck.
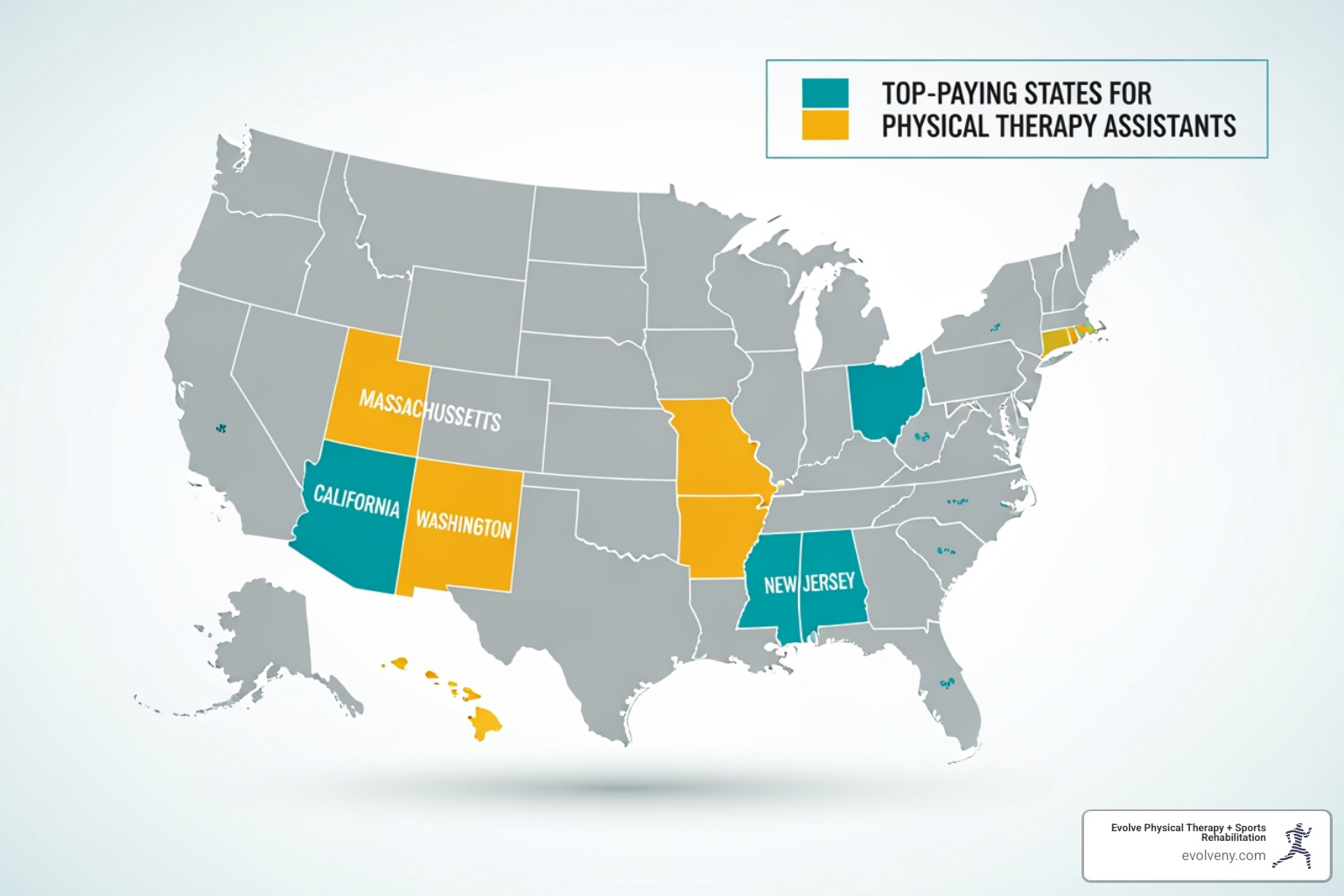
Location: Highest and Lowest Paying States and Cities
Geography can dramatically swing your salary. The highest paying states often have higher costs of living and robust healthcare systems. The District of Columbia leads at $73,146 annually, followed by California ($72,868), Massachusetts ($71,897), Washington ($71,633), and New Jersey ($71,606). These figures reflect regional economics and demand for specialized pediatric care.
Zooming in on cities, San Jose, California, is the highest paying city for Pediatric PTAs, with an average salary of $83,326 per year. This is well above the national average, though it comes with a higher cost of living.
In the New York area—particularly in Brooklyn neighborhoods like Marine Park, Gravesend, and Park Slope—the salary landscape is competitive. Physical Therapist Assistants in New York earn an average of $72,698 annually, reflecting high demand in metropolitan areas. While the cost of living is higher, so is the compensation.
On the other end, states like Mississippi ($59,062) and Arkansas ($59,830) have lower salary averages, which is often balanced by a lower cost of living. The choice between a higher salary in an expensive city and a more affordable area depends on your personal priorities.
Experience Level
As in most professions, experience pays. An entry-level Pediatric PTA with less than a year of experience can expect to earn about 13% below the median while building foundational skills. As you gain experience over your first few years, your earnings will climb toward the national average.
Mid-career PTAs (five to nine years) typically reach or exceed the median salary, reflecting their growing expertise and independence. Experienced professionals with over a decade of practice are highly valued for their deep knowledge and mentorship capabilities, with those in their late career (20+ years) earning as much as 14% above the median.
This progression highlights the financial rewards of dedication and continuing education. Pursuing opportunities like APTA's Advanced Proficiency Pathways can accelerate this growth and boost your earning potential.
Work Setting
The environment where you practice also affects your paycheck. Different settings come with different demands and pay scales.
Home healthcare services top the salary charts at $77,540 annually, reflecting the autonomy and travel involved. Nursing care facilities follow at $75,800, due to the complexity of patient needs. Other common settings include:
- Hospitals: Median salary of $66,300, aligning with the national average.
- Offices of physicians: Around $62,170.
- Offices of physical, occupational, and speech therapists: Average of $61,620.
Pediatric PTAs may also work in children's hospitals, specialized rehabilitation centers, or private clinics like ours at Evolve Physical Therapy. School-based physical therapy is another significant and rewarding setting, where you help children participate fully in their education. You can explore more about the diverse environments where kids physical therapy takes place and how each setting brings its own rewards.
The Role and Responsibilities of a Pediatric PTA
Working as a Pediatric Physical Therapy Assistant means helping patients from infancy through adolescence. It requires not just technical skills but a deep understanding of child development. As a Pediatric PTA, you work under a licensed physical therapist to bring their treatment plan to life, guiding children through therapeutic exercises designed to improve strength, balance, and mobility. A key part of the role is making therapy feel like play, so children are healing while having fun.
Your responsibilities extend beyond direct therapy. You will carefully document patient progress, providing crucial feedback to the supervising physical therapist to refine the care plan. You also act as a coach for families, teaching them how to continue exercises at home to support their child's development between sessions. This collaboration is vital for a child's success. To learn more about how this therapy transforms young lives, see our guide on Pediatric and Adolescent Physical Therapy.
Primary Duties and Work Environment

No two days are the same for a Pediatric PTA. Your hands-on work includes massage, stretching, and guiding children through exercises disguised as fun activities—like turning balance beam walks into adventure games. You'll use specialized equipment like balance balls, adaptive bikes, and resistance bands to help children achieve treatment goals while staying motivated.
Throughout each session, you'll assess the child's response, noting improvements in coordination, balance, and strength. This ongoing observation provides the physical therapist with detailed feedback to shape the treatment plan. Strong communication is woven into everything you do, from updating the supervising PT to educating families on injury prevention and home exercises.
Your work setting—whether an outpatient clinic like Evolve Physical Therapy, a hospital, a school, or a home health environment—shapes your daily experience. Regardless of the setting, expect to be active, spending most of your day on your feet. The physical demands are real, but so are the rewards. Explore our collection on kids physical therapy settings to see these diverse environments.
Essential Skills and Qualities
Technical training is the foundation, but certain personal qualities are essential for success as a Pediatric PTA. Thriving in this role requires a unique blend of traits.
Compassion is at the heart of the job, helping you connect with children and families during challenging times. Patience is vital, as progress happens at each child's own pace. The role demands physical stamina for active, often floor-based, therapy sessions. Strong interpersonal skills are needed to build trust with children, communicate clearly with parents, and collaborate with other healthcare professionals. Finally, attention to detail ensures accurate progress tracking, while the ability to communicate with children through play and simple instructions makes therapy effective and engaging. These qualities, combined with your training, allow you to make a real difference while building a career with a solid pediatric physical therapy assistant salary.
How to Become a Pediatric PTA and Increase Your Salary
Starting on a career as a Pediatric Physical Therapy Assistant is a well-defined journey that blends a passion for helping children with a rewarding profession. Once you're licensed, numerous opportunities exist for growth and a higher salary.
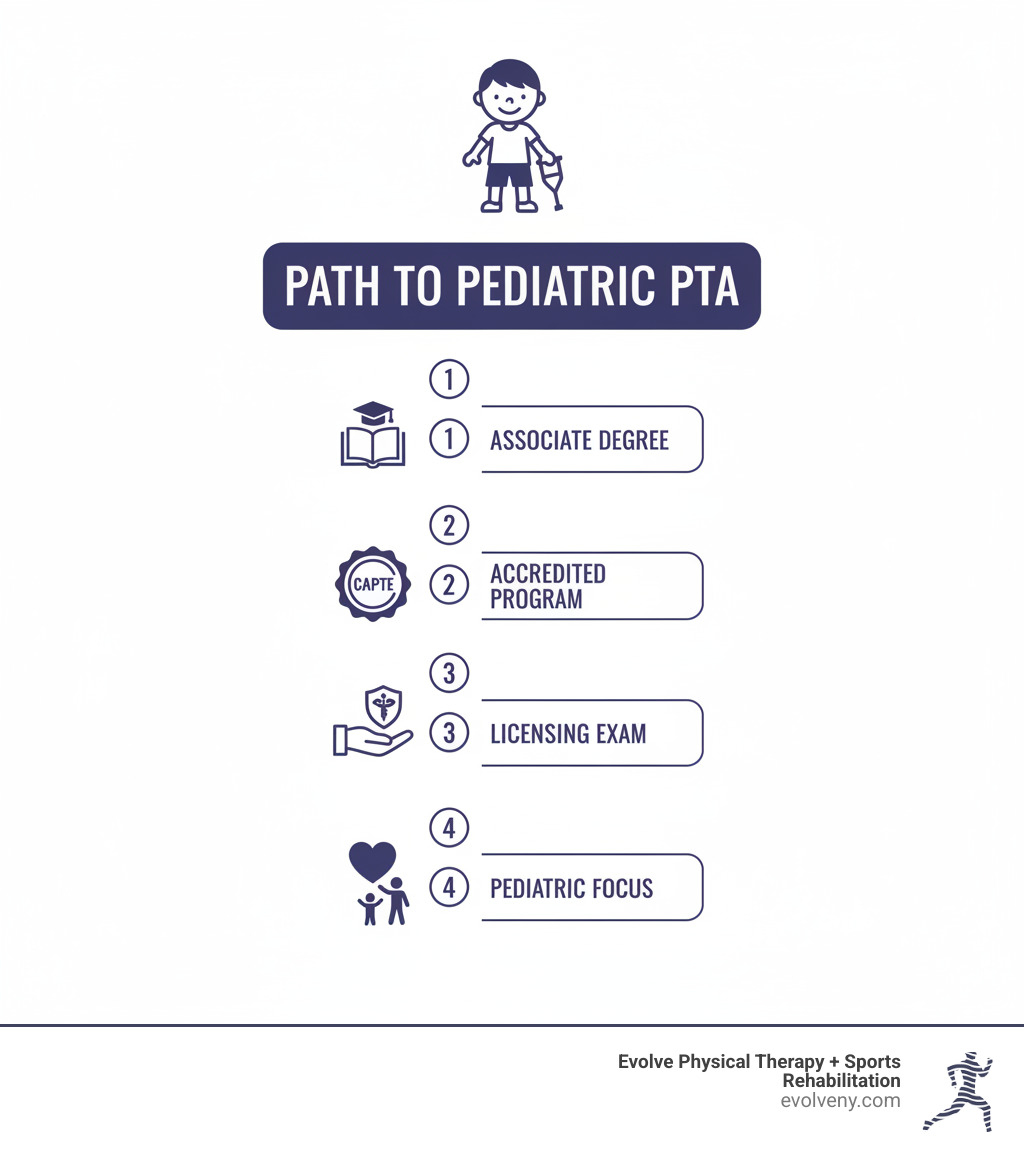
Educational and Licensure Requirements
The path to becoming a licensed Physical Therapy Assistant (PTA) is designed to ensure you are fully prepared to provide excellent care. The process involves several key steps:
- Complete an associate degree. You'll need to graduate from a two-year PTA program. It's crucial that the program is accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE). You can find a list of accredited programs on the CAPTE online website.
- Pass the national exam. After earning your degree, you must pass the National Physical Therapy Exam (NPTE), a comprehensive test of your knowledge and skills. More information is available here: NPTE details.
- Obtain state licensure. All states require PTAs to be licensed or certified. This final step typically involves a background check and may include an exam on state-specific laws.
- Pursue continuing education. To maintain your license and keep your skills sharp, most states require ongoing continuing education throughout your career.
How to Increase Your Earning Potential
Once you are a licensed Pediatric PTA, you can take several strategic steps to boost your pediatric physical therapy assistant salary and advance your career.
- Pursue advanced proficiency. The American Physical Therapy Association (APTA) offers Advanced Proficiency Pathways in areas like pediatrics. Earning this recognition requires significant work experience and demonstrates a high level of skill, which can lead to better-paying jobs.
- Gain experience in high-paying settings. As noted earlier, settings like home healthcare and nursing care facilities often offer higher salaries. Gaining experience in these environments can boost your overall earning potential.
- Consider travel PTA roles. If you are flexible, working as a travel PTA can lead to significantly higher earnings, sometimes over $105,140 a year, often with added perks like housing stipends.
- Master salary negotiation. Researching local salary benchmarks—including in competitive markets like our Brooklyn neighborhoods—and confidently articulating your value can often result in a better starting offer.
- Earn additional certifications. Obtaining certifications in areas like CPR, Basic Life Support (BLS), or specialized pediatric techniques makes you a more desirable candidate and can translate to a higher salary.
Job Outlook and Typical Benefits for a Pediatric PTA
If you're considering a career as a Pediatric PTA, the future is bright. The field offers exceptional growth and stability, making it a secure professional choice.
Employment for physical therapist assistants is projected to grow by 22% from 2024 to 2034, much faster than the average for all occupations, according to the U.S. Bureau of Labor Statistics. This translates to approximately 26,400 job openings each year, creating abundant opportunities for qualified professionals.
This remarkable growth is driven by several factors. While an aging population increases overall demand for physical therapy, the pediatric specialty is uniquely fueled by advancements in medical technology. These innovations help children with complex physical disabilities and developmental challenges thrive, creating a strong need for skilled Pediatric PTAs. This robust outlook means strong job security and a wide variety of career options, whether in a clinic like Evolve Physical Therapy, a hospital, or a school system.
Common Benefits Offered
Your total compensation is more than just your salary. The benefits you receive significantly improve your financial well-being and quality of life. Most full-time employers offer comprehensive packages to attract and retain talented PTAs.
When evaluating job offers, look beyond the pediatric physical therapy assistant salary at the complete benefits package. Common offerings include:
- Healthcare Coverage: Medical, dental, and vision insurance for you and your family.
- Retirement Plans: 401(k) plans, often with employer matching contributions, or pension plans to help you save for the future.
- Paid Time Off (PTO): Vacation days, sick leave, and paid holidays to support a healthy work-life balance.
- Disability Insurance: Short-term and long-term coverage provides a financial safety net in case of illness or injury.
- Continuing Education Reimbursement: Many employers help cover the cost of courses and certifications required to maintain your license and advance your skills.
A slightly lower base salary with exceptional benefits may offer better overall value than a higher salary with minimal perks. Calculating the true worth of these benefits is key to making the best career decision.
Conclusion
Choosing to become a Pediatric Physical Therapy Assistant is a rewarding decision, blending meaningful work with a strong financial outlook. The pediatric physical therapy assistant salary is competitive, averaging around $66,064 annually, with a projected job growth of 22% ensuring long-term career stability.
Your earning potential is not static; it can be maximized by choosing a strategic location, gaining experience, and pursuing specializations. Paired with comprehensive benefits, this career offers a complete and satisfying professional life.
At Evolve Physical Therapy + Sports Rehabilitation, our holistic philosophy values the dedicated professionals who make a real difference in children's lives. We understand the expertise and compassion required to help young patients move better, grow stronger, and thrive. If you're seeking expert pediatric care in a supportive environment, we invite you to explore our pediatric physical therapy services in Brooklyn. Whether you're a family needing support or a professional exploring this path, we're here to help you move forward.
Strain-Counterstrain: Is This Therapy Your Path to Pain Relief?
Understanding Strain-Counterstrain: A Gentle Path to Pain Relief

Strain counterstrain exercises are not exercises you perform yourself—they're a specialized manual therapy technique where a trained physical therapist gently positions your body to release painful tender points and restore normal muscle function.
Quick Answer: What You Need to Know
- It's a passive technique - The therapist does the work, you relax
- How it works - Therapist finds tender points, positions you for comfort, holds 90 seconds
- What it treats - Neck pain, back pain, headaches, joint stiffness, muscle spasms
- Why it's different - Moves away from pain, not into it
- Who benefits - Anyone seeking gentle, non-forceful pain relief
Developed by osteopath Dr. Lawrence Jones in 1955, Strain-Counterstrain (SCS) is a gentle osteopathic manual therapy. Unlike traditional stretching, it works by positioning your body into a state of ease—where pain decreases—and holding it for about 90 seconds. This allows tight muscles to "reset" their neuromuscular reflexes, providing relief without force. The technique is so gentle it can be used on nearly any patient, from infants to the elderly, helping manage pain quickly without medication.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. For nearly two decades, I've used strain counterstrain exercises in treatment plans for patients with chronic and complex pain who need gentle, effective relief. This guide will explore how the technique works, who it helps, and its role in a full rehabilitation program.
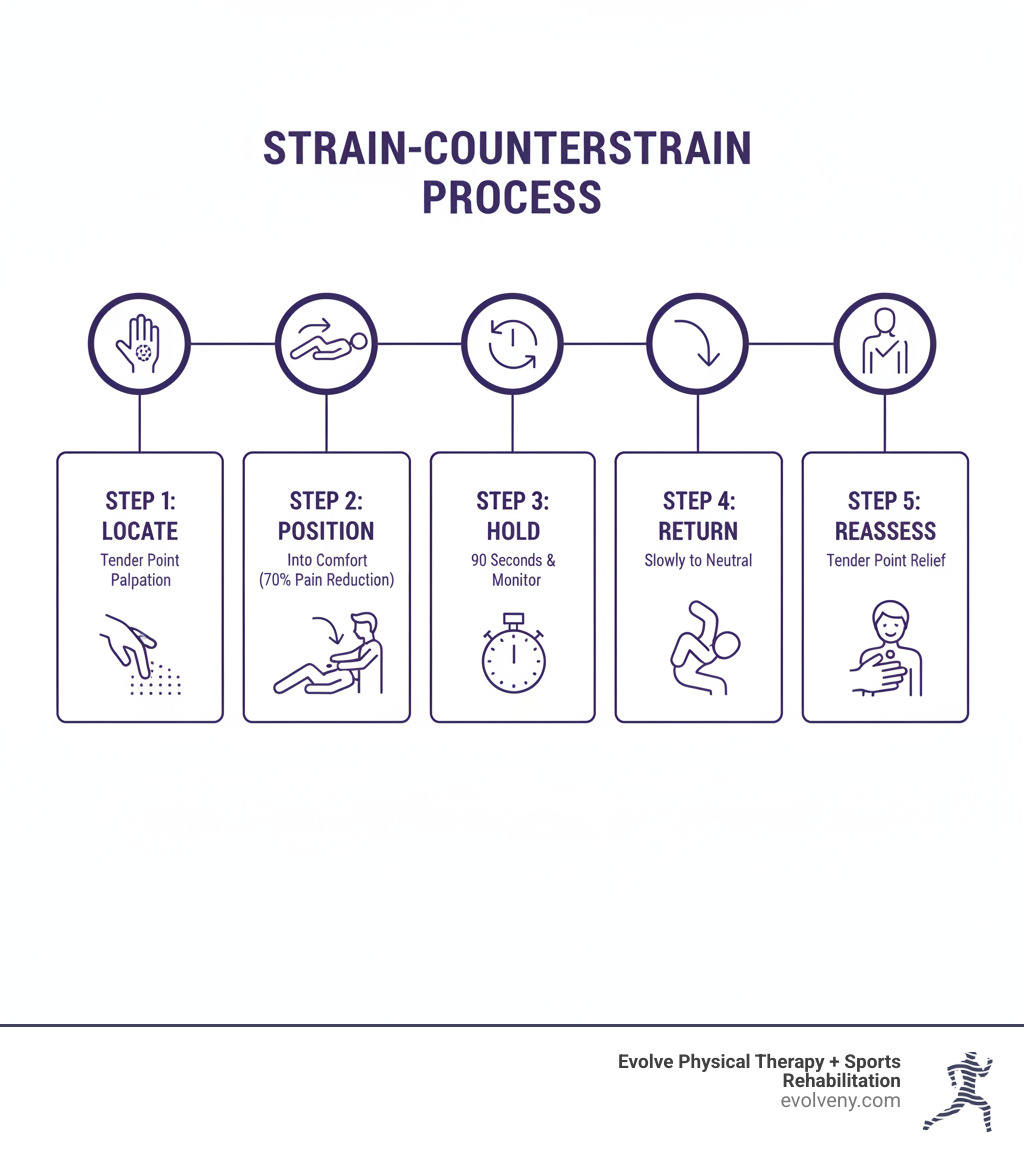
Decoding Strain-Counterstrain: What It Is and How It Works
If you've ever wondered how a technique so gentle could be so effective, the story behind Strain-Counterstrain is fascinating—and it explains why it's such a valuable tool in our Brooklyn practice.
Strain-Counterstrain has a serendipitous origin. In 1955, osteopathic physician Dr. Lawrence Jones made an accidental findy. While treating a patient with severe, persistent low back pain, he spent 20 minutes searching for a position of comfort. After finding one and letting the patient rest in it, he was stunned to find the man's pain had vanished upon standing up.
This became the foundation of Strain-Counterstrain, a cornerstone of osteopathic manipulative treatment (OMT). Dr. Jones realized that by moving a painful body part away from the barrier of pain and into comfort, he could release persistent muscle spasms. This gentle approach offers a different philosophy than the "no pain, no gain" mentality.
The beauty of SCS lies in its counterintuitive approach. Instead of stretching a tight muscle, we gently shorten it even further. This tells the nervous system that it's safe to release its protective hold. That's why strain counterstrain exercises feel so different—there's no force, just gentle positioning that allows your body to reset itself.
At Evolve Physical Therapy, we use SCS as part of our comprehensive manual therapy approach because it respects your body's natural healing processes. To learn more about how we combine hands-on techniques, visit our Manual Therapy Brooklyn page.
Here's how Strain-Counterstrain compares to other gentle manual therapy techniques:
| Technique | Description | Patient Involvement | Force Level | Primary Goal |
|---|---|---|---|---|
| Strain-Counterstrain | Indirect technique involving passive positioning into comfort to release tender points. | Passive | Very Gentle | Reset neuromuscular reflexes, reduce muscle spasm and pain. |
| Soft Tissue Therapy | Broad term for hands-on techniques (e.g., massage, myofascial release) to relax muscles, improve circulation, and reduce pain. | Passive | Gentle to Moderate | Improve tissue extensibility, reduce tension. |
| Therapeutic Exercise | Guided movements and activities designed to restore strength, flexibility, balance, and endurance. | Active | Variable | Improve function, prevent re-injury, build resilience. |
The Science Behind the Gentleness: Proposed Mechanisms
How can something so gentle create real change? The answer lies in your nervous system.
The most accepted explanation is the Proprioceptive Theory. When a muscle is strained, sensory organs called muscle spindles fire off alarm signals, locking the muscle into a protective, tight state. This creates a painful tender point. Sometimes, these spindles get stuck in "alarm mode," creating a faulty nerve reflex (aberrant neuromuscular reflex arc) that keeps the muscle chronically tight and painful, much like a car alarm that won't turn off.
SCS works by passively shortening the affected muscle, which silences the overactive muscle spindles. This allows the nervous system to reset the faulty reflex, calming the muscle. By addressing this root neurological issue, we reduce pain signals (nociceptive input). This release of tension also improves circulation, bringing oxygen to the tissue and clearing out waste products, which helps with inflammation reduction and promotes natural healing. For more detail, you can explore this scientific research on SCS mechanisms.
How SCS Differs from Other Manual Therapies
Strain-Counterstrain stands out in hands-on therapy for several key reasons.
First, SCS targets tender points, which are different from trigger points. Tender points are small, localized spots of pain that do not refer pain elsewhere when pressed. Trigger points, often found in tight muscle bands, cause pain to radiate to other areas.
Second, SCS is a completely passive technique. You relax while the therapist does all the work, unlike active techniques where you contract muscles against resistance.
The gentleness of SCS gives it an excellent safety profile. We move your body away from pain, not into it, making the treatment comfortable. There is no forceful pushing or "working through the pain," which makes it ideal for acute injuries or patients who can't tolerate aggressive therapies.
Finally, SCS is an indirect technique. Instead of pushing into a restriction, we move the body into a position of ease, away from the painful barrier. This different philosophy is often effective when direct approaches have failed. At Evolve Physical Therapy, our therapists select the best technique for your needs from a range of options. Learn more on our Soft Tissue Therapy Brooklyn page.
Who Can Benefit from Strain-Counterstrain?
Because SCS is so gentle, almost anyone experiencing pain can benefit. It's particularly effective for somatic dysfunction—when your muscles, joints, and connective tissues aren't working correctly. This includes hypertonic muscles (stuck in a state of tension) or joint restrictions that make movement painful.
At Evolve Physical Therapy, we've used this therapy on everyone from young athletes to grandparents with arthritis. We believe in finding the gentlest effective solution for your unique situation. For comprehensive strategies, explore our Pain Management Physical Therapy services.
Conditions Effectively Treated by SCS
The versatility of strain counterstrain exercises allows us to treat a wide range of conditions in our Brooklyn practice.
- Neck pain: SCS can reset tight neck muscles, whether the pain is from poor posture, sleeping wrong, or an injury.
- Low back pain: SCS releases deep muscle spasms that cause chronic low back pain, often leading to immediate mobility improvements.
- Headaches: By releasing tight neck and upper back muscles, SCS can address the root cause of tension and cervicogenic headaches.
- Sciatica: SCS can ease sciatica by reducing muscle spasms in the low back and pelvis that pressure the sciatic nerve.
- Arthritis: While not a cure, SCS improves quality of life by relaxing muscles around painful joints, reducing pain and increasing mobility.
- Tendinitis: SCS helps break the pain cycle of tendinitis by relaxing the protective muscle tightening around inflamed tendons. Learn more at Physical Therapy for Tendonitis Brooklyn.
- Other Conditions: The gentle positioning of SCS can also benefit conditions like plantar fasciitis, post-operative pain, and fibromyalgia.
Are You an Ideal Candidate for This Gentle Therapy?
One of the best things about SCS is its safety and suitability for a wide range of people.
We particularly recommend SCS for:
- Acute injuries: When an injury is fresh and highly sensitive, SCS provides relief without aggravating the tissue.
- Chronic pain sufferers: SCS can break the stubborn cycle of muscle tension, especially when other therapies have failed. Visit our Chronic Pain Physical Therapy Brooklyn page to learn more.
- Low pain tolerance: If you find other therapies too intense, you'll appreciate how SCS works with your comfort level, not against it.
- Sensitive populations: Post-surgical patients, elderly patients with osteoporosis, and even infants with torticollis benefit from SCS because it is non-forceful and safe for healing tissues or fragile bones.
However, a thorough assessment is crucial. Contraindications include unstable fractures, complete ligament tears, or severe acute illness. We proceed with extra caution for conditions like severe osteoporosis or ligamentous instability. Your consent and feedback are always essential for a safe and successful treatment.
What to Expect: The Strain Counterstrain Exercises and Treatment Process
Strain counterstrain exercises are not exercises you do yourself. SCS is a passive technique where your physical therapist performs all the work. Your role is simply to relax and provide feedback. While active exercises are part of a complete recovery plan, the SCS portion involves your therapist skillfully positioning you to release over 200 documented tender points in the body. Each point requires a specific position, held for 90 seconds, to allow your nervous system to reset.

The Key Steps of a Treatment Session
An SCS session at our Brooklyn clinic is methodical, gentle, and relaxing.
Step 1: Find the Tender Point Your therapist uses gentle palpation to locate a specific, hypersensitive tender point. Using very light pressure, we'll ask you to rate the tenderness on a 0-10 scale to establish a baseline for treatment.
Step 2: Position of Comfort We gently move your body into a "position of ease," shortening the muscle associated with the tender point. While monitoring the point, we search for a position that reduces tenderness by at least 70%. The position should feel comfortable and provide immediate relief.
Step 3: Hold for 90 Seconds We hold this position of comfort for 90 seconds. This specific duration allows your neuromuscular system time to reset. During this hold, you can relax as your therapist feels the tissue soften and release.
Step 4: Slow, Passive Return to Neutral After the hold, we slowly and passively guide your body back to a neutral position. This gradual return is crucial to prevent the muscle from re-tensing.
Step 5: Re-assessment of the Tender Point We re-check the tender point. You will likely notice a significant reduction in pain and an improvement in tissue texture. Many patients experience an immediate increase in their range of motion. This five-step process is a precise, systematic approach to pain relief. If you're curious about how this fits into the broader landscape of physical therapy, we've written a helpful overview at what is Physical Therapy.
Integrating Strain Counterstrain Exercises with Your Physical Therapy Plan
SCS is rarely a standalone treatment. At Evolve Physical Therapy, we see it as a powerful tool to prepare the body for active rehabilitation. By first reducing pain and releasing muscle guarding with SCS, we create a stable foundation for strengthening and mobility work.
Research supports this combined approach, showing that SCS paired with exercises yields significantly better results for conditions like chronic low back pain. We integrate SCS with other manual therapies like Instrument-Assisted Soft Tissue Mobilization (IASTM) and targeted therapeutic exercises. A typical plan starts with SCS to reduce pain, followed by exercises to build stability and mobility, ensuring a comprehensive and lasting recovery. To learn more about how we incorporate active exercise into your recovery, visit our Therapeutic Exercise Brooklyn page.
The Evidence and Advanced Applications of Strain-Counterstrain
At Evolve Physical Therapy, we believe in understanding the evidence behind our treatments. Strain-Counterstrain has been practiced for over half a century, and the clinical evidence for its effectiveness in providing pain reduction and improved range of motion continues to grow.
Research, including a systematic review, confirms that SCS is effective in reducing tender point pain and shows positive outcomes for neck and low back pain, often with immediate relief. You can explore the research landscape further in A systematic review on SCS effectiveness.
While clinical experience strongly supports its use, we acknowledge the research limitations. Like many manual therapies, creating high-quality, large-scale sham-controlled trials is challenging. Therefore, there is a need for more studies to fully validate its long-term efficacy across all conditions. For more on the science, check out this scientific research on SCS mechanisms.
Beyond the Muscles: Advanced Strain Counterstrain Applications
While many associate strain counterstrain exercises with muscles and joints, advanced applications reflect our holistic approach to healing at Evolve Physical Therapy. These techniques address tissues controlled by the autonomic nervous system, such as blood vessels, organs, and lymphatic pathways.
- Vascular SCS: Can improve circulation by releasing tension around blood vessels, helping with certain types of headaches.
- Visceral SCS: Targets restrictions around internal organs to help with GI issues, respiratory challenges, and other internal dysfunctions.
- Lymphatic SCS: Works to release restrictions in the lymphatic system to help manage lymphedema, reduce swelling, and support immune function.
- Disc SCS: Can provide relief for conditions like herniated discs and sciatica by reducing tension around the affected spinal disc.
These advanced applications demonstrate the potential of SCS to influence your body's complex systems, contributing to overall health. To learn more about how we integrate various therapies for comprehensive health, visit our Physical Therapy and Wellness page.
Frequently Asked Questions about Strain-Counterstrain
At Evolve Physical Therapy in Brooklyn, we want you to feel informed and comfortable. Here are answers to common questions about strain counterstrain exercises.
Is Strain-Counterstrain painful?
No. The entire technique is designed to be gentle and relaxing. We move your body into positions of comfort where pain decreases. While locating the tender point may cause momentary discomfort, the treatment itself is pain-free. Many patients find it so relaxing they feel their muscles "melt" or even doze off. Your comfort is our priority, and we encourage you to speak up if anything feels uncomfortable.
How many sessions will I need?
The number of sessions depends on your condition. Acute injuries often see significant improvement in just 1-3 sessions. Chronic conditions that have persisted for months or years typically require more sessions, often 6-10 or more, as part of a comprehensive plan that includes strengthening and mobility work. During your initial evaluation, we will provide a personalized treatment plan and timeline.
Can I perform Strain-Counterstrain on myself?
No. While the DIY spirit is admirable, SCS requires a trained professional. Identifying the precise location of over 200 tender points and finding the exact three-dimensional position of comfort requires extensive anatomical knowledge and skilled palpation. A therapist must feel subtle tissue changes while positioning you, which is impossible to do on yourself. Attempting to self-treat is ineffective and could potentially cause strain. It's a technique best left to a trained therapist to ensure it is performed safely and effectively.
Conclusion: Your Next Step Towards a Pain-Free Life
We've explored strain counterstrain exercises—a technique less about "exercise" and more about your body finding its own path to comfort. The core principle is simple: by holding a position of ease for 90 seconds, we can reset the nerve reflexes that cause pain. This gentle, safe, and non-pharmacological approach is effective for a vast range of conditions, from acute neck pain to chronic fibromyalgia.
Understanding that healing can come from ease, not force, is empowering. At Evolve Physical Therapy in Brooklyn, our hands-on philosophy is built on this principle. We create comprehensive plans that combine SCS with strengthening and other therapies to achieve lasting change, not just temporary relief. Our compassionate, evidence-based care, featured on NBC News, is custom to your unique needs.
You don't have to live with pain or limited mobility. A path forward exists, and it begins with reaching out. Take control of your pain with expert Manual Physical Therapy in Brooklyn. Let's work together to help you move better, feel better, and live the vibrant, pain-free life you deserve.
No More Tumbles! Best Fall Prevention Workshops for Older Adults
Why Fall Prevention Workshops Are Critical for Active Adults

Fall prevention workshops are educational programs that teach older adults how to reduce their fall risk through exercise, home safety, and lifestyle changes. Typically running 6-8 weeks, these workshops are led by health professionals who guide participants through balance training, strength exercises, and practical strategies.
Quick Overview: What You Need to Know About Fall Prevention Workshops
- Who Should Attend: Adults 60+ who have fallen, fear falling, or want to stay independent
- What You'll Learn: Balance exercises, home safety tips, medication management, proper footwear
- Where to Find Them: Senior centers, hospitals, Area Agencies on Aging, physical therapy clinics
- Cost: Many programs are free or low-cost; some accept insurance
- Format: Group classes (10-20 people) meeting weekly for 1-2 hours
- Evidence-Based Programs: Look for workshops backed by research and proven results
The statistics are sobering: one in four adults over 65 falls every year. But the good news is that most falls are preventable. The key is taking action before a fall happens. A fall can create a dangerous cycle: fear of falling leads to less activity, which causes weakness and makes another fall more likely. Fall prevention workshops break this cycle by building strength, improving balance, and restoring confidence.
These workshops address specific risk factors, from medication side effects to poor home lighting. As Lou Ezrick, founder of Evolve Physical Therapy, I've seen how proactive, evidence-based programs help people regain independence and reduce fall risk while maintaining the active lifestyles they love.

Understanding Your Key Risk Factors for Falls
Falls rarely happen out of nowhere; they usually result from a combination of manageable factors. Understanding your personal risk factors is the first step toward prevention.
Your Body Changes as You Age
As we age, our bodies undergo changes that affect stability. Sarcopenia, the gradual loss of muscle mass, weakens the leg muscles that prevent stumbles from becoming falls. Many older adults also experience balance problems from changes in the inner ear or nervous system. Vision and hearing changes also play a big role. Conditions like cataracts or glaucoma make it harder to spot obstacles, while reduced hearing can affect your spatial orientation. Chronic conditions like arthritis, diabetes, and Parkinson's disease all impact mobility and increase fall risk. For example, diabetes can cause neuropathy, or numbness in the feet, making it hard to feel the ground.
The Choices You Make Every Day
Daily habits significantly influence fall risk. The most dangerous behavior is inactivity. Fearing a fall, many people reduce their activity, which worsens muscle weakness and balance, creating a vicious cycle. Your footwear also matters. Shoes with slippery soles, poor support, or an improper fit are common culprits. Even moderate alcohol consumption can impair balance and judgment.
Hidden Dangers in Your Home
Your home can be full of environmental hazards. Throw rugs are a primary offender, as they easily slip or bunch up. Clutter, such as items on the floor or cords across walkways, creates trip hazards. Poor lighting in staircases and hallways can hide obstacles, and uneven surfaces like the transition from carpet to tile can catch your foot. Bathrooms are particularly dangerous due to wet, hard surfaces, making grab bars essential.
When Your Medications Work Against You
Taking multiple medications (polypharmacy) can increase fall risk due to medication side effects. Many common drugs cause dizziness, drowsiness, or a sudden drop in blood pressure upon standing (orthostatic hypotension).
Common medications that can increase fall risk:
- Antidepressants
- Blood pressure medications (antihypertensives)
- Sedatives and tranquilizers
- Antipsychotics
- Diuretics (water pills)
- Opioid pain relievers
- Antihistamines (especially older types)
- Muscle relaxants
This doesn't mean you should stop your medication. Instead, talk to your doctor or pharmacist. They can review your full list and may be able to adjust dosages or suggest alternatives to reduce your risk.
Assessing Your Personal Fall Risk
How do you know if you're at risk? Have you fallen in the past year, do you feel unsteady, or do you worry about falling? Do you take four or more medications or have chronic conditions affecting your movement? If you answered yes to any of these, it's time to talk to your doctor. They can review your fall history, conduct an assessment, and refer you to resources like fall prevention workshops or physical therapy. Addressing these risk factors before a fall is always the best strategy.
What You'll Gain from a Fall Prevention Workshop

When you join a fall prevention workshop, you're investing in a fuller, more confident life. Many participants walk in nervous and leave weeks later standing taller and moving with purpose.
The physical changes are measurable. Your balance and coordination will improve through targeted, progressive exercises. Your legs will get stronger through lower body strength training, combating age-related muscle loss (sarcopenia). You'll also gain improved flexibility, making everyday movements safer.
The emotional change is often just as powerful. As your body grows stronger, your confidence soars, and the reduced fear of falling is life-changing. Fear can be more limiting than physical weakness, but workshops break this cycle by giving you the physical and mental tools to feel secure. You'll also find social connection by learning alongside peers who share similar goals, which boosts motivation and well-being.
Core Skills Taught in Workshops
Fall prevention workshops provide a complete toolkit of practical skills.
Balance training exercises form the foundation. You'll progress from simple seated movements to more challenging ones like single-leg stands and heel-to-toe walking, improving both static and dynamic balance.
Strength and resistance training focuses on the leg, core, and back muscles that keep you stable, using body weight, resistance bands, or light weights.
Home safety modifications teach you to identify and remove hazards. You'll learn to eliminate clutter and throw rugs, improve lighting, and organize your space to keep items within easy reach.
Medication management is another key component. Experts like pharmacists may visit to explain how certain drugs increase fall risk and what questions to ask your doctor.
Proper footwear selection is crucial. You'll learn to choose shoes with non-slip soles, a proper fit, and adequate support.
You'll also learn how to get up safely from a fall. Knowing how to recover reduces both injury risk and panic. Some workshops also cover topics like nutrition for bone strength and foot health. This holistic approach gives you research-backed skills you can use immediately.
Exploring Different Types of Fall Prevention Workshops
When you start looking for fall prevention workshops, you'll find several options, allowing you to choose a program that fits your needs.
Community-based programs are often the most accessible, held at senior centers, YMCAs, or community halls. Many are free or low-cost and focus on group exercise and social connection.
Hospital or clinic-based programs, like those offered by healthcare providers such as Evolve Physical Therapy, integrate medical expertise. These may involve a multi-disciplinary team of physical and occupational therapists and might require a physician's referral.
Online virtual workshops have grown in popularity, offering convenience for those with mobility challenges or who live in remote areas. You can participate from home while still receiving expert instruction.
Workshops can also be peer-led by trained volunteers or professionally-led by credentialed healthcare professionals. Professionally-led programs typically offer deeper clinical expertise, which is beneficial if you have complex health conditions.
Evidence-Based Programs: The Gold Standard
You'll often hear the term "evidence-based"—this is your best indicator of a quality fall prevention workshop. It means the program is grounded in scientific research and has been proven to reduce falls.
Evidence-based programs use standardized curricula to ensure all essential components are covered. Instructors are required to have specific training, so you're getting proven interventions from qualified professionals. Research shows that a holistic, multi-faceted approach is most effective, which is why these programs integrate exercise, education, home modifications, and medication reviews. At Evolve Physical Therapy, we build our practice around evidence-based methods, like our Rock Steady Boxing program for Parkinson's patients, which was featured on NBC News. We believe in using scientifically validated approaches to improve lives and reduce fall risk.
What to Expect in a Typical Workshop
A typical fall prevention workshop is a supportive, interactive experience.
Most workshops are small groups of 10 to 20 participants, creating a sense of community. In terms of time commitment, programs usually run for 6 to 8 weeks, with sessions lasting 1 to 2 hours once or twice a week. Consistency is key to building new habits.
Workshops are highly interactive, involving hands-on practice of exercises and group discussions. Many programs also bring in guest experts, like pharmacists or vision specialists, to cover specialized topics. You'll be encouraged to set personal goals, tailoring the experience to your needs and giving you concrete targets to work toward. The atmosphere is warm, supportive, and focused on helping you feel stronger and more confident.
How to Find and Join a Program Near You

Finding a fall prevention workshop is easier than you think. Several community resources can point you in the right direction.
Your Local Area Agency on Aging (AAA) is an excellent starting point, as they specialize in services for older adults. Your neighborhood senior center is another great resource, as many workshops are held there. Also, check with your local health department and nearby hospitals or medical centers, which often run or sponsor fall prevention initiatives.
For online searches, many regions have online search directories on websites for public health or aging resources. And of course, we at Evolve Physical Therapy are always happy to guide you. With locations across Brooklyn—including Marine Park, Gravesend, and Park Slope—we can help you find the right resources, whether it's our one-on-one physical therapy or a quality workshop in your neighborhood.
Navigating Eligibility and Costs for Fall Prevention Workshops
Most workshops are designed for adults 60 or 65 and older who are living independently. There may be basic mobility requirements, such as being able to walk a short distance without assistance, to ensure safe participation. If you're unsure about your eligibility, just ask the program coordinator.
The good news is that many fall prevention workshops are free, especially those that are publicly funded. Some may charge a small fee for materials, but scholarships are often available if cost is a concern. While group workshops may not be directly covered by insurance, related services like physical therapy for balance improvement often are. At Evolve Physical Therapy, we work with various insurance providers, including TriCare, and can help you understand your benefits.
Key Questions to Ask Before Registering for Fall Prevention Workshops
Before you sign up, ask a few key questions to ensure a program is the right fit.
- Instructor's qualifications: Are they a certified leader, physical therapist, or nurse?
- Is the program evidence-based? This ensures the methods are proven to work. You can learn about program design from resources like the Canadian Fall Prevention Curriculum.
- Class size: Smaller groups (10-14 people) allow for more personal attention.
- Curriculum: Does it cover a comprehensive range of topics, including exercise, home safety, and medication review?
- Time commitment: Does the schedule fit your life?
- Eligibility and costs: Confirm any age or mobility requirements and all potential fees.
A quality program will welcome your questions and provide thorough answers.
Frequently Asked Questions about Fall Prevention
Let's address some common questions about fall prevention workshops.
I have a fear of falling, but haven't fallen recently. Should I still attend a workshop?
Yes, absolutely. You don't need to wait for a fall to take action. Fear of falling is a risk factor on its own. It can lead you to move less, which causes muscles to weaken and balance to decline, making a fall more likely. Fall prevention workshops are designed to break this cycle by building both physical strength and confidence. Think of it as preventive care for your independence.
How is a workshop different from just going to the gym?
While gym workouts are great for general fitness, fall prevention workshops are more specific. They teach exercises that directly target the muscles and movements that prevent falls, like balance recovery. Workshops also provide crucial education on home safety, medication risks, and proper footwear—topics you won't typically cover at a gym. The group setting with peers and guidance from trained health professionals who understand the needs of older adults also makes the experience unique and highly effective.
How quickly can I expect to see improvements in my balance?
It varies, but most people notice positive changes within a few weeks. You might feel more stable standing up or climbing stairs within the first month. By the six-week mark of a consistent program, measurable improvements in strength and balance are common. The key is consistency. Attending regularly and practicing the exercises will yield the best results. The goal is to build lasting skills that will serve you for years to come.
Conclusion: Take the First Step to a Safer, More Active Life
We know that one in four adults over 65 falls every year, and these falls are a leading cause of injury. But the most important fact is this: most falls are preventable, and you have the power to take control.
This guide has shown how fall prevention workshops build strength, improve balance, and restore confidence. They offer a roadmap to independence by teaching you practical skills, from spotting home hazards to understanding your medications. Perhaps most importantly, they help you build the confidence to live without fear and stay active.
At Evolve Physical Therapy + Sports Rehabilitation, we believe in treating the whole person. As our founder, Lou Ezrick, knows from years of experience, proactive, evidence-based interventions are the most effective. Our commitment is reflected in specialized programs like Rock Steady Boxing for Parkinson's patients (featured on NBC News) and our comprehensive physical therapy services across Brooklyn—from Marine Park to Park Slope.
Physical therapists play a crucial role in fall prevention. We improve core strength, coordination, and proprioception (your body's spatial awareness). We can assess your home for hazards and create a personalized exercise program to target your specific risks.
Don't wait for a fall to happen. Explore the fall prevention workshops in your area, or reach out to us to discuss how physical therapy can address your balance and strength needs. You deserve to live an active, independent, and engaged life. Take the first, most important step today.
Learn how physical therapy for seniors can improve your balance and strength
Personal Training for Sports Performance: Your Ultimate Guide
Why Sports Performance Personal Training is Essential for Athletes at Every Level
Sports performance personal training is specialized coaching designed to improve athletic abilities through targeted programming that improves strength, speed, power, and agility while reducing injury risk. Unlike general fitness, this training focuses on biomechanical analysis, movement optimization, and individualized programming customized to your sport, position, and competitive goals.
Key Differences Between General Personal Training and Sports Performance Training:
| Aspect | General Personal Training | Sports Performance Training |
|---|---|---|
| Primary Goal | Overall health, weight loss, general fitness | Improved athletic performance, competitive edge |
| Assessment | Basic fitness evaluation | Comprehensive movement screening, sport-specific analysis |
| Programming | General strength and cardio | Periodized, sport-specific power, speed, agility work |
| Focus | Looking good, feeling better | Moving better, performing better, injury prevention |
| Clientele | General population | Athletes from youth to professional, tactical athletes |
The global sports performance market is projected to reach $3.5 billion by 2030, reflecting the growing recognition that greatness is built, not born. Whether you're a weekend warrior, a high school athlete aiming for a scholarship, or a professional seeking a competitive edge, sports performance training offers a science-backed pathway to your full potential.
As Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, I've spent nearly two decades helping athletes optimize movement and overcome injuries. My approach combines manual therapy expertise with functional movement training to help active individuals like you maintain peak fitness and prevent recurring injuries.

What is Sports Performance Training and How Does It Differ from General Fitness?
What separates a good athlete from a great one often lies in how they train. Sports performance personal training is specialized coaching that goes far beyond a standard gym workout. Instead of just getting you "in shape," it's laser-focused on making you better at your specific sport.
Think of it this way: general fitness is like learning to drive a car, while sports performance personal training is like racing school—it teaches you to handle every curve and maximize acceleration. The difference comes down to sport-specific goals, where every exercise has a purpose tied directly to your performance. For a basketball player, we develop vertical jump power; for a runner, we optimize stride efficiency.
Key differentiators include:
- Biomechanical Analysis: We don't just watch you move; we analyze how you move to identify inefficiencies that can limit performance or cause injuries.
- Energy System Development: We train your body to efficiently fuel the specific demands of your sport, whether it's a 100-meter sprint (phosphagen system) or a marathon (aerobic system).
- Movement Pattern Optimization: We break down sport-specific movements, like a pitcher's throw or a soccer player's cut, and rebuild them for maximum efficiency and power.
The fundamental shift is from general health to peak athletic output. General fitness makes you healthier; sports performance training pushes you to your competitive edge safely and strategically.
| Aspect | General Personal Training | Sports Performance Training |
|---|---|---|
| Primary Goal | Overall health, weight loss, general fitness | Improved athletic performance, competitive edge |
| Assessment | Basic fitness evaluation | Comprehensive movement screening, sport-specific analysis |
| Programming | General strength and cardio | Periodized, sport-specific power, speed, agility work |
| Focus | Looking good, feeling better | Moving better, performing better, injury prevention |
| Clientele | General population | Athletes from youth to professional, tactical athletes |
The Athlete-Centric Approach
Your training should be as unique as you are. At Evolve Physical Therapy + Sports Rehabilitation, we don't use cookie-cutter programs. Our approach begins with a thorough needs analysis of your strengths, weaknesses, injury history, and goals. This shapes your individualized programming.
Positional demands are critical. A football lineman and a wide receiver require vastly different physical attributes, and their training reflects that. We also adjust for in-season versus off-season training. The off-season is for building foundational strength, while the in-season focuses on maintenance, fatigue management, and peak performance.
We also integrate mental conditioning. Physical ability is only part of the equation. We help you build focus, manage pressure, and develop the mental resilience needed to excel. The NSCA discusses how specific coping skills can improve performance under pressure, a key component of our training.
Who Can Benefit from This Specialized Training?
If you compete or push your body athletically, this training can help you perform better and safer. It's for:
- Youth athletes: Building a proper athletic foundation prevents injuries and creates healthy lifelong habits.
- High school athletes: Gaining a competitive edge for varsity spots or college scholarships through targeted speed, power, and agility training.
- Collegiate athletes: Withstanding the intense physical demands of a longer, more competitive season.
- Professional athletes: Refining technique, extending careers, and finding that critical advantage.
- Adult recreational athletes: Improving performance and staying injury-free in triathlons, golf, or competitive leagues.
- Tactical athletes: For first responders and military personnel, physical readiness is about job performance and saving lives.
The Core Components of a Sports Performance Personal Training Program
A comprehensive sports performance personal training program builds a body that's not just strong but also resilient, explosive, and capable of handling the demands of your sport. We address every piece of the performance puzzle.

Building a Foundation: Strength, Power, and Endurance
A solid athletic foundation starts here. We use smart principles like progressive overload and periodization to build functional strength. The Wall Street Journal highlights exercises that maximize leg strength and balance.
- Power development teaches your body to use strength explosively. We incorporate Olympic lifts and medicine ball throws to train your muscles to generate maximum force in minimum time.
- Plyometrics, such as box jumps and bounding drills, are highly effective for building explosive power. Even beginners can safely incorporate these exercises.
- Endurance conditioning is custom to your sport, whether it requires sustained aerobic capacity or repeated anaerobic bursts.
Enhancing Athleticism: Speed, Agility, and Mobility
Once the foundation is set, we focus on dynamic qualities.
- Speed training involves breaking down the mechanics of acceleration, top-end speed, and safe deceleration using drills like resisted and assisted sprints.
- Agility work, including ladder drills and cone drills, improves footwork, coordination, and your ability to change direction quickly without losing balance.
- Mobility is the ability to move a joint through its full range of motion with control. Unlike passive flexibility, active mobility is crucial for performance. Ankle mobility, for example, is vital for squatting, jumping, and running. We prioritize it to improve movement and power generation.
- Reaction time training sharpens your cognitive and physical responses using drills that mimic unpredictable game conditions.
The Crucial Role of Injury Prevention and Recovery
The best ability is availability. At Evolve Physical Therapy + Sports Rehabilitation, we train you to perform better and stay healthy.
- Corrective exercise addresses specific imbalances and movement dysfunctions identified in your assessment before they become injuries.
- Movement screening, like the Functional Movement Screen (FMS), helps us identify weak links in your movement patterns that could lead to injury.
- Active recovery techniques like foam rolling and dynamic stretching help your body bounce back faster by reducing muscle soreness and improving blood flow.
- Rest and regeneration are non-negotiable. Your body gets stronger during rest, so we build adequate recovery time and rest days into your program to avoid overtraining.
Our sports performance personal training programs are designed by professionals who understand both performance and rehabilitation. Learn more about how our physical therapy expertise helps athletes perform better and stay injury-free.
Finding Your Trainer: Qualifications, Costs, and What to Look For
Choosing the right guide for your sports performance personal training is a critical investment in your athletic future. It can be the difference between reaching your goals and getting injured.

Essential Qualifications for Sports Performance Personal Training
When vetting a trainer, look for specific credentials that prove their expertise in athletic development.
- The CSCS (Certified Strength and Conditioning Specialist) from the NSCA is the gold standard in sports performance training.
- The NASM-PES (Performance Improvement Specialist) is another respected credential from the National Academy of Sports Medicine, often considered a leader in personal training.
- A Bachelor's or Master's degree in Kinesiology, Exercise Science, or a related field provides a strong academic foundation.
Beyond credentials, look for relevant experience with athletes in your sport and position. A great trainer should also have deep sport-specific knowledge, a clear communication style, and an assessment process that is thorough and individualized.
Understanding the Investment: Costs and Program Structures
The cost of sports performance personal training is an investment in your body, performance, and athletic future. Prices vary by location and experience, but here's a general guide.
- One-on-one training typically ranges from $75 to $200+ per hour. You're paying for years of education, experience, and customized programming.
- Package pricing for multiple sessions or monthly/seasonal training can reduce the per-session cost and increase accountability.
- Program duration is custom to your goals, from a focused 8-12 week program to ongoing, year-round training.
- Group training offers a budget-friendly option that provides a competitive, motivating environment while still allowing for personalized attention.
When evaluating cost, consider the value of expertise. You're investing in reduced injury risk, improved performance that could lead to scholarships or professional opportunities, and long-term physical health. The sports training market is expected to grow significantly, reflecting the results that athletes at all levels are achieving through specialized training.
The right trainer with the right qualifications will help you achieve more than you could on your own, making it a worthwhile investment.
Advanced Concepts: Technology, Nutrition, and Measuring Success
Modern athletic training is about working smarter, not just harder. Today's sports performance personal training combines cutting-edge technology with fundamental nutrition principles to create holistic, measurable athlete development.

Integrating Technology and Data to Track Progress
Technology provides objective insights into your body's performance, moving beyond guesswork.
- Wearable technology like GPS trackers and heart rate monitors provides real-time data on speed, distance, and exertion, allowing us to adjust training loads precisely.
- Video analysis software allows for frame-by-frame breakdown of your technique, revealing subtle inefficiencies in a jump shot or sprint start.
- Force plates measure ground reaction forces during movements like jumps, giving us objective data on power output, explosiveness, and balance.
- Velocity-based training (VBT) uses the speed of your lifts to ensure you're always training at the optimal intensity for your specific goal, whether it's strength or power.
This data-driven approach is used to track your key performance indicators (KPIs)—specific, measurable benchmarks relevant to your sport. Regular re-testing shows us what's working and where to adjust, turning training into a calculated path to success.
Fueling for Peak Performance: The Role of Nutrition
You can't out-train a bad diet. Nutrition is the foundation for recovery, energy, and adaptation.
- Macronutrient timing involves eating the right things at the right times—carbohydrates for energy, protein for muscle repair, and healthy fats for overall function.
- Hydration strategies are critical for both physical and mental performance. We help develop a personalized plan based on your training and sweat rate.
- Pre-competition meals should provide sustained energy without causing digestive issues. We help you find the right strategy for your body.
- Post-workout recovery nutrition, typically a combination of protein and carbs, replenishes depleted stores and accelerates adaptation.
- Supplement guidance is offered based on evidence. We help you steer which supplements may genuinely support your goals and which to avoid.
At Evolve Physical Therapy + Sports Rehabilitation, we understand that performance is a complete picture. This holistic approach—combining smart training, proper fueling, and quantifiable progress—is what transforms good athletes into great ones.
Frequently Asked Questions about Sports Performance Training
How does training differ for team sports versus individual sports?
While fundamentals like strength and speed are universal, the application changes significantly.
For team sports, training must account for positional needs and inter-player dynamics. A football lineman's program will differ greatly from a wide receiver's. We incorporate drills that simulate the chaotic, reactive nature of game situations, focusing on agility, decision-making under fatigue, and developing the capacity for repeated high-intensity efforts.
For individual sports (e.g., swimming, golf, running), training allows for a hyper-personalized focus. We can dedicate more time to perfecting highly technical, repetitive movements with surgical precision. Mental conditioning also emphasizes sustained focus and self-motivation, as there are no teammates to lean on during competition. Conditioning is custom to the exact energy systems demanded by the specific event.
How does age impact a sports performance training program?
Age is a critical factor in designing safe and effective programs. We never use a one-size-fits-all approach.
- Youth athletes: The focus is on long-term athletic development. We build fundamental movement skills, coordination, and balance in a fun environment, prioritizing variety over early specialization.
- Adolescent/Young Adult athletes: As athletes mature, we can safely introduce more advanced strength work, power development, and sport-specific conditioning to meet competitive demands.
- Masters athletes: The priority shifts to maintaining strength and power while protecting joint health and emphasizing recovery. We adjust training volume and incorporate more mobility work to mitigate age-related decline and promote longevity in sport.
Injury risk also changes with age, and our programs are designed to address these age-specific vulnerabilities, from overuse injuries in youth to slower recovery in older athletes.
How quickly can I expect to see results from training?
The timeline for results depends on several factors, but consistency is the most important. Athletes who commit to the process see the best outcomes.
- Adaptation Timeline: You will likely feel changes within the first few weeks, such as increased energy and better movement quality. Measurable improvements in strength or speed often appear around the 4-6 week mark.
- Goals: More significant physiological adaptations—like substantial gains in muscle mass or endurance—generally take 8-12 weeks or more of dedicated training. Short-term goals may be achieved faster than long-term development goals.
- Individual Response: Genetics, training history, nutrition, sleep, and stress levels all influence how quickly your body adapts. Some people are rapid responders, while others progress more gradually.
At Evolve Physical Therapy + Sports Rehabilitation, we emphasize that sports performance personal training is a journey, not a quick fix. We are building resilient, high-performing athletes for the long haul.
Conclusion: Build Your Greatness and Open up Your Potential
We've explored how sports performance personal training differs from general fitness, its core components, and what to look for in a trainer. The key takeaway is that your athletic potential is waiting to be open uped through intelligent, consistent training.
Greatness is built, not born. Every rep, sprint, and recovery session is a building block for your future. Performance is a journey of deliberate steps that compound into remarkable results.
At Evolve Physical Therapy + Sports Rehabilitation, we have spent nearly two decades guiding athletes on this journey. Our holistic physical therapy services across Brooklyn—serving Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin—are built on hands-on care that addresses the whole athlete. We blend physical therapy expertise with a performance-focused mindset to help you not just return to the game, but to come back stronger and more resilient.
The same dedication that drives our specialized programs, like our Rock Steady Boxing for Parkinson's patients, powers our commitment to helping every athlete perform without limits.
Are you ready to invest in your athletic future? We're ready to help you get where you want to go.
Your journey toward peak performance starts with a single step. Take it today.
Start your journey with sports rehabilitation physical therapy in Brooklyn today.
Parkinson's Support Simplified: Where to Find Help
Why Finding Parkinson's Disease Support Matters

Parkinson's disease support comes in many forms, and knowing where to start can make all the difference in how you steer this journey. Here's what you need to know:
Quick Access to Support:
- National Helplines: Parkinson's Foundation (1-800-4PD-INFO), Parkinson Canada (1-888-664-1974)
- Support Groups: 120+ community groups across Canada, local and virtual options across the U.S.
- Online Communities: PD Conversations, CareFinder tool, peer mentorship programs
- Local Resources: Contact helplines for referrals to nearby specialists, support groups, and exercise programs
- Care Partner Support: Dedicated resources, counseling, and respite services available through major organizations
Parkinson's disease is a progressive neurological condition affecting movement and daily life. It occurs when dopamine-producing brain cells, which control movement, begin to die. This leads to common symptoms like tremors, stiffness, and balance issues, but it can also impact mood, sleep, and thinking.
Most importantly, you don't have to face this alone. Living with Parkinson's can feel overwhelming, but building a strong support network of medical professionals, peers, and educational resources is essential. This network is vital for both people with Parkinson's and their care partners as needs evolve.
With over 110,000 people living with Parkinson's in Canada alone, each journey is unique. The common thread is that the right support makes it possible to live well with Parkinson's. Whether you need emotional encouragement, practical advice, or just someone who understands, support is available.
As Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, I've spent years helping people with movement disorders maintain their independence and quality of life, including those seeking comprehensive Parkinson's disease support through specialized physical therapy and active rehabilitation programs. Throughout this guide, I'll walk you through the many types of support available and how to access them.
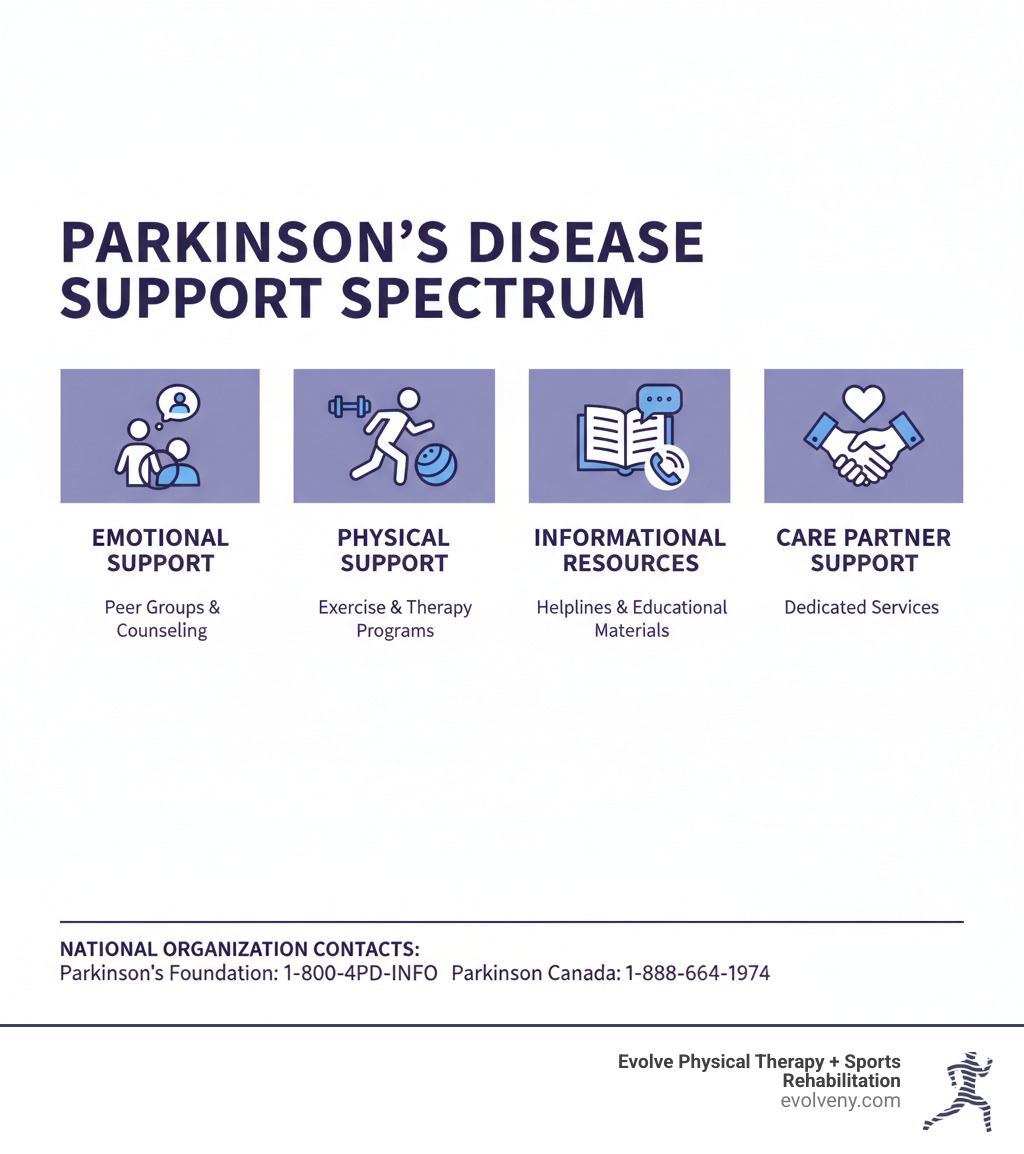
The Spectrum of Support: More Than Just Medical Advice
While medical care is essential, true Parkinson's disease support is a full spectrum that addresses every part of your life. It's about finding emotional, physical, informational, and even spiritual comfort.
- Emotional support provides a safe space to share experiences with peers or professionals.
- Physical support includes practical help and therapeutic interventions, like the specialized physical therapy we offer at Evolve Physical Therapy, to maintain independence.
- Informational resources empower you to make confident decisions about your care.
- Spiritual support can offer comfort through faith or spiritual practices.
- Peer mentorship pairs you with someone who has been there and can offer practical tips and encouragement.
This comprehensive approach recognizes that Parkinson's affects the whole person—body, mind, and spirit—and that care partners need support, too.
Emotional and Peer Connections
Isolation is one of the toughest parts of living with Parkinson's. The symptoms can be unpredictable and hard to explain to others. This is why emotional and peer connections are so powerful. Sharing your story with someone who gets it—whether it's about medication timing, freezing episodes, or daily frustrations—makes you realize you're not alone. One person shared: "Being able to meet people from so many walks of life to discuss what we have in common is so good for me."
These connections build emotional strength and create a community of empathy. Care partners also benefit by swapping coping strategies and finding a judgment-free zone, which helps prevent burnout and strengthens their relationships.
You can find these connections in several ways:
- Local support groups: Parkinson Canada, for example, has a network of 120 community groups offering virtual, in-person, or hybrid meetings, some for specific needs like early-onset PD.
- Online forums: For those who prefer privacy or can't travel, communities like the Parkinson's Foundation's "PD Conversations" are a great option. Explore more at our guide to Online Support Groups for Parkinson's Disease.
- Telephone support groups: An excellent choice for those who prefer talking on the phone.
- 1:1 peer support programs: These match you with a trained mentor for personalized guidance.
These connections offer more than just talk; they provide a resilient, supportive community.
Physical and Active Support
While emotional connections nurture your spirit, physical activity keeps your body strong. Parkinson's disease support through movement is essential. Staying active is a powerful way to fight motor symptoms like poor gait and balance, and it can also help with non-motor issues like low mood and poor sleep.

Physical therapy is foundational. Specialized therapists design personalized programs targeting your challenges with gait, balance, strength, and flexibility to reduce fall risk and combat stiffness. We also offer LSVT BIG® therapy, an intensive program that retrains the brain to make bigger, more normal-sized movements.
A particularly exciting program is Rock Steady Boxing. This non-contact boxing workout is incredibly effective, improving balance, speed, and agility. Our Parkinson's Boxing Classes empower people to fight back against their symptoms. In fact, our Rock Steady Boxing for Parkinson's Disease NYC program was featured on NBC Nightly News for its profound impact.
Beyond formal therapy, community exercise classes like dance or Tai Chi make staying active fun and social.
Informational and Educational Resources
Knowledge is power when navigating a complex condition like Parkinson's. Understanding your body and treatment options helps you feel more in control. Major Parkinson's organizations offer extensive, free educational resources:
- Webinars and podcasts: Learn from experts at home. The Parkinson's Foundation offers podcasts on topics from new treatments to symptom management.
- Educational presentations: Organizations like the Parkinson Association of Alberta host deep dives into specific topics.
- The PD Library: The Parkinson's Foundation's comprehensive online library is organized by topic, offering detailed information for every stage of the journey.
- Hospital Safety Guide: This guide from the Parkinson's Foundation provides tools to help you prepare for and steer hospital stays, where medication timing is critical.
- Research and treatment updates: Stay current to have informed conversations with your healthcare team. We explore this in our article, Is There Treatment for Parkinson Disease.
- Magazines and newsletters: These publications offer information, inspiration, and real-life stories.
These resources are designed for everyone touched by Parkinson's, including family, care partners, and healthcare professionals.
Major Organizations Offering Parkinson's Disease Support
When seeking Parkinson's disease support, knowing the major organizations can make a huge difference. Across North America, dedicated groups offer resources, education, and community, each with a unique focus. Some are national with vast online resources, while others emphasize local connections. Understanding their offerings helps you build the best support system.
- The Parkinson's Foundation (U.S.): Offers a comprehensive helpline for local referrals, an extensive PD Library, a Hospital Safety Guide, and the PD Conversations online community. Most services are free.
- Parkinson Canada: Features a nationwide network of 120 community support groups (virtual, in-person, and hybrid), a 1:1 peer support program, and a CareFinder tool to locate local resources. Their support line is free.
- Parkinson Association of Alberta: Provides presentations, counseling, and telephone support groups for those in Alberta and the Northwest Territories. An annual membership fee ($35 primary, $15 secondary) open ups their full program.
You don't have to choose just one; combining national resources with local groups is often the most effective approach.
The Parkinson's Foundation (U.S.)
In the United States, the Parkinson's Foundation is a primary source for Parkinson's disease support. Their standout feature is the helpline (1-800-4PD-INFO or Helpline@Parkinson.org), staffed by specialists who provide answers and connect you with local experts like neurologists and physical therapists.
Key resources include:
- PD Library: A comprehensive, topic-organized encyclopedia for every stage of Parkinson's.
- Hospital Safety Guide: An essential tool I recommend to patients for navigating hospital stays, where medication timing and specific PD needs are critical.
- PD Conversations: An online community for people with Parkinson's and care partners to share experiences in a judgment-free zone.
The Foundation also provides dedicated resources for care partners and healthcare professionals, funds research, and advocates for better policies. Explore all they offer at Resources & Support.
Parkinson Canada
Parkinson Canada is the national voice for Canadians with Parkinson's, offering a coast-to-coast support network.
Their key offerings include:
- 120 community support groups: These safe havens offer in-person, virtual, and hybrid meetings. They provide specialized groups for early-onset and newly diagnosed individuals, addressing unique challenges.
- 1:1 peer support program: This program matches you with a trained volunteer mentor who has lived experience with Parkinson's and can offer personal guidance.
- CareFinder tool: An easy-to-use online tool to locate support groups and services in your area.
You can also contact their support line at 1-888-664-1974 or support@parkinson.ca for information on everything from diagnosis to medication management. As a major funder of Parkinson's research, they are also committed to finding a cure. Learn more at Find support in community.
Finding Local Parkinson's Disease Support Groups
Connecting with a local Parkinson's disease support group provides a powerful blend of emotional support, practical advice, and friendship. These groups offer more than just meetings; they build community through social outings, exercise classes, and shared experiences.
Finding a local group is straightforward:
- Contact national helplines: Call the Parkinson's Foundation (1-800-4PD-INFO) or Parkinson Canada (1-888-664-1974). Their specialists can provide direct referrals.
- Use online search tools: Parkinson Canada's CareFinder and the Parkinson's Foundation's "Your Area" section map out local resources.
- Ask your healthcare team: Your neurologist or physical therapist is a great resource. At Evolve Physical Therapy, we regularly connect our patients in Brooklyn—from Marine Park to Park Slope—with helpful local groups.
- Check community hubs: Local hospitals, community centers, and places of worship often host groups.
The camaraderie in a local group can transform your experience, reminding you that you have a community at your back. We've written more about how Parkinson's Disease Support Groups empower people to live fuller lives.
The Care Partner's Journey: Support for the Supporters
We must not forget the unsung heroes of the Parkinson's journey: the care partners. Caregiving is a dynamic role with unique emotional, spiritual, and physical demands.
As Parkinson's progresses, a care partner's role evolves from occasional assistance to managing medications, daily tasks, and constant emotional support. This can be rewarding but also challenging, bringing feelings of grief, frustration, and anxiety.
It's normal for both the care partner and the person with Parkinson's to resist the "caregiver" label, as it marks a shift in the relationship. Acknowledging this difficulty and adapting to new roles is crucial for a healthy partnership. We explore this further in our guide to Caregiver Support for Parkinson's.
The Importance of Parkinson's Disease Support for Caregivers
Care partners need Parkinson's disease support just as much as the individuals they care for. A strong support network is a vital lifeline. Connecting with other caregivers helps you realize you're not alone and allows you to:
- Share coping strategies: Gain invaluable peer wisdom on managing daily challenges and navigating healthcare.
- Reduce isolation: Caregiving can be solitary. Connecting with others who understand alleviates loneliness.
- Find respite: Learn about respite care resources to get necessary breaks to recharge.
- Maintain a healthy partnership: Feeling supported helps you minimize stress and maximize connection with your loved one.
Dedicated Parkinson's Caregiver Support Groups offer a judgment-free zone to share your struggles and triumphs.
Self-Care Strategies for Care Partners
Taking care of yourself as a care partner is not selfish—it is essential. You cannot pour from an empty cup. Protecting your own well-being is fundamental to providing good care.
- Prioritize your own health: Don't skip your own doctor visits, and ensure you get a balanced diet and sufficient sleep. You can't provide good care if you aren't well.
- Maintain hobbies and social connections: Make time for activities and friends outside of your caregiving role to preserve your own identity.
- Exercise and mindfulness: Movement and practices like meditation are powerful stress reducers. Research even points to the Neuroprotective Effect of Green and Blue Spaces, so a walk in the park is good for body and mind.
- Set boundaries: It's necessary to say no sometimes. Establish clear limits on what you can realistically do to prevent burnout.
- Accept help: When friends or family offer to run an errand or help in other ways, let them.
- Seek professional support: If you're struggling emotionally, a counselor or therapist can provide invaluable guidance.
Self-care is a necessity for sustaining your energy and ability to provide compassionate care long-term.
Frequently Asked Questions about Parkinson's Support
We understand you likely have many questions about accessing Parkinson's disease support. Here are answers to some of the most common inquiries we hear:
How do I find a support group near me?
Start by contacting the helplines of major organizations like the Parkinson's Foundation (1-800-4PD-INFO) or Parkinson Canada (1-888-664-1974). Their specialists can provide local referrals for your area, including Brooklyn, Marine Park, Gravesend, Midwood, Park Slope, or Mill Basin. You can also use online tools like Parkinson Canada's CareFinder or ask your neurologist or physical therapist for recommendations.
Are there support services specifically for newly diagnosed individuals?
Yes. Many organizations offer specialized programs for the newly diagnosed. For example, Parkinson Canada has subject-specific groups, and Parkinson's UK offers a "First Steps" online program. These resources provide foundational knowledge, help you adjust to the diagnosis, and connect you with peers at a similar stage, which can reduce feelings of overwhelm.
What is the cost of joining a support group or accessing services?
Many essential Parkinson's disease support services are free. Most support groups, helplines, and online resources from national organizations are free to access. Some regional organizations, like the Parkinson Association of Alberta, may have a nominal annual membership fee (e.g., $35 primary, $15 secondary) for access to a wider range of programs. Always check with the specific organization, but accessible support is widely available.
Conclusion
Living with Parkinson's disease is not a solitary journey. As we've explored, a wide range of Parkinson's disease support is available, from peer connections and educational resources to physical programs that build strength and independence. The simple truth is: you are not alone. A combination of emotional, informational, and physical support creates a powerful toolkit for both individuals with Parkinson's and their care partners.
Taking proactive steps to find your community—by calling a helpline like the Parkinson's Foundation at 1-800-4PD-INFO, joining an online forum, or attending a local group—builds resilience and confidence.
For those in the Brooklyn area—including Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin—we're proud to offer physical therapy for Parkinson's at Evolve Physical Therapy. Our hands-on approach and specialized programs like the NBC News-featured Rock Steady Boxing help you maintain independence and quality of life. We treat the whole person and can connect you with the broader support network you need.
Seeking support is a sign of strength. It shows you're committed to living well and facing this challenge with every resource available. Whether you're newly diagnosed or a care partner, there's a place for you in this community. Reach out, connect, and take the next step forward. We're here to help.
Heal Your Hands: Premier Therapy Options Across Brooklyn
Why Your Hands Deserve Expert Care

Brooklyn hand therapy provides specialized treatment for injuries and conditions affecting your hands, wrists, elbows, and shoulders. If you're experiencing pain or limited function in your upper extremities, here's what you need to know:
Quick Guide to Brooklyn Hand Therapy:
- What it treats: Carpal tunnel syndrome, arthritis, fractures, tendonitis, trigger finger, post-surgical recovery, sports injuries, and nerve compressions
- Who provides it: Certified Hand Therapists (CHTs) - licensed Physical or Occupational Therapists with specialized training
- Common treatments: Custom splinting, manual therapy, therapeutic exercises, scar tissue management, and ergonomic education
- Timeline: Recovery varies from days to months depending on your condition
- Location options: Multiple clinics across Brooklyn neighborhoods including Park Slope, Marine Park, Mill Basin, Gravesend, and Midwood
As humans, we rely on our hands for all manner of tasks that we usually take for granted - from typing and eating to playing sports and caring for our families. When even one hand hurts, it can stop you from doing many normal daily tasks. Whether you've suffered a workplace injury, developed repetitive strain from computer use, or need post-surgical rehabilitation, hand therapy offers a non-surgical path to recovery.
The good news? Nearly one million hand injuries occur annually, and specialized hand therapy has helped countless people regain full function and return to the activities they love. Brooklyn is home to several hand therapy centers staffed with Certified Hand Therapists who use evidence-based techniques to restore your strength, reduce pain, and improve mobility.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn, where I've spent nearly two decades helping patients recover from complex injuries and chronic pain through hands-on manual therapy and customized rehabilitation programs. My experience with Brooklyn hand therapy cases ranges from simple sprains to complex post-surgical recoveries, and I've seen how proper treatment can transform someone's quality of life.
![[object Object] [object Object]](https://images.bannerbear.com/direct/4mGpW3zwpg0ZK0AxQw/requests/000/116/900/541/KPbegp4noQkDXgwKYlVkN03vE/ee040637b67a1afc58f42b5d3399a5b213e46c42.jpg)
Understanding Hand Therapy: Your Path to Recovery
When you think about hand therapy, you might picture someone working on just your fingers. But here's the thing: Brooklyn hand therapy actually covers much more ground than that. It's a specialized form of rehabilitation that treats the entire upper extremity—from your fingertips all the way up through your wrist, forearm, elbow, and shoulder.
Why such a broad focus? Because everything in your upper body is connected. A problem with your shoulder can affect how your hand functions, and vice versa. Hand therapy takes this whole-body approach to get you moving properly again.
The beautiful part about hand therapy is that it's completely non-surgical. Instead of going under the knife, you're working with skilled therapists who use targeted techniques to reduce your pain and restore function. The goal is simple: help you get back to doing the things you love—whether that's playing piano, working at your computer, cooking family dinners, or throwing a baseball with your kids.
At Evolve Physical Therapy + Sports Rehabilitation, we believe healing happens when you're an active partner in your recovery. Our Brooklyn hand therapy program focuses on understanding your specific situation and building a treatment plan around your life and goals. An injury anywhere along your upper extremity can throw your whole routine off balance, and we're here to help you find your way back.
Hand therapy is provided by licensed Occupational Therapists (OTs) or Physical Therapists (PTs) who've gone beyond their basic training to specialize in the intricate workings of the upper limb. These aren't just general therapists—they've invested serious time learning the complex anatomy and biomechanics of your hands, wrists, arms, and shoulders.
What makes this approach especially effective is the collaboration. Your hand therapist works directly with your referring physician to ensure everyone's on the same page about your recovery. This team approach means you're not just getting isolated treatment—you're getting coordinated care designed specifically for you.
Find more info about what hand physical therapy is and how it can help you.
The Gold Standard: Certified Hand Therapists (CHTs)
You might hear the term "Certified Hand Therapist" or CHT when exploring Brooklyn hand therapy options. This isn't marketing fluff—it's a credential that represents the highest level of expertise in the field.
A Certified Hand Therapist is an Occupational or Physical Therapist who's earned a prestigious certification from the Hand Therapy Certification Commission (HTCC). Think of it as the difference between a good cook and a master chef. Both can make you dinner, but one has proven expertise at the highest level.
Here's what it takes to become a CHT: First, you need at least three years of clinical experience as a therapist. But not just any experience—you must complete 4,000 hours or more of direct hands-on practice specifically in hand therapy. That's roughly two full years of doing nothing but treating upper extremity conditions.
Then comes the hard part: passing a rigorous certification examination that tests advanced knowledge of everything related to the upper extremity. We're talking about anatomy, biomechanics, pathology, assessment techniques, and treatment protocols. Only therapists who demonstrate mastery of these complex topics earn the CHT credential.
What does this mean for you? When you work with a CHT, you're getting someone who truly understands the intricate structures of your hands and arms. They've treated countless patients with conditions ranging from simple sprains to complex post-surgical rehabilitation, and they know how to steer the challenges that can arise during recovery.
One specialized skill that sets CHTs apart is custom splint fabrication. These aren't the generic braces you pick up at a pharmacy. Our CHTs at Evolve Physical Therapy + Sports Rehabilitation create custom orthoses custom precisely to your hand, your condition, and your recovery goals.
These custom splints serve different purposes depending on what you need. Some stabilize a fracture while it heals. Others protect a healing tendon from overstretching. Still others gently correct alignment issues or prevent unwanted movements while you sleep. Each one is carefully molded to fit your unique anatomy, providing the exact support you need—nothing more, nothing less.
This level of specialized knowledge and hands-on expertise means you're receiving care from professionals who've dedicated their careers to understanding the complexities of hand and upper extremity rehabilitation. When you're dealing with something as important as your ability to use your hands, that expertise makes all the difference.
Conditions That Benefit from Specialized Hand Therapy
Your hands are remarkable tools, but their complexity makes them vulnerable to injury and disease. Think about it: twenty-seven bones in each hand, dozens of muscles, tendons, and ligaments, all working together to let you type, cook, play guitar, or give someone a high-five. When something goes wrong anywhere from your fingertips to your shoulder, it can derail your entire day.
That's where specialized hand therapy comes in. Whether you're dealing with the aftermath of a workplace accident where you caught your hand in machinery, a sports injury from that weekend basketball game, or the gradual creep of a repetitive strain injury from years at a computer, hand therapy offers real solutions. We also work extensively with patients recovering from post-surgical procedures, helping them regain strength and mobility after operations on their hands, wrists, elbows, or shoulders.

Common Conditions Treated with Brooklyn Hand Therapy
At Evolve Physical Therapy + Sports Rehabilitation, we've seen just about every upper extremity problem you can imagine. Our Brooklyn hand therapy services address everything from sudden injuries to conditions that develop slowly over time.
Arthritis is one of the most common reasons people seek our help. Whether you're dealing with osteoarthritis wearing down your joints or rheumatoid arthritis causing inflammation, we create custom exercise programs, use manual therapy techniques, and teach activity modifications that help you manage pain and keep doing what you love.
If you're experiencing numbness and tingling in your hand, especially at night, you might be dealing with Carpal Tunnel Syndrome. This condition responds remarkably well to hand therapy. We use splinting to keep your wrist in the optimal position, teach you ergonomic adjustments for your workspace, and guide you through exercises that reduce pressure on the median nerve.
Trigger Finger can be frustrating—your finger catches or locks when you try to straighten it, sometimes with an audible pop. We treat the underlying inflammation of the tendon sheath through targeted exercises, splinting, and manual techniques that help restore smooth gliding motion.
Various forms of tendonitis bring many patients through our doors. De Quervain's Tenosynovitis affects the thumb side of your wrist and makes activities like lifting your baby or opening jars painful. We also treat tennis elbow, golfer's elbow, and other tendon inflammations throughout the forearm and elbow. Our approach focuses on reducing inflammation, improving flexibility, and gradually strengthening the affected tissues so they can handle daily demands.
Dupuytren's Contracture is a condition where tissue under the palm thickens and contracts, gradually pulling your fingers into a bent position. Hand therapy plays a crucial role in managing symptoms, maintaining range of motion, and supporting your recovery if you've had medical interventions like injections or surgery.
Nerve compressions and injuries can cause anything from annoying tingling to debilitating pain and weakness. Cubital Tunnel Syndrome, which affects your pinky and ring finger with that "pins and needles" feeling, responds well to specific exercises and nerve gliding techniques. We also treat other nerve injuries throughout the upper extremity, helping you regain sensation and movement.
When you've broken a bone in your hand, wrist, or elbow, or suffered a sprain or ligament injury, proper rehabilitation is essential. We work with you from the early stages of healing through full recovery, managing pain and swelling, then progressively restoring your strength and mobility. Mallet finger (where you can't straighten your fingertip) and finger dislocations require specialized care to ensure proper healing, and we provide exactly that.
Finally, if you've had surgery on your hand, wrist, elbow, or shoulder, our post-surgical rehabilitation programs guide you through structured recovery. We optimize healing, manage scar tissue formation, and help you regain full strength and mobility so you can return to your normal activities with confidence.
The Brooklyn Hand Therapy Process: From Evaluation to Results
When you walk through our doors at Evolve Physical Therapy + Sports Rehabilitation, you're not just getting a generic treatment protocol. We believe that your hand injury or condition is as unique as you are, which is why we build individualized treatment plans custom to your specific needs, lifestyle, and goals.
Think of us as your partners in recovery. We're not here to simply prescribe exercises and send you on your way. Instead, we work with you, teaching you about your condition, involving you in decisions about your care, and giving you the tools and knowledge you need to take an active role in your healing. Our focus is always on two things: healing the injury and strengthening your hand so you can return to the activities that matter most to you.
Whether you're recovering from hand surgery or trying to avoid it altogether, our specialized rehabilitation programs are designed to support you through every stage. Explore our hand surgery rehab services in Brooklyn.
What to Expect from Your Brooklyn Hand Therapy Evaluation
Your first visit sets the foundation for everything that follows. We dedicate significant time to this initial consultation because understanding your complete picture helps us create the most effective treatment plan possible.
During your evaluation, we'll start with a thorough medical history review. We want to know about any previous injuries, surgeries you've had, and medications you're taking. But we also dig deeper into your daily life. What does your typical day look like? What activities are you struggling with? Are you a musician who can't play anymore? A carpenter who can't grip tools? A parent who has trouble lifting your child? These details matter immensely because your recovery goals should reflect what's important to you.
Next comes the physical examination. Our therapists will carefully assess your upper extremity, looking at how well your joints move, testing your muscle strength, and checking nerve function. We might ask you to perform certain movements or tasks while we observe. Don't worry if some of these tests feel a bit uncomfortable—we're looking for specific information about what's limiting your function.
We'll also conduct an assessment of strength and sensation. Using specialized tools, we'll measure your grip strength and pinch strength. We'll test sensation in your hand and fingers, checking for areas of numbness or hypersensitivity. Nerve involvement plays a significant role in many hand conditions, so understanding your sensory function helps us target treatment more effectively.
An important part of your evaluation is the Activities of Daily Living (ADL) status check. We'll talk through specific tasks that most people take for granted—things like buttoning a shirt, opening jars, typing on a keyboard, or holding a coffee cup. Understanding exactly which movements cause you difficulty helps us focus on exercises and techniques that will make the biggest difference in your daily life.
Finally, we'll work together on goal setting. Based on everything we've learned during your evaluation and what matters most to you, we'll establish realistic, meaningful goals for your therapy. Maybe you want to return to playing tennis, or perhaps you just want to be able to tie your shoes without pain. Whatever your goals are, they become our roadmap for your recovery.
Advanced Treatments and Techniques
Once we understand your condition and goals, we'll create a personalized treatment plan using a variety of evidence-based techniques. Every Brooklyn hand therapy program at Evolve is different because every patient is different.
Manual therapy forms the foundation of much of what we do. This hands-on approach means your therapist uses their hands to mobilize stiff joints, release tight tissues, and reduce pain. It's not just massage—it's skilled, precise work that targets specific structures in your hand, wrist, and arm. Manual therapy improves circulation, reduces swelling, and helps restore normal movement patterns.

We'll also guide you through therapeutic exercises specifically designed for your condition. These aren't random stretches—they're targeted movements that improve your range of motion, rebuild strength, and restore coordination and dexterity. You might work with therapy putty to strengthen your grip, use resistance bands to build muscle, or practice fine motor tasks to improve precision. We'll teach you how to do these exercises correctly and give you a home program so your recovery continues between visits.
Custom orthoses and splinting is an area where our Certified Hand Therapists truly shine. Unlike generic splints you might buy at a pharmacy, custom-fabricated splints are molded specifically to your hand and your condition. These devices can stabilize fractures while they heal, protect surgically repaired tendons, correct deformities, or provide support during activities. The right splint at the right time can make an enormous difference in your recovery.
After surgery or a significant injury, scar tissue management becomes crucial. Scar tissue can limit your movement and cause discomfort long after the initial injury has healed. We use specialized massage techniques, stretching, and sometimes tools like silicone gel sheets to soften and remodel scar tissue. This helps restore normal tissue mobility and reduces that tight, pulling sensation many people experience.
Kinesio taping is a colorful addition to your treatment that serves a real purpose. This elastic therapeutic tape supports muscles and joints, reduces swelling, and alleviates pain—all without restricting your movement the way traditional athletic tape does. It's particularly useful for providing gentle support between therapy sessions.
For conditions affecting your nerves, sensory retraining helps your nervous system relearn normal sensation. Through specific exercises and techniques, we can improve your ability to discriminate between different textures and temperatures, reduce hypersensitivity, and help restore normal feeling to your hand.
Finally, we provide ergonomic education because preventing future problems is just as important as fixing current ones. We'll teach you how to modify your workspace, adjust your computer setup, and change how you perform certain tasks to reduce strain on your hands and upper extremities. Small changes in how you work, type, or lift can prevent injuries from recurring and help manage chronic conditions more effectively.
Explore more about hand therapy categories and techniques we offer.
The combination of these techniques, custom to your specific needs, creates a comprehensive approach that addresses not just your symptoms but the underlying causes of your hand problems. And throughout your entire treatment, we're right there with you, adjusting your program as you progress and celebrating each milestone along the way.
Frequently Asked Questions about Hand Therapy
When you're dealing with hand pain or an injury, you probably have plenty of questions swirling around in your mind. We hear them every day at our Brooklyn clinic, and we want to make sure you feel informed and comfortable before you even walk through our doors. Here are the most common questions people ask about Brooklyn hand therapy, answered honestly and clearly.
How long does hand therapy typically take?
I wish I could give you a simple answer like "six weeks" or "three months," but the truth is that every person's healing journey is unique. Your recovery timeline depends on what's going on with your hand, how severe the injury or condition is, your overall health, and how consistently you follow through with your home exercises.
Some of our patients with minor sprains or mild carpal tunnel syndrome notice real improvement within just a few days to weeks. Others dealing with more complex issues—like recovering from surgery or managing chronic arthritis—may need several months of therapy to reach their goals. It's not a race, though. What matters most is that you're making steady progress toward getting back to the activities you love.
During your initial evaluation, we'll give you a realistic timeline based on your specific situation. We'll also talk about the factors that can speed up or slow down your recovery. Here's what I can tell you for certain: consistency matters tremendously. The patients who do their prescribed exercises at home, follow our activity modification recommendations, and show up to their sessions tend to recover faster and more completely. Think of it as a partnership—we provide the expertise and guidance, but you're the one doing the important daily work of healing.
Is hand therapy painful?
This is probably the number one concern we hear, and it's completely understandable. After all, your hand already hurts—why would you want someone poking and prodding it? Here's the reassuring truth: the entire goal of hand therapy is to reduce your pain, not add to it.
Now, I'll be honest with you. As we work to restore your range of motion or strengthen muscles that have been weak or inactive, you might experience some discomfort. This is different from pain, though. It's more like the feeling you get when you stretch a tight muscle—a sensation of effort or mild challenge, not sharp or intense pain. We always explain the difference to our patients: discomfort often means we're working at the edge of your current abilities, which is where healing happens. Pain, on the other hand, is your body's alarm system telling us to back off.
Communication is absolutely essential here. If something we're doing feels genuinely painful, we want you to speak up immediately. There's no need to be tough or push through real pain. Our therapists are experts at modifying exercises and techniques to keep you comfortable while still making progress. We might adjust the intensity, try a different approach, or slow down the pace. Your recovery should challenge you, but it should never leave you dreading your next appointment.
Do I need a doctor's referral to see a hand therapist in Brooklyn?
This is a great question, and the answer might surprise you. In New York State, we have what's called "Direct Access" laws, which means you can often come see us for an evaluation and treatment without getting a referral from your doctor first. This is fantastic if you want to get started on your recovery right away without waiting for a doctor's appointment.
That said, there's an important caveat: your insurance company might have different rules. Some insurance plans still require a physician's referral or prescription before they'll cover physical therapy services. We know insurance can be confusing (believe us, we deal with it every day), so we're always happy to help you figure out what your specific plan requires. Just give us a call, and we can check your benefits and let you know what documentation you'll need.
Even though direct access allows you to come straight to us, we're big believers in teamwork when it comes to healthcare. We often work closely with your referring physician, especially for complex conditions or if you're recovering from surgery. This collaboration ensures everyone's on the same page about your treatment plan, and it means your doctor stays informed about your progress. It's all about giving you the most comprehensive care possible. If you have questions about referrals or how to coordinate with your healthcare team, just ask—we're here to help you steer through it all.
Finding Your Path to Healing in Brooklyn
Your hands are extraordinary tools that deserve equally extraordinary care. When injury or pain strikes, finding the right support can make all the difference between a frustrating recovery and getting back to the life you love.
At Evolve Physical Therapy + Sports Rehabilitation, we understand that choosing where to receive Brooklyn hand therapy is an important decision. You're not just looking for any treatment—you're looking for a team that truly understands the intricate workings of your hands, wrists, and upper extremities.
The best hand therapy clinics share certain qualities that set them apart. Certified Hand Therapists (CHTs) on staff is perhaps the most important factor, ensuring you're working with professionals who've dedicated years to mastering their specialty. An individualized approach matters too, because your injury and your life circumstances are unique. What works for one person might not be the right solution for you.
Look for a clinic that believes in a hands-on methodology—quite literally. Effective hand therapy often requires skilled manual techniques and direct interaction with your therapist, not just exercises on a sheet of paper. You also want comprehensive services under one roof, from custom splint fabrication to therapeutic exercises, ergonomic education to scar tissue management.
We're proud to offer all of this and more at our conveniently located clinics throughout Brooklyn, including Marine Park, Mill Basin, Park Slope, Gravesend, and Midwood. Our team of dedicated CHTs and physical therapists combines expert knowledge with genuine care, creating a supportive environment where healing happens naturally.
We've spent nearly two decades helping Brooklyn residents recover from hand injuries and conditions, from simple sprains to complex post-surgical rehabilitation. Every day, we see people regain abilities they thought they'd lost—typing without pain, playing guitar again, lifting their grandchildren, returning to their favorite sports.
Your hands have carried you through life's most important moments. Let us help you get them back to full strength.
Move Better, Live Better: Therapeutic Exercise and PT in Brooklyn
Why Physical Therapy Brooklyn Can Transform Your Recovery Journey

Physical therapy Brooklyn offers a proven path to pain relief, injury recovery, and improved mobility without relying on drugs or surgery. Whether you're dealing with chronic pain, recovering from an injury, or looking to prevent future problems, Brooklyn's physical therapy clinics provide specialized, hands-on care customized to your needs.
Quick Answer: Finding Physical Therapy in Brooklyn
- 144 physical therapy clinics operate throughout Brooklyn's neighborhoods
- No referral required in New York State for up to 10 visits or 30 days
- Services include: manual therapy, sports rehabilitation, post-surgical recovery, chronic pain management, and specialized programs for conditions like Parkinson's disease
- Most major insurance accepted: including Aetna, Cigna, Medicare, and UnitedHealthcare
- Average wait time: Under 20 minutes at top-rated clinics
- Treatment approach: One-on-one care with personalized plans focusing on evaluation, healing, and strengthening
Living in Brooklyn means staying active. When pain or injury disrupts your routine, the right physical therapist can help you get back to doing what you love. The borough's diverse physical therapy landscape ranges from large hospital systems to specialized clinics offering cutting-edge treatments like vestibular therapy, pelvic floor rehabilitation, and sports injury recovery.
Brooklyn's top physical therapy providers emphasize a holistic, hands-on approach. They perform comprehensive evaluations to find the root cause of your pain, then create individualized treatment plans. This three-phase approach involves pain relief, strengthening, and functional retraining to prevent future injuries.
I'm Lou Ezrick, founder of Evolve Physical Therapy + Sports Rehabilitation, where I've spent nearly two decades providing physical therapy Brooklyn residents trust for chronic pain management, sports injuries, and complex rehabilitation cases. My approach combines advanced manual therapy techniques with personalized exercise programs to help patients achieve lasting results and avoid unnecessary surgery.
The Core Benefits of Physical Therapy: More Than Just Injury Recovery
When you choose physical therapy Brooklyn, you're opting for a powerful, evidence-based approach to health and wellness. It’s about more than recovering from an injury; it’s about improving your quality of life, managing chronic conditions, and enhancing athletic performance. Our holistic approach at Evolve Physical Therapy + Sports Rehabilitation focuses on evaluating your unique situation, healing the source of your discomfort, and strengthening your body to prevent future issues.
Restoring Function and Independence
One of the most profound benefits of physical therapy is its ability to help you regain lost function and independence. Whether you're struggling with daily tasks or want to walk without pain, our therapists work with you to improve mobility and strength. We focus on exercises that translate to your daily life, reducing reliance on assistive devices. This is vital for pre-surgical rehabilitation to prepare your body for a procedure, or post-surgical rehabilitation to accelerate recovery. Our goal is to get you back to doing what you love, feeling stronger than before.
A Non-Invasive Path to Pain Management
Many people turn to physical therapy as a non-invasive, drug-free alternative to manage pain. Instead of masking symptoms, we address the root cause of your discomfort. Our therapists use a combination of manual therapy, therapeutic exercise, and advanced modalities like electrical stimulation (E-stim) and ultrasound therapy to alleviate pain and promote healing. This hands-on approach helps mobilize stiff joints, release muscle tension, and improve circulation, offering lasting relief without the side effects of medication or the risks of surgery.
What Conditions Can Physical Therapy in Brooklyn Treat?
If you're wondering whether physical therapy can help your specific issue, the answer is probably yes. The range of conditions we treat at Evolve Physical Therapy + Sports Rehabilitation is extensive. We work with everyone from marathon runners and office workers with chronic neck pain to seniors working to prevent falls and individuals managing complex neurological conditions.
Physical therapy Brooklyn clinics handle everything from acute injuries to chronic conditions. The most common issues we see are back pain, neck pain, and sciatica. We also treat sports injuries like rotator cuff tears and ACL reconstruction recovery, along with arthritis that limits daily activities. But our care extends far beyond that, including post-surgical recovery for procedures like joint replacements and help for neurological conditions like stroke recovery and Multiple Sclerosis.
Orthopedic and Sports Injuries
When injuries happen, we're here to get you back in action. We treat common issues like sprains and strains, tendinitis, and bursitis by reducing inflammation and addressing the underlying movement patterns causing the problem.
Rotator cuff injuries and ACL reconstruction recovery respond well to physical therapy. We find that targeted strengthening and manual therapy can often resolve shoulder pain without surgery, and we guide patients through the process of safely returning to their sport after ACL surgery. We also treat back pain, neck pain, and sciatica by digging into the root cause, whether it's poor posture or weak core muscles.
Core instability often underlies other problems, so we strengthen these essential muscles to support your spine. For those with myofascial pain syndrome, we use targeted techniques to release trigger points. Our approach also includes injury prevention strategies, teaching proper biomechanics and developing strengthening programs to keep you healthy. To learn more, check out our specialized sports rehabilitation programs.
Chronic and Neurological Conditions
Physical therapy can dramatically improve quality of life for those with chronic and neurological conditions. For Parkinson's disease, we offer programs like Rock Steady Boxing—a non-contact boxing program featured on NBC News that improves balance, coordination, and motor skills.
If you experience dizziness or unsteadiness, you might have vestibular disorders or vertigo. Our vestibular therapy retrains your balance system. We also address age-related balance issues with gait and balance assessments and training programs to reduce fall risk.
Chronic pain management for conditions like fibromyalgia and some types of headaches involves long-term strategies to reduce discomfort and improve function. For stroke recovery and Multiple Sclerosis, physical therapy focuses on regaining motor control and maintaining independence. Whether you have a recent injury or a long-term condition, physical therapy Brooklyn offers evidence-based solutions to help you feel and move better.
A Spectrum of Services: Types of Physical Therapy Available
At Evolve Physical Therapy + Sports Rehabilitation, you won't get a one-size-fits-all plan. We offer a comprehensive range of services built around our core philosophy: evaluate, heal, and strengthen. Our hands-on approach treats you as a whole person, not just a collection of symptoms. Our Brooklyn clinics combine time-tested manual therapy with modern modalities to create personalized treatment plans that guide you every step of the way.
Hands-On Techniques and Modalities
Our therapists don't just watch you do exercises; they actively work with your body to promote healing. Here are some of the techniques we use:
Manual therapy is the foundation of our approach. Our therapists use their hands to apply pressure to muscle tissue and mobilize joints, which is highly effective for reducing pain. This includes joint mobilization to restore proper movement to stiff joints.
For tight and painful muscles, soft tissue massage and myofascial release target problem areas to alleviate tension, reduce spasms, and boost circulation. These techniques address both muscles and the connective tissue around them.

We also use supportive and advanced modalities. Kinesio taping provides support to muscles and helps reduce swelling, while spinal traction gently stretches the spine to relieve pressure on compressed nerves. Electrical stimulation (E-stim) can reduce pain and muscle spasms, and ultrasound therapy uses sound waves to create therapeutic heat in soft tissues, promoting healing from within.
Specialized Physical Therapy Programs
Our Brooklyn community has varied healthcare needs, so we've developed specialized programs for specific conditions and populations, serving neighborhoods from Marine Park to Park Slope.
Sports Rehabilitation: We focus on getting athletes back to their sport quickly and safely, with an emphasis on performance and injury prevention. Learn more on our sports rehabilitation page.
Geriatric Physical Therapy: For older adults, we focus on improving balance, building strength, and preventing falls to maintain an active, independent lifestyle.
Post-Operative Rehabilitation: We provide comprehensive care after surgeries like joint replacements and ACL reconstruction to ensure an efficient and full recovery.
Neurological Rehabilitation: We offer specialized treatment for stroke survivors, people with Parkinson's disease (including our Rock Steady Boxing program), and those managing multiple sclerosis.
Pelvic Floor Rehabilitation: We treat conditions like urinary incontinence and pelvic organ prolapse with targeted exercises to strengthen and retrain these important muscles.
Vestibular Therapy: For those struggling with dizziness, vertigo, or balance disorders, this therapy can help recalibrate the inner ear and balance system.
For a complete overview of our offerings, visit our specialized programs page.
Your Path to Wellness: Choosing a Clinic and Your First Appointment
Finding the right physical therapist shouldn't add to your stress. With 144 physical therapy clinics in Brooklyn, you have options. We want to help you cut through the confusion and find a path to recovery that feels right for you.

How to Choose the Right Physical Therapist in Brooklyn
Choosing a physical therapist is like finding a partner for your recovery. Look for key qualities to ensure you get the best care. Start with credentials (a Doctor of Physical Therapy, or DPT, is the standard) and experience, especially for complex issues. Specialization is also crucial; if you have a condition like Parkinson's disease, you need a therapist with expertise in that area. At Evolve, we offer specialized programs like Rock Steady Boxing for Parkinson's patients, which has been featured on NBC News.
Check patient reviews and Google ratings to gauge a clinic's quality of care. We believe the best physical therapy Brooklyn clinics provide one-on-one care and a hands-on treatment guarantee. You deserve dedicated attention, not generic exercises in a crowded room. Finally, consider location and convenience. Our clinics in Marine Park, Gravesend, Midwood, Park Slope, and Mill Basin make quality care accessible throughout Brooklyn.
What to Expect During Your First Physical Therapy Appointment in Brooklyn
Your first session begins with a thorough initial evaluation. We'll discuss your medical history, current symptoms, and how your condition affects your daily life. Next is a movement investigation, where we'll watch how you move, analyze your gait, and assess your range of motion to understand the source of your pain.
Together, we'll establish clear, achievable goals that matter to you. Based on this, we'll create a personalized treatment plan—a roadmap designed for your body and your goals. We'll explain which techniques and exercises we'll use and why.
For your appointment, wear comfortable, loose-fitting clothing that allows for easy movement, like gym clothes. Plan for your session to last about an hour to an hour and a half, as we don't rush quality care.
Navigating Costs and Insurance for Physical Therapy in Brooklyn
We know healthcare costs are a concern. The good news is that physical therapy is often more affordable than you might think. We're in-network with most major insurance plans, including Aetna, BlueCross BlueShield, Cigna, Healthfirst, Medicare, MetroPlus, Oxford, and UnitedHealthcare. Our team can help you verify your specific coverage and understand your benefits.
Thanks to the Direct Access law in New York State, you typically don't need a doctor's referral to start physical therapy Brooklyn. You can see a physical therapist for up to 10 visits or 30 days, saving you time and getting you on the path to recovery faster.
Physical therapy is a cost-effective investment in your long-term health, helping you avoid expensive surgeries and ongoing prescription costs. Ready to take the first step? You can request an appointment through our online form or find us on Zocdoc to schedule your visit. Need directions? We're easy to find—get directions to our Shore Road location or visit our Avenue P clinic.
Frequently Asked Questions about Physical Therapy
We hear these questions all the time at Evolve Physical Therapy + Sports Rehabilitation. If you're considering physical therapy Brooklyn, you may have wondered about these same things.
Do I need a doctor's referral to start physical therapy in Brooklyn?
In most cases, no, you don't need a doctor's referral. New York State's Direct Access law allows you to see an experienced physical therapist directly for up to 10 visits or 30 days, whichever comes first. This saves you time and gets you on the path to recovery faster. If your treatment needs to continue beyond that, we will coordinate with your doctor. Our experienced team can determine if physical therapy is right for you or if you should see a physician for further evaluation.
Is physical therapy supposed to be painful?
Our goal is always pain relief, not causing more pain. However, it's important to distinguish between "pain" and "therapeutic discomfort." As we work to restore movement or strengthen a muscle, you might feel a temporary discomfort, similar to the feeling after a good workout. This should never be sharp or unbearable. The "no pain, no gain" mentality is a myth in modern physical therapy. We insist on open communication; if something hurts, we will adjust our approach immediately to ensure your treatment is both effective and tolerable.
How long does a typical physical therapy plan last?
The honest answer is: it varies. Every person and condition is different. A mild ankle sprain might take a few weeks, while post-surgical recovery or a chronic issue could take several months. Factors like the severity of your injury, your body's healing process, and your personal goals all influence the timeline. Your consistency is also key; patients who adhere to their home exercise program and attend sessions regularly often see faster results. During your initial evaluation, we'll provide an estimated timeline based on your specific situation and work with you to meet your goals.
Conclusion: Take the First Step to a Healthier Life in Brooklyn
You're ready for a change, and physical therapy Brooklyn offers real, lasting solutions. It's about more than injury recovery; it's about regaining control, moving without pain, and getting back to the life you love.
At Evolve Physical Therapy + Sports Rehabilitation, our philosophy is to evaluate, heal, and strengthen. We provide personalized, hands-on care that addresses the root cause of your discomfort, not just the symptoms. Our drug-free, non-invasive approach empowers you for long-term health. Whether you're an athlete, managing a chronic condition, or recovering from surgery, we're here to guide you.
Pain and limited mobility don't have to be your normal. With our convenient locations across Brooklyn, from Marine Park to Park Slope, expert care is within reach. Take the first step toward a healthier, more active life. Don't wait to feel better.
Ready to take control of your recovery? Find how our specialized programs can help you achieve your goals: Take control of your recovery with sports rehab physical therapy in Brooklyn.
Your journey to better movement starts now.
Pain Management for Herniated Discs: A Comprehensive Treatment Guide
Understanding Herniated Disc Pain and Your Treatment Options
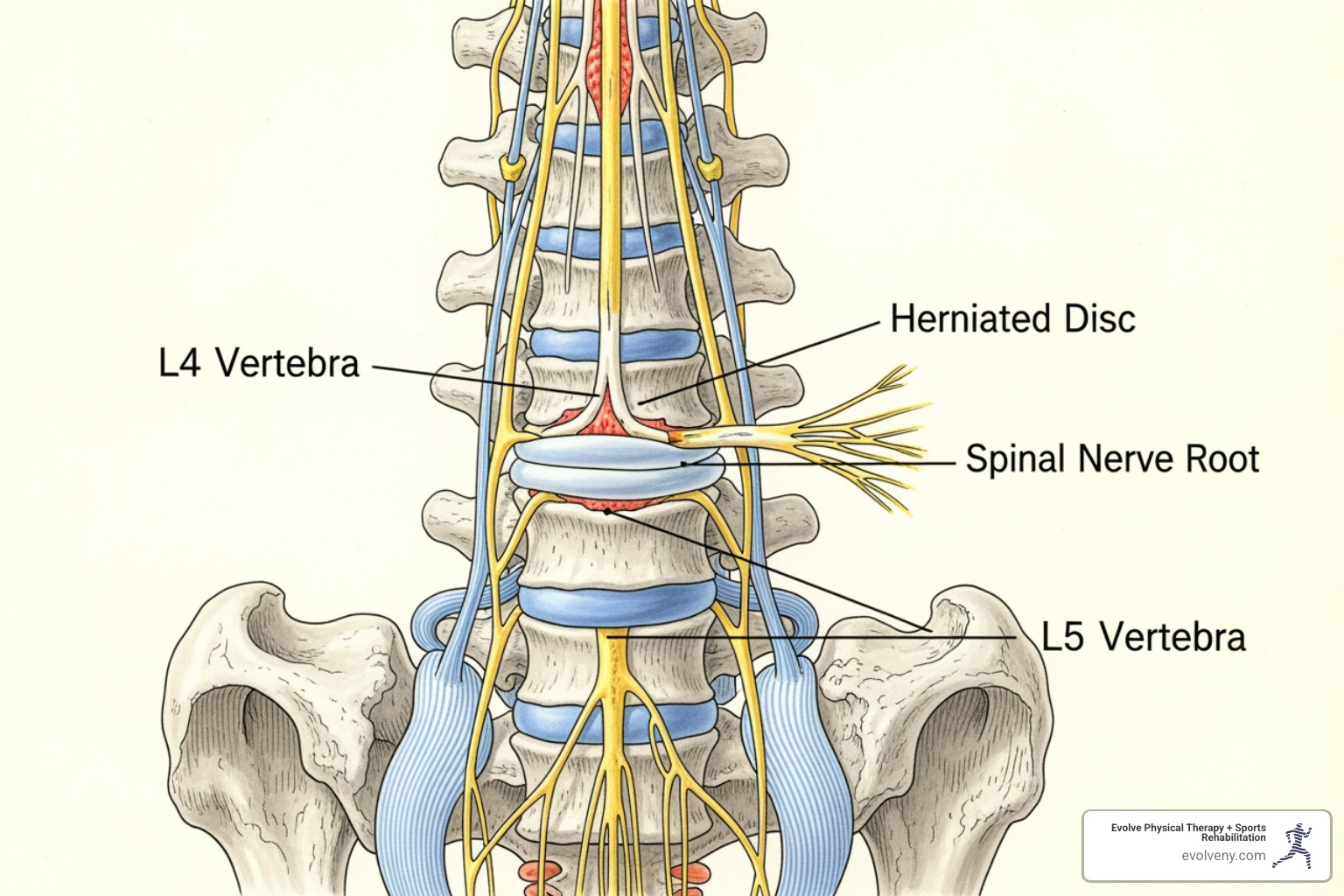
Pain management herniated disc treatment begins with understanding your condition and options. A herniated disc occurs when the soft, gel-like center (nucleus pulposus) of a spinal disc pushes through a crack in its tough outer layer (annulus fibrosus). This can press on nearby nerves, causing pain, numbness, or weakness that radiates down your leg (sciatica) or arm.
Most herniated discs occur in the lumbar spine (lower back), followed by the cervical spine (neck). While the pain can be debilitating, the prognosis is excellent. Over 85% of people improve within 8-12 weeks with conservative treatment, and surgery is rarely needed.
Effective Non-Surgical Treatments:
- Physical Therapy: Strengthens core muscles and relieves nerve pressure.
- NSAIDs: Reduces inflammation and pain (e.g., ibuprofen).
- Epidural Steroid Injections: Delivers targeted anti-inflammatory medication.
- Activity Modification: Avoiding movements that worsen pain while staying active.
- Manual Therapy: Hands-on techniques to improve mobility and reduce symptoms.
Surgery is typically only considered if conservative treatment fails after six weeks, or in cases of progressive muscle weakness or loss of bladder/bowel control (an emergency).
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. With nearly two decades specializing in pain management herniated disc treatment, I've seen how personalized, hands-on therapy helps thousands of New Yorkers avoid surgery and return to the activities they love.

How Herniated Discs Are Diagnosed
An accurate diagnosis is the first step toward relief. At Evolve Physical Therapy, we work with your doctor to pinpoint the cause of your pain through a combination of physical examination and advanced imaging.
A medical doctor will perform a physical and neurological exam, which includes:
- Muscle Strength Tests: To identify weakness caused by nerve compression.
- Sensation Tests: To map out numbness or tingling along nerve pathways.
- Reflex Testing: A diminished reflex can indicate a pinched nerve.
- Straight Leg Raise (SLR) Test: For lower back herniations, this test can reveal nerve root irritation if it causes pain to shoot down your leg.
While physical tests provide valuable clues, imaging confirms the diagnosis.
- MRI (Magnetic Resonance Imaging): The gold standard for diagnosing herniated discs. It uses magnetic fields to create detailed images of soft tissues like discs and nerves, showing exactly where compression is occurring.
- CT Scan: Provides cross-sectional images of the spine and is useful for viewing bone structures and discs.
- Myelogram: A CT scan performed after injecting dye into the spinal fluid to highlight pressure on the spinal cord or nerves.
- X-rays: Cannot show herniated discs but are used to rule out other problems like fractures or spinal alignment issues.
Combining a physical exam with detailed imaging allows your medical team to create the most effective pain management herniated disc strategy for you.
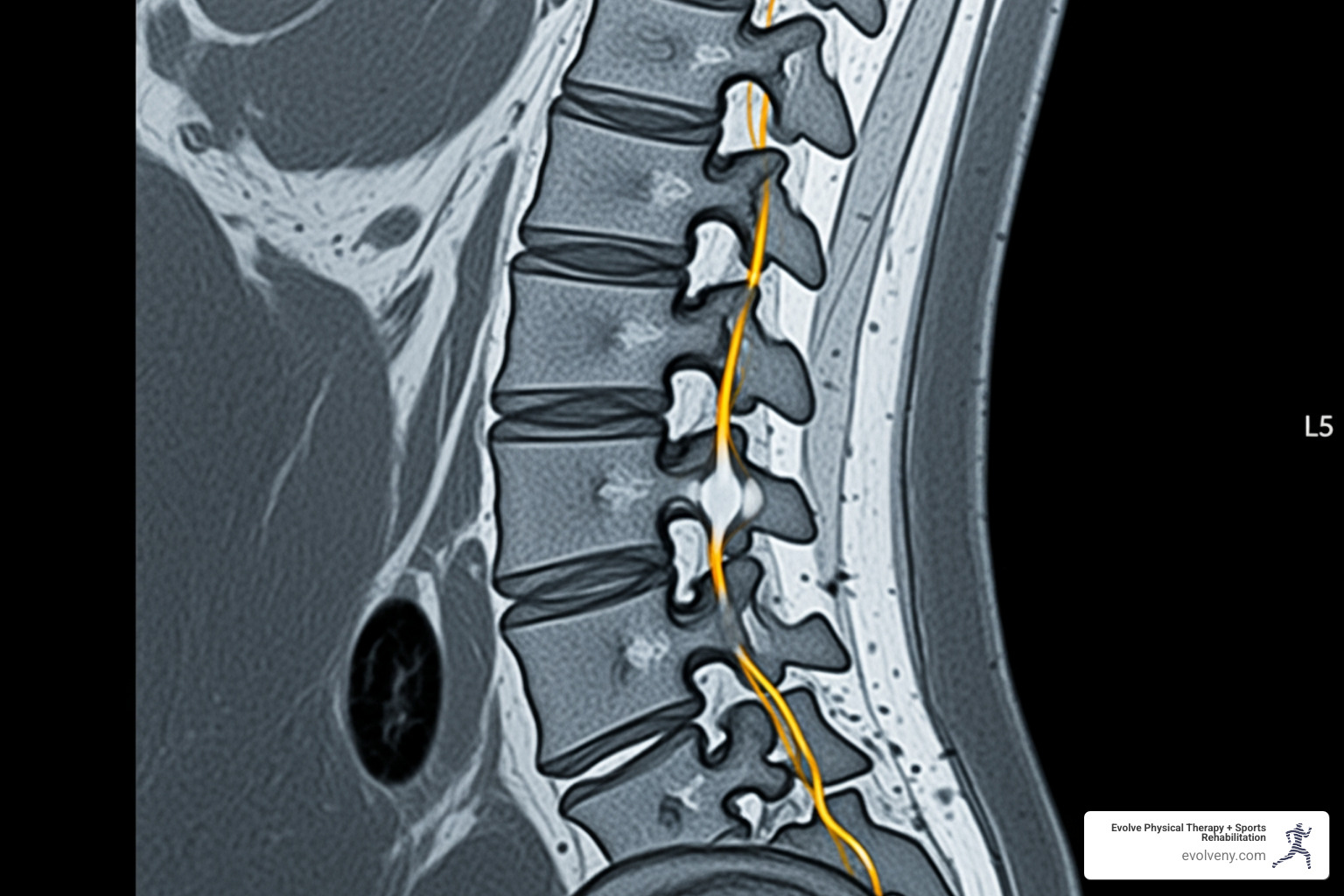
Comprehensive Pain Management for a Herniated Disc: Non-Surgical Options
The great news is that you likely won't need surgery. Over 85% of acute herniated disc symptoms resolve within 8 to 12 weeks with conservative treatment. The foundation of effective pain management herniated disc treatment is staying active. While it seems counterintuitive, staying active is far more essential to recovery than bed rest.
Activity modification is key: listen to your body and temporarily avoid heavy lifting, twisting, and prolonged sitting. The goal is to modify, not eliminate, activity to allow your spine to heal.
The Crucial Role of Physical Therapy
Physical therapy is often the most powerful tool for recovery. At Evolve Physical Therapy in Brooklyn, our hands-on care addresses the root cause of your pain for lasting relief.

A physical therapist will guide you through a program focused on:
- Pain Relief: Using techniques to reduce nerve irritation and muscle spasms.
- Core Strengthening: Building a natural support system for your spine to take pressure off the injured disc.
- Posture Improvement: Correcting daily habits that strain your discs.
- Flexibility: Using gentle stretching to improve range of motion and reduce tension.
Our Brooklyn team specializes in manual therapy combined with targeted exercises. This approach, detailed in our Physical Therapy for Herniated and Bulging Discs Brooklyn and Back Pain Physical Therapy Brooklyn programs, has helped thousands avoid surgery.
Medication-Based Pain Management
Medication can reduce inflammation and pain, enabling you to participate in physical therapy.
- Over-the-counter NSAIDs: Ibuprofen (Advil) or naproxen (Aleve) are a first-line defense against inflammation.
- Prescription Medications: Your doctor may prescribe muscle relaxants, oral corticosteroids for powerful anti-inflammatory effects, or anticonvulsants (like gabapentin) for nerve pain.
- Tricyclic Antidepressants: These can be effective for chronic pain as they increase neurotransmitters in your spine that relieve pain.
- Opioids: Used cautiously for severe, short-term pain only, due to their addictive nature.
Advanced Pain Management: Injections
When other methods aren't enough, injections deliver powerful anti-inflammatory medication directly to the pain source.

- Epidural Steroid Injections (ESIs): A corticosteroid is injected into the epidural space around the nerve roots. ESIs have success rates between 76% and 88% and create a window of pain relief ideal for making progress in physical therapy.
- Selective Nerve Root Blocks (SNRBs): A more targeted injection of a steroid-anesthetic mix around a specific nerve. They are both diagnostic and therapeutic, with success rates of around 75%.
Alternative and Complementary Therapies
Integrating other therapies can improve your recovery.
- Acupuncture: The pain-relieving benefits are evidence-supported, as it can trigger your body's natural pain-relief systems.
- Chiropractic Care: Spinal manipulation may help relieve nerve pressure for some individuals.
- Massage Therapy: Relaxes tense muscles, improves blood flow, and provides pain relief.
- Heat and Cold Therapy: Use ice packs initially to reduce inflammation, then switch to heat to relax muscles.
Our Physical Therapy and Pain Management approach integrates these methods for comprehensive care.
When Is Surgery Considered for a Herniated Disc?
Surgery is rarely the first option for pain management herniated disc treatment. It's typically considered only when specific criteria are met:
- Failure of conservative treatment: Pain and symptoms persist after six or more weeks of non-surgical care.
- Progressive neurological deficits: Increasing muscle weakness, numbness, or loss of sensation that impacts daily function.
- Cauda equina syndrome: A rare medical emergency causing loss of bladder/bowel control and severe numbness in the groin. This requires immediate surgical intervention.
- Intolerable pain: Severe pain that doesn't respond to other treatments and significantly impacts quality of life.
Microdiscectomy
This is the gold standard, accounting for approximately 90% of surgeries for this condition. A surgeon removes only the herniated portion of the disc pressing on the nerve. It is minimally invasive, and many patients go home the same day. Our specialized Rehab for Spinal Procedures Brooklyn supports recovery.
Laminectomy
In a laminectomy, the surgeon removes a portion of the lamina (the bony arch of the vertebra) to create more space for the nerves. This relieves pressure without removing disc material. Recovery time varies depending on whether the procedure is traditional or microscopic. Our Prehab for Spinal Procedures Brooklyn can help you prepare.
Spinal Fusion and Artificial Disc Replacement (ADR)
- Spinal Fusion: This procedure permanently joins two or more vertebrae to eliminate painful motion. It is less common for a simple herniated disc and is typically reserved for cases with spinal instability.
- Artificial Disc Replacement (ADR): A newer alternative to fusion, ADR involves replacing the damaged disc with an artificial one. The goal of ADR is to preserve movement in the spine, allowing for more natural mechanics and often a faster recovery than fusion.
Lifestyle Modifications and Self-Care for Long-Term Relief
The real secret to lasting pain management herniated disc success is about what you do every day. At Evolve Physical Therapy in Brooklyn, we empower patients with the knowledge to make smart lifestyle choices for long-term spinal health.
Key self-care strategies include:
- Patient Education: Understanding your condition, its cause, and your pain triggers is the first step toward taking control of your recovery.
- Ergonomics: If you sit at a desk, adjust your chair, monitor, and keyboard to reduce spinal strain. A lumbar support cushion can make a significant difference.
- Good Posture: Consciously maintaining good posture while sitting, standing, and walking distributes weight evenly and reduces pressure on your discs.
- Safe Lifting Techniques: Always bend at your knees, not your waist. Use your leg muscles to lift, keep the object close to your body, and never twist while lifting.
- Weight Management: Excess body weight, especially around the abdomen, adds stress to your lower back. Losing even a modest amount of weight can provide significant relief.
- Regular, Low-Impact Exercise: Activities like swimming, cycling, or walking strengthen the core muscles that support your spine without jarring it. For more guidance, check out our blog post: Low Back Pain: Why You Have It and How to Fix It.
- Stopping Smoking: Quitting smoking improves oxygen supply to your discs, which slows degeneration and promotes healing.
The prognosis for herniated discs is very positive, but there is a 20-25% chance of re-herniation. Committing to these lifestyle changes is your best defense against future pain.
Frequently Asked Questions about Herniated Disc Pain
Here are answers to common questions about pain management herniated disc treatment.
Can a herniated disc heal on its own?
Yes, most can. The body often reabsorbs the herniated disc material over time, relieving pressure on the nerve. This natural process, supported by conservative treatments like physical therapy, leads to significant improvement for most people within weeks to months. Our role at Evolve Physical Therapy is to create the optimal conditions for your body to heal itself.
What activities should be avoided with a herniated disc?
While staying active is crucial, you should temporarily modify certain movements to avoid re-injury. Avoid:
- High-impact sports: Running, jumping, and contact sports.
- Heavy lifting: This puts tremendous strain on your discs.
- Twisting motions: Such as swinging a golf club or reaching behind you.
- Prolonged sitting: This increases pressure on lumbar discs. Stand and move every 30 minutes.
- Bending at the waist: Always bend your knees and keep your back straight.
How long does pain from a herniated disc last?
The duration varies, but there are general patterns. With consistent conservative treatment, the acute pain for most people improves significantly within 6 to 12 weeks. Some may experience chronic or recurring pain, especially if the underlying issues aren't addressed. The key to lasting relief is a comprehensive strategy that includes physical therapy and lifestyle changes to build a strong, resilient spine.
Take Control of Your Herniated Disc Pain in Brooklyn
You don't have to live with the limitations of a herniated disc. The most important takeaway is that most people get better without surgery. Over 85% of acute symptoms resolve with conservative care like physical therapy and smart activity choices.
At Evolve Physical Therapy in Brooklyn, we see this happen every day for patients from Marine Park, Gravesend, Midwood, and Park Slope. We reject cookie-cutter approaches in favor of personalized pain management herniated disc strategies custom to your body and goals.
Physical therapy is the core of effective treatment. Through hands-on manual therapy, targeted strengthening, and patient education, we address your immediate pain and build long-term spinal health. The exercises you learn become your shield against future injury, helping you return to the activities you love.
Even if surgery becomes necessary, our specialized Prehab for Spinal Procedures Brooklyn and Rehab for Spinal Procedures Brooklyn programs support you at every step.
With the right guidance, you can return to your regular activities, often stronger than before. Our hands-on approach means we take the time to understand your unique pain and build a treatment plan for your real life.
Ready to take the first step? We're here in Brooklyn to create a plan that works for you.
Start your recovery with expert Physical Therapy for Herniated and Bulging Discs in Brooklyn
Post-Op Power-Up: Your Guide to Physical Therapy After Surgery
Why Surgery is Just the Beginning of Your Healing Journey
Post surgery physical therapy is a critical component of recovery that helps you regain strength, mobility, and function after an operation. Here's what you need to know:
Quick Answer: What is Post-Surgery Physical Therapy?
- Purpose: Restore movement, rebuild strength, and return you to daily activities safely
- When to Start: Typically within 24-48 hours to 2 weeks post-op, depending on your surgery
- Duration: Ranges from 6 weeks to 6+ months based on procedure complexity
- Key Benefits: Faster recovery, reduced pain, prevention of complications like blood clots and muscle loss
- What to Expect: Graduated phases from gentle movement to functional strengthening
Surgery is only the first step. As one orthopedic surgeon notes, "the success of their procedures is highly dependent on a personalized physical therapy plan." Without proper rehabilitation, you risk improper healing, reduced range of motion, and chronic pain.
Limiting mobility during recovery can lead to serious complications. Your body needs guided movement to heal properly, prevent scar tissue buildup, restore circulation, and rebuild lost strength. Physical therapy provides a structured, evidence-based roadmap to full functional recovery.
Research shows that patients who begin physical therapy within 24 hours after surgery can accelerate their recovery by up to 40%. Those aged 40-60 who receive proper post-operative PT reduce their complication risk by 60%. These numbers represent the difference between a smooth recovery and months of unnecessary struggle.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. With nearly two decades specializing in post surgery physical therapy, I've seen how the right rehabilitation approach transforms surgical outcomes.
Why Post-Surgical Physical Therapy is Essential for Your Recovery
After surgery, your surgeon has repaired the damage, but that's only half the battle. Your body has been through trauma, and without proper rehabilitation, you're leaving your recovery to chance. Post surgery physical therapy bridges the gap between the operating room and your real life, helping you recover your function, strength, and independence.
Pain and swelling management are among the first things we address. While medication helps, we use gentle manual therapy, targeted exercises, and modalities like ice to help your body manage pain naturally and reduce inflammation. Many patients find they need fewer pain medications when actively engaged in therapy.
Here's where PT becomes truly essential: preventing complications. Immobility is risky. It can lead to dangerous blood clots, muscle wasting within days, and stiff joints. For patients who've had abdominal or chest surgery, specialized breathing exercises can reduce the risk of lung complications by up to 40%.
We work on restoring your range of motion because stiff joints make everything harder. Using hands-on techniques and specific stretches, we help you move freely again. Every degree of motion we restore is a piece of your independence coming back.
Rebuilding muscle strength happens gradually and strategically. We design progressive exercise programs that safely challenge your muscles, building the stability and support your body needs. We also use soft tissue manipulation to break down restrictive scar tissue that can limit movement and cause discomfort.
The goal is improving your quality of life. We want you walking through Prospect Park, playing with your grandkids, or simply carrying groceries without a second thought. The psychological boost that comes from seeing yourself get stronger is powerful medicine.
Research backs this up. Studies on physiotherapy strategies for postoperative rehabilitation show that early mobilization prevents muscle atrophy, joint stiffness, and circulation problems. Our approach to post surgery physical therapy in Brooklyn follows these evidence-based strategies because they work. You can read more about optimizing recovery through physiotherapy strategies.
Surgery fixes the problem. Physical therapy makes sure you get your life back.
Your Recovery Roadmap: The Phases of Post Surgery Physical Therapy
Your recovery is a journey with distinct landmarks. Post surgery physical therapy follows a structured progression, with each phase building on the last to take you from initial healing to full function. Your timeline is unique, influenced by your surgery, health, and age. We work in close partnership with your surgeon, ensuring every step aligns with your body's healing.
Phase 1: The Acute/Protective Phase (Weeks 0-4)
This first phase is about protecting the surgical site to create the right conditions for healing. This may mean using a sling or limiting weight on a limb. We control pain and swelling with ice, compression, and elevation, ensuring exercises don't increase pain significantly. Even in this phase, movement is medicine. We guide you through passive range of motion exercises, where the therapist moves your limb, and simple ankle pumps to prevent blood clots. For shoulder surgeries, we use gentle pendulum swings, and for abdominal or chest surgeries, we focus on diaphragmatic breathing to reduce lung complication risks.
Phase 2: The Mobility/Early Strengthening Phase (Weeks 4-8)
As healing progresses, we start waking up muscles and reclaiming movement.

You become more active in your recovery, transitioning to active-assisted exercises where you do some of the work. Your therapist uses manual therapy to improve flexibility. Isometric exercises (contracting muscles without moving the joint) are key for rebuilding strength safely. We introduce light strengthening with resistance bands and begin proprioception training to help your body relearn its position in space, improving balance and coordination.
Phase 3: The Functional/Return-to-Activity Phase (Weeks 8+)
This is where you get back to living your life. We progress to more challenging exercises with weights and bands to build functional strength for real-life activities. Endurance and advanced balance exercises become a focus. For athletes, we design sport-specific drills, including agility and plyometrics, to prepare your body for the demands of your game. Research shows this step can help athletes return to sports 8-12 weeks sooner. We practice the movements specific to your life, ensuring you can perform them confidently and safely.
Common Treatments and Modalities Used in Post Surgery Physical Therapy
Throughout these phases, we use a toolkit of techniques:
- Manual therapy: Hands-on techniques to reduce pain, improve circulation, and restore movement.
- Therapeutic exercise: Custom-designed programs to restore strength, flexibility, and endurance.
- Heat and cold therapy: To manage pain, swelling, and muscle tightness.
- Electrical stimulation (TENS): Delivers mild electrical currents to block pain signals.
- Therapeutic ultrasound: Uses sound waves to promote tissue healing and reduce inflammation.
- Myofascial release: A manual technique to manage scar tissue and release deep tension.
- Gait training: Helps you relearn proper walking patterns and improve balance.
Your Partner in Recovery: The Role of You and Your Physical Therapist
Recovery from surgery is an active partnership. At Evolve Physical Therapy in Brooklyn, we see post surgery physical therapy as a team effort. We bring the roadmap and expertise; you drive the journey. Together, we'll steer the path from post-operative healing back to your life.
The Physical Therapist's Role: Your Expert Guide
Your physical therapist is a musculoskeletal expert who understands how the body heals. We practice evidence-based care, but we also recognize you're a whole person with unique goals. Our role includes:
- Comprehensive assessment: We evaluate your movement, pain, and strength to understand your starting point and what you hope to achieve.
- Custom treatment plan: We design a plan specifically for your body and surgery, collaborating closely with your surgeon.
- Monitoring and adjusting: We continuously track your progress, modifying the plan as you heal to overcome plateaus or advance your program.
- Patient education: We teach you the "why" behind each exercise and how to protect your body, empowering you with knowledge.
- Hands-on techniques: We use manual therapy to improve mobility, reduce pain, and break down scar tissue.
The Patient's Role: How to Maximize Your Results
Your active participation transforms good outcomes into great ones. You are the most important member of your recovery team. To maximize your results:
- Consider "pre-hab": Starting physical therapy before surgery can strengthen muscles and improve motion, giving your body a head start on recovery.
- Adhere to your home exercise program: The exercises we assign are your secret weapon. Consistency can reduce your overall healing time by up to 40%.
- Communicate openly about pain: We need to know what you're feeling. There's "good pain" (muscle soreness) and "bad pain" (sharp, stabbing). Never push through bad pain.
- Be patient and persistent: Recovery has ups and downs. Trust the process, and know we're here to support you through challenges and celebrate victories.
- Focus on nutrition: Your body needs adequate protein, vitamins, and minerals to repair tissues and build muscle.
Tailoring the Treatment: PT Protocols for Different Surgeries
Post surgery physical therapy isn't a cookie-cutter approach. What works for a hip replacement won't be right for an ACL reconstruction. Every surgery requires its own carefully crafted protocol, which we customize for your body, surgery, and timeline in collaboration with your surgeon.

Orthopedic Surgeries: Joint Replacements & Fracture Repair
For joint replacements (knee, hip, shoulder) or fracture repairs, the focus is on teaching your body how to use the new or repaired structure. This involves a careful weight-bearing progression, guided by your healing stages. We use gait analysis to correct limping or other compensatory patterns that can cause pain elsewhere. The goal is to restore joint mechanics for smooth, natural movement, whether you're climbing stairs in Midwood or walking in Prospect Park.
For more details, you can explore this resource: Read about specific rehabilitation protocols.
Soft Tissue Repairs: ACL, Rotator Cuff, and Tendons
Soft tissue surgeries (ACL, rotator cuff, Achilles tendon) require a delicate approach. Protecting the repaired tissue is critical, often involving a sling or restricted movement for several weeks to prevent re-injury. We use gradual loading strategies, introducing stress in tiny, calculated increments to allow the tissue to build strength without being overwhelmed. For example, rotator cuff rehab prioritizes restoring motion before adding resistance, a process that requires patience and precision over several months.
Here's an example of a detailed rotator cuff repair guide: Example of a rotator cuff repair protocol.
Abdominal and Core Surgeries
After hernia repair or other core surgeries, we focus on rebuilding strength while protecting the incision. We teach core stabilization exercises that engage deep muscles without straining the repair. Diaphragmatic breathing is a foundational technique. We enforce strict lifting precautions and teach proper mechanics to avoid strain. You'll also learn simple but crucial techniques like self-splinting (using a pillow for support when coughing) to manage discomfort and protect the healing tissues.
For a comprehensive look at this process, check out this guide: View an abdominal core surgery rehab guide.
The bottom line is that we have the expertise to guide you through a surgery-specific, personalized rehabilitation program that respects your body's healing timeline while pushing you toward your recovery goals.
Frequently Asked Questions about Post-Surgical Physical Therapy
It's normal to have questions about your recovery. We've guided hundreds of patients through their post surgery physical therapy journey in Brooklyn, and here are answers to the most common concerns.
When should I start physical therapy after surgery?
Your surgeon gives the final okay, but modern research favors early mobilization. For many procedures, starting gentle movements within 24-48 hours can prevent complications like blood clots and accelerate recovery by up to 40%. These initial movements are simple, like ankle pumps in bed. The formal start of outpatient PT may vary from a few days to a couple of weeks post-op, depending on the surgery, but the principle of early, safe movement is key.
How long will I need post-surgical physical therapy?
Recovery timelines are unique. The duration depends on the type of surgery (a minor procedure may need 6 weeks; a complex repair can take 6+ months), your overall health, and your recovery goals. Returning to competitive sports will take longer than returning to comfortable daily walks. Patients who are consistent with their home exercise program often heal significantly faster. We'll provide a realistic timeline at your first visit and adjust it as you progress.
Will physical therapy be painful?
Some discomfort after surgery is normal, but physical therapy should not cause "bad" pain. Our job is to work with you to distinguish between "good pain" (the muscle soreness that signals progress) and "bad pain" (sharp, stabbing, or worsening pain that is a warning sign). Our rule is that exercises shouldn't increase your pain by more than 2 points on a 10-point scale. Communication is everything. Your honest feedback allows us to adjust your program to a challenging but safe level. The goal is a productive, manageable recovery, and most of our patients feel better after their sessions, not worse.
Conclusion: Taking the First Step on Your Road to Recovery
Surgery is just the beginning. The real change happens in the weeks and months that follow, and post surgery physical therapy is your most powerful tool for a successful recovery.
This process empowers you to take control, actively rebuilding your body and your confidence. By committing to rehabilitation, you're investing in reduced pain, faster healing, and the prevention of long-term complications. You're building a stronger, more resilient version of yourself.
At Evolve Physical Therapy + Sports Rehabilitation, we've guided countless Brooklyn residents through this process. Our hands-on, personalized approach partners with you to achieve your goals, whether that's walking in Prospect Park or returning to your sport. We've seen patients who could barely walk return to running marathons—this is what happens when expert guidance meets patient dedication.
Your recovery is too important to leave to chance. Taking that first step toward proper rehabilitation is the best decision you can make for your surgical outcome.
Ready to begin? We're here to guide you every step of the way.
From Aspiring to Assisting: Your Path to Pediatric PTA
Why Becoming a Pediatric Physical Therapy Assistant is a Rewarding Career Path

A pediatric physical therapy assistant is a licensed healthcare professional who works under a physical therapist's supervision to help children (from birth to age 21) improve their strength, mobility, and independence through therapeutic exercises and play-based interventions.
Quick Path Overview:
- Education: Complete a 2-year accredited associate degree program.
- Examination: Pass the National Physical Therapy Exam (NPTE).
- Licensure: Obtain your state-specific PTA license.
- Specialization: Gain 2,000 hours of experience (500 in pediatrics) for advanced proficiency.
If you're drawn to helping children overcome physical challenges, this is a meaningful career path. Pediatric PTAs play a crucial role in treating conditions from cerebral palsy to sports injuries. You'll guide young patients through strengthening programs, teach families how to continue care at home, and witness children learn to crawl, walk, and play in settings like hospitals, schools, and rehabilitation centers.
The demand is strong, with the field expected to grow much faster than average. Physical therapist assistants earn an average annual salary of about $65,000, with top earners making over $80,840.
I'm Lou Ezrick, founder of Evolve Physical Therapy in Brooklyn. While my practice focuses on adult rehabilitation, I've worked with pediatric specialists and understand the dedication required for this role. In this guide, I'll walk you through what you need to know to start this rewarding career.
The Essential Role of a Pediatric Physical Therapy Assistant

A pediatric physical therapy assistant is a vital link between a child's treatment plan and their real-world progress. Working under a licensed physical therapist, PTAs help children improve movement, reduce pain, and build skills for everyday life. This role requires technical knowledge and a special talent for connecting with kids.
Pediatric PTAs collaborate with physical therapists to carry out treatment plans and partner with families to support therapy at home. This team approach often extends to other specialists, like occupational therapists and speech-language pathologists. The impact on a child's development can be life-changing, opening doors to independence by helping them reach motor milestones, improve balance, and gain the physical skills needed for school and play.
For more insights into how physical therapy supports children's development, explore our resources on kids physical therapy.
What Conditions Do Pediatric PTAs Help Treat?
Pediatric physical therapy assistants work with children facing a wide range of physical challenges, from congenital conditions to injuries. The goal is always to help each child move better and live fuller lives.
Common conditions treated include:
- Cerebral palsy: To improve muscle control, balance, and mobility.
- Developmental delays: Providing targeted interventions to help infants and toddlers catch up on milestones like sitting or walking.
- Sports injuries: Guiding young athletes through safe rehabilitation.
- Scoliosis: Using exercises to strengthen core muscles and improve posture.
- Muscular dystrophy: Helping maintain range of motion and strength.
- Traumatic brain injuries: Working to regain balance, coordination, and functional movement.
Other conditions include cystic fibrosis, congenital muscular torticollis, developmental dysplasia of the hip, and clubfeet. PTAs also help children with autism spectrum disorder improve motor skills.
To learn more about our specialized approach, visit our page on pediatric physical therapy for kids.
Daily Duties of a Pediatric Physical Therapy Assistant
No two days are the same for a pediatric physical therapy assistant, which is part of the job's appeal. The core responsibility is implementing the physical therapist's treatment plan, often through creative, play-based methods.
- Implementing Treatment Plans: This involves guiding children through specific exercises that often look like play. An obstacle course might develop motor planning, while a game of catch improves hand-eye coordination.
- Play-Based Therapy: This approach is essential. Instead of repetitive drills, a PTA might use tunnels, swings, or building blocks to achieve therapeutic goals in a fun, engaging way.
- Documentation: PTAs carefully track each child's response to treatment, noting progress and any changes. This data helps the supervising PT adjust the care plan.
- Family Education: A crucial duty is teaching parents and caregivers how to continue therapy at home, empowering them to support their child's progress between sessions.
Other tasks include gait training, range of motion exercises, and preparing treatment areas to ensure a clean, safe environment for young patients.
Where Do Pediatric PTAs Work?
The versatility of a pediatric physical therapy assistant leads to career opportunities in many settings:
- Children's hospitals for acute care and post-surgical recovery.
- Outpatient clinics for ongoing therapy for chronic conditions or injuries.
- Schools to help children with disabilities participate in educational activities.
- Home healthcare services to bring therapy directly to families.
- Rehabilitation centers for intensive, multidisciplinary care.
According to the U.S. Bureau of Labor Statistics, PTAs work across these settings, with pediatric specialists naturally gravitating toward environments designed for children's needs.
Your Roadmap to Becoming a Pediatric PTA

The journey to becoming a pediatric physical therapy assistant is a straightforward, two-year process that combines classroom learning with hands-on clinical training. This blend of theory and practice ensures you are fully prepared to help children upon earning your license. Let's walk through the steps.
Step 1: Earn Your Associate's Degree from an Accredited Program
The foundation of your career is an Associate's degree from a program accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE). This accreditation is mandatory to be eligible for the national licensing exam. You can find an accredited PTA program on CAPTE's website. These programs typically take two years.
Coursework is intensive, covering anatomy, physiology, and kinesiology (the study of human movement). You'll also take foundational science courses and medical terminology. Many programs offer pediatric-focused electives to specialize in child development and treatment techniques.
A significant part of your education is clinical training. You'll work in real healthcare settings under the supervision of licensed physical therapists and PTAs. This hands-on experience is invaluable for learning how to apply therapeutic principles to children with unique needs and personalities.
Step 2: Pass the National Physical Therapy Exam (NPTE)
After graduation, you must pass the National Physical Therapy Examination (NPTE) for PTAs, administered by the Federation of State Boards of Physical Therapy (FSBPT). This standardized exam ensures you are ready to practice safely and effectively.
The NPTE is a four-hour, 200 multiple-choice question exam covering physical therapy interventions, data collection, diseases, and professional responsibilities. Your degree program is designed to prepare you for this test.
Study resources are available, including the FSBPT's Practice Exam and Assessment Tool (PEAT). You can learn about the NPTE and practice with PEAT on their website. If you don't pass on your first attempt, you can retake the exam.
Step 3: Obtain Your State License
Passing the NPTE is the penultimate step; the final one is obtaining your state license. Every state requires licensure to practice, and each has its own specific requirements in addition to the NPTE.
This process typically involves submitting your NPTE scores, passing a state-specific jurisprudence exam on local laws, undergoing a background check, and paying application fees. In New York, for example, you apply through the state licensing board.
Once licensed, you must maintain it through renewal, usually every two years, which requires completing continuing education credits (CEUs). This commitment to lifelong learning keeps you current with best practices. The Federation of State Boards of Physical Therapy website is the best resource for state-specific requirements.
Skills, Salary, and Career Growth in Pediatric PT
Being a pediatric physical therapy assistant requires a unique blend of physical strength, mental agility, and genuine heart. The physical demands are real: you'll be on your feet, bending, kneeling, and lifting children and equipment. It's an active role that combines being a healthcare provider with a professional playmate.
Beyond physical capabilities, key personal attributes are essential for success:
- Compassion: A genuine desire to help children and their families through their challenges.
- Patience: Progress happens at a child's pace, and a patient approach builds trust.
- Communication: You must explain exercises to children, listen to parents, and report clearly to PTs.
- Creativity: The ability to turn therapy into an engaging adventure is a powerful tool for motivating kids.
- Problem-Solving: Adaptability is key to modifying treatments and finding new ways to motivate a child.
What is the Salary for a Pediatric Physical Therapy Assistant?
The financial outlook for a pediatric physical therapy assistant is positive. According to the U.S. Bureau of Labor Statistics, PTAs earn an average annual salary of about $65,000. The salary range can vary, with the highest 10 percent earning more than $80,840.
Factors influencing your salary include:
- Location: Areas with a higher cost of living, like Brooklyn, NY, often have higher salaries.
- Experience: More years in the profession typically lead to higher earning potential.
- Work Environment: Settings like home healthcare services and nursing care facilities often rank among the top-paying industries.
- Specialization: Advanced proficiency in pediatrics can command higher pay.
This career offers a stable, competitive income alongside personal fulfillment.
Career Advancement and Specialization
Your journey as a pediatric physical therapy assistant begins with licensure, but there are many opportunities for growth. The American Physical Therapy Association (APTA) offers the PTA Advanced Proficiency Pathway, a formal way to demonstrate advanced skills.
To achieve this recognition in pediatrics, you'll need at least 2,000 hours of work experience, with a minimum of 500 hours in pediatrics, plus other requirements. This designation showcases your expertise and can open doors to new opportunities.
Other career growth paths include:
- Supervising roles: Mentoring PTA students or newer PTAs.
- Lead PTA positions: Taking on administrative duties, scheduling, and team coordination.
- Specialized caseloads: Focusing on areas like early intervention or sports physical therapy.
- Education roles: Teaching in PTA programs.
The APTA Section on Pediatrics is an excellent resource for networking, education, and research in the field, supporting your continuous professional development.
Pediatric PT vs. PTA: Understanding the Key Differences
In pediatric physical therapy, there are two distinct roles: the Pediatric Physical Therapist (PT) and the Pediatric Physical Therapist Assistant (PTA). While both are committed to helping children, they have different educational paths, responsibilities, and scopes of practice.

| Feature | Pediatric Physical Therapist (PT) | Pediatric Physical Therapist Assistant (PTA) |
|---|---|---|
| Education Level | Doctor of Physical Therapy (DPT) degree (typically 3 years post-bachelor's) | Associate of Applied Science (AAS) degree (typically 2 years) |
| Primary Role | Evaluates, diagnoses, develops and modifies treatment plans, performs complex interventions | Implements treatment plans developed by the PT, collects data, performs routine interventions |
| Scope of Practice | Autonomous practitioner, responsible for initial evaluation, re-evaluation, diagnosis, prognosis, and discharge planning. | Works under the direct supervision of a licensed PT; cannot evaluate, diagnose, or independently alter a treatment plan. |
| Responsibilities | - Conducts comprehensive patient evaluations - Establishes patient diagnoses - Develops individualized treatment plans and goals - Performs complex assessments and interventions - Modifies treatment plans based on patient progress - Supervises PTAs and aides |
- Implements components of the treatment plan - Performs therapeutic exercises and modalities - Observes and documents patient responses and progress - Reports findings to the supervising PT - Educates patients and families on home exercise programs - Assists with patient transfers and equipment setup |
| Supervision | Supervises PTAs and physical therapy aides. | Requires supervision by a licensed PT. The level of supervision can vary by state and setting. |
The key difference is education and scope of practice. A PT earns a Doctor of Physical Therapy (DPT) degree, a post-bachelor's program. A pediatric physical therapy assistant earns a two-year Associate's degree, making it a faster path into the field.
The PT is the lead clinician who evaluates, diagnoses, and creates the treatment plan. The PTA is the skilled implementer who carries out that plan, working directly with the child day-to-day. While a PTA cannot independently change a treatment plan or perform initial evaluations, their role is vital for building rapport and executing the therapeutic activities.
The Collaborative PT-PTA Team
At Evolve Physical Therapy, we know the best outcomes result from seamless teamwork. The PT-PTA relationship is a partnership built on collaboration and communication.
The PT performs the initial evaluation and develops the care plan, then delegates portions to the PTA. The PTA acts as the PT's eyes and ears during sessions, implementing exercises, observing the child's response, and documenting progress. This information is crucial for the supervising PT to make informed decisions about modifying the treatment.
This collaborative model allows each professional to work at the top of their license, ensuring children receive comprehensive and effective care. To learn more about the profession, the American Physical Therapy Association (APTA) is an excellent resource.
Frequently Asked Questions about a Career as a Pediatric PTA
Choosing a career is a big decision. Here are clear, honest answers to common questions about becoming a pediatric physical therapy assistant.
How long does it take to become a pediatric PTA?
Typically, it takes about two years. This timeframe includes completing a 2-year accredited Associate's degree program, which combines classroom study with hands-on clinical experience. After graduating, you must pass the National Physical Therapy Examination (NPTE) and obtain your state license to begin practicing.
What are the most important skills for a pediatric PTA?
Success in this field requires both technical and soft skills. Beyond the clinical knowledge gained in your degree program, the most crucial attributes are:
- Patience and Compassion: To connect with children and their families.
- Creativity: To make therapy sessions fun and engaging.
- Strong Communication: To explain exercises to a child, listen to a parent, and report to a PT.
- Physical Stamina: The job is active and requires you to be on your feet, bending, and lifting.
- Keen Observation: To notice subtle changes in a child's progress.
Is becoming a pediatric PTA a good career choice?
Yes, for those who are passionate about helping children, it is an outstanding career choice. Here's why:
- Job Security: The field is projected to grow much faster than average, ensuring strong demand.
- Good Salary: The national average salary is around $65,000, with opportunities for higher earnings with experience and specialization.
- Meaningful Impact: You play a direct role in helping children achieve life-changing milestones, like taking their first steps or returning to a beloved sport.
- Variety: You can work in diverse settings, including hospitals, clinics, schools, and home health.
- Growth Opportunities: You can pursue advanced proficiency in pediatrics through the American Physical Therapy Association after gaining 2,000 hours of work experience (with 500 in pediatrics).
If you enjoy hands-on healthcare and find satisfaction in helping others overcome physical challenges, this demanding but highly rewarding career could be an excellent fit.
Conclusion: Start Your Journey to Help Children Thrive
The path to becoming a pediatric physical therapy assistant is more than a career choice—it's a chance to make a meaningful impact. You'll witness and contribute to life-changing victories, from a child's first independent step to a young athlete's return to the game.
This hands-on profession allows you to build trust, celebrate progress, and give families hope. At Evolve Physical Therapy, while our Brooklyn clinics focus on adults, we deeply respect the unique blend of compassion, skill, and creativity that pediatric PTAs bring to their work.
If you are drawn to a career where play becomes therapy and every milestone matters, this could be your calling. The demand is strong, the work is rewarding, and the children need dedicated professionals like you.
To learn more about how we approach pediatric care in our Brooklyn community, visit our page on pediatric physical therapy in Brooklyn. Your journey to helping children thrive starts now.

































